Abstract
Background
South-Asia is known as a hub for multidrug-resistant (MDR) bacteria. Unfortunately, proper surveillance and documentation of MDR pathogens is lacking in Pakistan. The alarming increase in the prevalence of extended-spectrum β-lactamase (ESBL)-producing Enterobacteriaceae is a serious problem. From this perspective, we analysed published data regarding ESBL-producing Enterobacteriaceae in different regions of Pakistan.
Methods
A meta-analysis was performed to determine the prevalence of ESBL-producing Enterobacteriaceae in Pakistan. A Web-based search was conducted in electronic databases, including PubMed, Scopus and PakMedi Net (for non-indexed Pakistani journals). Articles published (in either indexed or non-indexed journals) between January 2002 and July 2016 were included in the study. Relevant data were extracted, and statistical analysis was performed using the Metaprop command of STATA version 14.1.
Results
A total of 68 studies were identified from the electronic data base search, and 55 of these studies met our inclusion criteria. Pakistan’s overall pooled proportion of ESBL-producers was 0.40 (95% CI: 0.34–0.47). The overall heterogeneity was significant (I2 = 99.75%, p < 0.001), and significant ES = 0 (Z = 18.41, p < 0.001) was found. OXA, SHV, TEM and CTX-M were the most commonly found gene variants for ESBLs in these studies.
Conclusion
The prevalence of ESBL-producing Enterobacteriaceae is high in Pakistan. Little is known about the annual frequency of ESBLs and their prevalence in different provinces of Pakistan. No data are available regarding ESBL frequency in Baluchistan. This underscores an urgent demand for regular surveillance to address this antimicrobial resistance problem. Surveillance to better understand the annual ESBL burden is crucial to improve national and regional guidelines.
Similar content being viewed by others
Background
Antimicrobial resistance has been declared a global threat to public health, as a massive increase in this problem has been observed in different parts of the world [1]. Although the magnitude of the antimicrobial resistance problem differs by country and geographical region, South-Asia is considered to be a major region for multidrug-resistant (MDR) bacteria [2]. The reported frequency of MDRs is increasing, putting strain on the public health organizations that are attempting to control this issue in many countries [3].
The alarming increase in the prevalence of extended-spectrum β-lactamase (ESBL)-producing Enterobacteriaceae has serious consequences for treatment outcomes [4]. Escherichia coli and Klebsiella spp. are important pathogens isolated from community-acquired and nosocomial-acquired infections, and have been studied extensively [5–22]. The ESBL enzymes produced by these bacteria make them resistant to the first-choice antibiotic therapies that are commonly used. ESBL-positive strains are associated with a delay in the commencement of suitable antibiotic therapy, which consequently lengthens hospital stay and raises hospital costs [23]. Failure of antibiotic therapy is responsible for higher mortality rates in patients infected with these bacteria [24].
Epidemiological studies around the world have investigated the prevalence of ESBL-producing Enterobacteriaceae and they have seen multiple mechanisms of drug-resistance [25–33]. Several studies on ESBL infection in Asian-pacific region reported 60–80% of such cases were nosocomial-acquired while, remaining were community-acquired infections [1, 3, 34–39]. Over the last decade in Pakistan, an increase in resistance against quinolones has been observed in Enterobacteriaceae [40]. However, not much is known about fluoroquinolone-resistance in ESBLs and its relationship with plasmid-encoded genes.
MDRs are posing a treatment challenge, and are emerging as a major cause of morbidity and mortality worldwide. Unfortunately, proper surveillance and documentation of such pathogens is very limited, especially in developing countries. It has been estimated that more than 70% of antibiotic resistance occurs in the Asia-pacific region of the world, making antimicrobial resistance extremely problematic for Asian countries [1]. In Pakistan, ESBLs are especially problematic in terms of their contribution to the MDR bacteria problem. From this perspective, we analysed all of the available data regarding the prevalence of ESBL-producing isolates in different regions of Pakistan.
Antimicrobial resistance is on the rise. There are many factors associated with increasing antimicrobial resistance, one of which is ESBL production. The distribution of ESBLs differs in different communities, and every community must design their own protocol regarding the prevention and treatment of such infections [41]. Developed countries have annual surveillance systems to monitor the impact of antibiotic resistance as well as to determine the causative agents of antibiotic resistant infections. Such surveillance systems are often inadequate in developing countries. This meta-analysis will improve understanding of the distribution and epidemiology of ESBLs with different gene variants in Pakistan. This study also highlights the need to use molecular techniques to determine the different gene variants associated with ESBL-producing bacteria in Pakistan. To our knowledge, this is the first meta-analysis report from Pakistan, which would aid in updating the national treatment guidelines for ESBL infections. The purpose of this study was to determine the pooled prevalence of ESBL-producing Enterobacteriaceae with different gene variants in Pakistan.
Methods
Study design
This is a descriptive, meta-analysis study and is comprised of different studies reported from within Pakistan.
Literature search and strategy
A Web-based search using the key words: ESBLs, Pakistan, ESBL genes and Enterobacteriaceae, were performed using the electronic databases PubMed, Scopus, PakMedi Net and Web of Science in September 2016. Articles published in the English language were included in the study. A comprehensive search was carried out for publications on the subject of ESBLs from Pakistan. Furthermore, the references cited within the articles were also carefully screened to look for additional relevant publications.
Study selection procedures and criteria
Study selection was carried out by three authors in three steps independently (SH, SA and SR). As a first step, all of the titles and abstracts that were related to the study question were reviewed, and these were included in a group of eligible articles with irrelevant articles being excluded. All articles in the initially selected group were further screened in a second step by reviewing the full details of the articles. As a third step, selected articles were evaluated by other authors specifically for meta-analysis (RAK, NA, H H, SR), which was conducted using software STATA version 14.1 (College Station, Texas, USA) as previously described [42].
All studies were included based on the following criteria 1) studies that reported the prevalence of ESBLs in any province of Pakistan; 2) studies on bacterial strains isolated from human specimen; 3) all relevant national and international full text original research articles; 4) studies with confirmed ESBLs using phenotypic detection methods; 5) studies that used molecular techniques for ESBL gene variants.
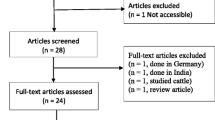
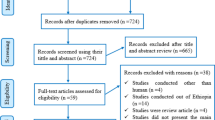
Studies were excluded based on the following criteria 1) studies with incomplete information related to phenotypic ESBL detection methods; 2) duplicate articles, case reports, very small datasets (few strains < 15), abstracts/titles only, posters and review articles 3) studies on β-lactamases other than ESBL; 4) studies on animals and environmental strains of non-human origin. After reading the full texts, 13 further articles were removed for miscellaneous reasons [no phenotypic testing for ESBLs was performed (n = 3), case reports (n = 1), duplicates (n = 2), letter or posters (n = 2), studies about MBLs (n = 2), Studies specific on cancer patients and (mettalo-β-lactamases) MBLs (n = 1) and reviews (n = 2)] (Figs. 1 and 2).
Data extraction
The data were extracted by SH, SA and SR from the eligible studies and included. The data extracted from eligible studies consisted of; year of publication, year in which study was conducted, name of authors, location where the study was conducted (different provinces of Pakistan), sample size, strains detected ESBL, phenotypic detection techniques including; the double disc synergy test (DDST), the combination disc test (CDST), the epsilometric test (E-Test) and molecular detection techniques for gene variants (PCR) (Tables 1 and 2). Data were extracted and analysed twice to remove any discordance.
Statistical analysis and reporting
Statistical analysis was performed using the Metaprop command in STATA version 14.1 (College Station, Texas, USA) to pool the published data regarding the predominance of ESBLs in different regions of Pakistan. Statistical heterogeneity was calculated using the I2 statistic (measure of inconsistency) at the significance level of 5%. Heterogeneity was used to study the variation in studies using the I2 statistic. The p-values (typically considered significant at 0.05) were used for converting meta-analysis results to defined/known tests of statistics. Random-effects model (REM) was used to estimate the pooled prevalence and 95% CI. A funnel plot and Begg tests were performed to evaluate the publication partiality using data graphically and statistically.
Results
Distribution of articles describing ESBLs in Pakistan
Electronic database searches yielded a total of 68 studies. A total of 55 articles reviewed from four provinces of Pakistan included 14 (25.4%) from Punjab, 23 (41.8%) from the Islamabad/Rawalpindi, 9 (16.4%) from the KPK, while the remaining 9 (16.4%) were from the Sindh. No studies were found from Baluchistan province (Fig. 3 and Table 3). The maximum number of articles on this subject was published in year 2013, followed by 2011, with the number of published articles in Pakistan decreasing afterwards (Fig. 4). In total, 42 (76.4%) of the articles reviewed included cases from in-patient and out-patient departments (OPD), 10 (15%) included patients attending in-patient departments, and 3 (6.3%) included patients attending OPD. A total of 21, 232 ESBL-bacterial isolates were included in the analysis. A total of 53 (96.4%) of the reviewed studies were conducted on both adults and children, while only 2 (3.6%) studies were based solely on the paediatric population. No studies were found on male and females separately (Table 2).
Laboratory methods used to estimate the proportion of ESBLs
For the variable phenotype methods, out of 55 studies, 48 (87.3%) had performed the double disc synergism test (DDST). However, only 13 (23.6%) had performed the combination disc test (CDST), and only 5 (9.09%) had performed the epsilometric test (E-Test). None of the studies had used the broth minimum inhibitory concentration (MIC) method. Out of 55 studies, 28 (50.9%) were published in local journals while the remaining 27 (49.1%) were in international journals (Table 2).
Molecular methods used to estimate the proportion of ESBLs
For molecular detection methods, 6 (11%) out of 55 articles reported PCR-based gene detection methods. Among these, 50% of articles reported CTX-M group as the most prevalent group, and CTXM-1 as the most commonly found gene variant. Additionally, CTX-M and TEM combinations were found in 33% of selected articles. One study reported the association of qnrB genes with the appearance of the ESBLs phenotype (Table 1).
Prevalence of ESBLs and their distribution in different geographical areas of Pakistan
Based on the available data (Table 1), Pakistan’s overall pooled proportion of ESBL-production was 0.40 (95% CI: 0.34–0.47). The overall heterogeneity was significant (I2 = 99.75%, p < 0.001), and significant ES = 0 (Z = 18.41, p < 0.001). The pooled proportion of ESBL-production for the Punjab, the Islamabad/Rawalpindi region, the KPK and the Sindh regions was 0.33 (95% CI: 0.21–0.46), 0.50 (95% CI: 0.39–0.62), 0.26 (95% CI: 0.15–0.39) and 0.43 (95% CI: 0.27–0.60) respectively. Significant heterogeneity (I2) for four regions with p < 0.001 is 99.77, 99.46, 99.59 and 99.81% respectively. Significant ES = 0 at p < 0.001 for the Punjab, the Islamabad/Rawalpindi, the KPK and the Sindh regions is Z = 8.32, 12.65, 7.43 and 7.87 respectively (Fig. 2 and Table 2).
Discussion
To address the issue of MDR bacteria, it is necessary to raise awareness about the magnitude of the problem by collecting data about antibiotic-resistance in various countries and regions [1, 29, 43]. The scarcity of studies available from Pakistan warrants attention for future research. Limited data regarding the overall predominance of ESBLs from Pakistan are available, but with no studies specifically from Baluchistan. This is the first meta-analysis about the extent of the ESBL problem in the Pakistani population. This is the first meta-analysis regarding the extent of the ESBL problem in the Pakistani population. However, this meta-analysis finds a high percentage of ESBL-producing Enterobacteriaceae across different geographical regions of Pakistan [5, 7, 12, 20, 44–50].
This meta-analysis is comprised of different studies reported from within Pakistan. The overall pooled proportion for ESBLs in this meta-analysis for Pakistan was 40% (Table 2). In China, a nationwide survey comprised of 30 different hospitals reported a 46% ESBL proportion, which is quite close to the data reported in our study [51]. A survey conducted in the hospitals of East Africa reported an overall pooled ESBL proportion of 42% (95% CI: 0.34–0.50) [52]. Previous research showed a considerably higher frequency of ESBL in Asian and African countries compared to developed countries [53]. For instance, the German population showed the estimated ESBL proportion in the range of 10 to 15% [54]. Similarly, a report was published from the US in 2012, which was based on the surveillance of ESBLs in nine census regions of the US, and they reported 4 to 12% resistance due to ESBLs [55]. However, among the Asian continent, an increase in ESBL mediated resistance was observed among the Japanese community, where the pooled ESBL proportion increased from 6.3% to 20% in 9 years [56].
These results indicate an extensive and statistically significant degree of disparity in ESBL proportion estimates (p < 0.05). The variation in ESBL occurrence reported in this systematic report may depend on several factors, including the socio-economic status of a society and the availability of antibiotics [57]. Moreover, differences in the sensitivity and specificity of the different methods applied in determining the proportions are also contributing factors. The majority of studies used purely phenotypic approaches, while some studies used molecular methods along with phenotypic testing [7, 9, 16, 17, 44, 47, 49, 58, 59]. Differences in ESBL proportions have been documented from all over the world established by hospital or community-based surveys [60–62]. In a study conducted in Ha’Emek Medical Center Israel> 50% ESBL prevalence was reported for community-acquired infections [63]. Whereas studies in Egypt, Cameroon, Bamako, Spain, China, Saudi Arabia, United Kingdom, United States, Latin America between 2004 to 2008 indicated a prevalence of ESBLs between 10 and 61% in different hospital and community settings [63–68].
Due to limited resources and a lack of infrastructure, only a few articles (11%) have investigated the molecular characterization and presence of ESBL encoding genes [4, 7, 16, 24, 29, 44, 45, 50, 51, 58]. OXA, SHV, TEM and CTX-M were the most commonly found gene variants in these studies for ESBLs [7, 16, 17, 50, 69]. The CTX-M group was found to be prevalent in 50% of studies reporting utilization of PCR-based molecular detection methods. The CTXM-15 gene variant of CTX-M group 1 has already been reported in many studies in the Asian continent [70–73]. In particular, CTXM and TEM is a common gene variant combination [7, 50]. One study reported the association of qnrB gene variants with the appearance of an ESBL phenotype, as this gene is involved in fluoroquinolone resistance [17]. However, few studies have reported the incidence of NDM genes, which are responsible for Carbapenem-resistance [52]. There are many reasons for variations in ESBL prevalence in the four studied regions of Pakistan. There may be substrate preferences, higher use of any specific class of antibiotics, co-resistances to other classes of antibiotics, poor health and diagnostic facilities [74, 75]. With this limited available information to hand, it is challenging to plan intensive and effective interventions for combating the problem of resistance.
Conclusion and recommendations
This meta-analysis indicated that there is a high ESBL burden in Pakistan. Few papers are available that address the annual frequency of ESBLs and their distribution in different provinces of Pakistan. No paper is available regarding the frequency of ESBLs in Baluchistan. Only 6 papers that reported gene detection were found. Detection of gene variants in β-lactamase-producing bacteria is essential information for the appropriate and effective treatment of patients. This underscores an urgent demand for regular surveillance to address this antimicrobial resistance issue. National and regional guidelines would be based upon such surveillance in order to understand the annual ESBLs burden. Effective measures such as the establishment of active surveillance and infection control programmes, emphasizing hand hygiene together with coherent antibiotic policies in hospitals and clinics should be implemented to stop and manage the spread of ESBLs in hospitals and communities.
Abbreviations
- CDST:
-
Combination disc test
- DDST:
-
Double disc synergy test
- ESBL:
-
Extended-spectrum β-lactamases
- ESBLs:
-
Extended-spectrum β-lactamase-producing strains
- E-Test:
-
epsilometric test
- KPK:
-
Khyber Pakhtunkhawa
- MBLs:
-
Mettalo-β-lactamases
- MDR:
-
Multidrug-resistant
- MIC:
-
Minimum inhibitory concentration
- OPD:
-
Out-patient department
References
Kang C-I, Song J-H. Antimicrobial resistance in Asia: current epidemiology and clinical implications. Infect Chemother. 2013;45:22–31.
Bhatia R, Narain J-P. The growing challenge of antimicrobial resistance in the South-East Asia region-are we losing the battle? Indian J Med Res. 2010;132:482–6.
Jean SS, Hsueh P-R. High burden of antimicrobial resistance in Asia. Int J Antimicrob Agents. 2011;37:291–5.
Pitout JD. Infections with extended-spectrum β-lactamase-producing Enterobacteriaceae. Drugs. 2010;70:313–33.
Ahmed K, Raja I, Hussain I, Jan M, Nafees M, Jahan Z, Javeed M, Shah G, Latif A. Prevalence of Escherichia coli in suspected urinary tract infected patients and their sensitivity pattern against various Escherichia coli in suspected urinary tract infected patients and their sensitivity pattern against various antibiotics in Gilgit-Baltistan, Pakistan. Pak J Zool. 2014;46:1783–8.
Hafeez R, Aslam M, Mir F, Tahir M, Javaid I, Ajmal A. Frequency of extended spectrum β-lactamase producing gram negative bacilli among clinical isolates. Biomedica. 2009;25:112–5.
Riaz S, Bashir MF. Phenotypic and molecular characterization of plasmid-encoded extended spectrum β-lactamases produced by Escherichia coli and Klebsiella Spp from Lahore, Pakistan. Trop J Pharmaceut Res. 2015;14:1597–604.
Riaz S, Faisal M, Hasnain S. Antibiotic susceptibility pattern and multiple-antibiotic-resistances (MAR) calculation of extended spectrum β-lactamase (ESBL) producing Escherichia coli and Klebsiella species in Pakistan. Afri J Biotechnol. 2011;10:6325–31.
Ejaz H, ul-Haq I, Saqib Mahmood S, Zafar A, Javed M-M. Detection of extended-spectrum β-lactamases in Klebsiella pneumoniae: comparison of phenotypic characterization methods. Pak J Med Sci. 2013;29:788–94.
Amin H, Zafar A, Ejaz H, Jameel N-A. Phenotypic characterization of ESBL-producing Enterobacter Cloacae among children. Pak J Med Sci. 2013;29:144–7.
Ejaz H, ul-Haq K, Zafa A, Mahmood S, Javed M-M. Urinary tract infections caused by extended spectrum β-lactamase (ESBL) producing Escherichia coli and Klebsiella pneumoniae. Afric J Biotechnol. 2011;10:16661–6.
Anwar M. Frequency of extended spectrum β-lactamase producing Klebsiella pnumoniae and Escherichia coli isolates. Biomedica. 2007;23:34–8.
Qureshi M, Asif N, Baig S. Evaluation of extended spectrum β-lactamase mediated resistance in Escherichia coli and Klebsiella in urinary tract infection at a tertiary care hospital. Biomedica. 2013;29:78–83.
Khan J, Naz N, AbdEl-Salam N-M, Nayab Nayab N, Tabassum A, Hussain H, Ullah R. ESBL determination and antibacterial drug resistance pattern of Klebsiella pneumoniae amongst patients at PIMS Islamabad. Afric J Tradit Complement Alternv Med. 2015;12:70–7.
Amin A, Ghumro P-B, Hussain S, Hameed A. Prevalence of antibiotic resistance among clinical isolates of Klebsiella pneumoniae isolated from a tertiary care hospital in Pakistan. Malays J Microbiol. 2009;5:81–6.
Habeeb M-A, Sarwar Y, Ali A, Salman M, Haque A. High prevalence of 16S rRNA methylase Rmtb among CTX-M extended-spectrum β-lactamase-producing Klebsiella pneumoniae from Islamabad, Pakistan. Int J Antimicrob Agents. 2013;41:524–6.
Ali I, Rafaque Z, Ahmed S, Malik S, Dasti J-I. Prevalence of multidrug-resistant uropathogenic Escherichia coli in Potohar region of Pakistan. Asian Pac J Trop Biomed. 2016;6:60–6.
Shafiq M, Rahman H, Qasim M, Ayub N, Hussain S, Khan J, Naeem M. Prevalence of plasmid-mediated Ampc β-Lactamases in Escherichia coli and Klebsiella pneumoniae at tertiary care hospital of Islamabad, Pakistan. Eur J Microbiol Immunol. 2013;3:267–71.
Ilyas M, Shabeer Ahmad MK, Mazhar K, Sajid A. Susceptibility pattern of extended spectrum β-lactamases positive Escherichia coli isolated from a tertiary care hospital of Peshawar, Pakistan. World Appl Sci J. 2014;30:253–7.
Ullah F, Malik S-A, Ahmed J. Antimicrobial susceptibility pattern and ESBL prevalence in Klebsiella pneumoniae from urinary tract infections in the north-west of Pakistan. Afr J Microbiol Res. 2009;3:676–80.
Bari F, Shah H, Wazir R. Frequency and detection of extended spectrum-β-lactamase in Escherichia coli and Klebsiella pneumoniae: a study at lady reading hospital Peshawar. J Postgrad Med Inst. 2015;29:256–9.
Riaz S, Faisal M, Hasnain S. Prevalence and comparison of β-lactamase-producing Escherichia coli and Klebsiella Spp from clinical and environmental sources in Lahore, Pakistan. Afr J Microbiol Res. 2012;6:465–70.
Ndir A, Diop A, Ka R, Faye PM, Dia-Badiane NM, Ndoye B, Astagneau P. Infections caused by extended-spectrum β-lactamases producing Enterobacteriaceae: clinical and economic impact in patients hospitalized in 2 teaching hospitals in Dakar, Senegal. Antimicrob Resis Infect Control. 2016;5:13–20.
Slama TG. Gram-negative antibiotic resistance: there as a price to pay. Crit Care. 2008;12:S4.
Xiao Y-H, Giske CG, Wei Z-Q, Shen P, Heddini A, Li L-J. Epidemiology and characteristics of antimicrobial resistance in China. Drug Resist Updat. 2011;14:236–50.
Falagas ME, Maraki S, Karageorgopoulos DE, Kastoris AC, Mavromanolakis E, Samonis G. Antimicrobial susceptibility of multidrug-resistant (MDR) and extensively drug-resistant (XDR) Enterobacteriaceae isolates to fosfomycin. Int J Antimicrob Agents. 2010;35:240–3.
Savard P, Perl TM. A call for action: managing the emergence of multidrug-resistant Enterobacteriaceae in the acute care settings. Curr Opin Infect Dis. 2012;25:371–7.
Hoban DJ, Bouchillon SK, Hawser SP, Badal RE. Trends in the frequency of multiple drug-resistant Enterobacteriaceae and their susceptibility to ertapenem, imipenem, and other antimicrobial agents: data from the study for monitoring antimicrobial resistance trends 2002 to 2007. Diagn Microbiol Infect Dis. 2010;66:78–86.
Kelesidis T, Karageorgopoulos DE, Kelesidis I, Falagas ME. Tigecycline for the treatment of multidrug-resistant Enterobacteriaceae: a systematic review of the evidence from microbiological and clinical studies. J Antimicrob Chemother. 2008;62:895–904.
Casella T, Rodríguez MM, Takahashi JT, Ghiglione B, Dropa M, Assunção E, Nogueira ML, Lincopan N, Gutkind G, Nogueira MCL. Detection of Bla CTX-M-type genes in complex class 1 integrons carried by Enterobacteriaceae isolated from retail chicken meat in Brazil. Int J Food Microbiol. 2015;197:88–91.
Chen I-L, Lee C-H, Su L-H, Tang Y-F, Chang S-J, Liu J-W. Antibiotic consumption and healthcare-associated infections caused by multidrug-resistant gram-negative bacilli at a large medical center in Taiwan from 2002 to 2009: implicating the importance of antibiotic stewardship. PLoS One. 2013;8:E65621.
Falagas ME, Kastoris AC, Kapaskelis AM, Karageorgopoulos DE. Fosfomycin for the treatment of multidrug-resistant, including extended-spectrum β-lactamase producing, Enterobacteriaceae infections: a systematic review. Lancet Infect Dis. 2010;10:43–50.
Coates AR, Halls G, Hu Y. Novel classes of antibiotics or more of the same? Br J Pharmacol. 2011;163:184–94.
Kucheria R, Dasgupta P, Sacks S, Khan M, Sheerin N. Urinary tract infections: new insights into a common problem. Postgrad Med J. 2005;81:83–6.
David MZ, Daum RS. Community-associated methicillin-resistant Staphylococcus aureus: epidemiology and clinical consequences of an emerging epidemic. Clin Microbiol Rev. 2010;23:616–87.
Kurutepe S, Surucuoglu S, Sezgin C, Gazi H, Gulay M, Ozbakkaloglu B. Increasing antimicrobial resistance in Escherichia coli isolates from community-acquired urinary tract infections during 1998-2003 in Manisa, Turkey. Jpn J Infect Dis. 2005;58:159–62.
Song J-H, Jung S-I, Ko KS, Kim NY, Son JS, Chang H-H, Ki HK, Oh WS, Suh JY, Peck KR. High prevalence of antimicrobial resistance among clinical Streptococcus pneumoniae isolates in Asia (an ANSORP study). Antimicrob Agents Chemother. 2004;48:2101–7.
Hsueh P-R, Hoban DJ, Carmeli Y, Chen S-Y, Desikan S, Alejandria M, Ko W-C, Binh TQ. Consensus review of the epidemiology and appropriate antimicrobial therapy of complicated urinary tract infections in asia-pacific region. J Inf Secur. 2011;63:114–23.
Sunenshine RH, Wright M-O, Maragakis LL, Harris AD, Song X, Hebden J, Cosgrove SE, Anderson A, Carnell J, Jernigan DB. Multidrug-resistant Acinetobacter infection mortality rate and length of hospitalization. Emerg Infect Dis. 2007;13:97–103.
Yasmin F, Akhtar N, Hameed A. In-vitro synergistic effect of ciprofloxacin with aminoglycosides against multidrug resistant-Pseudomonas aeruginosa. Pak J Pharm Sci. 2013;26:1041–4.
Okeke IN, Lamikanra A. Export of antimicrobial drugs by west African travelers. J Travel Med. 2003;10:133–5.
Nyaga VN, Arbyn M, Aerts M. Metaprop : a Stata command to perform meta-analysis of binomial data. Arch Public Health. 2014;72:1–10.
Kumar SG, Adithan C, Harish B, Sujatha S, Roy G, Malini A. Antimicrobial resistance in India: a review. J Nat Sc Biol Med. 2013;4:286–91.
Hannan A, Qamar MU, Usman M, Waheed KAI, Rauf K. Multidrug resistant microorganisms causing neonatal septicemia: in a tertiary care hospital Lahore, Pakistan. Afr J Microbiol Res. 2013;7:1896–902.
Hussain M, Hasan F, Shah AA, Hameed A, Jung M, Rayamajhi N, Cha S-B, Yoo HS. Prevalence of class a and Ampc β-Lactamases in clinical Escherichia coli isolates from Pakistan Institute of Medical Science, Islamabad, Pakistan. Jpn J Infect Dis. 2011;64:249–52.
Kausar A, Akram M, Shoaib M, Mehmood RT, Abbasi MN, Muhammad A, Aziz H, Asad MJ. Isolation and identification of UTI causing agents and frequency of ESBL (extended Spectrum β-Lactamase) in Pakistan. Amer JPhytomed Clin Ther. 2014;2:963–75.
Ali A, Rafi S, Qureshi A. Frequency of extended spectrum β-lactamase producing gram negative bacilli among clinical isolates at clinical laboratories of Army medical college, Rawalpindi. PRO. 2004;2:25–9.
Begum S, Hasan F, Hussain S, Shah AA. Prevalence of multidrug-resistant Acinetobacter Baumannii in the clinical samples from tertiary care hospital in Islamabad, Pakistan. Pak J Med Sci. 2013;29:1253–8.
Ullah F, Malik SA, Ahmed J. Antibiotic susceptibility pattern and ESBL prevalence in nosocomial Escherichia coli from urinary tract infections in Pakistan. Afric J Biotechnol. 2009;8:3921–6.
Rahman H, Naeem M, Khan I, Khan J, Haroon M, Bari F, Ullah R, Qasim M. Molecular prevalence and antibiotics resistance pattern of class a bla CTX-M-1 and bla TEM-1 β- Lactamases in uropathogenic Escherichia coli isolates from Pakistan. Turk J Med Sci. 2016;46:897–902.
Zhang J, Zheng B, Zhao L, Wei Z, Ji J, Li L, Xiao Y. Nationwide high prevalence of CTX-M and an increase of CTX-M-55 in Escherichia coli isolated from patients with community-onset infections in Chinese county hospitals. BMC Infect Dis. 2014;14:659–63.
Sonda T, Kumburu H, van Zwetselaar M, Alifrangis M, Lund O, Kibiki G, Aarestrup FM. Meta-analysis of proportion estimates of extended-spectrum-β-lactamase-producing Enterobacteriaceae in East Africa hospitals. Antimicrob Resis Infect Control. 2016;5:18–26.
Livermore DM. Current epidemiology and growing resistance of gram-negative pathogens. Korean J Intern Med. 2012;27:128–42.
Leistner R, Schröder C, Geffers C, Breier A-C, Gastmeier P, Behnke M. Regional distribution of nosocomial infections due to ESBL-positive Enterobacteriaceae in Germany: data from the German national reference center for the surveillance of nosocomial infections (KISS). Clin Microbiol Infect. 2015;21:255.
Flamm RK, Sader HS, Farrell DJ, Jones RN. Ceftaroline potency among 9 US census regions: report from the 2010 AWARE program. Clin Infect Dis. 2012;55:S194–205.
Castanheira M, Farrell SE, Krause KM, Jones RN, Sader HS. Contemporary diversityof β-Lactamases among Enterobacteriaceae in the nine United States census regions and ceftazidime-avibactam activity tested against isolates producing the most prevalent β-lactamase groups. Antimicrob Agents Chemother. 2014;58:833-838.
Spanu T, Luzzaro F, Perilli M, Amicosante G, Toniolo A, Fadda G, Group IES. Occurrence of extended-Spectrum β-Lactamases in members of the family Enterobacteriaceae in Italy: implications for resistance to β-lactams and other antimicrobial drugs. Antimicrob Agents Chemother. 2002;46:196–202.
Mahmood K, Izhar M, Choudhry N, Mujtaba G, Rashid N. Emergence of extended-spectrum-lactamase producing Salmonella Typhi in Pakistan. Afric J Microbiol Res. 2012;6:793–7.
Ahmad M, Hassan M, Khalid A, Tariq I, Asad MHHB, Samad A, Mahmood Q, Murtaza G. Prevalence of extended spectrum β-lactamase and antimicrobial susceptibility pattern of clinical isolates of Pseudomonas from patients of Khyber Pakhtunkhwa, Pakistan. Biomed Res Int. 2016:2016–26.
Lonchel CM, Meex C, Gangoué-Piéboji J, Boreux R, Assoumou M-CO, Melin P, De Mol P. Proportion of extended-spectrum ß-lactamase-producing Enterobacteriaceae in community setting in Ngaoundere, Cameroon. BMC Infect Dis. 2012;12:53–9.
Bourjilat F, Bouchrif B, Dersi N, Claude JDPG, Amarouch H, Timinouni M. Emergence of extended-spectrum beta-lactamases-producing Escherichia coli in community-acquired urinary infections in Casablanca, Morocco. J Infect Dev Ctries. 2011;5:850–5.
Muvunyi CM, Masaisa F, Bayingana C, Mutesa L, Musemakweri A, Muhirwa G. Decreased susceptibility to commonly used antimicrobial agents in bacterial pathogens isolated from urinary tract infections in Rwanda: need for new antimicrobial guidelines. Am J Trop Med Hyg. 2011;84:923–8.
Colodner R, Rock W, Chazan B, Keller N, Guy N, Sakran W, Raz R. Risk factors for the development of extended-spectrum β-lactamase-producing bacteria in non-hospitalized patients. Euro J Clin Microbiol Infect Dis. 2004;23:163–7.
Tandé D, Jallot N, Bougoudogo F, Montagnon T, Gouriou S, Sizun J. Extended-spectrum β-lactamase–producing Enterobacteriaceae in a Malian orphanage. Emerg Infect Dis. 2009;15:472–4.
Valverde A, Coque TM, Sánchez-Moreno MP, Rollán A, Baquero F, Cantón R. Dramatic increase in prevalence of fecal carriage of extended-spectrum β-lactamase-producing Enterobacteriaceae during non-outbreak situations in Spain. J Clin Microbiol. 2004;42:4769–75.
Ho P, Poon WW, Loke S, Leung MS, Chow K, Wong RC, Yip K, Lai EL, Tsang KW. Community emergence of CTX-M type extended-spectrum β-lactamases among urinary Escherichia coli from women. J Antimicrob Chemother. 2007;60:140–4.
Rodríguez-Bano J, Navarro MD, Romero L, Martínez-Martínez L, Muniain MA, Perea EJ, Pérez-Cano R. Epidemiology and clinical features of infections caused by extended-spectrum β-lactamase-producing Escherichia coli in non-hospitalized patients. J Clin Microbiol. 2004;42:1089–94.
Kader A, Kamath K. Faecal carriage of extended-spectrum beta-lactamase-producing bacteria in the community. East Mediterr Health J. 2009;15:1365–70.
Day KM, Ali S, Mirza IA, Sidjabat HE, Silvey A, Lanyon CV, Cummings SP, Abbasi SA, Raza MW, Paterson DL. Prevalence and molecular characterization of Enterobacteriaceae producing NDM-1 carbapenemase at a military hospital in Pakistan and evaluation of two chromogenic media. Diagnostic Microbiol Infect Dis. 2013;75:187–91.
Sheng W-H, Badal RE, Hseuh P-R. Distribution of extended-spectrum β-lactamases (ESBLs), Ampc β-lactamases, and carbapenemases among Enterobacteriaceae isolates causing intra-abdominal infections in Asia-Pacific: the study for monitoring antimicrobial resistance trends (SMART). Antimicrob Agents Chemother. 2013;57:2981-2988.
Lahlaoui H, Khalifa ABH, Moussa MB. Epidemiology of Enterobacteriaceae producing CTX-M type extended spectrum β-lactamase (ESBL). Mede Malad Infect. 2014;44:400–4.
Altinkum SM, Ergin S, Bahar H, Torun MM. CTX-M-15 type extended spectrum-lactamase producing Escherichia coli and Klebsiella pneumoniae: a developing problem in infected outpatients and hospitalised patients in Istanbul, Turkey. African J Microbiol Res. 2013;7:692–7.
Chandramohan L, Revell PA. Prevalence and molecular characterization of extended-spectrum-β-lactamase-producing Enterobacteriaceae in a pediatric patient population. Antimicrob Agents Chemother. 2012;56:4765–70.
Winokur P, Canton R, Casellas J-M, Legakis N. Variations in the prevalence of strains expressing an extended-spectrum β-lactamase phenotype and characterization of isolates from Europe, the Americas, and the western Pacific region. Clin Infect Dis. 2001;32:94–103.
Winokur P, Canton R, Casellas J-M, Legakis N. Regional variation in the prevalence of extended-spectrum β-lactamase–producing clinical isolates in the Asia-Pacific region (SENTRY 1998–2002). Diag Microbiol Infect Dis. 2005;52:323–9.
Shah S. Susceptibility patterns of Escherichia coli: prevalence of multidrug-resistant isolates and extended spectrum β-lactamase phenotype. J Pak Med Assoc. 2002;52:132–8.
Shah AA, Hasan F, Ahmed S, Hameed A. Prevalence of extended-spectrum β-lactamases in nosocomial and out-patients (ambulatory). Pak J Med Sci. 2003;19:187–91.
Mumtaz S, Ahmad M, Aftab I, Akhtar N, Hassan M, Hamid A. Extended spectrum β-lactamases in enteric gram-negative bacilli: related to age and gender. J Ayub Med Coll Abbott. 2007;19:107–11.
Khan E, Schneiders T, Zafar A, Aziz E, Parekh A, Hasan R. Emergence of CTX-M group 1-ESBL producing Klebsiella pneumonia from a tertiary care centre in Karachi, Pakistan. J Infect Dev Countr. 2010;4:472–6.
Roshan M, Ikram A, Mirza IA, Malik N, Abbasi SA, Alizai SA. Susceptibility pattern of extended spectrum ß-lactamase producing isolates in various clinical specimens. J Coll Physicians Surg Pak. 2011;21:342–6.
Hassan A, Usman J, Kaleem F, Omair M, Khalid A, Iqbal M. Frequency and antibiotic susceptibility pattern of amp C β-lactamase producing bacteria isolated from a tertiary care hospital of Rawalpindi, Pakistan. Pak J Med Sci. 2011;27:578–81.
Habeeb MA, Haque A, Nematzadeh S, Iversen A, Giske CG. Rapid emergence of ESBL producers in E. coli causing urinary and wound infections in Pakistan. Pak J Med Sci. 2013;29:540–4.
Khalid A, Usman J, Kaleem F, Hassan A, Omair M, Anjum R. The frequency and antimicrobial sensitivity pattern of extended spectrum-lactamase (ESBLs) producing gram negative bacilli isolated from urine in a tertiary care hospital of Pakistan. Afric J Microbiol Res. 2013;7:2040–3.
Sabir S, Anjum AA, Ijaz T, Ali MA, Rehman MU, Nawaz M. Isolation and antibiotic susceptibility of E. coli from urinary tract infections in a tertiary care hospital. Pak J Med Sci. 2014;30:389–92.
Saboor MAM, Waheed U, Anwarullah, Umar M. Prevalence of ESBL producing Enterobacteriaceae in a private hospital in Islamabad. Int J Rehab Sci. 2014;3:18–22.
Sohail M, Khurshid M, Saleem HGM, Javed H, Khan AA. Characteristics and antibiotic resistance of urinary tract pathogens isolated from Punjab, Pakistan. Jundishapur J Microbiol. 2015;8:e19272.
Ahmed I, Sajed M, Sultan A, Murtaza I, Yousaf S, Maqsood B, Vanhara P, Anees M. The erratic antibiotic susceptibility patterns of bacterial pathogens causing urinary tract infections. EXCLI J. 2015;14:916.
Jamil B, Bokhari MTM, Saeed A, Bokhari MZM, Hussain Z, Khalid T, Bukhari H, Imran M, Abbasi SA. Bacteremia: prevalence and antimicrobial resistance profiling in chronic kidney diseases and renal transplant patients. J Pak Med Assoc. 2016;66:705.
Anwar M, Ejaz H, Zafar A, Hamid H. Phenotypic detection of metallo-β-lactamases in carbapenem resistant Acinetobacter baumannii isolated from pediatric patients in Pakistan. J Pathog. 2016;2016:1–6.
Mumtaz S, Ahmed J, Ali L, Hussain H. Prevalence of extended spectrum β-lactamases (ESBL) in clinical isolates from a teaching hospital in Peshawar, Pakistan. Afric J Microbiol Res. 2011;5:2880–4.
Iqbal R, Majid A, Alvi IA, Hayat A, Andaleeb F, Gul S, Irfan S, Rahman MU. Multiple drug resistance and ESBL production in bacterial urine culture isolates. Amer J Biosci. 2014;2:5–12.
Jabeen K, Zafar A, Hasan R. Comparison of double disc and combined disc method for the detection of extended spectrum ß-lactamases in Enterobacteriaceae. J Pak Med Asso. 2003;53:534–7.
Jabeen K, Znfar A, Hasan R. Frequency and sensitivity pattern of extended spectrum β-lactamase producing isolates in a tertiary care hospital laboratory of Pakistan. J Pak Med Assoc. 2005;55:436.
Ahmed E, Durrani M, Qamar S, Kharal S. Detection of extended spectrum β-lactamase (ESBL) producing organisms in Enterobacteriaceae Family like Escherichia coli (E. coli) and Klebsiella pneumoniae by double disc diffusion method (DDDM). Pak J Pharmacol. 2009;26:25–30.
Jabeen K, Zafar A, Irfan S, Khan E, Mehraj V, Hasan R. Increase in isolation of extended spectrum beta lactamase producing multidrug resistant non typhoidal Salmonellae in Pakistan. BMC Infect Dis. 2010;10:101–6.
Khan E, Ejaz M, Zafar A, Jabeen K, Shakoor S, Inayat R, Hasan R. Increased isolation of ESBL producing Klebsiella pneumoniae with emergence of carbapenem resistant isolates in Pakistan: report from a tertiary care hospital. J Pak Med Assoc. 2010;60:186–9.
Afridi, F.I., B.J. Farooqi, And A. Hussain, Frequency of extended spectrum beta lactamase producing Enterobacteriaceae among urinary pathogen isolates. J Coll Physicians Surg Pak. 2011;21:741-744.
Hassan SA, Jamal SA, Kamal M. Occurrence of multidrug resistant and ESBL producing E. coli causing urinary tract infections. J Basic Appl Sci. 2011;7:39–43.
Afridi FI, Farooqi BJ. Activity of β-lactam β-lactamase inhibitor combinations against extended spectrum β-lactamase producing Enterobacteriaceae in urinary isolates. J Coll Physicians Surg Pak. 2012;22:358–62.
Ullah F, Malik SA, Ahmed J. Antimicrobial susceptibility and ESBL prevalence in Pseudomonas aeruginosa isolated from burn patients in the north-west of Pakistan. Burns. 2009;35:1020–5.
Mirza SH, Salman M, Khurshid U, Wiqar MA. CTX-M ESBL enzyme in Escherichia coli from urology patients in Rawalpindi, Pakistan. J Pak Med Assoc. 2006;56:576–80.
Acknowledgments
We would like to acknowledge the staff of Citilab and Research center Lahore and Department of Statistical and Actual Sciences, University of the Punjab, Lahore, for providing unconditional support for completion of this work.
Funding
No funding was received for this study.
Availability of data and materials
The data sets analyzed during the current study are available from the corresponding author.
Declaration
This study is part of Ph. D thesis of Samyyia Abrar.
Author information
Authors and Affiliations
Contributions
SR is the supervisor and conceived the idea; SH gathered data, analysed data and contributed to draft preparation; SA rechecked the data, contributed to data analysis and contributed to draft preparation; NA and MH analysed data and contributed to draft preparation; RA worked on statistical analysis; all authors read, revised and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by local ethics committee (CitiLab and Research Centre Ref # 27th − 17 CLRC/ 27th).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Abrar, S., Hussain, S., Khan, R.A. et al. Prevalence of extended-spectrum-β-lactamase-producing Enterobacteriaceae: first systematic meta-analysis report from Pakistan. Antimicrob Resist Infect Control 7, 26 (2018). https://doi.org/10.1186/s13756-018-0309-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13756-018-0309-1