Abstract
Background
The physiological effects of high-flow nasal cannula O2 therapy (HFNC) have been evaluated mainly in patients with hypoxemic respiratory failure. In this study, we compared the effects of HFNC and conventional low-flow O2 therapy on the neuroventilatory drive and work of breathing postextubation in patients with a background of chronic obstructive pulmonary disease (COPD) who had received mechanical ventilation for hypercapnic respiratory failure.
Methods
This was a single center, unblinded, cross-over study on 14 postextubation COPD patients who were recovering from an episode of acute hypercapnic respiratory failure of various etiologies. After extubation, each patient received two 1-h periods of HFNC (HFNC1 and HFNC2) alternated with 1 h of conventional low-flow O2 therapy via a face mask. The inspiratory fraction of oxygen was titrated to achieve an arterial O2 saturation target of 88–92%. Gas exchange, breathing pattern, neuroventilatory drive (electrical diaphragmatic activity (EAdi)) and work of breathing (inspiratory trans-diaphragmatic pressure-time product per minute (PTPDI/min)) were recorded.
Results
EAdi peak increased from a mean (±SD) of 15.4 ± 6.4 to 23.6 ± 10.5 μV switching from HFNC1 to conventional O2, and then returned to 15.2 ± 6.4 μV during HFNC2 (conventional O2: p < 0.05 versus HFNC1 and HFNC2). Similarly, the PTPDI/min increased from 135 ± 60 to 211 ± 70 cmH2O/s/min, and then decreased again during HFNC2 to 132 ± 56 (conventional O2: p < 0.05 versus HFNC1 and HFNC2).
Conclusions
In patients with COPD, the application of HFNC postextubation significantly decreased the neuroventilatory drive and work of breathing compared with conventional O2 therapy.
Similar content being viewed by others
Background
High-flow nasal cannula oxygen therapy (HFNC) consists of a totally conditioned, warmed, and humidified air/oxygen blend through a wide-bore nasal cannula at a flow rate between 20 and 60 L/min [1]. Compared with the ‘conventional’ oxygen therapy devices, which deliver gas at 5–20 L/min (conventional O2), during HFNC the tracheal inspiratory oxygen fraction (FiO2) is more predictable [2] and the mucociliary function is better preserved [3]. In addition, HFNC generates a positive airway pressure (between 2 and 8 cmH2O at the pharyngeal level) which resembles positive end-expiratory pressure (PEEP) and is proportional to the administered gas flow rate and varies with the patient breathing pattern (i.e., breathing with the mouth open or closed) [4]. Furthermore, HFNC results in a significant, flow-dependent ‘CO2 wash out effect’ of the nasopharyngeal space which decreases the anatomical dead space ventilation and therefore the CO2 rebreathing [5]. It seems likely that the overall impact of HFNC on the respiratory function results from the synergistic interaction of the mechanisms described above as well as other, more subtle, and as yet incompletely understood mechanisms [6].
Since its introduction, HFNC has been applied to treat patients with hypoxemic respiratory failure [2, 7,8,9] and to prevent reintubation in patients at risk of extubation failure [10,11,12]. In these patients, compared with conventional O2 therapy, HFNC improves oxygenation and decreases the work of breathing (WOB) [10, 13]. Studies in patients with stable chronic obstructive pulmonary disease (COPD) in a home-care setting suggest favorable effects on the WOB and gas exchange [14,15,16]. However, far less known are the physiological effects of HFNC on neuroventilatory drive and WOB in patients with COPD in the critical care setting.
The electric activity of the diaphragm (EAdi) is a ‘processed’ diaphragmatic electromyography signal recorded through an array of electrode pairs mounted on the wall of a nasogastric feeding tube [17]. The EAdi is proportional to the intensity of the electrical stimuli directed to the diaphragm, i.e., the neuroventilatory drive [18,19,20]. Recently, Bellani and coworkers demonstrated that EAdi can be used to estimate the instantaneous WOB [21].
In this physiological study, we administered HFNC and conventional O2 therapy via a face mask postextubation in patients with a background of COPD who had received mechanical ventilation for hypercapnic respiratory failure from various etiologies. The hypothesis of this study was that, in these patients, HFNC decreases the neuroventilatory drive and WOB compared with conventional O2 therapy.
Methods
Patient selection
We enrolled patients with a background of moderate-severe COPD who were admitted to the intensive care unit (ICU) at the University Hospital of Bari (Italy) between December 2015 and December 2016 and required mechanical ventilation for acute hypercapnic ventilatory failure of various etiologies. The diagnosis of COPD was made by three experts, including one pulmonologist (PP) and two intensivists (SG and TS), and was graded in accordance with the Global Initiative for Chronic Obstructive Lung Disease (GOLD) criteria (http://goldcopd.org/gold-2017-global-strategy-diagnosis-management-prevention-copd/). For each patient, the three assessors reviewed the clinical history, medical records, smoking history, frequency of exacerbation, spirometry data, radiological findings, physical examination, and measurement of static intrinsic PEEP on admission to ICU. The GOLD spirometry criterion for the diagnosis of COPD was a postbronchodilator forced expiratory volume in 1 s/forced vital capacity (FEV1/FVC) < 0.7. Based on the FEV1 impairment, the severity of COPD was defined as follows: GOLD stage 1 (mild), FEV1 ≤ 80% predicted; GOLD stage 2 (moderate), 50% ≤ FEV1 < 80% predicted; GOLD stage 3 (severe) 30% ≤ FEV1 < 50% predicted; GOLD stage 4 (very severe), FEV1 < 30% predicted. The local ethics committee approved the study protocol and informed consent requirements were met according to local regulations (Azienda Ospedaliero-Universitaria Policlinico di Bari Ethic Committee, protocol number: 885/C.E., May 2014).
Patients ready for extubation, as assessed by the treating clinician, were eligible for the study. According to our clinical protocol, the criteria defining readiness for extubation were: a) resolution or improvement of the condition leading to acute respiratory failure; b) set PEEP lower than 6 cmH2O and FiO2 lower than 0.6 with a PaO2/FiO2 ratio greater than 150 mmHg; c) arterial pH > 7.35; c) Richmond Agitation Sedation Scale (RASS) between 0 and −1 [22], with no sedation or with a continuous infusion of dexmedetomidine (0.1–1.4 μg/kg/h); and d) ability to trigger the ventilator, i.e., to decrease pressure airway opening (PAO) > 3 cmH2O during a brief (5–10 s) end-expiratory occlusion test. Other criteria included normothermia and hemodynamic stability unsupported by vasopressors or inotropes, but we allowed low-dose dobutamine (< 5 μg/kg/min) or low-dose dopamine (< 3 μg/kg/min). All patients underwent a 30-min spontaneous breathing trial (SBT) consisting of pressure support ventilation at 5 cmH2O with a PEEP of 5 cmH2O. Patients were eligible to be included in the study after a successful SBT.
Exclusion criteria were: age < 18 years; < 48 h of invasive mechanical ventilation; presence of a tracheostomy; contraindications to the insertion of the EAdi catheter (e.g., recent upper gastrointestinal surgery, esophageal varices, esophageal trauma); and concomitant neurological or neuromuscular pathologies and/or known phrenic nerve dysfunction. We also excluded patients showing paradoxical abdominal movements or the use of accessory inspiratory muscles. The reason for the latter exclusion criterion is because the correlation between work of breathing and EAdi is valid only if the diaphragm contributes to approximately 75% of the overall WOB [23], and the calculation of WOB from EAdi may be inaccurate if the work carried out by the accessory inspiratory muscles is more than that of the diaphragm.
Before extubation, all patients were ventilated with a Servo-i ventilator (Maquet, Getinge group Critical Care, Solna, Sweden) equipped with the EAdi software (Maquet, Getinge group Critical Care, Solna, Sweden). At the beginning of the study, the standard feeding nasogastric tube was replaced with a 16-Fr, 125-cm EAdi catheter (Maquet, Getinge group Critical Care, Solna, Sweden) unless an EAdi catheter was already in place. The EAdi catheter was first positioned based on the corrected nose-earlobe-xyphoid distance formula, in accordance with the manufacturer’s instructions [24]. Its position was subsequently adjusted using the ventilator EAdi catheter position tool (Servo-i ventilator NAVA software) [24].
Measurements
Patients were studied in the semirecumbent position. The EAdi signal was collected from the RS232 ventilator port at a sampling rate of 100 Hz (NAVA tracker software, Maquet Getinge group Critical Care, Solna, Sweden) and stored in a personal computer. The NAVA tracker files were subsequently converted and analyzed using the ICULab software package (Kleistek Engineering, Bari, Italy).
The inspiratory EAdi peak (EAdiPEAK), the integral of the inspiratory EAdi deflection over time (EAdiPTP), the slope of the EAdi from the beginning of inspiration to the peak (EAdiSLOPE), the respiratory rate (RR), and the neural inspiratory time (TiNEUR) were measured from the EAdi waveform [25].
Given that all patients were breathing spontaneously, tidal volume (VT) was not measured to avoid any modification in breathing pattern caused by the measurement apparatus.
The pressure generated by the diaphragm (i.e., the trans-diaphragmatic pressure, PDI) throughout the inspiratory phase was calculated from the EAdi signal as described by Bellani and coworkers [21]. Briefly, we calculated first the diaphragmatic neuromuscular efficiency (NME), i.e., the ratio between the negative peak in airway opening pressure (PAO) during a spontaneous inspiratory effort (recorded during a brief end-expiratory occlusion lasting 5–10 s) and the corresponding peak in the EAdi curve [19, 26, 27]. Since the fall in PAO during a spontaneous inspiratory effort against the occluded airways is, by definition, equal to the corresponding fall in esophageal pressure (PES) [28, 29], the NME is an index of diaphragmatic neuromechanical coupling, and accordingly can be used as a factor to convert the EAdi into PDI (PDI = EAdi × NME) [21]. The inspiratory PDI pressure-time product per breath (PTPDI/b) was calculated as the area under the PDI signal. The inspiratory PDI pressure-time product per minute (PTPDI/min) was calculated as:
Study protocol
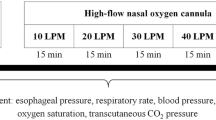
At the beginning of the study, 5–10 min before extubation, the NME was calculated after a brief (5–10 s) end-expiratory occlusion. Immediately after extubation, patients underwent a cross-over protocol with an ON–OFF–ON design, alternating HFNC with conventional O2 delivered through a face mask (i.e., HFNC1 – conventional O2 therapy – HFNC2), with each phase lasting for 1 h (Fig. 1).
Study protocol timeline. ABG arterial blood gas, Conventional O2 period of conventional low flow oxygen therapy through a non-occlusive face mask, EAdi diaphragm electrical activity, HFNC1 first period of high flow nasal cannula oxygen therapy, HFNC2 second period of high flow nasal cannula oxygen therapy
The HFNC was administered through the AIRVO™ 2 system (Fisher & Paykel Healthcare, Auckland, New Zealand) and specific medium/large nasal prongs to fit the size of the nostrils (Fisher & Paykel Healthcare, Auckland, New Zealand). The system allows for the administration of humidified and warmed gas flow (10–60 L/min in the adult configuration). The gas flow was titrated upwards at 5–10 L/min steps starting from 20 L/min, up to the highest flow compatible with patient comfort (maximum allowed flow 60 L/min) [30]. The FiO2 was titrated to achieve an hemoglobin oxygen saturation (SaO2) target of 88–92%. The temperature of the heated humidifier was set at 37 °C.
In keeping with previous studies [13], the conventional O2 therapy was administered through a standard nonocclusive oxygen facial mask connected to a O2/air mixer (0–20 L/min). The mask gas flow was set to 10 L/min in all the patients. The FiO2 in the mask flow was titrated to achieve the 88–92% SaO2 target.
At the end of each study period, arterial blood gas analysis was performed. EAdi and PDI parameters were calculated from the digital recordings of EAdi curve on the last 30 min of each step.
Extubation success was defined as the ability of the patient to breathe spontaneously without signs of respiratory distress and without the requirement of rescue noninvasive ventilation (NIV) for 48 h postextubation. Signs of respiratory distress were defined as: a) paradoxical abdominal movement, use of accessory respiratory muscles, or evidence of respiratory muscle fatigue; b) cardiovascular instability (systolic blood pressure (SBP) > 160 or < 90 mmHg or a 20% change from the pre-SBT values; heart rate (HR) > 120 or < 60 beats/min or 20% change from the pre-SBT values; c) arterial desaturation with SaO2 < 88%), hypercapnia, and respiratory acidosis with pH < 7.35; and d) retention of secretions.
Statistical analysis
The power analysis indicated a sample size of 14 patients with a power of 0.8, a significance level of 0.05 and an expected effect size of 0.25. The effect size refers to the magnitude of variability in an outcome explained by the intervention divided by the total variability of the same outcome measure. We have hypothesized that the variability explained by the study condition in EAdiPEAK had to be at least 5% of total variability that corresponds approximatively to a medium effect size of 0.25. A sphericity correction of 0.8 and a correlation of 0.8 were assumed from pilot measurements. The sample size was determined using the software GPower version 3.1.9.2.
Continuous quantitative variables were summarized as mean ± standard deviation (SD) if normally distributed or as median and interquartile range if non-normally distributed. Comparisons were performed with analysis of variance (ANOVA) for repeated measures or Friedman’s test as appropriate. A p value < 0.05 was considered statistically significant, except in the multiple comparison procedure, when the p value was adjusted. The analyses were carried out with SAS software v.9.4 for Windows PC.
Results
The CONSORT diagram of our study (Fig. 2) shows that 20 out of the 57 COPD patients admitted to our unit during the study period were eligible for the study and 16 were enrolled. Two patients were excluded from the final analysis because of technical difficulties in recording the EAdi signal. Therefore, the final number of patients was 14. Patient demographics and clinical characteristics are shown in Table 1.
Five patients (31.5%) failed the initial extubation attempt and were reintubated. Patients who required reintubation were similar to the ones who were successfully extubated in terms of age, reason for ICU admission (COPD exacerbation vs other causes), days of mechanical ventilation, COPD severity (based on FEV1, FEV1/FVC ratio, GOLD stage, Simplified Acute Physiology Score (SAPS) II on admission, and Sequential Organ Failure Assessment (SOFA) score; Additional file 1).
Four patients (25%) died after a mean (±SD) ICU length of stay of 25.2 ± 2.6 days. The cause of death for two patients was septic shock and multiple organ failure, while the other two died of right cardiac failure and cardiogenic shock.
Breathing pattern and gas exchange
Table 2 shows the breathing pattern and gas exchange recorded for each of the three experimental conditions. To achieve the oxygenation target (SaO2 between 88 and 92%), the applied FiO2 during HFNC1 and HFNC2 periods was 0.46 ± 0.1 and 0.46 ± 0.12, respectively (p = not significant), whereas during the conventional (mask) O2 period it was 0.80 ± 0.19. However, a comparison between the FiO2 during HFNC and conventional O2 is not meaningful given the difference in the delivered gas flow rates. Indeed, the FiO2 delivered during conventional O2 therapy is almost certainly overestimated since the patient’s inspiratory flow is higher than the mask flow (10 L/min) and, therefore, the difference between patient inspiratory flow and the mask flow is provided by room air. This also makes any comparison between the PaO2/FiO2 in the different experimental conditions inappropriate. Respiratory rate, TiNEUR, arterial PCO2, and pH remained similar throughout the study (Table 2).
Neuroventilatory drive and work of breathing
Figure 3 shows EAdi traces obtained at the end of each study period in three representative patients. In all patients, the neuroventilatory drive, expressed by the EAdi waveforms, clearly increased between HFNC1 and conventional O2 therapy and decreased again when the HFNC was reinstituted (HFNC2). Table 3 shows that neuroventilatory drive (EAdiPEAK) and work of breathing (PTPDI/b and PTPDI/min) increased significantly while on conventional O2 therapy, and decreased again when HFNC was reinstituted. Figure 4 shows the individual changes in these parameters during the three study periods.
Experimental record showing the diaphragm electrical activity (EAdi) in the three experimental conditions in three representative patients. Conventional O2 period of conventional low flow oxygen therapy through a non-occlusive face mask, HFNC1 first period of high flow nasal cannula oxygen therapy, HFNC2 second period of high flow nasal cannula oxygen therapy
Trend of the neuroventilatory drive, as expressed by the diaphragm electrical activity peak EAdiPEAK, and of work of breathing, as expressed by the inspiratory PDI pressure-time product per breath (PTPDI/b) and per minute (PTPDI/min). *Significant difference compared to the HFNC1 period (ANOVA with Bonferroni correction); §Significant difference compared to the HFNC2 period (ANOVA with Bonferroni correction). Conventional O2 period of conventional low flow oxygen therapy through a non-occlusive face mask, HFNC1 first period of high flow nasal cannula oxygen therapy, HFNC2 second period of high flow nasal cannula oxygen therapy
We were not able to find any significant differences between patients that were reintubated and patients successfully extubated in terms of EAdi parameters or work of breathing during each experimental condition (Additional file 2). For the same parameters, there were no significant differences between patients admitted for hypercapnic respiratory failure due to an exacerbation of COPD and patients with a background of COPD but whose hypercapnic respiratory failure was due to other precipitating causes (Additional file 3).
Discussion
This study shows that postextubation HFNC significantly decreases the neuroventilatory drive and work of breathing in patients with COPD who had received mechanical ventilation for hypercapnic respiratory failure due to various etiologies.
The EAdi reflects the rate of discharge of the phrenic nerve and therefore it is a measure of the neuroventilatory drive [17,18,19,20, 31, 32]. Thus, our data clearly show that HFNC decreases the neuroventilatory drive (EAdiPEAK and EAdiSLOPE) compared with conventional O2 therapy. Neuroventilatory drive and work of breathing are key factors for the weaning process and an excessive respiratory drive predicts weaning failure [26, 32]. In fact, a high ventilatory drive may be associated either with excessive mechanical load posed on the inspiratory muscles, diaphragm weakness, or inappropriately high activation of the respiratory centers due to pain, fever, anxiety, and acidosis [32]. In a mixed population of critically ill patients, Liu and coworkers found that an EAdiPEAK lower than 15–20 μV during a spontaneous breathing trial (T-tube) was associated with weaning success [26]. Similar results were recently obtained in two other studies by Dres et al. [33] and Barwing et al. [34]. In our study, we found that the EAdiPEAK was below this threshold in most of the patients during both HFNC periods (Fig. 4), while it was on average 1.5-times higher than this threshold during conventional O2. Accordingly, considering that COPD patients are intrinsically at risk of weaning failure [35], our results are potentially clinically relevant.
Although the work of breathing is proportional to the neuroventilatory drive, its absolute value depends on the ability of the respiratory muscles to convert the electrical stimuli into mechanical contraction (electromechanical coupling) [18, 32]. We measured the work of breathing in terms of PTPDI per breath and per minute, a well-known index of respiratory muscle oxygen consumption (Table 3 and Fig. 4). According to physiological studies in mixed populations of critically ill patients, an ‘acceptable’ PTPDI/min is between 50 and 150 cmH2O/s/min [36, 37]. The PTPDI/min was in this range in 64.3% of our patients (i.e., 9/14) both during HFNC1 and HFNC2 periods, whereas the PTPDI/min was above this acceptable range in 78.6% of patients during the conventional O2 period (i.e., 11/14) (Fig. 3).
According to the 2017 European Respiratory Society–American Thoracic Society (ERS/ATS) guidelines [38], COPD patients benefit from noninvasive ventilation to prevent reintubation. Therefore, it would have been of interest to compare the physiological effects of HFNC and NIV in our patients. However, at the time of the study, postextubation preventative NIV was not applied on a routine basis in our institution. Interestingly, a recent study by Hernandez et al. showed that HFNC is noninferior to NIV in preventing acute postextubation respiratory failure in patients at “high risk” of postextubation respiratory failure, including patients older than 65 years or those with heart failure, moderate to severe COPD, an Acute Physiology and Chronic Health Evaluation (APACHE) II score higher than 12 on extubation day, a body mass index of more than 30, those with airway patency problems, and, finally, patients with difficult or prolonged weaning [11].
Further studies are needed to assess the beneficial mechanisms of HFNC in COPD patients. We speculate that two mechanisms are of particular relevance: a) the HFNC “PEEP” effect [14], that may have counterbalanced the flow-limited intrinsic positive end-expiratory pressure (PEEPi), and b) the “CO2 wash-out” effect of the anatomical dead space [5] that may have decreased the diaphragmatic workload. The better preservation of the mucociliary function as compared with conventional O2 therapy may have been an adjunctive mechanism [3], but we believe that it was less important since the cross-over periods were relatively short.
In hypoxemic patients, Mauri et al. [39] and Maggiore et al. [10] found that HFNC significantly decreased RR compared with conventional O2 therapy. Mauri estimated the VT through electrical impedance tomography (EIT) and found that it remained stable. In contrast, in our COPD patients, the RR remained unchanged (Table 2), while we have no data on VT since patients were breathing spontaneously and we wanted to avoid any modification in breathing pattern caused by the measurement apparatus. However, the VT likely increased since animal studies show that VT is proportional to the electrical activity of the diaphragm during unassisted spontaneous breathing [40]. Based on this hypothesis, in our patients, the response to HFNC removal during the conventional O2 period would have been similar to the physiological response to a sudden increase in respiratory workload during to CO2 rebreathing, i.e., to maintain the RR as constant and to increase the VT [41, 42]. The different impact of HFNC on RR between our study and those of Mauri and Maggiore could be explained by the different background of the respiratory failure of the studied patients (hypoxemic versus hypercapnic).
In our study, similar to previous studies [13], we used a standard, nonocclusive oxygen facial mask with a fixed gas flow of 10 L/min in all the patients during the conventional O2 study step (see the Methods section). Hence, in our patients the peak inspiratory flow was very likely greater than the mask gas flow and therefore the true fraction of inhaled oxygen was lower than the one provided by the mask. The “Venturi Mask” is a high-flow oxygen delivery system that provides 35–45 L/min of a mixture of oxygen and air with a delivered FiO2 of 0.24–0.6 by taking advantage of the Bernoulli principle [43]. By using a Venturi Mask instead of the standard mask, it is possible that we would have better matched the patient’s inspiratory flow during the conventional O2 study period. One could also speculate that a higher mask flow could have other effects in terms of CO2 washout from the mask or from the airways, but we are not aware of studies comparing Venturi mask and HFNC.
We must acknowledge some study limitations. First, we studied a population of patients with COPD that was admitted to the ICU with hypercapnic ventilatory failure due to various etiologies (Table 1). Only 8/14 (57%) of COPD patients were admitted because of a COPD exacerbation, while the other 6 (43%) received mechanical ventilation for postoperative ventilatory failure. In this regard, our population could be deemed as heterogenous. However, we point out that: 1) our study was conducted in the postextubation phase when the primary reason for the acute respiratory failure had resolved or at least improved (see Methods); and 2) all our patients had moderate to very severe COPD according to the GOLD classification. Second, we were not able to measure several respiratory parameters during spontaneous breathing (VT, PEEPi, inspiratory flow) that could have provided us with a more complete interpretation of the treatment effect. However, our study was conducted in spontaneously breathing patients and we sought to avoid any modification in breathing pattern caused by the measurement apparatus. Third, we measured the work of breathing based on a method recently validated by Bellani and coworkers [21], but the correlation between work of breathing and EAdi may be misleading if the contraction of the accessory inspiratory muscles is dominant compared with the diaphragmatic contraction. Indeed, the estimation of work of breathing from EAdi assumes that the diaphragm contributes approximately 75% to the overall WOB (as occurs in normal conditions) [23]. However, we assessed all patients for signs of paradoxical abdominal motion and use of accessory inspiratory muscles throughout the study. In addition, the method described by Bellani et al. assumes a linear relationship between EAdi and PDI at different lung volumes based on a close correlation at different lung volumes between the PDI obtained from the esophageal pressure and the PDI obtained through the formula EAdi × NME [21]. However, Bellani et al. studied patients ventilated with different levels of pressure support ventilation (PSV) and neurally adjusted ventilatory assist (NAVA) while we studied spontaneously breathing patients. Of note, other authors showed a nonlinearity between diaphragmatic efficiency and lung volumes, but only for intense diaphragmatic contractions [19]. Fourth, we studied a small patient number that, while appropriate for a physiologically oriented study, weakens any speculation on the clinical outcomes (e.g., ICU and hospital length of stay and reintubation rate).
Conclusions
In conclusion, we found that HFNC, as compared with conventional O2 therapy, significantly decreases the neuroventilatory drive and the work of breathing in patients with COPD recovering from an episode of acute respiratory failure after a planned extubation.
Abbreviations
- COPD:
-
Chronic obstructive pulmonary disease
- EAdi:
-
Electric activity of the diaphragm
- FEV1 :
-
Forced expiratory volume in 1 s
- FiO2 :
-
Inspiratory oxygen fraction
- FVC:
-
Forced vital capacity
- GOLD:
-
Global Initiative for Chronic Lung Disease
- HFNC:
-
High-flow nasal cannula oxygen therapy
- ICU:
-
Intensive care unit
- NIV:
-
Noninvasive ventilation
- NME:
-
Neuromuscular efficiency
- PAO :
-
Pressure airway opening
- PEEP:
-
Positive end-expiratory pressure
- PEEPi:
-
Intrinsic positive end-expiratory pressure
- PTPDI/b :
-
Pressure-time product per breath
- PTPDI/min :
-
Pressure-time product per minute
- RR:
-
Respiratory rate
- SaO2 :
-
Arterial hemoglobin oxygen saturation
- SBP:
-
Systolic blood pressure
- SBT:
-
Spontaneous breathing trial
- TiNEUR :
-
Neural inspiratory time
- VT:
-
Tidal volume
- WOB:
-
Work of breathing
References
Papazian L, Corley A, Hess D, Fraser JF, Frat JP, Guitton C, Jaber S, Maggiore SM, Nava S, Rello J, et al. Use of high-flow nasal cannula oxygenation in ICU adults: a narrative review. Intensive Care Med. 2016;42(9):1336–49.
Sztrymf B, Messika J, Bertrand F, Hurel D, Leon R, Dreyfuss D, Ricard JD. Beneficial effects of humidified high flow nasal oxygen in critical care patients: a prospective pilot study. Intensive Care Med. 2011;37(11):1780–6.
Spoletini G, Alotaibi M, Blasi F, Hill NS. Heated humidified high-flow nasal oxygen in adults: mechanisms of action and clinical implications. Chest. 2015;148(1):253–61.
Parke RL, McGuinness SP. Pressures delivered by nasal high flow oxygen during all phases of the respiratory cycle. Respir Care. 2013;58(10):1621–4.
Moller W, Feng S, Domanski U, Franke KJ, Celik G, Bartenstein P, Becker S, Meyer G, Schmid O, Eickelberg O, et al. Nasal high flow reduces dead space. J Appl Physiol (1985). 2017;122(1):191–7.
Goligher EC, Slutsky AS. Not just oxygen? Mechanisms of benefit from high-flow nasal cannula in hypoxemic respiratory failure. Am J Respir Crit Care Med. 2017;195(9):1128–31.
Messika J, Ben Ahmed K, Gaudry S, Miguel-Montanes R, Rafat C, Sztrymf B, Dreyfuss D, Ricard JD. Use of high-flow nasal cannula oxygen therapy in subjects with ARDS: a 1-year observational study. Respir Care. 2015;60(2):162–9.
Nagata K, Morimoto T, Fujimoto D, Otoshi T, Nakagawa A, Otsuka K, Seo R, Atsumi T, Tomii K. Efficacy of high-flow nasal cannula therapy in acute hypoxemic respiratory failure: decreased use of mechanical ventilation. Respir Care. 2015;60(10):1390–6.
Frat JP, Thille AW, Mercat A, Girault C, Ragot S, Perbet S, Prat G, Boulain T, Morawiec E, Cottereau A, et al. High-flow oxygen through nasal cannula in acute hypoxemic respiratory failure. N Engl J Med. 2015;372(23):2185–96.
Maggiore SM, Idone FA, Vaschetto R, Festa R, Cataldo A, Antonicelli F, Montini L, De Gaetano A, Navalesi P, Antonelli M. Nasal high-flow versus Venturi mask oxygen therapy after extubation. Effects on oxygenation, comfort, and clinical outcome. Am J Respir Crit Care Med. 2014;190(3):282–8.
Hernandez G, Vaquero C, Colinas L, Cuena R, Gonzalez P, Canabal A, Sanchez S, Rodriguez ML, Villasclaras A, Fernandez R. Effect of postextubation high-flow nasal cannula vs noninvasive ventilation on reintubation and postextubation respiratory failure in high-risk patients: a randomized clinical trial. JAMA. 2016;316(15):1565–74.
Hernandez G, Vaquero C, Gonzalez P, Subira C, Frutos-Vivar F, Rialp G, Laborda C, Colinas L, Cuena R, Fernandez R. Effect of postextubation high-flow nasal cannula vs conventional oxygen therapy on reintubation in low-risk patients: a randomized clinical trial. JAMA. 2016;315(13):1354–61.
Mauri T, Turrini C, Eronia N, Grasselli G, Volta CA, Bellani G, Pesenti A. Physiologic effects of high-flow nasal cannula in acute hypoxemic respiratory failure. Am J Respir Crit Care Med. 2017;195(9):1207–15.
Fraser JF, Spooner AJ, Dunster KR, Anstey CM, Corley A. Nasal high flow oxygen therapy in patients with COPD reduces respiratory rate and tissue carbon dioxide while increasing tidal and end-expiratory lung volumes: a randomised crossover trial. Thorax. 2016;71(8):759–61.
Pisani L, Fasano L, Corcione N, Comellini V, Musti MA, Brandao M, Bottone D, Calderini E, Navalesi P, Nava S. Change in pulmonary mechanics and the effect on breathing pattern of high flow oxygen therapy in stable hypercapnic COPD. Thorax. 2017;72(4):373–5.
Pisani L, Vega ML. Use of nasal high flow in stable COPD: rationale and physiology. COPD. 2017;14(3):346–50.
Sinderby C, Navalesi P, Beck J, Skrobik Y, Comtois N, Friberg S, Gottfried SB, Lindstrom L. Neural control of mechanical ventilation in respiratory failure. Nat Med. 1999;5(12):1433–6.
Doorduin J, van Hees HW, van der Hoeven JG, Heunks LM. Monitoring of the respiratory muscles in the critically ill. Am J Respir Crit Care Med. 2013;187(1):20–7.
Beck J, Sinderby C, Lindstrom L, Grassino A. Effects of lung volume on diaphragm EMG signal strength during voluntary contractions. J Appl Physiol (1985). 1998;85(3):1123–34.
Beck J, Sinderby C, Lindstrom L, Grassino A. Influence of bipolar esophageal electrode positioning on measurements of human crural diaphragm electromyogram. J Appl Physiol (1985). 1996;81(3):1434–49.
Bellani G, Mauri T, Coppadoro A, Grasselli G, Patroniti N, Spadaro S, Sala V, Foti G, Pesenti A. Estimation of patient's inspiratory effort from the electrical activity of the diaphragm. Crit Care Med. 2013;41(6):1483–91.
Sessler CN, Gosnell MS, Grap MJ, Brophy GM, O'Neal PV, Keane KA, Tesoro EP, Elswick RK. The Richmond agitation-sedation scale: validity and reliability in adult intensive care unit patients. Am J Respir Crit Care Med. 2002;166(10):1338–44.
Tobin MJ. Respiratory monitoring in the intensive care unit. Am Rev Respir Dis. 1988;138(6):1625–42.
Barwing J, Ambold M, Linden N, Quintel M, Moerer O. Evaluation of the catheter positioning for neurally adjusted ventilatory assist. Intensive Care Med. 2009;35(10):1809–14.
Di Mussi R, Spadaro S, Mirabella L, Volta CA, Serio G, Staffieri F, Dambrosio M, Cinnella G, Bruno F, Grasso S. Impact of prolonged assisted ventilation on diaphragmatic efficiency: NAVA versus PSV. Crit Care. 2016;20(1):1.
Liu L, Liu H, Yang Y, Huang Y, Liu S, Beck J, Slutsky AS, Sinderby C, Qiu H. Neuroventilatory efficiency and extubation readiness in critically ill patients. Crit Care. 2012;16(4):R143.
Schmidt M, Kindler F, Cecchini J, Poitou T, Morawiec E, Persichini R, Similowski T, Demoule A. Neurally adjusted ventilatory assist and proportional assist ventilation both improve patient-ventilator interaction. Crit Care. 2015;19:56.
Hedenstierna G. Esophageal pressure: benefit and limitations. Minerva Anestesiol. 2012;78(8):959–66.
Baydur A, Behrakis PK, Zin WA, Jaeger M, Milic-Emili J. A simple method for assessing the validity of the esophageal balloon technique. Am Rev Respir Dis. 1982;126(5):788–91.
Mauri T, Alban L, Turrini C, Cambiaghi B, Carlesso E, Taccone P, Bottino N, Lissoni A, Spadaro S, Volta CA, et al. Optimum support by high-flow nasal cannula in acute hypoxemic respiratory failure: effects of increasing flow rates. Intensive Care Med. 2017;43(10):1453–63.
Beck J, Gottfried SB, Navalesi P, Skrobik Y, Comtois N, Rossini M, Sinderby C. Electrical activity of the diaphragm during pressure support ventilation in acute respiratory failure. Am J Respir Crit Care Med. 2001;164(3):419–24.
Telias I, Brochard L, Goligher EC. Is my patient’s respiratory drive (too) high? Intensive Care Med. 2018;
Dres M, Schmidt M, Ferre A, Mayaux J, Similowski T, Demoule A. Diaphragm electromyographic activity as a predictor of weaning failure. Intensive Care Med. 2012;38(12):2017–25.
Barwing J, Pedroni C, Olgemoller U, Quintel M, Moerer O. Electrical activity of the diaphragm (EAdi) as a monitoring parameter in difficult weaning from respirator: a pilot study. Crit Care. 2013;17(4):R182.
Thille AW, Harrois A, Schortgen F, Brun-Buisson C, Brochard L. Outcomes of extubation failure in medical intensive care unit patients. Crit Care Med. 2011;39(12):2612–8.
Sassoon CS, Light RW, Lodia R, Sieck GC, Mahutte CK. Pressure-time product during continuous positive airway pressure, pressure support ventilation, and T-piece during weaning from mechanical ventilation. Am Rev Respir Dis. 1991;143(3):469–75.
Mancebo J, Isabey D, Lorino H, Lofaso F, Lemaire F, Brochard L. Comparative effects of pressure support ventilation and intermittent positive pressure breathing (IPPB) in non-intubated healthy subjects. Eur Respir J. 1995;8(11):1901–9.
Rochwerg B, Brochard L, Elliott MW, Hess D, Hill NS, Nava S, Navalesi P, Antonelli M, Brozek J, Conti G, et al. Official ERS/ATS clinical practice guidelines: noninvasive ventilation for acute respiratory failure. Eur Respir J. 2017;50(2):1602426-46.
Mauri T, Langer T, Zanella A, Grasselli G, Pesenti A. Extremely high transpulmonary pressure in a spontaneously breathing patient with early severe ARDS on ECMO. Intensive Care Med. 2016;42(12):2101–3.
Lourenco RV, Cherniack NS, Malm JR, Fishman AP. Nervous output from the respiratory center during obstructed breathing. J Appl Physiol. 1966;21(2):527–33.
Yan S, Lichros I, Zakynthinos S, Macklem PT. Effect of diaphragmatic fatigue on control of respiratory muscles and ventilation during CO2 rebreathing. J Appl Physiol (1985). 1993;75(3):1364–70.
Bradley GW, von Euler C, Marttila I, Roos B. Steady state effects of CO2 and temperature on the relationship between lung volume and inspiratory duration (Hering-Breuer threshold curve). Acta Physiol Scand. 1974;92(3):351–63.
Bateman NT, Leach RM. ABC of oxygen. Acute oxygen therapy. BMJ. 1998;317(7161):798–801.
Acknowledgements
We would like to thank Dr. Joanna Brown for reviewing the final manuscript.
Funding
No specific funding was received for this study.
Availability of data and materials
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Author information
Authors and Affiliations
Contributions
SG, RDm, and SS contributed to the design of the conception and design of the study. RDm, SS, TS, and PP were responsible for patient screening and enrollment. PT performed the statistical analysis. SG, CAV, FB, LC, and FS analyzed the data and wrote the manuscript. All authors contributed to interpretation of the data. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval was obtained by the local ethics committee (Azienda Ospedaliero-Universitaria Policlinico di Bari Ethic Committee, protocol number: 885/C.E., May 2014). All patients or their relatives provided informed consent to participate.
Consent for publication
Not applicable.
Competing interests
SG has given talks in symposia organized by Getinge Critical Care (Solna Sweden), Estor Critical Care (Mirandola, Italy), and Fisher and Paykel (Auckland, New Zealand), and has received compensation for related travel and accommodation fees. He declares no other relationship or activities that could appear to have influence the submitted work. The remaining authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional files
Additional file 1:
Independent sample t tests. Comparison between patients who required reintubation and patients who were successfully extubated in terms of age, reason for ICU admission (COPD exacerbation versus other causes), days of mechanical ventilation, COPD severity (based on FEV1, FEV1/FVC ratio, GOLD stage, SAPS II on admission, and SOFA score). (DOCX 26 kb)
Additional file 2:
Independent sample t tests. Comparison between patients who required reintubation and patients who were successfully extubated in terms of EAdi parameters or work of breathing during each experimental condition. (DOCX 42 kb)
Additional file 3:
Independent sample t tests. Comparison between patients admitted for hypercapnic respiratory failure due to an exacerbation of COPD and patients with a background of COPD but whose hypercapnic respiratory failure was due to other precipitating causes in terms of EAdi parameters or work of breathing during each experimental condition. (DOCX 60 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Di mussi, R., Spadaro, S., Stripoli, T. et al. High-flow nasal cannula oxygen therapy decreases postextubation neuroventilatory drive and work of breathing in patients with chronic obstructive pulmonary disease. Crit Care 22, 180 (2018). https://doi.org/10.1186/s13054-018-2107-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13054-018-2107-9