Abstract
Aims
Mobile Airways Sentinel NetworK (MASK) belongs to the Fondation Partenariale MACVIA-LR of Montpellier, France and aims to provide an active and healthy life to rhinitis sufferers and to those with asthma multimorbidity across the life cycle, whatever their gender or socio-economic status, in order to reduce health and social inequities incurred by the disease and to improve the digital transformation of health and care. The ultimate goal is to change the management strategy in chronic diseases.
Methods
MASK implements ICT technologies for individualized and predictive medicine to develop novel care pathways by a multi-disciplinary group centred around the patients.
Stakeholders
Include patients, health care professionals (pharmacists and physicians), authorities, patient’s associations, private and public sectors.
Results
MASK is deployed in 23 countries and 17 languages. 26,000 users have registered.
EU grants (2018)
MASK is participating in EU projects (POLLAR: impact of air POLLution in Asthma and Rhinitis, EIT Health, DigitalHealthEurope, Euriphi and Vigour).
Lessons learnt
(i) Adherence to treatment is the major problem of allergic disease, (ii) Self-management strategies should be considerably expanded (behavioural), (iii) Change management is essential in allergic diseases, (iv) Education strategies should be reconsidered using a patient-centred approach and (v) Lessons learnt for allergic diseases can be expanded to chronic diseases.
Similar content being viewed by others
Introduction
In all societies, the burden and cost of allergic and chronic respiratory diseases (CRDs) is increasing rapidly. Most economies are struggling to deliver modern health care effectively. There is a need to support the transformation of the health care system for integrated care with organizational health literacy. MASK (Mobile Airways Sentinel Network) [1] is a new development of the ARIA (Allergic Rhinitis and its Impact on Asthma) initiative [2, 3]. It works closely with POLLAR (Impact of Air POLLution on Asthma and Rhinitis, EIT Health) [4], and collaborates with professional and patient organizations in the field of allergy and airway diseases. MASK proposes real-life care pathways (ICPs) centred around the patient with rhinitis and/or asthma multimorbidity. It uses mHealth monitoring of environmental exposure and considers biodiversity. With the help of three EU projects (DigitalHealthEurope, Eurifi and Vigour) recently accepted on the digital transformation of health, MASK proposes a second change management strategy. The first one was the ARIA change management associated with the recognition and wide acceptance by all stakeholders of the essential links between rhinitis and asthma. The second one deals with change management of care pathways for rhinitis and asthma [5].
In the context of implementing communication on the digital transformation of health and care, specifically in relation to chapter 5 of the document “Digital tools for citizen empowerment and for person-centred care”, DG SANTE has taken steps towards supporting the scaling-up and wider implementation of good practices in the field of digitally-enabled, integrated, person-centred care. This work was carried out in collaboration with the newly-established Commission Expert Group, the “Steering Group on Health Promotion, Disease Prevention and Management of Non-Communicable Diseases”.
For this purpose, DG SANTE—in collaboration with the Commission’s Joint Research Centre—organized a “marketplace” workshop with the Joint Research Centre in Ispra, the third biggest European Commission site after Brussels and Luxembourg. The aim of this workshop was for representatives from Member States and other countries participating in the 3rd Health Programme to learn more about the 10 good practices and key policy initiatives in the domain of digitally-enabled, integrated, person-centred care, with a view to possible transfer and replication of the presented practices.
The current paper reviews the questions raised during the workshop concerning the good practice on allergic rhinitis and asthma: ARIA digitally-enabled, integrated, person-centred care for rhinitis and asthma multimorbidity using real-world evidence [1]. This practice is a GARD (Global Alliance against Chronic Respiratory Diseases) demonstration project.
The practice
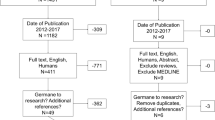
The practice includes the care pathways defined in 2014 [6,7,8] (Fig. 1) as well as ICT (Information and Communication Technology) solutions (cell phones for patients, inter-operable tablets for health care professionals and a web-based questionnaire for physicians) [1, 9] (Fig. 2). The aim is to develop a change management strategy for chronic diseases [5].
MASK is a patient-centred ICT system [8]. A mobile phone app (the Allergy Diary, now called MASK-air), central to MASK, is available in 23 countries. It has been validated [10] and found to be an easy and effective method of assessing the symptoms of allergic rhinitis (AR) and work productivity [10,11,12,13]. MASK follows the checklist for the evaluation of Good Practices developed by the European Union Joint Action JA-CHRODIS (Joint Action on Chronic Diseases and Promoting Healthy Ageing across the Life Cycle) [14]. One of the major aims of MASK is to provide care pathways [15] in rhinitis and asthma multimorbidity [16] including a sentinel network using the geolocation of users [17]. It can also inform the App users of the pollen and/or pollution risk level in their area, by means of geolocation (Table 1).
The practice has been developed for allergic rhinitis (and asthma multimorbidity), being the most common chronic disease globally [18, 19] and affecting all age groups from early childhood to old age. There are several unmet needs that should be addressed in an ICP. Moreover, the lessons learnt will benefit all chronic diseases since rhinitis is considered as a mild disease although it impairs social life, school and work productivity considerably [20]. It is estimated that, in the EU, work loss accounts for 30–100 b€ annually. Moreover, it is essential to consider mild chronic diseases and to establish health promotion and management strategies early in life in order to prevent a severe outcome and to promote healthy ageing [21].
Level of care integration
MASK is used for the integration of primary and specialist care, of primary-secondary-tertiary health care, as well as of health and social care for disease management.
Deployment
Many of the GPs that are developed in one region (country) take into account health systems, availability of treatments and legal considerations which makes it difficult to scale up the practice without customization. MASK has taken the opposite direction starting with a tool immediately available in 10 languages and 14 countries and regularly scaled up. Moreover, the tool is included in a generic ICP (Fig. 2) that can be customized easily in any country globally.
Geographical scope of the practice
MASK was developed in English and is currently available in 23 countries and 17 languages (Table 2).
New countries
Deployment is in process in Bolivia, Colombia, Japan and Peru. The involvement of developing countries is needed to offer a practice for middle- and low-income countries that will benefit poverty areas of developed countries and that will be in line with the mission of GARD. Deployment to the US is being discussed with the National Institute for Allergy and Infectious diseases (NIH).
Transfer of innovation of allergic rhinitis and asthma multimorbidity in the elderly (MASK Reference Site Twinning, EIP on AHA)
The EIP on AHA includes 74 Reference Sites. The aim of this TWINNING is to transfer innovation from the MASK App to other reference sites. The phenotypic characteristics of rhinitis and asthma multimorbidity in adults and the elderly have been compared using validated mHealth tools (i.e. the Allergy Diary and CARAT [22]) in 23 Reference Sites or regions across Europe, Argentina, Australia, Brazil and Mexico [23].
Individuals/institutions reached
ARIA has been implemented in over 70 countries globally [3], and several governments use the practice. Approximately 26,000 users have registered to the MASK database. 700 patients have been enrolled in the Twinning. Due to privacy, there is no possibility of assessing users who have reported data.
Timeframe
The project was initiated in 1999 during a World Health Organization (WHO) workshop (ARIA) and undergoes continuous developments. The ARIA initiative, commenced during a WHO workshop in 1999 [2], has been further developed by the WHO Collaborating Center for Asthma and Rhinitis (2002–2013). The initial goals (Phase 1) were (1) to propose a new AR classification, (2) to promote the concept of multimorbidity in asthma and rhinitis and (3) to develop guidelines with all stakeholders that could be used globally for all countries and all populations. ARIA has been disseminated and implemented in over 70 countries [3, 19, 24,25,26,27,28,29,30,31,32]. It was developed as a guideline [19] using the GRADE approach [33,34,35,36,37,38,39].
MASK, the Phase 3 ARIA initiative, is focusing on (1) the implementation of multi-sectoral care pathways (2) using emerging technologies (3) with real world data (4) for individualized and predictive medicine (5) in rhinitis and asthma multimorbidity (6) by a multi-disciplinary group or by patients themselves (self-care) using the AIRWAYS ICPs algorithm (7) across the life cycle [8, 17]. It will be scaled up using the EU EIP on AHA strategy [26].
Phase 4 began in 2018. It concerns “change management” and includes the impact of air pollution in asthma and rhinitis (EIT Health 2018–2019: POLLAR, Impact of Air POLLution in Asthma and Rhinitis) [4] as well as the digital transformation of health and care (DigitalHealthEurope, Euriphi and Vigour).
Developments for 2019 include a multimorbidity App and the deployment of an app for home services.
The MASK project is intended to be sustainable and a business plan has been initiated.
The medium-term future is to develop care pathways for the prevention and control of chronic diseases to sustain planetary health. A symposium during the Finnish Presidency of the EU Council is planned for October 2019.
Scientific evidence and conceptual framework for configuring the practice
The scientific evidence is based on a validated “research” tool (The Allergy Diary, –2018) that has led to large scale deployment (MASK-air, 2019–):
-
Validation of the app using COSMIN guidelines [40].
-
Baseline characteristics informed [12].
-
Work productivity associated with the control of allergic diseases [41, 42].
-
EQ-5D is available and has been found to correlate to baseline characteristics [43].
-
Novel phenotypes of allergic diseases have been discovered [44].
-
Adherence to treatment is extremely low and novel approaches to inform the efficacy of treatment have been proposed [45] leading to novel studies for a better understanding of guidelines [46, 47].
Evidence of impact
MASK has identified novel phenotypes of allergic diseases [44] that have been confirmed in classical epidemiologic studies by re-analyzing them [48,49,50,51]. One of the studies used the MASK baseline characteristics [49]. These phenotypes allowed the re-classification of allergic multimorbidity and the discovery of a new extreme phenotype of allergic diseases that need to be considered in the stratification of patients.
MASK has shown real-life mHealth data for the first time in allergy treatment in 9,950 users [1, 45]. This led to next-generation care pathways for allergic diseases (meeting co-organized by POLLAR, a member of EIT Health, EIP on AHA and GARD (WHO alliance): 3-12-2018) and proposed a change management strategy [5].
MASK is involved in an EIT Health project (POLLAR) which assesses the interactions between air pollution, asthma and rhinitis [4].
With the EIP on AHA, MASK is involved in 3 EU projects on the digital transformation of health and care (DigiHealthEurope, Euriphi and Vigour).
MASK is also involved in a large project on Planetary Health in a side event which will take place during the Presidency of the EU council (Finland). This event will gather researchers, academic leaders and other experts from European institutions as well as other stakeholders and will discuss Planetary Health global challenges and their scientific solutions. Experts on human health as well as on effects of climate change, urbanization and food production will be invited to prepare a European initiative to promote effective and sustainable research on planetary health issues. The event similarly aims at raising political awareness about the need for multidisciplinary and systemic approaches to Planetary Health issues globally and in the EU. The multimorbid App developed by MASK may be used in the project.
Contextual relevance
The practice addresses a public health priority
Chronic respiratory diseases (CRDs) are major non-communicable diseases (NCDs) [18]. Rhinitis and asthma multimorbidity is common and the two diseases should be considered jointly [19]. Asthma is the most common NCD in children and rhinitis is the most common chronic disease in Europe. They often start early in life, persist across the life cycle and cause a high disease burden in all age groups [19]. By 2020, rhinitis will affect at least 20% of the old age population [52,53,54,55,56]. These diseases represent an enormous burden associated to medical and social costs and they impact health and social inequalities.
The practice is based on a local/regional/national strategic action plan
The Polish Presidency of the EU Council (3051st Council Conclusions) made the prevention, early diagnosis and treatment of asthma and allergic diseases a priority to reduce health inequalities [57, 58]. The 3206th Cyprus Council Conclusions [59] recommended that the diagnosis and treatment of chronic diseases should be initiated as early as possible to improve AHA. Debates at the European Parliament recommended the early diagnosis and management of CRDs in order to promote active and healthy ageing (AHA) [60,61,62].
The practice is also a WHO-associated project: Initial workshop (1999), WHO Collaborating Center for rhinitis and asthma (2004–2014), Global Alliance against Chronic Respiratory Diseases (GARD) [63, 64] demonstration project (2015–).
Unmet needs
Several unmet needs have been identified in allergic diseases. They include (1) suboptimal rhinitis and asthma control due to medical, cultural and social barriers [65, 66], (2) better understanding of endotypes [67], phenotypes and multimorbidities, (3) assessment of allergen and pollutants as risk factors to promote sentinel networks in care pathways, (4) stratification of patients for optimized care pathways [68] and (5) promotion of multidisciplinary teams within integrated care pathways, endorsing innovation in clinical trials and encouraging patient empowerment [17, 69].
Overall goal
The general objective of AIRWAYS-ICPs [6,7,8] is to develop multi-sectoral ICPs for CRDs used across European countries and regions in order to (1) reduce the burden of the diseases in a patient-centred approach, (2) promote AHA, (3) create a care pathways simulator tool which can be applied across the life cycle and in older adults, (4) reduce health and social inequalities, (5) reduce gender inequalities, (6) use the lessons learned in CRDs for chronic diseases and (7) promote SDG3 (more specifically 3.4) (https://www.who.int/sdg/targets/en/). In September 2015, the UN General Assembly established the Sustainable Development Goals (SDGs), a set of global goals for fair and sustainable health at every level from planetary biosphere to local community [70, 71], essential for sustainable development. SDG 3 prioritizes health and well-being for all ages.
The aim of AIRWAYS-ICPs is also to generalise the approach of the uniform definition of severity, control and risk of severe asthma presented to WHO [66] and allergic diseases [72] in order to develop a uniform risk stratification usable for chronic diseases in most situations.
MASK further refined AIRWAYS ICPs using mobile technology to promote the digital transformation of health and care in developed and developing countries for all age groups.
Target population
In the initial phase, the target population included all patients with allergic rhinitis and asthma multimorbidity. Rhinitis and asthma are considered as a model for all chronic diseases and the project is being extended to chronic diseases.
All patients able to use a smartphone (≥ 12 years) represent the target population. A special effort is being placed in underserved populations from developing countries as the practice is a GARD (Global Alliance against Chronic Respiratory Diseases, WHO alliance) demonstration project.
Stakeholders involved
Involvement in the design, implementation (including the creation of ownership), evaluation, continuity/sustainability
As from the very first workshop in 1999, the ARIA initiative has included all stakeholders required to develop a WHO programme on CRDs (GARD). In particular, patient’s organizations were involved. All health care professionals were also involved (physicians, primary care, pharmacists, other health care professionals). Another important component of ARIA was the deployment to developing countries [73]. Moreover, policy makers were also actively involved.
ARIA has grown regularly over the past 20 years and an ARIA chapter is ongoing in over 70 countries in all continents with a very active scaling up strategy [26]. MASK has used the ARIA working group to scale up the practice.
All stakeholders were highly receptive
The ARIA and now the MASK community is very cohesive and all members are extremely reactive. They have been particularly active in deploying MASK in the 23 countries and we have received requests from many other countries in which MASK-air is not yet available.
Resistance or conflict of interest: None
Implementation methodology/strategy
We used the scaling up strategy of the European Innovation Partnership on Active and Healthy Ageing and proposed a 5‐step framework for developing an individual: (1) what to scale up: (1‐a) databases of good practices, (1‐b) assessment of viability of the scaling up of good practices, (1‐c) classification of good practices for local replication and (2) how to scale up: (2‐a) facilitating partnerships for scaling up, (2‐b) implementation of key success factors and lessons learnt, including emerging technologies for individualized and predictive medicine. This strategy has already been applied to the chronic respiratory disease action plan of the European Innovation Partnership on Active and Healthy Ageing [26].
Consistency in the pace of delivery
For the past 20 years, ARIA has been a success story in over 72 countries [3, 8, 19, 24, 25, 27, 28, 30,31,32, 38, 46, 74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100]. A Pocket Guide has been translated into 52 languages. MASK is following ARIA with the same group and the same strategy.
Main outcomes and evaluation of the practice
The ARIA strategy was to change management in the treatment of asthma and rhinitis since nasal symptoms—often the most troublesome—were not considered in most asthmatics. Over 85% of asthma in children and adolescents is associated with rhinitis, suggesting common pathways, whereas only 20–30% of rhinitis patients have asthma, suggesting rhinitis-specific genes. There is a link between asthma severity and rhinitis multimorbidity. Asthma is more severe in patients with rhinitis [101]. The strategy at all levels of care indicates that it is essential to consider multimorbidity in the management of asthma for the benefit of the patient and the satisfaction of the treatment as shown in many surveys (Fig. 3). Some studies have found that the ARIA strategy is more effective than free treatment choice [102]. Moreover, EMA has used the ARIA recommendations for the approval of a house dust mite immunotherapy tablet including asthma and rhinitis multimorbidity [103].
Change management strategy in ARIA Phases 1 and 2. From [5]
The change management strategy of MASK has not yet been evaluated. However, the results of the first studies indicate that the vast majority of patients are not adherent to treatment [45] and that next-generation care pathways are needed (Figs. 4 and 5). Next-generation care pathways were initiated in Paris, December 3, 2018, as part of POLLAR, MASK and GARD.
Next-generation care pathways. From [5]
Embedding air pollution and biodiversity in care pathways. From [4]
Additional (secondary) outcomes assessed
Work productivity and school performance are measured. When rhinitis and/or asthma are not well controlled, work productivity is impaired [1, 41, 43].
Sustainability of the practice
The MASK App, The Allergy Diary, was used to demonstrate the scientific value of the project [1]. It has been replaced by the commercial App, MASK-air, which is version 3.0 and which includes questionnaires (e.g. tobacco and allergens) and sleep (VAS and Epworth questionnaire [104]) (Fig. 6). A business plan is in place for the sustainability of the practice.
Communication about the practice and dissemination of results
A communication strategy has been set up [1] and includes a website (mask-air.com), media coverage, leaflets and newsletters, publications in scientific journals and lay press, partners’ networks and events. The MASK community includes over 300 members in all countries in which MASK is deployed.
Budget required to implement the practice
The budget required to implement the MASK strategy is around 1.5 M€. It will be provided by the private sector (1 M€) and from EU grants, in particular a Structural and Development Fund. POLLAR has an additive budget of 2 M€ to embed outdoor air pollution and aerobiology data in the ICP using artificial intelligence.
It is difficult to estimate human resources since many physicians worked in the 23 countries for the translation, adaptation of the practice and its implementation. It can be proposed that 50–100 h have been spent working in each country.
The practice has been presented to multiple national and international meetings.
Sustainability has been carefully evaluated and a business plan is in place.
Main lessons learned
-
Adherence to treatment is the major problem of allergic disease.
-
Self-management strategies should be considerably expanded (behavioural).
-
Change management is essential in allergic diseases.
-
Education strategies should be reconsidered using a patient-centred approach.
-
Lessons learned for allergic diseases can be expanded to chronic diseases.
Improvement and expansion of the practice
An expert meeting took place at the Pasteur Institute in Paris, December 3, 2018, to discuss next-generation care pathways and lessons learnt (Fig. 7, Annex 1): (1) patient participation, health literacy and self-care through technology-assisted “patient activation”, (2) implementation of care pathways by pharmacists and (3) next-generation guidelines assessing the recommendations of GRADE guidelines in rhinitis and asthma using real-world evidence (RWE) assessed by mobile technology. The meeting was organized by POLLAR and MASK in collaboration with GARD, patient’s organizations and all European scientific societies in the field.
Sponsors of the meeting (Paris, December 3, 2018). POLLAR: Impact of Air POLLution in Asthma and Rhinitis, EIT Health: European Institute for Innovation and Technology, ARIA: Allergic Rhinitis and its Impact on Asthma, Euforea: European Forum for Research and Education in Allergy and Airways Diseases GA2LEN: Global Allergy and Asthma European Network, CEmPac: Centre for Empowering Patients and Communities, EAACI: European Academy of Allergy and Clinical Immunology, EFA: European Federation of Allergy and Airways Diseases Patients’ Associations, ERS: European Respiratory Society, ERS: European Rhinology Society, GARD: Global Alliance against Chronic Respiratory Diseases (WHO Alliance), GINA: Global Initiative for Asthma, MACVIA: Fondation VIA-LR, SPLF: Societé de Pneumologie de Langue Française, SFA: Société française d’Allergologie, WAO: World Allergy Organization
Change history
09 October 2019
Following publication of the original article [1], the authors reported that one of the collaborators’ names was spelled incorrectly. In this Correction the incorrect and correct author name are shown. In the author list of this Correction article, only the corresponding author and institutional author are presented.
Abbreviations
- AHA:
-
active and healthy ageing
- AIRWAYS ICPs:
-
integrated care pathways for airway diseases
- AR:
-
allergic rhinitis
- ARIA:
-
allergic rhinitis and its impact on asthma
- CDSS:
-
clinical decision support system
- CRD:
-
chronic respiratory disease
- DG CONNECT:
-
directorate general for communications networks, content and technology
- DG Santé:
-
directorate general for health and food safety
- EIP on AHA:
-
European innovation partnership on AHA
- EIP:
-
European innovation partnership
- EQ-5D:
-
euroquol
- Euforea:
-
European forum for research and education in allergy and airways diseases
- GARD:
-
global alliance against chronic respiratory diseases
- GP:
-
good practice
- HCP:
-
health care professional
- ICP:
-
integrated care pathway
- JA-CHRODIS:
-
joint action on chronic diseases and promoting healthy ageing across the life cycle
- MACVIA-LR:
-
contre les MAladies chroniques pour un VIeillissement Actif (Fighting chronic diseases for AHA)
- MASK:
-
Mobile airways sentinel networK
- MeDALL:
-
Mechanisms of the development of ALLergy (FP7)
- mHealth:
-
mobile health
- NCD:
-
non-communicable disease
- POLLAR:
-
impact of air POLLution on Asthma and Rhinitis
- QOL:
-
quality of life
- TRL:
-
technology readiness level
- VAS:
-
visual analogue scale
- WHO:
-
World Health Organization
- WPAI-AS:
-
Work Productivity and Activity questionnaire
References
Bousquet J, Arnavielhe S, Bedbrook A, Bewick M, Laune D, Mathieu-Dupas E, et al. MASK 2017: ARIA digitally-enabled, integrated, person-centred care for rhinitis and asthma multimorbidity using real-world-evidence. Clin Transl Allergy. 2018;8:45.
Bousquet J, Van Cauwenberge P, Khaltaev N. Allergic rhinitis and its impact on asthma. J Allergy Clin Immunol. 2001;108(5 Suppl):S147–334.
Bousquet J, Schunemann HJ, Samolinski B, Demoly P, Baena-Cagnani CE, Bachert C, et al. Allergic rhinitis and its impact on asthma (ARIA): achievements in 10 years and future needs. J Allergy Clin Immunol. 2012;130(5):1049–62.
Bousquet J, Anto JM, Annesi-Maesano I, Dedeu T, Dupas E, Pepin JL, et al. POLLAR: impact of air pollution on asthma and rhinitis; a European Institute of Innovation and Technology Health (EIT Health) project. Clin Transl Allergy. 2018;8:36.
Bousquet J, Hellings PW, Agache I, Amat F, Annesi-Maesano I, Ansotegui IJ, et al. ARIA Phase 4 (2018): Change management in allergic rhinitis and asthma multimorbidity using mobile technology. J Allergy Clin Immunol. 2018:https://doi.org/10.1016/j.jaci.2018.08.049.
Bousquet J, Addis A, Adcock I, Agache I, Agusti A, Alonso A, et al. Integrated care pathways for airway diseases (AIRWAYS-ICPs). Eur Respir J. 2014;44(2):304–23.
Bousquet J, Barbara C, Bateman E, Bel E, Bewick M, Chavannes NH, et al. AIRWAYS-ICPs (European Innovation Partnership on Active and Healthy Ageing) from concept to implementation. Eur Respir J. 2016;47(4):1028–33.
Bousquet J, Hellings PW, Agache I, Bedbrook A, Bachert C, Bergmann KC, et al. ARIA 2016: care pathways implementing emerging technologies for predictive medicine in rhinitis and asthma across the life cycle. Clin Transl Allergy. 2016;6:47.
Courbis AL, Murray RB, Arnavielhe S, Caimmi D, Bedbrook A, Van Eerd M, et al. Electronic clinical decision support system for allergic rhinitis management: MASK e-CDSS. Clin Exp Allergy. 2018;48(12):1640–53.
Caimmi D, Baiz N, Tanno LK, Demoly P, Arnavielhe S, Murray R, et al. Validation of the MASK-rhinitis visual analogue scale on smartphone screens to assess allergic rhinitis control. Clin Exp Allergy. 2017;47(12):1526–33.
Bousquet J, Bewick M, Arnavielhe S, Mathieu-Dupas E, Murray R, Bedbrook A, et al. Work productivity in rhinitis using cell phones: The MASK pilot study. Allergy. 2017;72(10):1475–84.
Bousquet J, Caimmi DP, Bedbrook A, Bewick M, Hellings PW, Devillier P, et al. Pilot study of mobile phone technology in allergic rhinitis in European countries: the MASK-rhinitis study. Allergy. 2017;72(6):857–65.
Bousquet J, Arnavielhe S, Bedbrook A, Fonseca J, Morais Almeida M, Todo Bom A, et al. The ARIA score of allergic rhinitis using mobile technology correlates with quality-of-life: The MASK study. Allergy. 2017;73(2):505–10.
Bousquet J, Onorato GL, Bachert C, Barbolini M, Bedbrook A, Bjermer L, et al. CHRODIS criteria applied to the MASK (MACVIA-ARIA Sentinel NetworK) Good Practice in allergic rhinitis: a SUNFRAIL report. Clin Transl Allergy. 2017;7:37.
Hellings PW, Borrelli D, Pietikainen S, Agache I, Akdis C, Bachert C, et al. European summit on the prevention and self-management of chronic respiratory diseases: report of the European Union Parliament Summit (29 March 2017). Clin Transl Allergy. 2017;7:49.
Cingi C, Gevaert P, Mosges R, Rondon C, Hox V, Rudenko M, et al. Multi-morbidities of allergic rhinitis in adults: European Academy of Allergy and Clinical Immunology Task Force Report. Clin Transl Allergy. 2017;7:17.
Bousquet J, Schunemann HJ, Fonseca J, Samolinski B, Bachert C, Canonica GW, et al. MACVIA-ARIA Sentinel NetworK for allergic rhinitis (MASK-rhinitis): the new generation guideline implementation. Allergy. 2015;70(11):1372–92.
Bousquet J, Khaltaev N. Global surveillance, prevention and control of chronic respiratory diseases. a comprehensive approach. Global Alliance against Chronic Respiratory Diseases. World Health Organization. ISBN 978 92 4 156346 8. 2007:148 p.
Bousquet J, Khaltaev N, Cruz AA, Denburg J, Fokkens WJ, Togias A, et al. Allergic rhinitis and its impact on asthma (ARIA) 2008 update (in collaboration with the World Health Organization, GA(2)LEN and AllerGen). Allergy. 2008;63(Suppl 86):8–160.
Vandenplas O, Vinnikov D, Blanc PD, Agache I, Bachert C, Bewick M, et al. Impact of rhinitis on work productivity: a systematic review. J Allergy Clin Immunol Pract. 2018;6(4):1274–86.
Bousquet J, Anto JM, Berkouk K, Gergen P, Antunes JP, Auge P, et al. Developmental determinants in non-communicable chronic diseases and ageing. Thorax. 2015;70(6):595–7.
Fonseca JA, Nogueira-Silva L, Morais-Almeida M, Azevedo L, Sa-Sousa A, Branco-Ferreira M, et al. Validation of a questionnaire (CARAT10) to assess rhinitis and asthma in patients with asthma. Allergy. 2010;65(8):1042–8.
Bousquet J, Agache I, Aliberti MR, Angles R, Annesi-Maesano I, Anto JM, et al. Transfer of innovation on allergic rhinitis and asthma multimorbidity in the elderly (MACVIA-ARIA) - Reference Site Twinning (EIP on AHA). Allergy. 2017;73(1):77–92.
Agache I, Deleanu D, Khaltaev N, Bousquet J. Allergic rhinitis and its impact upon asthma–update (ARIA 2008). Romanian perspective. Pneumologia. 2009;58(4):255–8.
Bachert C, Jorissen M, Bertrand B, Khaltaev N, Bousquet J. Allergic Rhinitis and its impact on asthma update (ARIA 2008). The Belgian perspective. B-ENT. 2008;4(4):253–7.
Bousquet J, Farrell J, Crooks G, Hellings P, Bel EH, Bewick M, et al. Scaling up strategies of the chronic respiratory disease programme of the European Innovation Partnership on Active and Healthy Ageing (Action Plan B3: Area 5). Clin Transl Allergy. 2016;6:29.
Cagnani CE, Sole D, Diaz SN, Zernotti ME, Sisul JC, Borges MS, et al. Allergic rhinitis update and its impact on asthma (ARIA 2008). Latin American perspective. Rev Alerg Mex. 2009;56(2):56–63.
Kalayci O, Yorgancioglu A, Kalyoncu F, Khaltaev AN, Bousquet J. Allergic rhinitis and its impact on asthma update (ARIA 2008): the Turkish perspective. Turk J Pediatr. 2008;50(4):307–12.
Mullol J, Valero A, Alobid I, Bartra J, Navarro AM, Chivato T, et al. Allergic rhinitis and its impact on asthma update (ARIA 2008): the perspective from Spain. J Investig Allergol Clin Immunol. 2008;18(5):327–34.
Pali-Scholl I, Pohl W, Aberer W, Wantke F, Horak F, Jensen-Jarolim E, et al. Allergic rhinitis and its impact on asthma (ARIA update 2008) The Austrian perspective. Wien Med Wochenschr. 2009;159(3–4):87–92.
Pawankar R, Bunnag C, Chen Y, Fukuda T, Kim YY, Le LT, et al. Allergic rhinitis and its impact on asthma update (ARIA 2008)–western and Asian-Pacific perspective. Asian Pac J Allergy Immunol. 2009;27(4):237–43.
Yorgancioglu A, Kalayci O, Kalyoncu AF, Khaltaev N, Bousquet J. Allergic rhinitis and its impact on asthma update (ARIA 2008). The Turkish perspective. Tuberk Toraks. 2008;56(2):224–31.
Bousquet J, Schunemann HJ, Zuberbier T, Bachert C, Baena-Cagnani CE, Bousquet PJ, et al. Development and implementation of guidelines in allergic rhinitis - an ARIA-GA2LEN paper. Allergy. 2010;65(10):1212–21.
Brozek JL, Akl EA, Alonso-Coello P, Lang D, Jaeschke R, Williams JW, et al. Grading quality of evidence and strength of recommendations in clinical practice guidelines. Part 1 of 3. An overview of the GRADE approach and grading quality of evidence about interventions. Allergy. 2009;64(5):669–77.
Brozek JL, Akl EA, Compalati E, Kreis J, Terracciano L, Fiocchi A, et al. Grading quality of evidence and strength of recommendations in clinical practice guidelines part 3 of 3. The GRADE approach to developing recommendations. Allergy. 2011;66(5):588–95.
Brozek JL, Akl EA, Jaeschke R, Lang DM, Bossuyt P, Glasziou P, et al. Grading quality of evidence and strength of recommendations in clinical practice guidelines: part 2 of 3. The GRADE approach to grading quality of evidence about diagnostic tests and strategies. Allergy. 2009;64(8):1109–16.
Brozek JL, Baena-Cagnani CE, Bonini S, Canonica GW, Rasi G, van Wijk RG, et al. Methodology for development of the Allergic Rhinitis and its Impact on Asthma guideline 2008 update. Allergy. 2008;63(1):38–46.
Brozek JL, Bousquet J, Baena-Cagnani CE, Bonini S, Canonica GW, Casale TB, et al. Allergic rhinitis and its impact on asthma (ARIA) guidelines: 2010 revision. J Allergy Clin Immunol. 2010;126(3):466–76.
Padjas A, Kehar R, Aleem S, Mejza F, Bousquet J, Schunemann HJ, et al. Methodological rigor and reporting of clinical practice guidelines in patients with allergic rhinitis: QuGAR study. J Allergy Clin Immunol. 2014;133(3):777–83.
Caimmi D, Baiz N, Tanno LK, Demoly P, Arnavielhe S, Murray R, et al. Validation of the MASK-rhinitis visual analogue scale on smartphone screens to assess allergic rhinitis control. Clin Exp Allergy. 2017;47(12):1526–33.
Bousquet J, Bewick M, Arnavielhe S, Mathieu-Dupas E, Murray R, Bedbrook A, et al. Work productivity in rhinitis using cell phones: the MASK pilot study. Allergy. 2017;72(10):1475–84.
Bousquet J, VandenPlas O, Bewick M, Arnavielhe S, Bedbrook A, Murray R, et al. The Work Productivity and Activity Impairment Allergic Specific (WPAI-AS) Questionnaire Using Mobile Technology: the MASK Study. J Investig Allergol Clin Immunol. 2018;28(1):42–4.
Bousquet J, Arnavielhe S, Bedbrook A, Fonseca J, Morais Almeida M, Todo Bom A, et al. The Allergic Rhinitis and its impact on Asthma (ARIA) score of allergic rhinitis using mobile technology correlates with quality of life: the MASK study. Allergy. 2018;73(2):505–10.
Bousquet J, Devillier P, Anto JM, Bewick M, Haahtela T, Arnavielhe S, et al. Daily allergic multimorbidity in rhinitis using mobile technology: a novel concept of the MASK study. Allergy. 2018;73(8):1622–31.
Bousquet J, Devillier P, Arnavielhe S, Bedbrook A, Alexis-Alexandre G, van Eerd M, et al. Treatment of allergic rhinitis using mobile technology with real-world data: the MASK observational pilot study. Allergy. 2018;73(9):1763–74.
Brozek JL, Bousquet J, Agache I, Agarwal A, Bachert C, Bosnic-Anticevich S, et al. Allergic Rhinitis and its impact on asthma (ARIA) guidelines—2016 revision. J Allergy Clin Immunol. 2017;140(4):950–8.
Bousquet J, Meltzer EO, Couroux P, Koltun A, Kopietz F, Munzel U, et al. Onset of action of the fixed combination intranasal azelastine-fluticasone propionate in an allergen exposure chamber. J Allergy Clin Immunol Pract. 2018;6(5):1726–32.
Garcia-Aymerich J, Benet M, Saeys Y, Pinart M, Basagana X, Smit HA, et al. Phenotyping asthma, rhinitis and eczema in MeDALL population-based birth cohorts: an allergic comorbidity cluster. Allergy. 2015;70(8):973–84.
Amaral R, Bousquet J, Pereira AM, Araujo LM, Sa-Sousa A, Jacinto T, et al. Disentangling the heterogeneity of allergic respiratory diseases by latent class analysis reveals novel phenotypes. Allergy. 2018. https://doi.org/10.1111/all.13670.
Siroux V, Ballardini N, Soler M, Lupinek C, Boudier A, Pin I, et al. The asthma-rhinitis multimorbidity is associated with IgE polysensitization in adolescents and adults. Allergy. 2018;73(7):1447–58.
Siroux V, Boudier A, Nadif R, Lupinek C, Valenta R, Bousquet J. Association between asthma, rhinitis and conjunctivitis multimorbidities with molecular IgE sensitization in adults. Allergy. 2018. https://doi.org/10.1111/all.13676.
Bousquet J, Samolinski B. Allergy and active and healthy ageing. In: Akdis C, Agache I, Demoly P, Hellinbgs P, Muraro A, Papadopoulos N, et al., editors. Global atlas of allergy European Academy of Allergy and Clinical Immunology 2014. p. 379–81.
Morais-Almeida M, Pite H, Pereira AM, Todo-Bom A, Nunes C, Bousquet J, et al. Prevalence and classification of rhinitis in the elderly: a nationwide survey in Portugal. Allergy. 2013;68(9):1150–7.
Baptist AP, Nyenhuis S. Rhinitis in the elderly. Immunol Allergy Clin North Am. 2016;36(2):343–57.
Ventura MT, Gelardi M, D’Amato A, Buquicchio R, Tummolo R, Misciagna G, et al. Clinical and cytologic characteristics of allergic rhinitis in elderly patients. Ann Allergy Asthma Immunol. 2012;108(3):141–4.
Ohta K, Bousquet PJ, Aizawa H, Akiyama K, Adachi M, Ichinose M, et al. Prevalence and impact of rhinitis in asthma. SACRA, a cross-sectional nation-wide study in Japan. Allergy. 2011;66(10):1287–95.
Samolinski B, Fronczak A, Wlodarczyk A, Bousquet J. Council of the European Union conclusions on chronic respiratory diseases in children. Lancet. 2012;379(9822):e45–6.
Samolinski B, Fronczak A, Kuna P, Akdis CA, Anto JM, Bialoszewski AZ, et al. Prevention and control of childhood asthma and allergy in the EU from the public health point of view: Polish Presidency of the European Union. Allergy. 2012;67(6):726–31.
Council conclusions on Healthy Ageing across the Lifecycle. 3206th Employment, social policy, ehalth and consumer affairs Council meeting. Brussels, 7 December 2012. http://wwwconsiliumeuropaeu/uedocs/cms_data/docs/pressdata/en/lsa/134097pdf. 2012.
Bousquet J, Tanasescu C, Camuzat T, Anto J, Blasi F, Neou A, et al. Impact of early diagnosis and control of chronic respiratory diseases on active and healthy ageing: a debate at the European Union Parliament. Allergy. 2013;68(5):555–61.
Muraro A, Fokkens WJ, Pietikainen S, Borrelli D, Agache I, Bousquet J, et al. European symposium on precision medicine in allergy and airways diseases: report of the European Union parliament symposium (October 14, 2015). Allergy. 2016;71(5):583–7.
Muraro A, Steelant B, Pietikainen S, Borrelli D, Childers N, Callebaut I, et al. European symposium on the awareness of allergy: report of the promotional campaign in the European Parliament (26–28 April 2016). Allergy. 2017;72(2):173–6.
Bousquet J, Dahl R, Khaltaev N. Global alliance against chronic respiratory diseases. Allergy. 2007;62(3):216–23.
Yorgancioglu A, Cruz AA, Bousquet J, Khaltaev N, Mendis S, Chuchalin A, et al. The global alliance against respiratory diseases (GARD) country report. Prim Care Respir J. 2014;23(1):98–101.
Bousquet J, Bachert C, Canonica GW, Casale TB, Cruz AA, Lockey RJ, et al. Unmet needs in severe chronic upper airway disease (SCUAD). J Allergy Clin Immunol. 2009;124(3):428–33.
Bousquet J, Mantzouranis E, Cruz AA, Ait-Khaled N, Baena-Cagnani CE, Bleecker ER, et al. Uniform definition of asthma severity, control, and exacerbations: document presented for the World Health Organization Consultation on Severe Asthma. J Allergy Clin Immunol. 2010;126(5):926–38.
De Greve G, Hellings PW, Fokkens WJ, Pugin B, Steelant B, Seys SF. Endotype-driven treatment in chronic upper airway diseases. Clin Transl Allergy. 2017;7:22.
Hellings PW, Fokkens WJ, Bachert C, Akdis CA, Bieber T, Agache I, et al. Positioning the principles of precision medicine in care pathways for allergic rhinitis and chronic rhinosinusitis—an EUFOREA-ARIA-EPOS-AIRWAYS ICP statement. Allergy. 2017;72(9):1297–305.
Hellings PW, Fokkens WJ, Akdis C, Bachert C, Cingi C, Dietz de Loos D, et al. Uncontrolled allergic rhinitis and chronic rhinosinusitis: where do we stand today? Allergy. 2013;68(1):1–7.
Spencer G, Corbin JH, Miedema E. Sustainable development goals for health promotion: a critical frame analysis. Health Promot Int. 2018. https://doi.org/10.1093/heapro/day036.
Morton S, Pencheon D, Squires N. Sustainable Development Goals (SDGs), and their implementation: a national global framework for health, development and equity needs a systems approach at every level. Br Med Bull. 2017;124(1):81–90.
Bousquet J, Anto JM, Demoly P, Schunemann HJ, Togias A, Akdis M, et al. Severe chronic allergic (and related) diseases: a uniform approach–a MeDALL–GA2LEN–ARIA position paper. Int Arch Allergy Immunol. 2012;158(3):216–31.
Ait-Khaled N, Enarson D, Bousquet J. Chronic respiratory diseases in developing countries: the burden and strategies for prevention and management. Bull World Health Organ. 2001;79(10):971–9.
Bousquet J, VanCauwenberge P, Khaltaev N. Allergic rhinitis and its impact on asthma (ARIA)—executive summary. Allergy. 2002;57(9):841–55.
Bachert C. Allergic rhinitis and its impact on asthma (ARIA)–what does it mean for the future of SIT? Arb Paul Ehrlich Inst Bundesamt Sera Impfstoffe Frankf A M. 2003;94:229–35.
Bachert C, van Cauwenberge P. The WHO ARIA (allergic rhinitis and its impact on asthma) initiative. Chem Immunol Allergy. 2003;82:119–26.
Bousquet J, Van Cauwenberge P, Bachert C, Canonica GW, Demoly P, Durham SR, et al. Requirements for medications commonly used in the treatment of allergic rhinitis. European Academy of Allergy and Clinical Immunology (EAACI), Allergic Rhinitis and its Impact on Asthma (ARIA). Allergy. 2003;58(3):192–7.
Demoly P, Allaert FA, Lecasble M, Bousquet J. Validation of the classification of ARIA (allergic rhinitis and its impact on asthma). Allergy. 2003;58(7):672–5.
ARIA in the pharmacy: management of allergic rhinitis symptoms in the pharmacy. Allergic rhinitis and its impact on asthma. Allergy. 2004;59(4):373–87.
Bousquet J, Bindslev-Jensen C, Canonica GW, Fokkens W, Kim H, Kowalski M, et al. The ARIA/EAACI criteria for antihistamines: an assessment of the efficacy, safety and pharmacology of desloratadine. Allergy. 2004;59(Suppl 77):4–16.
Plavec D. ARIA–one airway, one disease: what links our research to the concept? Arh Hig Rada Toksikol. 2004;55(2–3):135–40.
Up-to-date Mexican consensus in Allergic Rhinitis and its Impact on Asthma, 2005. ARIA. Rev Alerg Mex. 2005;52(1):51–64.
Bonini S, Bonini M, Bousquet J, Brusasco V, Canonica GW, Carlsen KH, et al. Rhinitis and asthma in athletes: an ARIA document in collaboration with GA2LEN. Allergy. 2006;61(6):681–92.
Bousquet J, van Cauwenberge P, Ait Khaled N, Bachert C, Baena-Cagnani CE, Bouchard J, et al. Pharmacologic and anti-IgE treatment of allergic rhinitis ARIA update (in collaboration with GA2LEN). Allergy. 2006;61(9):1086–96.
Passalacqua G, Bousquet PJ, Carlsen KH, Kemp J, Lockey RF, Niggemann B, et al. ARIA update: I-Systematic review of complementary and alternative medicine for rhinitis and asthma. J Allergy Clin Immunol. 2006;117(5):1054–62.
Antonicelli L, Micucci C, Voltolini S, Senna GE, Di Blasi P, Visona G, et al. Relationship between ARIA classification and drug treatment in allergic rhinitis and asthma. Allergy. 2007;62(9):1064–70.
Bousquet PJ, Bousquet-Rouanet L, Co Minh HB, Urbinelli R, Allaert FA, Demoly P. ARIA (Allergic Rhinitis and Its Impact on Asthma) Classification of Allergic Rhinitis Severity in Clinical Practice in France. Int Arch Allergy Immunol. 2007;143(3):163–9.
Bousquet PJ, Combescure C, Neukirch F, Klossek JM, Mechin H, Daures JP, et al. Visual analog scales can assess the severity of rhinitis graded according to ARIA guidelines. Allergy. 2007;62(4):367–72.
Baiardini I, Braido F, Tarantini F, Porcu A, Bonini S, Bousquet PJ, et al. ARIA-suggested drugs for allergic rhinitis: what impact on quality of life? A GA2LEN review. Allergy. 2008;63(6):660–9.
Mendez NH, Velazquez AC, del Rivero HL, Hernandez VL, Espinola RG, Mondragon GR. Increased knowledge of ARIA and GINA guides 2006 to general physicians by an educational intervention. Rev Alerg Mex. 2008;55(5):201–5.
Singh AB, Shahi S. Aeroallergens in clinical practice of allergy in India—ARIA Asia Pacific Workshop report. Asian Pac J Allergy Immunol. 2008;26(4):245–56.
Zhang L, Han DM. An introduction of allergic rhinitis and its impact on asthma (ARIA) 2008 update. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2008;43(7):552–7.
Shah A, Pawankar R. Allergic rhinitis and co-morbid asthma: perspective from India—ARIA Asia-Pacific Workshop report. Asian Pac J Allergy Immunol. 2009;27(1):71–7.
del Cuvillo A, Montoro J, Bartra J, Valero A, Ferrer M, Jauregui I, et al. Validation of ARIA duration and severity classifications in Spanish allergic rhinitis patients: the ADRIAL cohort study. Rhinology. 2010;48(2):201–5.
Van Hoecke H, Van Cauwenberge P, Thas O, Watelet JB. The ARIA guidelines in specialist practice: a nationwide survey. Rhinology. 2010;48(1):28–34.
Jauregui I, Davila I, Sastre J, Bartra J, del Cuvillo A, Ferrer M, et al. Validation of ARIA (Allergic Rhinitis and its Impact on Asthma) classification in a pediatric population: the PEDRIAL study. Pediatr Allergy Immunol. 2011;22(4):388–92.
Yorgancioglu A, Ozdemir C, Kalayci O, Kalyocu AF, Bachert C, Baena-Cagnani CE, et al. ARIA (Allergic rhinitis and its impact on asthma) achievements in 10 years and future needs. Tuberk Toraks. 2012;60(1):92–7.
Hellings PW, Fokkens WJ, Bachert C, Akdis CA, Bieber T, Agache I, et al. Positioning the principles of precision medicine in care pathways for allergic rhinitis and chronic rhinosinusitis: a EUFOREA-ARIA-EPOS-AIRWAYS ICP statement. Allergy. 2017;72(9):1297–305.
Ivancevich JC, Neffen H, Zernotti ME, Asayag E, Blua A, Ciceran A, et al. ARIA 2016 executive summary: integrated care pathways for predictive medicine throughout the life cycle in Argentina. Rev Alerg Mex. 2017;64(3):298–308.
Yorgancioglu AA, Kalayci O, Cingi C, Gemicioglu B, Kalyoncu AF, Agache I, et al. ARIA 2016 executive summary: integrated care pathways for predictive medicine across the life cycle. Tuberk Toraks. 2017;65(1):32–40.
Amaral R, Fonseca JA, Jacinto T, Pereira AM, Malinovschi A, Janson C, et al. Having concomitant asthma phenotypes is common and independently relates to poor lung function in NHANES 2007-2012. Clin Transl Allergy. 2018;8:13.
Bousquet J, Bodez T, Gehano P, Klossek JM, Liard F, Neukirch F, et al. Implementation of guidelines for allergic rhinitis in specialist practices: a randomized pragmatic controlled trial. Int Arch Allergy Immunol. 2009;150(1):75–82.
Summary of product characteristics. Acarizax 12 SQ-HDM oral lyophilisate. European Medicines Agency. https://mricts-mrpeu/Human/Downloads/DE_H_1947_001_FinalSPCpdf. 2016.
Bousquet J, Bullinger M, Fayol C, Marquis P, Valentin B, Burtin B. Assessment of quality of life in patients with perennial allergic rhinitis with the French version of the SF-36 Health Status Questionnaire. J Allergy Clin Immunol. 1994;94(2 Pt 1):182–8.
Samreth D, Arnavielhe S, Ingenrieth F, Bedbrook A, Onorato GL, Murray R, et al. Geolocation with respect to personal privacy for the Allergy Diary app: a MASK study. World Allergy Organ J. 2018;11(1):15.
Bousquet J, Anto JM, Akdis M, Auffray C, Keil T, Momas I, et al. Paving the way of systems biology and precision medicine in allergic diseases: The MeDALL success story. Allergy. 2016;71(11):1513–25.
Bousquet J, Burney PG, Zuberbier T, Cauwenberge PV, Akdis CA, Bindslev-Jensen C, et al. GA2LEN (Global Allergy and Asthma European Network) addresses the allergy and asthma ‘epidemic’. Allergy. 2009;64(7):969–77.
Yorgancioglu AA, Gemicioglu B, Kalayci O, Kalyoncu AF, Cingi C, Murray R, et al. MASK (Mobile Airways Sentinel networK) in Turkey-the ARIA integrated mobile solution for allergic rhinitis and asthma multimorbidity. Tuberk Toraks. 2018;66(2):176–81.
Gomez RM, Gonzalez-Diaz SN, Urrutia-Pereira M, Valentin-Rostan M, Yanez A, Jares E, et al. 2017 Brussels agreement for Latin America: an initiative of the GARD and Slaai. Rev Alerg Mex. 2018;65(3):137–41.
Bousquet J, Agache I, Aliberti MR, Angles R, Annesi-Maesano I, Anto JM, et al. Transfer of innovation on allergic rhinitis and asthma multimorbidity in the elderly (MACVIA-ARIA)—EIP on AHA Twinning Reference Site (GARD research demonstration project). Allergy. 2018;73(1):77–92.
Bousquet J, Schunemann HJ, Hellings PW, Arnavielhe S, Bachert C, Bedbrook A, et al. MACVIA clinical decision algorithm in adolescents and adults with allergic rhinitis. J Allergy Clin Immunol. 2016;138(2):367–74.
Authors’ contributions
All authors are MASK members and have contributed to the design of the project. Many authors also included users and disseminated the project in their own country. All authors read and approved the final manuscript.
Acknowledgements
Practice presented during the Steering Group on Promotion and Prevention marketplace workshop on “digitally-enabled, integrated, person-centred care” best practices on 12–13 December 2018 in the premises of the Joint Research Centre in Ispra, Italy.
Mask Study Group
J Bousquet1-3, PW Hellings4, W Aberer5, I Agache6, CA Akdis7, M Akdis7, MR Aliberti8, R Almeida9, F Amat10, R Angles11, I Annesi-Maesano12, IJ Ansotegui13, JM Anto14-17, S Arnavielle18, E Asayag19, A Asarnoj20, H Arshad21, F Avolio22, E Bacci23, C Bachert24, I Baiardini25, C Barbara26, M Barbagallo27, I Baroni28, BA Barreto29, X Basagana14, ED Bateman30, M Bedolla-Barajas31, A Bedbrook2, M Bewick32, B Beghé33, EH Bel34, KC Bergmann35, KS Bennoor36, M Benson37, L Bertorello23, AZ Białoszewski38, T Bieber39, S Bialek40, C Bindslev-Jensen41 , L Bjermer42, H Blain43,44, F Blasi45, A Blua46, M Bochenska Marciniak47, I Bogus-Buczynska47, AL Boner48, M Bonini49, S Bonini50, CS Bosnic-Anticevich51, I Bosse52, J Bouchard53, LP Boulet54, R Bourret55, PJ Bousquet12, F Braido25, V Briedis56, CE Brightling57, J Brozek58, C Bucca59, R Buhl60, R Buonaiuto61, C Panaitescu62, MT Burguete Cabañas63 , E Burte3, A Bush64, F Caballero-Fonseca65, D Caillaud67, D Caimmi68, MA Calderon69, PAM Camargos70, T Camuzat71, G Canfora72, GW Canonica25, V Cardona73, KH Carlsen74, P Carreiro-Martins75, AM Carriazo76, W Carr77, C Cartier78, T Casale79, G Castellano80, L Cecchi81, AM Cepeda82, NH Chavannes83, Y Chen84, R Chiron68, T Chivato85, E Chkhartishvili86, AG Chuchalin87, KF Chung88, MM Ciaravolo89, A Ciceran90, C Cingi91, G Ciprandi92, AC Carvalho Coehlo93, L Colas94, E Colgan95, J Coll96, D Conforti97, J Correia de Sousa98, RM Cortés-Grimaldo99, F Corti100, E Costa101, MC Costa-Dominguez102, AL Courbis103, L Cox104, M Crescenzo105, AA Cruz106, A Custovic107, W Czarlewski108, SE Dahlen109, G D’Amato381, C Dario110, J da Silva111, Y Dauvilliers112, U Darsow113, F De Blay114, G De Carlo115, T Dedeu116, M de Fátima Emerson117, G De Feo118, G De Vries119, B De Martino120, NP Motta Rubina121, D Deleanu122, P Demoly12,68, JA Denburg123, P Devillier124, S Di Capua Ercolano125, N Di Carluccio66, A Didier126, D Dokic127, MG Dominguez-Silva128, H Douagui129, G Dray103, R Dubakiene130, SR Durham131, G Du Toit132, MS Dykewicz133, Y El-Gamal134, P Eklund135, E Eller41, R Emuzyte136, J Farrell95, A Farsi81, J Ferreira de Mello Jr137, J Ferrero138, A Fink-Wagner139, A Fiocchi140, WJ Fokkens141, JA Fonseca142, JF Fontaine143, S Forti97, JM Fuentes-Perez144, JL Gálvez-Romero145, A Gamkrelidze146, J Garcia-Aymerich14, CY García-Cobas147, MH Garcia-Cruz148, B Gemicioğlu149, S Genova150, G Christoff151, JE Gereda152, R Gerth van Wijk153, RM Gomez154, J Gómez-Vera155, S González Diaz156, M Gotua157, I Grisle158, M Guidacci159, NA Guldemond160, Z Gutter161, MA Guzmán162, T Haahtela163, J Hajjam164, L Hernández165, JO’B Hourihane166, YR Huerta-Villalobos167, M Humbert168, G Iaccarino169, M Illario170 , Z Ispayeva380, JC Ivancevich171, EJ Jares172, E Jassem173, SL Johnston174, G Joos175, KS Jung176, J Just 10, M Jutel177, I Kaidashev178, O Kalayci179, AF Kalyoncu180, J Karjalainen181, P Kardas182, T Keil183, PK Keith184, M Khaitov185, N Khaltaev186, J Kleine-Tebbe187, L Klimek188, ML Kowalski189, M Kuitunen190, I Kull191, P Kuna47, M Kupczyk47, V Kvedariene192, E Krzych-Fałta193, P Lacwik47, D Larenas-Linnemann194, D Laune18, D Lauri195, J Lavrut196, LTT Le197, M Lessa198, G Levato199, J Li200, P Lieberman201, A Lipiec193, B Lipworth202, KC Lodrup Carlsen203, R Louis204, O Lourenço205, JA Luna-Pech206, A Magnan94, B Mahboub207, D Maier208, A Mair209, I Majer210, J Malva211, E Mandajieva212, P Manning213, E De Manuel Keenoy214, GD Marshall215, MR Masjedi216, JF Maspero217, E Mathieu-Dupas18, JJ Matta Campos218, AL Matos219, M Maurer220, S Mavale-Manuel221, O Mayora97, MA Medina-Avalos222, E Melén223, E Melo-Gomes26, EO Meltzer224, E Menditto225, J Mercier226, N Miculinic227, F Mihaltan228, B Milenkovic229, G Moda230, MD Mogica-Martinez231, Y Mohammad232, I Momas233,234, S Montefort235, R Monti236, D Mora Bogado237, M Morais-Almeida238, FF Morato-Castro239, R Mösges240, A Mota-Pinto241, P Moura Santo242, J Mullol243, L Münter244, A Muraro245, R Murray246, R Naclerio247, R Nadif3, M Nalin28, L Napoli248, L Namazova-Baranova249, H Neffen250, V Niedeberger251, K Nekam252, A Neou253, A Nieto254, L Nogueira-Silva255, M Nogues2,256, E Novellino257, TD Nyembue258, RE O’Hehir259, C Odzhakova260, K Ohta261, Y Okamoto262, K Okubo263, GL Onorato2, M Ortega Cisneros264, S Ouedraogo265, I Pali-Schöll266, S Palkonen115, P Panzner267, NG Papadopoulos268, HS Park269, A Papi270, G Passalacqua271, E Paulino272, R Pawankar273, S Pedersen274, JL Pépin275, AM Pereira276, M Persico277, O Pfaar278, J Phillips280, R Picard281, B Pigearias282, I Pin283, C Pitsios284, D Plavec285, W Pohl286, TA Popov287, F Portejoie2, P Potter288, AC Pozzi289, D Price290, EP Prokopakis291, R Puy259, B Pugin292, RE Pulido Ross293, M Przemecka47, KF Rabe294, F Raciborski193, R Rajabian-Soderlund295, S Reitsma141, I Ribeirinho296, J Rimmer297, D Rivero-Yeverino298, JA Rizzo299, MC Rizzo300, C Robalo-Cordeiro301, F Rodenas302, X Rodo14, M Rodriguez Gonzalez303, L Rodriguez-Mañas304, C Rolland305, S Rodrigues Valle306, M Roman Rodriguez307, A Romano308, E Rodriguez-Zagal309, G Rolla310, RE Roller-Wirnsberger311, M Romano28, J Rosado-Pinto312, N. Rosario313, M Rottem314, D Ryan315, H Sagara316, J Salimäki317, B Samolinski193, M Sanchez-Borges318, J Sastre-Dominguez319, GK Scadding320, HJ Schunemann58, N Scichilone321, P Schmid-Grendelmeier322, FS Serpa323, S Shamai240, A Sheikh324, M Sierra96, FER Simons325, V Siroux326, JC Sisul327, I Skrindo378, D Solé328, D Somekh329, M Sondermann330, T Sooronbaev331, M Sova332, M Sorensen333, M Sorlini334, O Spranger139, C Stellato118, R Stelmach335, R Stukas336, J Sunyer14–17, J Strozek193, A Szylling193, JN Tebyriçá337, M Thibaudon338, T To339, A Todo-Bom340, PV Tomazic341, S Toppila-Salmi163, U Trama342, M Triggiani118, C Suppli Ulrik343, M Urrutia-Pereira344, R Valenta345, A Valero346, A Valiulis347, E Valovirta348, M van Eerd119, E van Ganse349, M van Hague350, O Vandenplas351, MT Ventura352, G Vezzani353, T Vasankari354, A Vatrella118, MT Verissimo211, F Viart78, G Viegi355, D Vicheva356, T Vontetsianos357, M Wagenmann358, S Walker359, D Wallace360, DY Wang361, S Waserman362, T Werfel363, M Westman364, M Wickman191, DM Williams365, S Williams366, N Wilson379, J Wright367, P Wroczynski40, P Yakovliev368, BP Yawn369, PK Yiallouros370, A Yorgancioglu371, OM Yusuf372, HJ Zar373, L Zhang374, N Zhong200, ME Zernotti375, I Zhanat380, M Zidarn376, T Zuberbier35, C Zubrinich259, A Zurkuhlen377
1University Hospital, Montpellier, France. 2MACVIA-France, Fondation partenariale FMC VIA-LR, Montpellier, France. 3VIMA. INSERM U 1168, VIMA: Ageing and chronic diseases Epidemiological and public health approaches, Villejuif, Université Versailles St-Quentin-en-Yvelines, UMR-S 1168, Montigny le Bretonneux, France and Euforea, Brussels, Belgium. 4Laboratory of Clinical Immunology, Department of Microbiology and Immunology, KU Leuven, Leuven, Belgium. 5Department of Dermatology, Medical University of Graz, Graz, Austria. 6Transylvania University Brasov, Brasov, Romania. 7Swiss Institute of Allergy and Asthma Research (SIAF), University of Zurich, Davos, Switzerland. 8Project Manager, Chairman of the Council of Municipality of Salerno, Italy. 9Center for Health Technology and Services Research- CINTESIS, Faculdade de Medicina, Universidade do Porto; and Medida, Lda Porto, Portugal. 10Allergology department, Centre de l’Asthme et des Allergies Hôpital d’Enfants Armand-Trousseau (APHP); Sorbonne Université, UPMC Univ Paris 06, UMR_S 1136, Institut Pierre Louis d’Epidémiologie et de Santé Publique, Equipe EPAR, Paris, France. 11Innovación y nuevas tecnologías, Salud Sector sanitario de Barbastro, Barbastro, Spain. 12Epidemiology of Allergic and Respiratory Diseases, Department Institute Pierre Louis of Epidemiology and Public Health, INSERM and Sorbonne Université, Medical School Saint Antoine, Paris, France. 13Department of Allergy and Immunology, Hospital Quirón Bizkaia, Erandio, Spain. 14ISGlobAL, Centre for Research in Environmental Epidemiology (CREAL), Barcelona, Spain. 15IMIM (Hospital del Mar Research Institute), Barcelona, Spain. 16CIBER Epidemiología y Salud Pública (CIBERESP), Barcelona, Spain. 17Universitat Pompeu Fabra (UPF), Barcelona, Spain. 18KYomed INNOV, Montpellier, France. 19Argentine Society of Allergy and Immunopathology, Buenos Aires, Argentina. 20Clinical Immunology and Allergy Unit, Department of Medicine Solna, Karolinska Institutet, Stockholm, and Astrid Lindgren Children’s Hospital, Department of Pediatric Pulmonology and Allergy, Karolinska University Hospital, Stockholm, Sweden. 21David Hide Asthma and Allergy Research Centre, Isle of Wight, United Kingdom. 22Regionie Puglia, Bari, Italy. 23Regione Liguria, Genoa, Italy. 24Upper Airways Research Laboratory, ENT Dept, Ghent University Hospital, Ghent, Belgium. 25Allergy and Respiratory Diseases, Ospedale Policlinico San Martino, University of Genoa, Italy. 26PNDR, Portuguese National Programme for Respiratory Diseases, Faculdade de Medicina de Lisboa, Lisbon, Portugal. 27Director of the Geriatric Unit, Department of Internal Medicine (DIBIMIS), University of Palermo, Italy. 28Telbios SRL, Milan, Italy. 29Universidade do Estado do Pará, Belem, Brazil. 30Department of Medicine, University of Cape Town, Cape Town, South Africa. 31Hospital Civil de Guadalajara Dr Juan I Menchaca, Guadalarara, Mexico. 32iQ4U Consultants Ltd, London, UK. 33Section of Respiratory Disease, Department of Oncology, Haematology and Respiratory Diseases, University of Modena and Reggio Emilia, Modena, Italy. 34Department of Respiratory Medicine, Academic Medical Center (AMC), University of Amsterdam, The Netherlands. 35Charité - Universitätsmedizin Berlin, corporate member of Freie Universität Berlin, Humboldt-Universität zu Berlin, and Berlin Institute of Health, Comprehensive Allergy Center, Department of Dermatology and Allergy, Global Allergy and Asthma European Network (GA2LEN), Berlin, Germany. 36Dept of Respiratory Medicine, National Institute of Diseases of the Chest and Hospital, Dhaka, Bangladesh. 37Centre for Individualized Medicine, Department of Pediatrics, Faculty of Medicine, Linköping, Sweden. 38Department of Prevention of Environmental Hazards and Allergology, Medical University of Warsaw, Poland. 39BIEBER. Department of Dermatology and Allergy, Rheinische Friedrich-Wilhelms-University Bonn, Bonn, Germany. 40Dept of Biochemistry and Clinical Chemistry, University of Pharmacy with the Division of Laboratory Medicine, Warsaw Medical University, Warsaw, Poland. 41Department of Dermatology and Allergy Centre, Odense University Hospital, Odense Research Center for Anaphylaxis (ORCA), Odense, Denmark. 42Department of Respiratory Medicine and Allergology, University Hospital, Lund, Sweden. 43Department of Geriatrics, Montpellier University Hospital, Montpellier, France. 44EA 2991, Euromov, University Montpellier, France. 45Department of Pathophysiology and Transplantation, University of Milan, IRCCS Fondazione Ca’Granda Ospedale Maggiore Policlinico, Milan, Italy. 46Argentine Association of Respiratory Medicine, Buenos Aires, Argentina. 47Division of Internal Medicine, Asthma and Allergy, Barlicki University Hospital, Medical University of Lodz, Poland. 48Pediatric Department, University of Verona Hospital, Verona, Italy. 49UOC Pneumologia, Istituto di Medicina Interna, F. Policlinico Gemelli IRCCS, Università Cattolica del Sacro Cuore, Rome, Italy, and National Heart and Lung Institute, Royal Brompton Hospital & Imperial College London, UK. 50Second University of Naples and Institute of Translational Medicine, Italian National Research Council. 51Woolcock Institute of Medical Research, University of Sydney and Woolcock Emphysema Centre and Local Health District, Glebe, NSW, Australia. 52Allergist, La Rochelle, France. 53Associate Professor of Clinical medecine, Laval’s University, Quebec city, Head of medecine department, Hôpital de la Malbaie, Quebec, Canada. 54Quebec Heart and Lung Institute, Laval University, Québec City, Quebec, Canada. 55Centre Hospitalier Valenciennes, France. 56Head of Department of Clinical Pharmacy of Lithuanian University of Health Sciences, Kaunas, Lithuania. 57Institute of Lung Health, Respiratory Biomedical Unit, University Hospitals of Leicester NHS Trust, Leicestershire, UK; Department of Infection, Immunity and Inflammation, University of Leicester, Leicester, UK. 58Department of Health Research Methods, Evidence and Impact, Division of Immunology and Allergy, Department of Medicine, McMaster University, Hamilton, ON, Canada. 59Chief of the University Pneumology Unit- AOU Molinette, Hospital City of Health and Science of Torino, Italy. 60Universitätsmedizin der Johannes Gutenberg-Universität Mainz, Mainz, Germany. 61Pharmacist, Municipality Pharmacy, Sarno, Italy. 62University of Medicine and Pharmacy Victor Babes, Timisoara, Romania. 63Instituto de Pediatria, Hospital Zambrano Hellion Tec de Monterrey, Monterrey, Mexico. 64Imperial College and Royal Brompton Hospital, London, UK. 65Centro Medico Docente La Trinidad, CaRacas, Venezuela. 66Regional Director Assofarm Campania and Vice President of the Board of Directors of Cofaser, Salerno, Italy. 67Service de pneumologie, CHU et université d’Auvergne, Clermont-Ferrand, France. 68Department of Respiratory Diseases, Montpellier University Hospital, France. 69Imperial College London - National Heart and Lung Institute, Royal Brompton Hospital NHS, London, UK. 70Federal University of Minas Gerais, Medical School, Department of Pediatrics, Belo Horizonte, Brazil. 71Assitant Director General, Montpellier, Région Occitanie, France. 72Mayor of Sarno and President of Salerno Province, Director, Anesthesiology Service, Sarno “Martiri del Villa Malta” Hospital, Italy. 73Allergy Section, Department of Internal Medicine, Hospital Vall d’Hebron & ARADyAL Spanish Research Network, Barcelona, Spain. 74Department of Paediatrics, Oslo University Hospital and University of Oslo, Oslo, Norway. 75CEDOC, Integrated Pathophysiological Mechanisms Research Group, Nova Medical School, Campo dos Martires da Patria, Lisbon, and Serviço de Imunoalergologia, Centro Hospitalar de Lisboa Central, EPE, Lisbon, Portugal. 76Regional Ministry of Health of Andalusia, Seville, Spain. 77Allergy and Asthma Associates of Southern California, Mission Viejo, CA, USA. 78ASA - Advanced Solutions Accelerator, Clapiers, France. 79Division of Allergy/Immunology, University of South Florida, Tampa, Fla, USA. 80Celentano pharmacy, Massa Lubrense, Italy. 81SOS Allergology and Clinical Immunology, USL Toscana Centro, Prato, Italy. 82Allergy and Immunology Laboratory, Metropolitan University Hospital, Branquilla, Columbia. 83Department of Public Health and Primary Care, Leiden University Medical Center, Leiden, The Netherlands. 84Capital Institute of Pediatrics, Chaoyang district, Beijing, China. 85School of Medicine, University CEU San Pablo, Madrid, Spain. 86David Tvildiani Medical University - AIETI Highest Medical School, David Tatishvili Medical Center Tbilisi, Georgia. 87Pulmonolory Research Institute FMBA, Moscow, Russia and GARD Executive Committee, Moscow, Russia. 88National Heart & Lung Institute, Imperial College, London, UK. 89Specialist social worker, Sorrento, Italy. 90Argentine Federation of Otorhinolaryngology Societies, Buenos Aires, Argentina. 91Eskisehir Osmangazi University, Medical Faculty, ENT Department, Eskisehir,Turkey. 92Medicine Department, IRCCS-Azienda Ospedaliera Universitaria San Martino, Genoa, Italy. 93Universidade Federal da Bahia, Escola de Enfermagem, Brazil. 94Plateforme Transversale d’Allergologie, Institut du Thorax, CHU de Nantes, Nantes, France. 95LANUA International Healthcare Consultancy, Northern Ireland, UK. 96Innovación y nuevas tecnologías, Salud Sector sanitario de Barbastro, Barbastro, Spain. 97Innovation and Research Office, Department of Health and Social Solidarity, Autonomous Province of Trento, Italy. 98Life and Health Sciences Research Institute (ICVS), School of Medicine, University of Minho, Braga, Portugal; ICVS/3B’s, PT Government Associate Laboratory, Braga/Guimarães, Portugal. 99Servicio de Allergologia, Hospital Angeles del Carmen, Guadalajara, Mexico. 100FIMMG (Federazione Italiana Medici di Medicina Generale), Milan, Italy. 101UCIBIO, REQUINTE, Faculty of Pharmacy and Competence Center on Active and Healthy Ageing of University of Porto (Porto4Ageing), Porto, Portugal. 102Allergologo, Mexico City, Mexico. 103IMT Mines Alès, Unversité Montpellier, Alès, France. 104Department of Medicine, Nova Southeastern University, Davie, University of Miami Dept of Medicine, Miami, Florida, USA. 105Regional Director Assofarm Campania and Vice President of the Board of Directors of Cofaser, Salerno, Italy. 106ProAR – Nucleo de Excelencia em Asma, Federal University of Bahia, Brasil and WHO GARD Planning Group, Brazil. 107Centre for Respiratory Medicine and Allergy, Institute of Inflammation and Repair, University of Manchester and University Hospital of South Manchester, Manchester, UK. 108Medical Consulting Czarlewski, Levallois, France. 109The Centre for Allergy Research, The Institute of Environmental Medicine, Karolinska Institutet, Stockholm, Sweden. 110Azienda Provinciale per i Servizi Sanitari di Trento (APSS-Trento), Italy. 111Department of Internal Medicine and Allergy Clinic of Professor Polydoro Ernani de São Thiago University Hospital, Federal University of Santa Catarina (UFSC), Florianópolis, Santa Catarina, Brazil. 112Sleep Unit, Department of Neurology, Hôpital Gui-de-Chauliac Montpellier, Inserm U1061, France. 113Department of Dermatology and Allergy, Technische Universität München, Munich, Germany; ZAUM-Center for Allergy and Environment, Helmholtz Center Munich, Technische Universität München, Munich, Germany. 114Allergy Division, Chest Disease Department, University Hospital of Strasbourg, Strasbourg, France. 115EFA European Federation of Allergy and Airways Diseases Patients’ Associations, Brussels, Belgium. 116AQuAS, Barcelna, Spain & EUREGHA, European Regional and Local Health Association, Brussels, Belgium. 117Policlínica Geral do Rio de Janeiro, Rio de Janeiro – Brasil. 118Department of Medicine, Surgery and Dentistry “Scuola Medica Salernitana”, University of Salerno, Salerno, Italy. 119Peercode BV, Geldermalsen, The Netherlands. 120Social workers oordinator, Sorrento, Italy. 121Federal University of the State of Rio de Janeiro, School of Medicine and Surgery, Rio de Janeiro, Brazil. 122Allergology and Immunology Discipline, “Iuliu Hatieganu” University of Medicine and Pharmacy, Cluj-Napoca, Romania. 123Department of Medicine, Division of Clinical Immunology and Allergy, McMaster University, Hamilton, Ontario, Canada. 124Laboratoire de Pharmacologie Respiratoire UPRES EA220, Hôpital Foch, Suresnes, Université Versailles Saint-Quentin, Université Paris Saclay, France. 125Farmacie Dei Golfi Group, Massa Lubrense, Italy. 126Rangueil-Larrey Hospital, Respiratory Diseases Department, Toulouse, France. 127University Clinic of Pulmology and Allergy, Medical Faculty Skopje, Republic of Macedonia. 128Allergologo, Mexico City, Mexico. 129Service de Pneumo-Allergologie, Centre Hospitalo-Universitaire de Béni-Messous, Algiers, Algeria. 130Clinic of infectious, chest diseases, dermatology and allergology, Vilnius University, Vilnius, Lithuania. 131Allergy and Clinical Immunology National Heart and Lung Institute, Imperial College London, UK. 132Guy’s and st Thomas’ NHS Trust, Kings College London, UK. 133Section of Allergy and Immunology, Saint Louis University School of Medicine, Saint Louis, Missouri, USA. 134Pediatric Allergy and Immunology Unit, Children’s Hospital, Ain Shams University, Cairo, Egypt. 135Department of Computing Science, Umeå University, Sweden and Four Computing Oy, Finland. 136Clinic of Children’s Diseases, Faculty of Medicine, Vilnius University, Vilnius, Lithuania. 137University of São Paulo Medical School, Sao Paulo, Brazil. 138Andalusian Agency for Healthcare Quality, Seville, Spain. 139Global Allergy and Asthma Platform GAAPP, Vienna, Austria. 140Division of Allergy, Department of Pediatric Medicine - The Bambino Gesù Children’s Research Hospital Holy see, Rome, Italy. 141Department of Otorhinolaryngology, Academic Medical Centers, Amsterdam, the Netherlands. 142CINTESIS, Center for Research in Health Technologies and Information Systems, Faculdade de Medicina da Universidade do Porto, Porto, Portugal and MEDIDA, Lda, Porto, Portugal. 143Allergist, Reims, France. 144Hospital General Regional 1 “Dr Carlos Mc Gregor Sanchez Navarro” IMSS, Mexico City, Mexico. 145Regional hospital of ISSSTE, Puebla, Mexico. 146National Center for Disease Control and Public Health of Georgia, Tbilisi, Georgia. 147Allergologo, Guadalajara, Mexico. 148Allergy Clinic, National Institute of Respiratory Diseases, Mexico City, Mexico. 149Department of Pulmonary Diseases, Istanbul University-Cerrahpasa, Cerrahpasa Faculty of Medicine, Istambul,Turkey. 150Allergology unit, UHATEM “NIPirogov”, Sofia, Bulgaria. 151Medical University, Faculty of Public Health, Sofia, Bulgaria. 152Allergy and Immunology Division, Clinica Ricardo Palma, Lima, Peru. 153Department of Internal Medicine, section of Allergology, Erasmus MC, Rotterdam, The Netherlands. 154Allergy & Asthma Unit, Hospital San Bernardo Salta, Argentina. 155Allergy Clinic, Hospital Regional del ISSSTE ‘Lic. López Mateos’, Mexico City, Mexico. 156Head and Professor, Centro Regional de Excelencia CONACYT y WAO en Alergia, Asma e Inmunologia, Hospital Universitario, Universidad Autónoma de Nuevo León, Monterrey NL, Mexico. 157Center of Allergy and Immunology, Georgian Association of Allergology and Clinical Immunology, Tbilisi, Georgia. 158Latvian Association of Allergists, Center of Tuberculosis and Lung Diseases, Riga, Latvia. 159Federal District Base Hospital Institute, Brasília, Brazil. 160Institute of Health Policy and Management iBMG, Erasmus University, Rotterdam, The Netherlands. 161University Hospital Olomouc – National eHealth Centre, Czech Republic. 162Immunology and Allergy Division, Clinical Hospital, University of Chile, Santiago, Chile. 163Skin and Allergy Hospital, Helsinki University Hospital, University of Helsinki, Helsinki, Finland. 164Centich: centre d’expertise national des technologies de l’information et de la communication pour l’autonomie, Gérontopôle autonomie longévité des Pays de la Loire, Conseil régional des Pays de la Loire, Centre d’expertise Partenariat Européen d’Innovation pour un vieillissement actif et en bonne santé, Nantes, France. 165Autonomous University of Baja California, Ensenada, Baja California, Mexico. 166Department of Paediatrics and Child Health, University College Cork, Cork, Ireland. 167Hospital General Regional 1 “Dr. Carlos MacGregor Sánchez Navarro” IMSS, Mexico City, Mexico. 168Université Paris-Sud; Service de Pneumologie, Hôpital Bicêtre; Inserm UMR_S999, Le Kremlin Bicêtre, France. 169Dipartimento di medicina, chirurgia e odontoiatria, università di Salerno, Italy. 170Division for Health Innovation, Campania Region and Federico II University Hospital Naples (R&D and DISMET) Naples, Italy. 171Servicio de Alergia e Immunologia, Clinica Santa Isabel, Buenos Aires, Argentina. 172President, Libra Foundation, Buenos Aires, Argentina. 173Medical University of Gdańsk, Department of Allergology, Gdansk, Poland. 174Airway Disease Infection Section, National Heart and Lung Institute, Imperial College; MRC & Asthma UK Centre in Allergic Mechanisms of Asthma, London, UK. 175Dept of Respiratory Medicine, Ghent University Hospital, Ghent, Belgium. 176Hallym University College of Medicine, Hallym University Sacred Heart Hospital, Gyeonggi-do, South Korea. 177Department of Clinical Immunology, Wrocław Medical University, Poland. 178Ukrainina Medical Stomatological Academy, Poltava, Ukraine. 179Pediatric Allergy and Asthma Unit, Hacettepe University School of Medicine, Ankara, Turkey. 180Hacettepe University, School of Medicine, Department of Chest Diseases, Immunology and Allergy Division, Ankara, Turkey. 181Allergy Centre, Tampere University Hospital, Tampere, Finland. 182First Department of Family Medicine, Medical University of Lodz, Poland. 183Institute of Social Medicine, Epidemiology and Health Economics, Charité - Universitätsmedizin Berlin, Berlin, and Institute for Clinical Epidemiology and Biometry, University of Wuerzburg, Germany. 184Department of Medicine, McMaster University, Health Sciences Centre 3V47, West, Hamilton, Ontario, Canada. 185National Research Center, Institute of Immunology, Federal Medicobiological Agency, Laboratory of Molecular immunology, Moscow, Russian Federation. 186GARD Chairman, Geneva, Switzerland. 187Allergy & Asthma Center Westend, Berlin, Germany. 188Center for Rhinology and Allergology, Wiesbaden, Germany. 189Department of Immunology and Allergy, Healthy Ageing Research Center, Medical University of Lodz, Lodz, Poland. 190Children’s Hospital and University of Helsinki, Finland. 191Department of Clinical Science and Education, Södersjukhuset, Karolinska Institutet, Stockholm and Sach´s Children and Youth Hospital, Södersjukhuset, Stockholm, Sweden. 192Faculty of Medicine, Vilnius University, Vilnius, Lithuania. 193Department of Prevention of Envinronmental Hazards and Allergology, Medical University of Warsaw, Poland. 194Center of Excellence in Asthma and Allergy, Médica Sur Clinical Foundation and Hospital, México City, Mexico. 195Presidente CMMC, Milano, Italy. 196Head of the Allergy Department of Pedro de Elizalde Children’s Hospital, Buenos Aires, Argentina. 197University of Medicine and Pharmacy, Hochiminh City, Vietnam. 198Federal University of Bahia, Brazil. 199Sifmed, Milano, Italy. 200State Key Laboratory of Respiratory Diseases, Guangzhou Institute of Respiratory Disease, the First Affiliated Hospital of Guangzhou Medical University, Guangzhou, China. 201Departments of Internal Medicine and Pediatrics (Divisions of Allergy and Immunology), University of Tennessee College of Medicine, Germantown, TN, USA. 202Scottish Centre for Respiratory Research, Cardiovascular & Diabetes Medicine, Medical Research Institute, Ninewells Hospital, University of Dundee, UK. 203Oslo University Hospital, Department of Paediatrics, Oslo, and University of Oslo, Faculty of Medicine, Institute of Clinical Medicine, Oslo, Norway. 204Department of Pulmonary Medicine, CHU Sart-Tilman, and GIGA I3 research group, Liege, Belgium. 205Faculty of Health Sciences and CICS – UBI, Health Sciences Research Centre, University of Beira Interior, Covilhã, Portugal. 206Department of Philosophical, Methodological and Instrumental Disciplines, CUCS, University of Guadalajara, Guadalajara, Mexico. 207Department of Pulmonary Medicine, Rashid Hospital, Dubai, UAE. 208Biomax Informatics AG, Munich, Germany. 209Director General for Health and Social Care, Scottish Government, Edinburgh, UK. 210Department of Respiratory Medicine, University of Bratislava, Bratislava, Slovakia. 211Coimbra Institute for Clinical and Biomedical Research (iCBR), Faculty of Medicine, University of Coimbra, Portugal; Ageing@Coimbra EIP-AHA Reference Site, Coimbra, Portugal. 212Medical center Iskar Ltd Sofia, Bulgaria. 213Department of Medicine (RCSI), Bon Secours Hospital, Glasnevin, Dublin, Ireland. 214Kronikgune, International Centre of Excellence in Chronicity Research Barakaldo, Bizkaia, Spain. 215Division of Clinical Immunology and Allergy, Laboratory of Behavioral Immunology Research, The University of Mississippi Medical Center, Jackson, Mississippi, USA. 216Tobacco Control Research Centre;Iranian Anti Tobacco Association, Tehran, Iran. 217Argentine Association of Allergy and Clinical Immunology, Buenos Aires, Argentina. 218Hospital de Especialidades, Centro Medico Nacional Siglo XXI, Mexico City, Mexico. 219University of Southeast Bahia, Brazil. 220Allergie-Centrum-Charité at the Department of Dermatology and Allergy, Charité - Universitätsmedizin Berlin, Germany. 221Maputo Central Hospital, Department of Paediatrics, Maputo, Mozambique. 222Allergologo, Veracruz, Mexico. 223Sachs’ Children and Youth Hospital, Södersjukhuset, Stockholm and Institute of Environmental Medicine, Karolinska Institutet, Stockholm, Sweden. 224Allergy and Asthma Medical Group and Research Center, San Diego, California, USA. 225CIRFF, Federico II University, Naples, Italy. 226Department of Physiology, CHRU, University Montpellier, Vice President for Research, PhyMedExp, INSERM U1046, CNRS UMR 9214, France. 227Croatian Pulmonary Society. 228National Institute of Pneumology M Nasta, Bucharest, Romania. 229Clinic for Pulmonary Diseases, Clinical Center of Serbia, Faculty of Medicine, University of Belgrade, Serbian Association for Asthma and COPD, Belgrade, Serbia. 230Regione Piemonte, Torino, Italy. 231Col Jardines de Sta Monica, Tlalnepantla, Mexico. 232National Center for Research in Chronic Respiratory Diseases, Tishreen University School of Medicine, Latakia, Syria. 233Department of Public health and health products, Paris Descartes University-Sorbonne Paris Cité, EA 4064 and Paris Municipal Department of social action, childhood, and health, Paris, France. 234Paris municipal Department of social action, childhood, and health, Paris, France. 235Lead Respiratory Physician Mater Dei Hospital Malta, Academic Head of Dept and Professor of Medicine University of Malta, Deputy Dean Faculty of Medicine and Surgery University of Medicine, La Valette, Malta. 236Department of Medical Sciences, Allergy and Clinical Immunology Unit, University of Torino & Mauriziano Hospital, Torino, Italy. 237Instituto de Prevision Social IPS HC, Socia de la SPAAI, Tesorera de la SLAAI, Asuncion, Paraguay. 238Allergy Center, CUF Descobertas Hospital, Lisbon, Portugal. 239Universidade de São Paulo, São Paulo, Brazil. 240Institute of Medical Statistics, and Computational Biology, Medical Faculty, University of Cologne, Germany and CRI-Clinical Research International-Ltd, Hamburg, Germany. 241General Pathology Institute, Faculty of Medicine, University of Coimbra, Portugal; Ageing@Coimbra EIP-AHA Reference Site, Coimbra, Portugal. 242Federal University of Bahia, Brazil. 243Rhinology Unit & Smell Clinic, ENT Department, Hospital Clínic; Clinical & Experimental Respiratory Immunoallergy, IDIBAPS, CIBERES, University of Barcelona, Spain. 244Danish Commitee for Health Education, Copenhagen East, Denmark. 245Food Allergy Referral Centre Veneto Region, Department of Women and Child Health, Padua General University Hospital, Padua, Italy. 246Director, Medical Communications Consultant, MedScript Ltd, Dundalk, Co Louth, Ireland and New Zealand, and Honorary Research Fellow, OPC, Cambridge, UK. 247Johns Hopkins School of Medicine, Baltimore, Maryland, USA. 248General Manager of COFASER - Pharmacy Services Consortium, Salerno, Italy. 249Scientific Centre of Children’s Health under the MoH, Moscow, Russian National Research Medical University named Pirogov, Moscow, Russia. 250Director of Center of Allergy, Immunology and Respiratory Diseases, Santa Fe, Argentina Center for Allergy and Immunology, Santa Fe, Argentina. 251Dept of Otorhinolaryngology, Medical University of Vienna, AKH, Vienna, Austria. 252Hospital of the Hospitaller Brothers in Buda, Budapest, Hungary. 253Die Hautambulanz and Rothhaar study center, Berlin, Germany. 254Neumología y Alergología Infantil, Hospital La Fe, Valencia, Spain. 255Center for Health Technology and Services Research - CINTESIS and Department of Internal Medicine, Centro Hospitalar Sao Joao, Porto, Portugal. 256Caisse d’assurance retraite et de la santé au travail du Languedoc-Roussillon (CARSAT-LR), Montpellier, France. 257Director of Department of Pharmacy of University of Naples Federico II, Naples, Italy. 258ENT Department, University Hospital of Kinshasa, Kinshasa, Congo. 259Department of Allergy, Immunology and Respiratory Medicine, Alfred Hospital and Central Clinical School, Monash University, Melbourne, Victoria, Australia; Department of Immunology, Monash University, Melbourne, Victoria, Australia. 260Medical center “Research expert”, Varna, Bulgaria. 261National Hospital Organization, Tokyo National Hospital, Tokyo, Japan. 262Dept of Otorhinolaryngology, Chiba University Hospital, Chiba, Japan. 263Dept of Otolaryngology, Nippon Medical School, Tokyo, Japan. 264Allergologo, Jalisco, Guadalajara, Mexico. 265Centre Hospitalier Universitaire Pédiatrique Charles de Gaulle, Ouagadougou, Burkina Faso. 266Dept of Comparative Medicine; Messerli Research Institute of the University of Veterinary Medicine and Medical University, Vienna, Austria. 267Department of Immunology and Allergology, Faculty of Medicine and Faculty Hospital in Pilsen, Charles University in Prague, Pilsen, Czech Republic. 268Division of Infection, Immunity & Respiratory Medicine, Royal Manchester Children’s Hospital, University of Manchester, Manchester, UK, and Allergy Department, 2nd Pediatric Clinic, Athens General Children’s Hospital “P&A Kyriakou,” University of Athens, Athens, Greece. 269Department of Allergy and Clinical Immunology, Ajou University School of Medicine, Suwon, South Korea. 270Respiratory Medicine, Department of Medical Sciences, University of Ferrara, Ferrara, Italy. 271Allergy and Respiratory Diseases, Ospedale Policlino San Martino -University of Genoa, Italy. 272Farmacias Holon, Lisbon, Portugal. 273Department of Pediatrics, Nippon Medical School, Tokyo, Japan. 274University of Southern Denmark, Kolding, Denmark. 275Université Grenoble Alpes, Laboratoire HP2, Grenoble, INSERM, U1042 and CHU de Grenoble, France. 276Allergy Unit, CUF-Porto Hospital and Institute; Center for Research in Health Technologies and information systems CINTESIS, Universidade do Porto, Portugal. 277Sociologist, municipality area n33, Sorrento, Italy. 278Center for Rhinology and Allergology, Wiesbaden, Germany. 279Department of Otorhinolaryngology, Head and Neck Surgery, Universitätsmedizin Mannheim, Medical Faculty Mannheim, Heidelberg University, Mannheim, Germany. 280Centre for empowering people and communites, Dublin, UK. 281Conseil Général de l’Economie Ministère de l’Economie, de l’Industrie et du Numérique, Paris, France. 282Société de Pneumologie de Langue Française, Espace francophone de Pneumologie, Paris, France. 283Département de pédiatrie, CHU de Grenoble, Grenoble France. 284Medical School, University of Cyprus, Nicosia, Cyprus. 285Children’s Hospital Srebrnjak, Zagreb, School of Medicine, University J.J. Strossmayer, Osijek, Croatia. 286Karl Landsteiner Institute for Clinical and Experimental Pneumology, Hietzing Hospital, Vienna, Austria. 287University Hospital ‘Sv. Ivan Rilski’”, Sofia, Bulgaria. 288Allergy Diagnostic and Clinical Research Unit, University of Cape Town Lung Institute, Cape Town, South Africa. 289Vice-Presidente of IML, Milano, Italy. 290Centre of Academic Primary Care, Division of Applied Health Sciences, University of Aberdeen, Aberdeen, United Kingdom; Observational and Pragmatic Research Institute, Singapore, Singapore. 291Department of Otorhinolaryngology University of Crete School of Medicine, Heraklion, Greece. 292European Forum for Research and Education in Allergy and Airway Diseases (EUFOREA), Brussels, Belgium. 293Allergologo, cancun quintana roo, Mexico. 294LungenClinic Grosshansdorf, Airway Research Center North, Member of the German Center for Lung Research (DZL), Grosshansdorf, Germany Department of Medicine, Christian Albrechts University, Airway Research Center North, Member of the German Center for Lung Research (DZL), Kiel, Germany. 295Department of Nephrology and Endocrinology, Karolinska University Hospital, Stockholm, Sweden. 296Farmácia São Paio, Vila Nova de Gaia, Porto, Portugal. 297St Vincent’s Hospital and University of Sydney, Sydney, New South Wales, Australia. 298Allergologo, Mexico City, Mexico. 299Serviço de Pneumologia-Hosp das Clinicas UFPE-EBSERH, Recife, Brazil. 300Universidade Federal de São Paulo, São Paulo, Brazil. 301Centre of Pneumology, Coimbra University Hospital, Portugal. 302Polibienestar Research Institute, University of Valencia, Valencia, Spain. 303Pediatric Allergy and Clinical Immunology, Hospital Angeles Pedregal, Mexico City, Mexico. 304Getafe University Hospital Department of Geriatrics, Madrid, Spain. 305Association Asthme et Allergie, Paris, France. 306Universidade Federal do Rio de Janeiro, Rio de Janeiro, Brazil. 307Primary Care Respiratory Research Unit Institutode Investigación Sanitaria de Palma IdisPa, Palma de Mallorca, Spain. 308Allergy Unit, Presidio Columbus, Rome, Catholic University of Sacred Heart, Rome and IRCCS Oasi Maria SS, Troina, Italy. 309Hospital General, Mexico City, Mexico. 310Regione Piemonte, Torino, Italy. 311Medical University of Graz, Department of Internal Medicine, Graz, Austria. 312Serviço de Imunoalergologia Hospital da Luz, Lisboa, Portugal. 313Hospital de Clinicas, University of Parana, Brazil. 314Division of Allergy Asthma and Clinical Immunology, Emek Medical Center, Afula, Israel. 315Honorary Clinical Research Fellow, Allergy and Respiratory Research Group, The University of Edinburgh, Edinburgh, UK. 316Showa University School of Medicine, Tokyo, Japan. 317Association of Finnish Pharmacies, Helsinki, Finland. 318Allergy and Clinical Immunology Department, Centro Médico-Docente la, Trinidad and Clínica El Avila, Caracas, Venezuela. 319Faculty of Medicine, Autnonous University of Madrid, Spain. 320The Royal National TNE Hospital, University College London, UK. 321DIBIMIS, University of Palermo, Italy. 322Allergy Unit, Department of Dermatology, University Hospital of Zurich, Zürich, Switzerland. 323Asthma Reference Center, Escola Superior de Ciencias da Santa Casa de Misericordia de Vitoria - Esperito Santo, Brazil. 324The Usher Institute of Population Health Sciences and Informatics, The University of Edinburgh, Edinburgh, UK. 325Department of Pediatrics & Child Health, Department of Immunology, Faculty of Medicine, University of Manitoba, Winnipeg, Manitoba, Canada. 326INSERM, Université Grenoble Alpes, IAB, U 1209, Team of Environmental Epidemiology applied to Reproduction and Respiratory Health, Université Joseph Fourier, Grenoble, France. 327Sociedad Paraguaya de Alergia Asma e Inmunologı´a, Paraguay. 328Division of Allergy, Clinical Immunology and Rheumatology, Department of Pediatrics, Federal University of São Paulo, São Paulo, Brazil. 329European Health Futures Forum (EHFF), Dromahair, Ireland. 330ENT, Aachen, Germany. 331Kyrgyzstan National Centre of Cardiology and Internal medicine, Euro-Asian respiratory Society, Bishkek, Kyrgyzstan. 332University Hospital Olomouc, Czech Republic. 333Department of Paediatric and Adolescent medicine, University Hospital of North Norway, Tromsø, Paediatric Research Group, Deptarment of Clinical Medicine, Faculty of Health Sciences, UiT The Arctic University of Norway, Tromsø, Norway. 334Presidente, IML (Lombardy Medical Initiative), Bergamo, Italy. 335Pulmonary Division, Heart Institute (InCor), Hospital da Clinicas da Faculdade de Medicina da Universidade de Sao Paulo, Sao Paulo, Brazil. 336Public Health Institute of Vilnius University, Vilnius, Lithuania. 337Universidade Federal do Estado do Rio de Janeiro, Rio de Janeiro, Brazil. 338RNSA (Réseau National de Surveillance Aérobiologique), Brussieu, France. 339The Hospital for Sick Children, Dalla Lana School of Public Health, University of Toronto, Canada. 340Imunoalergologia, Centro Hospitalar Universitário de Coimbra and Faculty of Medicine, University of Coimbra, Portugal. 341Department of ENT, Medical University of Graz, Austria. 342Campania Region, Division on Pharmacy and devices policy, Naples, Italy. 343Department of Respiratory Medicine, Hvidovre Hospital & University of Copenhagen, Denmark. 344Universidade Federal dos Pampas, Uruguaiana, Brazil. 345Division of Immunopathology, Department of Pathophysiology and Allergy Research, Center for Pathophysiology, Infectiology and Immunology, Medical University of Vienna, Vienna, Austria. 346Pneumology and Allergy Department CIBERES and Clinical & Experimental Respiratory Immunoallergy, IDIBAPS, University of Barcelona, Spain. 347Vilnius University Institute of Clinical Medicine, Clinic of Children’s Diseases, and Institute of Health Sciences, Department of Public Health, Vilnius, Lithuania; European Academy of Paediatrics (EAP/UEMS-SP), Brussels, Belgium. 348Department of Lung Diseases and Clinical Immunology Allergology, University of Turku and Terveystalo allergy clinic, Turku, Finland. 349PELyon; HESPER 7425, Health Services and Performance Resarch - Université Claude Bernard Lyon, France. 350Immunology and Allergy Unit, Department of Medicine Solna, Karolinska Institutet and University Hospital, Stockholm. 351Department of Chest Medicine, Centre Hospitalier Universitaire UCL Namur, Université Catholique de Louvain, Yvoir, Belgium. 352University of Bari Medical School, Unit of Geriatric Immunoallergology, Bari, Italy. 353Pulmonary Unit, Department of Medical Specialties, Arcispedale SMaria Nuova/IRCCS, AUSL di Reggio Emilia, Italy. 354FILHA, Finnish Lung Association, Helsinki, Finland. 355Pulmonary Environmental Epidemiology Unit, CNR Institute of Clinical Physiology, Pisa, Italy; and CNR Institute of Biomedicine and Molecular Immunology “A Monroy”, Palermo, Italy. 356Medical University, Plovdiv, Bulgaria, Department of Otorhinolaryngology, Plovdiv, Bulgaria. 357Sotiria Hospital, Athens, Greece. 358Dept of Otorhinolaryngology, Universitätsklinikum Düsseldorf, Germany. 359Asthma UK, Mansell street, London, UK. 360Nova Southeastern University, Fort Lauderdale, Florida, USA. 361Department of Otolaryngology, Yong Loo Lin School of Medicine, National University of Singapore, Singapore, Singapore. 362Department of Medicine, Clinical Immunology and Allergy, McMaster University, Hamilton, Ontario, Canada. 363Division of Immunodermatology and Allergy Research, Department of Dermatology and Allergy, Hannover Medical School, Hannover, Germany. 364Department of Medicine Solna, Immunology and Allergy Unit, Karolinska Institutet and Department of ENT diseases, Karolinska University Hospital, Stockholm, Sweden. 365Eshelman School of Pharmacy, University of North Carolina, Chapel Hill, NC, USA. 366International Primary Care Respiratory Group IPCRG, Aberdeen, Scotland. 367Bradford Institute for Health Research, Bradford Royal Infirmary, Bradford, UK. 368Allergologyst - Medical College of Medical Faculty, Thracian University, Stara Zagora, Bulgaria. 369Department of Research, Olmsted Medical Center, Rochester, Minnesota, USA. 370Cyprus International Institute for Environmental & Public Health in Association with Harvard School of Public Health, Cyprus University of Technology, Limassol, Cyprus; Department of Pediatrics, Hospital “Archbishop Makarios III”, Nicosia, Cyprus. 371Celal Bayar University Department of Pulmonology, Manisa, Turkey. 372The Allergy and Asthma Institute, Islamabad, Pakistan. 373Department of Paediatrics and Child Health, Red Cross Children’s Hospital, and MRC Unit on Child & Adolescent Health, University of Cape Town, Cape Town, South Africa. 374Department of Otolaryngology Head and Neck Surgery, Beijing TongRen Hospital and Beijing Institute of Otolaryngology, Beijing, China. 375Universidad Católica de Córdoba, Córdoba, Argentina. 376University Clinic of Respiratory and Allergic Diseases, Golnik, Slovenia. 377Gesundheitsregion KölnBonn - HRCB Projekt GmbH, Kohln, Germany. 378Akershus University Hospital, Department of Otorhinolaryngology, Akershus, Norway. 379Chief of Staff, the Northern Health Science Alliance (NHSA) and Director and Founder of Northern Health Matters Ltd, Manchester, UK. 380President of Kazakhstan Association of Allergology and Clinical Immunology, Department of Allergology and Clinical Immunology of the Kazakh National Medical University, Kazakhstan. 381Division of Respiratory and Allergic Diseases,Hospital ‘A Cardarelli’, University of Naples Federico II, Naples, Italy.
Competing interests
Dr. Ansotegui reports personal fees from Mundipharma, Roxall, Sanofi, MSD, Faes Farma, Hikma, UCB, Astra Zeneca, outside the submitted work. Dr. Bosnic-Anticevich reports grants from TEVA, personal fees from TEVA, Boehringer Ingelheim, AstraZeneca, Sanofi, Mylan, outside the submitted work. Dr Bousquet reports personal fees and others from Chiesi, Cipla, Hikma, Menarini, Mundipharma, Mylan, Novartis, Sanofi-Aventis, Takeda, Teva, Uriach, others from Kyomed, outside the submitted work. Dr. Boulet reports and Disclosure of potential conflicts of interest—last 3 years research grants for participation to multicentre studies, AstraZeneca, Boston Scientific, GlaxoSmithKline, Hoffman La Roche, Novartis, Ono Pharma, Sanofi, Takeda.Support for research projects introduced by the investigator AstraZeneca, Boehringer-Ingelheim, GlaxoSmithKline, Merck, Takeda. Consulting and advisory boards Astra Zeneca, Novartis, Methapharm. Royalties Co-author of “Up-To-Date” (occupational asthma). Nonprofit grants for production of educational materials AstraZeneca, Boehringer-Ingelheim, GlaxoSmithKline, Merck Frosst, Novartis. Conference fees AstraZeneca, GlaxoSmithKline, Merck, Novartis. Support for participation in conferences and meetings Novartis, Takeda. Other participations Past president and Member of the Canadian Thoracic Society Respiratory Guidelines Committee; Chair of the Board of Directors of the Global Initiative for Asthma (GINA). Chair of Global Initiative for Asthma (GINA) Guidelines Dissemination and Implementation Committee; Laval University Chair on Knowledge Transfer, Prevention and Education in Respiratory and Cardiovascular Health; Member of scientific committees for the American College of Chest Physicians, American Thoracic Society, European Respiratory Society and the World Allergy Organization;1st Vice-President of the Global Asthma Organization “InterAsma”. Dr. Casale reports grants and non-financial support from Stallergenes, outside the submitted work. Dr. Cruz reports grants and personal fees from GlaxoSmithKline, personal fees from Boehrinher Ingelheim, AstraZeneca, Novartis, Merk, Sharp & Dohme, MEDA Pharma, EUROFARMA, Sanofi Aventis, outside the submitted work. Dr. Ebisawa reports personal fees from DBV Technologies, Mylan EPD maruho, Shionogi & CO., Ltd., Kyorin Pharmaceutical Co., Ltd., Thermofisher Diagnostics, Pfizer, Beyer, Nippon Chemifar, Takeda Pharmaceutical Co., Ltd., MSD, outside the submitted work. Dr. Ivancevich reports personal fees from Euro Farma Argentina, Faes Farma, non-financial support from Laboratorios Casasco, outside the submitted work. Dr. Haahtela reports personal fees from Mundipharma, Novartis, and Orion Pharma, outside the submitted work. Dr. Klimek reports grants and personal fees from ALK Abelló, Denmark, Novartis, Switzerland, Allergopharma, Germany, Bionorica, Germany, GSK, Great Britain, Lofarma, Italy, personal fees from MEDA, Sweden, Boehringer Ingelheim, Germany, grants from Biomay, Austria, HAL, Netherlands, LETI, Spain, Roxall, Germany, Bencard, Great Britain, outside the submitted work. V.KV has received payment for consultancy from GSK and for lectures from StallergensGreer, Berlin-CHemie and sponsorship from MYLAN for in the following proffesional training: ARIA masterclass in allergic rhinitis participation. Dr. Larenas Linnemann reports personal fees from GSK, Astrazeneca, MEDA, Boehringer Ingelheim, Novartis, Grunenthal, UCB, Amstrong, Siegfried, DBV Technologies, MSD, Pfizer., grants from Sanofi, Astrazeneca, Novartis, UCB, GSK, TEVA, Chiesi, Boehringer Ingelheim, outside the submitted work. Dr. Mösges reports personal fees from ALK, grants from ASIT biotech, Leti, BitopAG, Hulka, Ursapharm, Optima; personal fees from allergopharma, Nuvo, Meda, Friulchem, Hexal, Servier, Bayer, Johnson&Johnson, Klosterfrau, GSK, MSD, FAES, Stada, UCB, Allergy Therapeutics; grants and personal fees from Bencard, Stallergenes; grants, personal fees and non-financial support from Lofarma; non-financial support from Roxall, Atmos, Bionorica, Otonomy, Ferrero; personal fees and non-financial support from Novartis; Dr. Okamoto reports personal fees from Eizai Co., Ltd., Shionogi Co., Ltd., Torii Co., Ltd., GSK, MSD, Kyowa Co., Ltd., grants and personal fees from Kyorin Co., Ltd., Tiho Co., Ltd., grants from Yakuruto Co., Ltd., Yamada Bee Farm, outside the submitted work. Dr. Papadopoulos reports grants from Gerolymatos, personal fees from Hal Allergy B.V., Novartis Pharma AG, Menarini, Hal Allergy B.V., outside the submitted work. Dr. Pépin reports grants from AIR LIQUIDE FOUNDATION, AGIR à dom, ASTRA ZENECA, FISHER & PAYKEL, MUTUALIA, PHILIPS, RESMED, VITALAIRE, other from AGIR à dom, ASTRA ZENECA, BOEHRINGER INGELHEIM, JAZZ PHARMACEUTICAL, NIGHT BALANCE, PHILIPS, RESMED, SEFAM, outside the submitted work. Dr. Pfaar reports grants and personal fees from ALK-Abelló, Allergopharma Stallergenes Greer, HAL Allergy Holding B.V./HAL Allergie GmbH, Bencard Allergie GmbH/Allergy Therapeutics, Lofarma, grants from Biomay, ASIT Biotech Tools S.A, Laboratorios LETI/LETI Pharma, Anergis S.A., grants from Nuvo, Circassia, Glaxo Smith Kline, personal fees from Novartis Pharma, MEDA Pharma, Mobile Chamber Experts (a GA2LEN Partner), Pohl-Boskamp, Indoor Biotechnologies, grants from, outside the submitted work. Dr. Todo-Bom reports grants and personal fees from Novartis, Mundipharma, GSK Teva Pharma, personal fees from AstraZeneca, grants from Leti, outside the submitted work. Dr. Tsiligianni reports advisory boards from Boehringer Ingelheim and Novartis and a grant from GSK, outside the submitted work. Dr. Wallace reports and Indicates that she is the co-chair of the Joint Task Force on Practice Parameters, a task force composed of 12 members of the American Academy of Allergy, Asthma, and Immunology and the American College of Allergy, Asthma, and Immunology. Dr. Waserman reports other from CSL Behring, Shire, AstraZeneca,Teva, Meda, Merck, outside the submitted work. Dr. Zuberbier reports and Organizational affiliations: Commitee member: WHO-Initiative “Allergic Rhinitis and Its Impact on Asthma” (ARIA). Member of the Board: German Society for Allergy and Clinical Immunology (DGAKI). Head: European Centre for Allergy Research Foundation (ECARF) Secretary General: Global Allergy and Asthma European Network (GA2LEN). Member: Committee on Allergy Diagnosis and Molecular Allergology, World Allergy Organization (WAO).
Availability of data and materials
Not applicable.
Consent for publication
Not applicable.
Ethics approval and consent to participate
Not applicable.
Funding
FMC VIA LR.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Consortia
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Bousquet, J., Bedbrook, A., Czarlewski, W. et al. Guidance to 2018 good practice: ARIA digitally-enabled, integrated, person-centred care for rhinitis and asthma. Clin Transl Allergy 9, 16 (2019). https://doi.org/10.1186/s13601-019-0252-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13601-019-0252-0