Abstract
Background
Recent studies have challenged radical procedures for less extensive surgery in selected patients with early-stage cervical cancer at low risk of parametrial invasion. Our objective was to identify a subgroup of patients at low risk of parametrial invasion among women having undergone surgical treatment.
Methods
Data of 1447 patients with cervical cancer treated between 1996 and 2016 were extracted from maintained databases of 10 French University hospitals. Patients with early-stage (IA2–IIA) disease treated by radical surgery including hysterectomy and trachelectomy, were selected for further analysis. The Kaplan–Meier method was used to estimate the survival distribution. A Cox proportional hazards model including all the parameters statistically significant in univariate analysis, was used to account for the influence of multiple variables.
Results
Out of the 263 patients included for analysis, on final pathology analysis 28 (10.6%) had parametrial invasion and 235 (89.4%) did not. Factors significantly associated with parametrial invasion on multivariate analysis were: age > 65 years, tumor > 30 mm in diameter measured by MRI, lymphovascular space invasion (LVSI) on pathologic analysis. Among the 235 patients with negative pelvic lymph nodes, parametrial disease was seen in only 7.6% compared with 30.8% of those with positive pelvic nodes (p < 0.001). In a subgroup of patients presenting tumors < 30 mm, negative pelvic status and no LVSI, the risk of parametrial invasion fell to 0.6% (1/173 patients).
Conclusion
Our analysis suggests that there is a subgroup of patients at very low risk of parametrial invasion, potentially eligible for less radical procedures.
Similar content being viewed by others
Background
The success of prevention campaigns and widespread screening for cervical cancer has led to more women being diagnosed with early-stage disease [1, 2]. Current recommendations for surgical management of patients with early-stage cervical cancer include modified radical hysterectomy and pelvic lymph node dissection (PLND). Women desiring to preserve fertility can be treated with radical trachelectomy associated with PLND [3, 4]. The rationale for “radical” surgery is the extent to which paracervical tissue is involved and the risk of lymphatic disease. Indeed, cervical cancer has a lymphatic spread pattern and the parametrium is a key area of the cervical plexus drainage area [5, 6].
Recent studies have challenged these radical procedures for less extensive surgery in selected patients [7, 8] with a low risk of parametrial invasion. This is important as extensive lymphadenectomy and parametrectomy are the main causes of postoperative complications [9,10,11]. Serious urinary and rectal dysfunction, impairing patients’ quality of life, have been reported after parametrial resection [12,13,14,15]. Analysis of the nerve and lymphatic pathways have shown that the technique of radical hysterectomy could change to spare high density nerve regions [16, 17], and recent studies have even suggested there might be a subgroup of patients that could be treated without radical surgery [18,19,20,21]. The crucial issue remains of which criteria could best select patients who might benefit from less radical surgery without jeopardizing oncological results.
The main objective of our study was to identify a subgroup of patients with a very low risk of parametrial invasion among women who had been surgically treated for early-stage cervical cancer.
Methods
Patients included
We conducted a retrospective analysis of patients treated in 10 French institutions (Creteil University hospital, Tenon University Hospital, Reims University Hospital, Dijon cancer center, Lille University hospital and Lille cancer center, Tours University hospital, Bondy University hospital, Rennes University hospital, Marseille Public hospital North). The research protocol was approved by the Institutional Review Board (IRB) of the French College of Obstetrics and Gynaecology (CEROG 2016—GYN—0502).
The maintained databases included all patients treated with radical surgery (i.e., trachelectomy or hysterectomy) for early-stage cervical cancer between January 1996 and December 2016. Early-stage cervical cancer was defined as disease stages IA2–IIA clinically, and on preoperative pelvic magnetic resonance imaging (MRI) according to the latest 2009 International Federation of Gynecology and Obstetrics (FIGO) classification [22].
The following patient characteristics were extracted from their medical charts: age, BMI, medical and surgical history, surgical procedure, FIGO stage, final pathological analysis, treatment received.
Inclusion criteria:
-
Stage IA2–IIA, based on our review of the literature, as this choice was made by many reports including prospective studies evaluating less radical surgery in this subgroup of patients.
-
Patients treated by type II–III hysterectomy as described by Piver-Rutledge-Smith in 1974 [23] or type B-C according to the Querleu and Morrow classification [24].
-
Patients diagnosed with stage IA2–IB1 desiring to preserve their fertility, treated with radical trachelectomy in accordance with the latest European guidelines [3].
Exclusion criteria:
-
Preoperative FIGO stage > IIA.
-
Non-radical surgery, i.e., without parametrectomy.
-
Preoperative brachytherapy.
-
Patients with missing histologic data such as parametrial involvement, lymphovascular space invasion (LVSI), and the size of the tumor.
Initial management
All patients underwent clinical examination. Disease stage was initially assessed by preoperative pelvic MRI including an evaluation of tumor size. Indeed, this exam is more powerful than clinical examination to precisely assess parametrial invasion, the presence of extra uterine disease and tumor size.
Patients with FIGO stage IA2–IIA2 underwent bilateral pelvic lymph node dissection and radical hysterectomy or radical trachelectomy. Patients with preoperative brachytherapy—if the tumor size was > 2 cm or if there was LVSI—were excluded. Similarly, patients with peroperative diagnosis of metastatic pelvic nodes were also excluded as they did not undergo radical hysterectomy but subsequent surgical paraaortic staging. Operative complications were evaluated using the Clavien–Dindo classification. Complications of grade III (requiring surgical, endoscopic or radiological intervention) or more were considered severe.
Parametrial invasion as well as the main tumor characteristics were determined by pathologic analysis. Parametrium involvement was defined as the presence of tumor cells in or beyond the parametrial vessels. Each of the participating centers conducted pathologic analysis according to local practice. None of the centers in our cohort performed ultra-staging.
The decision to perform adjuvant therapy, such as vaginal brachytherapy or concomitant chemoradiotherapy and brachytherapy, was made by multidisciplinary committees according to the national guidelines at the time the patient was treated [3].
Follow-up protocols included gynecological examination every 3 months for 2 years and then every 6 months for 2 years. Computed tomography (CT) or positron emission tomography—computed tomography (PET/CT) scans were performed systematically when clinically indicated. Recurrences were diagnosed either by biopsy or with an imaging exam. Disease-free survival (DFS) and overall survival (OS) were calculated from the date of the initial surgery.
Statistical analysis
Databases were managed using Excel (Microsoft Corporation, Redmond, WA, USA) and statistical analyses were performed using R software (3.3.1 version, available online). Statistical analysis was based on the Student’s t test for continuous variable and the χ2 test or Fisher’s exact test for categorical variables. The Kaplan–Meier method was used to estimate the survival distribution. Comparisons of survival were made using the log rank test. A logistic regression model including all the parameters statistically significant in univariate analysis, was used to account for the influence of multiple variables. Values of p < 0.05 were considered to denote significant differences. Optimal cut off for age and size were obtained by a minimal p value approach. The performance of the model was quantified with respect to discrimination and calibration. An internal validation of the model was performed with a bootstrapping method to obtain relatively unbiased estimates.
Results
Main characteristics of the patients included
Between 1996 and 2016, 1446 patients were diagnosed and treated for a cervical cancer in the participating centers. Of these, 263 met our inclusion criteria and had data available for analysis as shown in the patient flow chart (Fig. 1). Mean follow up of the patients was 45.6 months (QI 17.4–64.0). Twenty-eight patients (10.6%) had parametrial invasion on final pathology analysis.
The preoperative clinical factors of the patients are presented in Table 1. Patients with parametrial invasion and those without were statistically different for most of the characteristics studied. In particular, patients with parametrial invasion were significantly older (p < 0.001), more often menopausal (p < 0.001), had a higher BMI (p < 0.01), and had more often disease staged IB2 or IIA (p < 0.001).
Table 2 summarizes the surgical management of patients with and without parametrial invasion. Patients with parametrial involvement were more likely to have undergone open surgery (p = 0.03) and less likely to have had surgical staging (p = 0.02). Patients with parametrial involvement also had significantly more peroperative complications [6 (21.4%) vs. 19 (8.1%), p = 0.03]. The rate of postoperative complications was similar in the two groups [6 (21.4%) vs. 41 (17.4%), p = 0.6] as was the rate of severe postoperative complications [3 (10.7%) vs. 12 (5.1%), p = 0.2]. Additional file 1 displays surgical outcomes by FIGO stages.
The main pathologic features on final analysis were statistically different in the patients with and without parametrial involvement (Table 2). More specifically, patients with parametrial involvement had larger tumors (p < 0.001), and were more likely to have lymph node involvement (p < 0.001) and LVSI (p < 0.001).
Survival analysis
Patients with parametrial involvement had a lower OS (p = 0.08) (Fig. 2a) and DFS (p = 0.153) (Fig. 2b), without reaching statistical significance. All recurrences in patients with parametrial invasion (four patients) occurred within 3 years compared to 17/22 (77.3%) of those without parametrial invasion. Two of the patients with parametrial invasion who experienced recurrence had initial positive lymph nodes.
Kaplan–Meier curve for disease free survival (a) and overall survival (b) in patients with and without parametrial invasion on final pathologic analysis. Continued line is for patients without parametrial involvement. Dotted line is for patients with parametrial involvement (for DFS and OS, p = 0.153 and p = 0.08, respectively)
During follow up, three (10.7%) and 10 (4.25%) patients died in the group of patients with and without parametrial involvement, respectively. Mean OS was 41.4 (IQ 18–67) and 45.6 (IQ 17–62) months in patients with and without parametrial involvement, respectively.
Predictive factors
An age at diagnosis of 65 years and tumor size of > 30 mm on preoperative MRI were the most relevant thresholds for predicting parametrial invasion, using an optimal threshold approach. In multivariate analysis, three clinicopathologic factors remained significantly associated with parametrial invasion: age > 65 years, a tumor > 30 mm and LVSI (Table 3). Our model showed an area under the receiver operating characteristic curve (AUC) of 0.95 with good calibration: the mean absolute error in predicted probabilities was 1.9%, and the maximum error was 11.8% with an unreliability index U < 0.0001 (Additional files 2, 3).
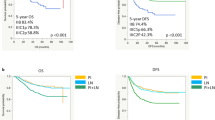
Parametrial disease was seen in 7.6% of the 235 patients with negative pelvic lymph nodes, compared with 30.8% of the 28 with positive pelvic nodes. The risk of parametrial invasion fell to 0.6% (1/173 patients) in the subgroup of women with negative pelvic nodes, tumors < 30 mm and no LVSI (Fig. 3). There was no significant difference in further subgroup analysis for DFS (p = 0.124) (Fig. 4a) or OS (p = 0.417) (Fig. 4b).
Kaplan–Meier curve for disease free survival (a) and overall survival (b) in patients stratified by tumor size (< or > 3 cm) and by LVSI status (positive or negative). In black, patients with tumors < 3 cm and without LVSI. In red, patients with tumors < 3 cm and LVSI. In green, patients with tumors > 3 cm and without LVSI. In blue, patients with tumors > 3 cm and LVSI
Discussion
We report a large multicenter cohort of patients with early-stage cervical cancer treated with radical surgery and pelvic lymphadenectomy. Patients with parametrial invasion represented 11.9% of the patients included. Patients younger than 65 with tumors of less than 30 mm and without LVSI had a very low risk of parametrial invasion, especially in the node-negative group (0.6%).
Despite many studies addressing this issue, the role of parametrectomy in early-stage cervical cancer management remains controversial, mainly because of the morbidity associated with radical surgery. Urinary, sexual and anorectal dysfunction are well known direct consequences of parametrial resection [10, 12, 13, 25]. Reducing morbidity in radical surgery means either modifying the surgical technique or improving selection of the most eligible patients.
Pathology studies describing the tumor spread have failed to identify predictable patterns of dissemination with concomitant invasion of the medial and lateral parametria [26, 27]. Benedetti–Panici reported that parametrial invasion was through direct extension in 37% of cases, by lymph node metastases in 59% and LVSI in 52% [28]. These findings underline the difficulty of reducing the surgical extent of the resection without running the risk of leaving residual tumor tissue in situ.
Some authors have reported techniques leading to less morbidity, such as the “nerve sparing” hysterectomy described by Fuji et al. [29] or the “Laparoscopic Neuro-Navigation (LANN) technique” by Possover et al. [30]. However, even though these techniques show a benefit in terms of quality of life, they are difficult to perform in small volume centers and the learning curve limits their applicability in current practice, even if surgery of cervix cancer has to be performed by gynecologist oncologist in order to ensure its quality.
Another promising approach for predicting parametrial invasion is the nomogram. Nomograms have recently been developed to assess an individual probability of a certain event with validated indications in other gynecological malignancies [31, 32]. Kong et al. recently described such a nomogram for patients with stage IB disease [33]. Their model includes four parameters combining biological and imaging criteria to accurately predict parametrial invasion preoperatively. However, the model was developed in a population with a surprisingly high rate of parametrial invasion (64/298, 21.5%) when compared with what has been described in other studies including ours [34, 35]; especially as they only included patients with supposedly stage IB disease. Furthermore, the criteria they included are also somewhat surprising regarding the classic prognostic factors such as LVSI or tumor size, and may prove difficult to use in daily practice. Finally, external validation is required to test it.
Another way to reduce morbidity without compromising oncologic prognosis is through a better selection of patients that would benefit from radical surgery [36]. It would seem that there is a subgroup of patients among those with early-stage disease who are at very low risk of parametrial invasion. Most of the reports retain a tumor size < 2 cm, negative pelvic lymph nodes and the absence of LVSI, but there is currently a lack of consensus about these criteria [18, 37, 38]. It has been reported that elderly women have a higher incidence of LVSI and parametrial invasion even when their tumors are < 2–3 cm in size [20, 39]. This emphasizes the importance of including an age-based criterion to correctly identify patients at very low risk of parametrial invasion and is consistent with our findings.
Benedetti–Panici et al. identified parametrial lymph nodes in more than 90% of patients treated with radical hysterectomy for stage IIA or less cervical cancer [28]. Consequently, most authors concluded that the parametrium was the first “stop” on the tumor pathway to metastases. The development of the sentinel lymph node (SLN) procedure in early-stage cervical cancer, after being developed with great success in many other gynecological cancers, might challenge this model. Indeed, a recent study by Salvo et al. [40] found that only 4% of the SLNs were located within the parametrium. These results have been confirmed by others [41] with most SLNs being found in iliac or obturator locations. In our study, lymph node invasion was not significantly associated with parametrial invasion on multivariate analysis which is in line with the description of the SLN locations. Moreover, around half of the recurrences in patients with early-stage cancer after radical surgery are distant [42, 43]. This highlights our poor understanding of the factors associated with local and distant control and that we are still unable to properly identify patients who will benefit from surgery without experiencing high morbidity. In all fairness, we could suppose that generalization of the SLN approach would reduce morbidity to some extent as pelvic and paraaortic lymphadenectomy are partly responsible for the morbidity of radical surgery [44, 45].
From a patient’s perspective, it is of paramount importance to be able to determine the actual risk of parametrial invasion before performing morbid surgery. As many studies are currently evaluating less radical surgery in patients with early-stage cervical cancer [46], we feel these patients would highly benefit from a two-step approach: initial surgical staging and conization to assess LVSI and pelvic lymph node invasion followed by either a simple or radical hysterectomy/trachelectomy. The emergence of preoperative vaginal brachytherapy and neoadjuvant chemotherapy should increase the benefit harvested from such an approach by reducing the number of patients with parametrial invasion. Uzan et al. [47] reported that only one patient out of 162 had parametrial residual disease after preoperative vaginal brachytherapy. Similar results have been reported by other teams [48, 49]. Neoadjuvant chemotherapy response could also improve our selection of patients who might truly benefit from radical surgery as reported in a small cohort of 21 patients [50]. Unfortunately, our data were insufficient to further confirm these results.
Retrospective studies are often perceived as providing low-level evidence mostly because of missing data and patient selection bias. However, a major strength of our study lies in its multicentric nature and in the size of our cohort that could scarcely be reached using a prospective randomized trial, especially since parametrial invasion remains a rare event in early-stage cervical cancer. Our findings are perfectly in line with what has been reported elsewhere further confirming the need to adapt our management for early-stage cervical cancer patients by reconsidering the need for radical procedures for some patients. Finally, we eagerly await the results of three ongoing randomized controlled trials evaluating less radical surgery in patients with early-stage cervical cancer, such as the SHAPE and MD Anderson Centre studies [51,52,53].
Conclusions
Our analysis suggests that there is a subgroup of patients with early-stage cervical cancer who do not benefit from radical surgery. These patients might be eligible for a two-step surgical approach consisting of initial nodal staging and conization prior to a radical procedure. This could reduce morbidity without jeopardizing oncological safety.
References
Quinn MA, Benedet JL, Odicino F, et al. Carcinoma of the cervix uteri. FIGO 26th Annual Report on the results of treatment in gynecological cancer. Int J Gynaecol Obstet. 2006;95(Suppl 1):S43–103.
Greggi S, Scaffa C. Surgical management of early cervical cancer: the shape of future studies. Curr Oncol Rep. 2012;14(6):527–34.
Marth C, Landoni F, Mahner S, McCormack M, Gonzalez-Martin A, Colombo N. Cervical cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2017;28(suppl_4):iv72–83.
Koh W-J, Greer BE, Abu-Rustum NR, Apte SM, Campos SM, Cho KR, et al. Cervical cancer, Version 2.2015. J Natl Compr Canc Netw. 2015;13(4):395–404.
Lichtenegger W, Anderhuber F, Ralph G. Operative anatomy and technique of radical parametrial resection in the surgical treatment of cervical cancer. Baillieres Clin Obstet Gynaecol. 1988;2(4):841–56.
Rob L, Strnad P, Robova H, et al. Study of lymphatic mapping and sentinel node identification in early stage cervical cancer. Gynecol Oncol. 2005;98(2):281–8.
Landoni F, Maneo A, Cormio G, et al. Class II versus class III radical hysterectomy in stage IB–IIA cervical cancer: a prospective randomized study. Gynecol Oncol. 2001;80(1):3–12.
Bouchard-Fortier G, Reade CJ, Covens A. Non-radical surgery for small early-stage cervical cancer. Is it time? Gynecol Oncol. 2014;132(3):624–7.
Pluta M, Rob L, Charvat M, et al. Less radical surgery than radical hysterectomy in early stage cervical cancer: a pilot study. Gynecol Oncol. 2009;113(2):181–4.
Sood AK, Nygaard I, Shahin MS, Sorosky JI, Lutgendorf SK, Rao SSC. Anorectal dysfunction after surgical treatment for cervical cancer. J Am Coll Surg. 2002;195(4):513–9.
Hoffman MS. Extent of radical hysterectomy: evolving emphasis. Gynecol Oncol. 2004;94(1):1–9.
Jackson KS, Naik R. Pelvic floor dysfunction and radical hysterectomy. Int J Gynecol Cancer. 2006;16(1):354–63.
Photopulos GJ, Zwaag RV. Class II radical hysterectomy shows less morbidity and good treatment efficacy compared to class III. Gynecol Oncol. 1991;40(1):21–4.
Mauroy B, Demondion X, Bizet B, Claret A, Mestdagh P, Hurt C. The female inferior hypogastric (= pelvic) plexus: anatomical and radiological description of the plexus and its afferences–applications to pelvic surgery. Surg Radiol Anat SRA. 2007;29(1):55–66.
Zullo MA, Manci N, Angioli R, Muzii L, Panici PB. Vesical dysfunctions after radical hysterectomy for cervical cancer: a critical review. Crit Rev Oncol Hematol. 2003;48(3):287–93.
Touboul C, Fauconnier A, Zareski E, Bouhanna P, Daraï E. The lateral infraureteral parametrium: myth or reality? Am J Obstet Gynecol. 2008;199(3):242.e1–6.
Bonneau C, Cortez A, Lis R, et al. Lymphatic and nerve distribution throughout the parametrium. Gynecol Oncol. 2013;131(3):708–13.
Wright JD, Grigsby PW, Brooks R, et al. Utility of parametrectomy for early stage cervical cancer treated with radical hysterectomy. Cancer. 2007;110(6):1281–6.
Jung D-C, Kim M-K, Kang S, et al. Identification of a patient group at low risk for parametrial invasion in early-stage cervical cancer. Gynecol Oncol. 2010;119(3):426–30.
Covens A, Rosen B, Murphy J, et al. How important is removal of the parametrium at surgery for carcinoma of the cervix? Gynecol Oncol. 2002;84(1):145–9.
Steed H, Capstick V, Schepansky A, Honore L, Hiltz M, Faught W. Early cervical cancer and parametrial involvement: is it significant? Gynecol Oncol. 2006;103(1):53–7.
Pecorelli S. Revised FIGO staging for carcinoma of the vulva, cervix, and endometrium. Int J Gynaecol Obstet. 2009;105(2):103–4.
Piver MS, Rutledge F, Smith JP. Five classes of extended hysterectomy for women with cervical cancer. Obstet Gynecol. 1974;44(2):265–72.
Querleu D, Morrow CP. Classification of radical hysterectomy. Lancet Oncol. 2008;9(3):297–303.
Frumovitz M, Sun CC, Schover LR, et al. Quality of life and sexual functioning in cervical cancer survivors. J Clin Oncol. 2005;23(30):7428–36.
Girardi F, Lichtenegger W, Tamussino K, Haas J. The importance of parametrial lymph nodes in the treatment of cervical cancer. Gynecol Oncol. 1989;34(2):206–11.
Burghardt E, Haas J, Girardi F. The significance of the parametrium in the operative treatment of cervical cancer. Baillieres Clin Obstet Gynaecol. 1988;2(4):879–88.
Benedetti-Panici P, Maneschi F, D’Andrea G, et al. Early cervical carcinoma: the natural history of lymph node involvement redefined on the basis of thorough parametrectomy and giant section study. Cancer. 2000;88(10):2267–74.
Fujii S. Original film of the Okabayashi’s radical hysterectomy by Okabayashi himself in 1932, and two films of the precise anatomy necessary for nerve-sparing Okabayashi’s radical hysterectomy clarified by Shingo Fujii. Int J Gynecol Cancer. 2008;18(2):383–5.
Possover M, Quakernack J, Chiantera V. The LANN technique to reduce postoperative functional morbidity in laparoscopic radical pelvic surgery. J Am Coll Surg. 2005;201(6):913–7.
Bendifallah S, Uzan C, Fauvet R, Morice P, Darai E. External multicentre validation of a nomogram predicting the risk of relapse in patients with borderline ovarian tumours. Br J Cancer. 2013;109(11):2774–7.
Bendifallah S, Daraï E, Ballester M. Predictive modeling: a new paradigm for managing endometrial cancer. Ann Surg Oncol. 2016;23(3):975–88.
Kong T-W, Kim J, Son J-H, et al. Preoperative nomogram for prediction of microscopic parametrial infiltration in patients with FIGO stage IB cervical cancer treated with radical hysterectomy. Gynecol Oncol. 2016;142(1):109–14.
Winter R, Haas J, Reich O, et al. Parametrial spread of cervical cancer in patients with negative pelvic lymph nodes. Gynecol Oncol. 2002;84(2):252–7.
Kristensen GB, Abeler VM, Risberg B, Trop C, Bryne M. Tumor size, depth of invasion, and grading of the invasive tumor front are the main prognostic factors in early squamous cell cervical carcinoma. Gynecol Oncol. 1999;74(2):245–51.
Höckel M. Principles and practice of surgical treatment for cervical cancer: it’s time for a change. Womens Health Lond Engl. 2009;5(5):459–62.
Stegeman M, Louwen M, van der Velden J, et al. The incidence of parametrial tumor involvement in select patients with early cervix cancer is too low to justify parametrectomy. Gynecol Oncol. 2007;105(2):475–80.
Chang S-J, Bristow RE, Ryu H-S. A model for prediction of parametrial involvement and feasibility of less radical resection of parametrium in patients with FIGO stage IB1 cervical cancer. Gynecol Oncol. 2012;126(1):82–6.
Kodama J, Kusumoto T, Nakamura K, Seki N, Hongo A, Hiramatsu Y. Factors associated with parametrial involvement in stage IB1 cervical cancer and identification of patients suitable for less radical surgery. Gynecol Oncol. 2011;122(3):491–4.
Salvo G, Ramirez PT, Levenback CF, et al. Sensitivity and negative predictive value for sentinel lymph node biopsy in women with early-stage cervical cancer. Gynecol Oncol. 2017;145(1):96–101.
Wuntakal R, Papadopoulos AJ, Montalto SA, Perovic M, Coutts M, Devaja O. Location of sentinel lymph node in cervical carcinoma and factors associated with unilateral detection. Int J Gynecol Cancer. 2015;25(9):1663–8.
Laterza RM, Uccella S, Casarin J, et al. Recurrence of early stage cervical cancer after laparoscopic versus open radical surgery. Int J Gynecol Cancer. 2016;26(3):547–52.
Perez CA, Grigsby PW, Camel HM, Galakatos AE, Mutch D, Lockett MA. Irradiation alone or combined with surgery in stage IB, IIA, and IIB carcinoma of uterine cervix: update of a nonrandomized comparison. Int J Radiat Oncol Biol Phys. 1995;31(4):703–16.
Conte M, Panici PB, Guariglia L, Scambia G, Greggi S, Mancuso S. Pelvic lymphocele following radical para-aortic and pelvic lymphadenectomy for cervical carcinoma: incidence rate and percutaneous management. Obstet Gynecol. 1990;76(2):268–71.
Levenback C, Coleman RL, Burke TW, et al. Lymphatic mapping and sentinel node identification in patients with cervix cancer undergoing radical hysterectomy and pelvic lymphadenectomy. J Clin Oncol. 2002;20(3):688–93.
Höckel M, Horn L-C, Fritsch H. Association between the mesenchymal compartment of uterovaginal organogenesis and local tumour spread in stage IB–IIB cervical carcinoma: a prospective study. Lancet Oncol. 2005;6(10):751–6.
Uzan C, Merlot B, Gouy S, et al. Laparoscopic radical hysterectomy after preoperative brachytherapy for stage IB1 cervical cancer: feasibility, results, and surgical implications in a large bicentric study of 162 consecutive cases. Ann Surg Oncol. 2013;20(3):872–80.
Resbeut MR, Alzieu C, Gonzague-Casabianca L, et al. Combined brachytherapy and surgery for early carcinoma of the uterine cervix: analysis of extent of surgery on outcome. Int J Radiat Oncol Biol Phys. 2001;50(4):873–81.
Ngô C, Alran S, Plancher C, et al. Outcome in early cervical cancer following pre-operative low dose rate brachytherapy: a ten-year follow up of 257 patients treated at a single institution. Gynecol Oncol. 2011;123(2):248–52.
Maneo A, Chiari S, Bonazzi C, Mangioni C. Neoadjuvant chemotherapy and conservative surgery for stage IB1 cervical cancer. Gynecol Oncol. 2008;111(3):438–43.
Radical versus simple hysterectomy and pelvic node dissection in patients with low-risk early stage cervical cancer (SHAPE)—Full Text View—ClinicalTrials.gov. [cited 2017 Apr 16]. https://clinicaltrials.gov/ct2/show/NCT01658930?term=gynecologic+cancer+intergroup&rank=17.
Conservative surgery for women with cervical cancer—Full Text View—ClinicalTrials.gov. [cited 2017 Apr 16]. https://clinicaltrials.gov/show/NCT01048853.
Studying the physical function and quality of life before and after surgery in patients with stage I cervical cancer—Full Text View—ClinicalTrials.gov. [cited 2017 Apr 16]. https://clinicaltrials.gov/show/NCT01649089.
Authors’ contributions
Conceptualization: CT, BH, ED. Validation: SB. Formal analysis: YD, MB, VL, ER, CH. Investigation: CW, MB, XC, SB, LO, GC, ER, CC, OG, PC, AB. Data curation: XC, CC. Original draft: YD, CW, CT. Review: All authors Visualization: PC, AB. Supervision: CT, BH, MB. All authors revised the manuscript for important intellectual content. All authors reviewed and agree to be accountable for all aspects of the work. All authors read and approved the final manuscript.
Acknowledgements
Not applicable.
Competing interests
CT is an occasional consultant for TWA-ADELPHI. The remaining authors report no competing interests.
Availability of data and materials
Not applicable.
Consent for publication
Not applicable.
Ethics approval and consent to participate
The research protocol was approved by the Institutional Review Board (IRB) of the French College of Obstetrics and Gynaecology (CEROG 2016 – GYN – 0502). As our study was non interventional and retrospective, formal written consent from patients included was not necessary.
Funding
None.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional files
Additional file 1: Table S1.
Surgical outcomes and final pathologic analysis in patients with and without parametrial involvement diversified by stage.
Additional file 2.
Discrimination of the prediction model for predicting parametrial invasion in our cohort of 263 patients. Area under the curve: 0.95.
Additional file 3.
Calibration of the prediction model for predicting parametrial invasion in our cohort of 263 patients. The x-axis represents the probability of parametrial invasion calculated with our model and y – axis represents the actual rate of parametrial invasion in our cohort.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Dabi, Y., Willecocq, C., Ballester, M. et al. Identification of a low risk population for parametrial invasion in patients with early-stage cervical cancer. J Transl Med 16, 163 (2018). https://doi.org/10.1186/s12967-018-1531-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12967-018-1531-6