Abstract
Background
Successful clinical outcomes of faecal microbiota transplantation (FMT) for recurrent Clostridium difficile infection have been reported in humans and a marmoset. However, it has been unclear whether oral FMT was effective for the treatment of C. difficile-associated diarrhoea in dogs.
Case presentation
An 8-month-old, intact male French bulldog was presented with a 4-month history of intermittent large bowel diarrhoea. Physical and clinical examinations did not identify any specific causes for diarrhoea. Real-time PCR analysis and immunochromatography detected C. difficile antigen and toxin A&B genes and proteins in a faecal sample. Based on these findings, diarrhoea in the dog was considered to be induced by C. difficile-associated colitis. The dog was treated with oral FMT, in which a faecal solution obtained from a healthy beagle was orally administered to the subject. Stool consistency and frequency and faecal blood and mucus became normal 2–3 days after oral FMT, and real-time PCR analysis and immunochromatography was negative for C. difficile antigen and toxin A&B genes and proteins. No adverse events were observed.
Conclusion
The present case report demonstrated that oral FMT was an effective treatment for C. difficile-associated diarrhoea in a dog. The findings in this report provide a rationale to evaluate clinical efficacy of oral FMT for other gastrointestinal diseases in dogs.
Similar content being viewed by others
Background
Clostridium difficile is the most common cause of antibiotic-associated pseudomembranous colitis and induces severe and recurrent diarrhoea, especially in hospitalized human patients [1]. C. difficile is also associated with enterocolitis and diarrhoea in animals including dogs [2] and marmosets [3]. Metronidazole is an effective antibiotic for the treatment of C. difficile infection (CDI) in humans [1] and animals [2]. However, recurrent CDI after treatment with antibiotics including metronidazole has become a clinical problem in human patients [1].
Faecal microbiota transplantation (FMT) is a treatment option performed by introducing faecal microbiota obtained from a healthy donor into the gastrointestinal (GI) tract of a recipient [4, 5]. Successful clinical outcomes of FMT for recurrent CDI have been reported in humans [5,6,7] and a marmoset [3]. However, it has been unclear whether FMT was effective for the treatment of C. difficile-associated diarrhoea in dogs. Here, we report persistent recovery from C. difficile-associated diarrhoea in a dog after oral FMT without any adverse events.
Case presentation
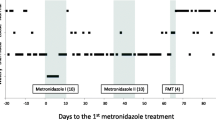
An 8-month-old, 11.0-kg, sexually intact male French bulldog was presented on day 1 with a 4-month history of intermittent diarrhoea and a 7-day history of focal seizures that had been observed almost every day for 7 days. Stool consistency had been very soft to watery, and stool frequency had been > 7 times/day. Blood and mucus had been observed in the faeces. Thus, diarrhoea was considered to be induced by colitis. Four months prior to the current presentation, a faecal sample of the dog was subjected to real-time PCR analysis (IDEXX Laboratories, Inc., Tokyo, Japan) for Cryptosporidium spp., Giardia spp., Clostridium perfringens α toxin, Clostridium difficile toxin A&B, Campylobacter jejuni, Campylobacter coli, Salmonella spp., Canine parvovirus type 2, canine distemper virus and canine enteric coronavirus genes by a veterinary practitioner; a positive reaction for Campylobacter jejuni was detected in the analysis. The dog was treated with tylosin (Tylan, Eli Lilly Japan K.K., Kobe, Japan; 10 mg/kg PO, q12h) for 7 days by a veterinary practitioner; however, stool conditions did not improve. Administration of an antidiarrhoeal (Diabuster, Kyuritsu, Tokyo, Japan; 1 tablet PO, q12h) containing berberine tannate, bismuth subnitrate, geranium herb, nutgalls and scopolia extract, and an antiflatulent (Bioymbuster, Kyuritsu, Tokyo, Japan; 1 tablet PO, q12h) containing Bacillus coagulans, Bifidobacterium longuin, Lactobacillus acidophilus, Streptococcus faecalis and pancreatin, improved stool conditions. However, once these drugs were discontinued, the diarrhoea recurred.
On day 1, physical and clinical examinations, including a complete blood count (CBC), a serum biochemical analysis, radiography, an abdominal ultrasound and faecal examination, did not reveal any specific causes for chronic diarrhoea and focal seizures. A faecal sample was subjected to real-time PCR analysis (IDEXX Laboratories, Inc.) to investigate an infectious cause of diarrhoea. Meanwhile, the dog was administered erythromycin (Erythromycin, Sawai Pharmaceutical, Osaka, Japan; 10 mg/kg PO, q12h) for 14 days based on the positive result for C. jejuni infection 4 months earlier.
On day 2, real-time PCR analysis of a faecal sample collected on day 1 was found to be positive for C. difficile toxin A&B genes and negative for other pathogens. The presence of C. difficile antigen and toxin A&B proteins in a faecal sample collected on day 1 was also confirmed by an immunochromatographic test kit (Techlab C. Diff Quick Chek Complete, Alere, Chiba, Japan).
In the follow-up visit on day 16, stool conditions did not improve after administration of erythromycin in the dog. Based on the clinical and investigative findings, diarrhoea in the dog was considered to be induced by C. difficile-associated colitis. Treatment with metronidazole was proposed; however, the owner rejected this treatment because of the potential for metronidazole-induced neuropathy. To investigate the cause of focal seizures, computed tomography and magnetic resonance imaging were performed. Mild ventriculomegaly was detected in the brain of the dog on imaging, but it was unclear whether the lesion was related to the seizures. After initiating treatment with zonisamide (Consave, DS Pharma Animal Health, Osaka, Japan; 10 mg/kg PO, q12h), the seizure frequency decreased.
On day 25, the dog still had large bowel diarrhoea. Real-time PCR analysis and immunochromatography confirmed that C. difficile antigen and toxin A&B genes and proteins were still positive in a faecal sample collected on day 25. Therefore, instead of treatment with metronidazole, oral faecal microbiota transplantation (FMT) was performed after obtaining written informed consent from the owner. This treatment was approved by the Research Ethics Committee of Tokyo University of Agriculture and Technology. Fresh faeces were collected from a 9-year-old, 11.0-kg, sexually intact healthy male beagle maintained for research purposes. The healthy dog was housed in a cage and fed a commercial diet (Science Diet Adult, Hill’s-Colgate Ltd., Tokyo, Japan) once daily. Water was provided ad libitum. Physical and clinical examinations, including a CBC, a serum biochemical analysis, radiography, an abdominal ultrasound and faecal examination, did not find any abnormalities in the healthy dog, and real-time PCR analysis of a faecal sample did not detect any pathogens. Immediately after faecal collection, approximately 60 g of faeces was dissolved in 50 mL of tap water. The faecal solution was filtered through a medical gauze pad twice. A total of 30 mL of a filtered faecal solution was obtained and orally administered to the recipient dog using a syringe.
Stool consistency became normal, and stool frequency was reduced to 4–5 times/day 2–3 days after oral FMT. Faecal blood and mucus were not observed after oral FMT. Real-time PCR analysis of a faecal sample collected at 7 days after oral FMT (day 32) was negative for C. difficile toxin A&B genes. Further real-time PCR analysis of faecal samples collected on days 61 and 149 confirmed that C. difficile toxin A&B genes were still negative. The absence of C. difficile antigen and toxin A&B proteins was also verified in the faecal samples by an immunochromatographic test kit after oral FMT. In addition, diarrhoea did not recur after oral FMT and further medications were unnecessary. Stool conditions are still normal on day 190.
Discussion and conclusions
The present case report demonstrated that C. difficile antigen and toxin A&B genes and proteins turned into negative, and stool consistency and frequency and faecal blood and mucus became normal after oral FMT in a dog with large bowel diarrhoea. Successful clinical outcomes of FMT for recurrent CDI have been reported in humans [5,6,7] and a marmoset [3]. These findings collectively suggest that correction of gut microbiota with FMT can be a useful treatment option for C. difficile-associated diarrhoea across animal species.
The pathogenesis of CDI is well established in humans, and involves toxin production by colonic C. difficile and depletion of non-C. difficile colonic microbiota [5]. However, it is still controversial whether C. difficile plays a pathological role in the development of diarrhoea in dogs [8]. C. difficile has been isolated both from the faeces of diarrheic dogs and those of healthy, non-diarrheic dogs, with various incidence rates depending on sample populations [9,10,11,12,13]. Several studies suggested a significant association between the presence of C. difficile toxins in faeces and canine diarrhoea [9,10,11]. An outbreak of C. difficile-associated disease was also reported in a small animal veterinary teaching hospital [14]. In contrast, a previous study failed to reproduce CDI in healthy adult dogs after administration of C. difficile with or without antibiotics [15]. In the present report, real-time PCR analysis and immunochromatography detected C. difficile antigen and toxin A&B genes and proteins in a faecal sample. Physical and clinical examinations did not identify any other causes for chronic large bowel diarrhoea. In addition, C. difficile antigen and toxin A&B genes and proteins became negative after oral FMT, and diarrhoea did not recur despite no further pharmacological treatment. Based on these clinical and molecular findings, diarrhoea in this dog was considered to be induced by C. difficile-associated colitis.
FMT can be performed via the upper or lower GI tract [5]. Theoretical guidelines for FMT have been recently proposed in dogs and cats [16]. In a recent study that reported the clinical efficacy of FMT for puppies with canine parvovirus infection [17], faecal suspension was infused into the proximal portion of the rectum in puppies by retention enema. Since clinical data of FMT are very limited in veterinary medicine, there is no consensus regarding the appropriate method of faecal administration in dogs. In the present case, FMT was performed by oral administration of faeces diluted with tap water. Oral FMT was also shown to be effective for the treatment of CDI in a marmoset [3], whereby faeces were mixed with the marmoset’s usual food and fed to the subject. In human patients with CDI, there was a report of cases refractory to lower GI delivery that responded to FMT via oral frozen faecal capsules [18]. Oral FMT is much easier than other methods of FMT, such as FMT with endoscopy, nasogastric/nasoenteric tubes and retention enema. Although potential advantages and disadvantages exist for FMT via the upper or lower GI tract, the present report suggests that oral administration of a faecal solution can be a useful FMT method in dogs.
The recipient dog in this report did not show any adverse events after oral FMT until day 190. The recipient dog was orally administered a fresh faecal solution prepared from a healthy beagle that did not have any abnormalities on physical and clinical examinations and any faecal pathogens.
Metronidazole is reported to be an effective antibiotic for the treatment of CDI in dogs [2] and humans [1]. However, in vitro analyses showed metronidazole-resistant strains in faeces of dogs [19, 20]. In human patients, as many as 20% of CDI cases treated with antibiotics including metronidazole was reported to recur [5] and a target for FMT. In this report, because metronidazole was not administered at the owner’s request, it is unclear whether C. difficile detected in the dog was metronidazole-resistant. Previous studies have shown that FMT was effective for the treatment of antibiotics-resistant recurrent CDI in humans, with cure rates of > 80% [5,6,7], and a marmoset [3]. To evaluate the effect of FMT for metronidazole-resistant recurrent CDI in dogs, further studies are required.
The mechanism underlying FMT is considered to be the reestablishment of the normal gut microbiota as a host defense against CDI [21]. A previous study showed that faecal microbiota in human patients with CDI had a lower bacterial diversity than healthy humans; in these patients, FMT improved the microbiota diversity [7]. In the current report, faecal microbiota was not analyzed in the dog with CDI. To clarify the mechanism by which oral FMT exerts a treatment effect on CDI in dogs, it is necessary to compare faecal microbiota in canine patients with those in healthy dogs, and to evaluate the microbiota in canine patients before and after oral FMT.
In conclusion, the present report revealed that oral FMT was an effective treatment for C. difficile-associated diarrhoea in a dog. FMT can reintroduce normal microbiota from healthy individuals into patients, correcting the underlying dysbiosis in the gut. Previous studies have reported dysbiosis was associated with acute and chronic GI diseases in dogs, including idiopathic inflammatory bowel disease [22,23,24]. The findings in the present report provide a rationale to evaluate clinical efficacy of oral FMT for other GI diseases in dogs.
Abbreviations
- C. difficile :
-
Clostridium difficile
- CBC:
-
complete blood count
- CDI:
-
Clostridium difficile infection
- FMT:
-
Faecal microbiota transplantation
- GI:
-
Gastrointestinal
References
Aslam S, Hamill RJ, Musher DM. Treatment of Clostridium difficile-associated disease: old therapies and new strategies. Lancet Infect Dis. 2005;5:549–57.
Marks SL. Enteric bacterial diseases. In: Ettinger SJ, Feldman EC, Côté E, editors. Textbook of veterinary internal medicine. 8th ed. Missouri: Elsevier; 2017. p. 957–62.
Yamazaki Y, Kawarai S, Morita H, Kikusui T, Iriki A. Faecal transplantation for the treatment of Clostridium difficile infection in a marmoset. BMC Vet Res. 2017;13:150.
Borody TJ, Khoruts A. Faecal microbiota transplantation and emerging applications. Nat Rev Gastroenterol Hepatol. 2011;9:88–96.
Kelly BJ, Tebas P. Clinical practice and infrastructure review of faecal microbiota transplantation for Clostridium difficile infection. Chest. 2018;153:266–77.
Kassam Z, Lee CH, Yuan Y, Hunt RH. Faecal microbiota transplantation for Clostridium difficile infection: systematic review and meta-analysis. Am J Gastroenterol. 2013;108:500–8.
van Nood E, Vrieze A, Nieuwdorp M, Fuentes S, Zoetendal EG, de Vos WM, et al. Duodenal infusion of donor faeces for recurrent Clostridium difficile. N Engl J Med. 2013;368:407–15.
Marks SL, Rankin SC, Byrne BA, Weese JS. Enteropathogenic bacteria in dogs and cats: diagnosis, epidemiology, treatment, and control. J Vet Intern Med. 2011;25:1195–208.
Cave NJ, Marks SL, Kass PH, Melli AC, Brophy MA. Evaluation of a routine diagnostic faecal panel for dogs with diarrhoea. J Am Vet Med Assoc. 2002;221:52–9.
Weese JS, Staempfli HR, Prescott JF, Kruth SA, Greenwood SJ, Weese HE. The roles of Clostridium difficile and enterotoxigenic Clostridium perfringens in diarrhoea in dogs. J Vet Intern Med. 2001;15:374–8.
Marks SL, Kather EJ, Kass PH, Melli AC. Genotypic and phenotypic characterization of Clostridium perfringens and Clostridium difficile in diarrheic and healthy dogs. J Vet Intern Med. 2002;16:533–40.
Hascall KL, Kass PH, Saksen J, Ahlmann A, Scorza AV, Lappin MR, et al. Prevalence of Enteropathogens in dogs attending 3 regional dog parks in northern California. J Vet Intern Med. 2016;30:1838–45.
Chouicha N, Marks SL. Evaluation of five enzyme immunoassays compared with the cytotoxicity assay for diagnosis of Clostridium difficile-associated diarrhoea in dogs. J Vet Diagn Investig. 2006;18:182–8.
Weese JS, Armstrong J. Outbreak of Clostridium difficile-associated disease in a small animal veterinary teaching hospital. J Vet Intern Med. 2003;17:813–6.
Clooten JK, Kruth SA, Weese JS. Genotypic and phenotypic characterization of Clostridium perfringens and Clostridium difficile in diarrheic and healthy dogs. J Vet Intern Med. 2003;17:123 author reply 123.
Redfern A, Suchodolski J, Jergens A. Role of the gastrointestinal microbiota in small animal health and disease. Vet Rec. 2017;181:370.
Pereira GQ, Gomes LA, Santos IS, Alfieri AF, Weese JS, Costa MC. Faecal microbiota transplantation in puppies with canine parvovirus infection. J Vet Intern Med. 2018;32:707–11.
Stollman N, Smith M, Giovanelli A, Mendolia G, Burns L, Didyk E, et al. Frozen encapsulated stool in recurrent Clostridium difficile: exploring the role of pills in the treatment hierarchy of faecal microbiota transplant nonresponders. Am J Gastroenterol. 2015;110:600–1.
Orden C, Blanco JL, Álvarez-Pérez S, Garcia-Sancho M, Rodriguez-Franco F, Sainz A, et al. Isolation of Clostridium difficile from dogs with digestive disorders, including stable metronidazole-resistant strains. Anaerobe. 2017;43:78–81.
Andrés-Lasheras S, Martín-Burriel I, Mainar-Jaime RC, Morales M, Kuijper E, Blanco JL, et al. Preliminary studies on isolates of Clostridium difficile from dogs and exotic pets. BMC Vet Res. 2018;14:77.
Khoruts A, Dicksved J, Jansson JK, Sadowsky MJ. Changes in the composition of the human faecal microbiome after bacteriotherapy for recurrent Clostridium difficile-associated diarrhoea. J Clin Gastroenterol. 2010;44:354–60.
Suchodolski JS, Markel ME, Garcia-Mazcorro JF, Unterer S, Heilmann RM, Dowd SE, et al. The faecal microbiome in dogs with acute diarrhoea and idiopathic inflammatory bowel disease. PLoS One. 2012;7:e51907.
Suchodolski JS, Xenoulis PG, Paddock CG, Steiner JM, Jergens AE. Molecular analysis of the bacterial microbiota in duodenal biopsies from dogs with idiopathic inflammatory bowel disease. Vet Microbiol. 2010;142:394–400.
Xenoulis PG, Palculict B, Allenspach K, Steiner JM, Van House AM, Suchodolski JS. Molecular-phylogenetic characterization of microbial communities imbalances in the small intestine of dogs with inflammatory bowel disease. FEMS Microbiol Ecol. 2008;66:579–89.
Acknowledgements
Not applicable.
Funding
None.
Availability of data and materials
All data generated or analysed during this study are included in this published article.
Author information
Authors and Affiliations
Contributions
KS and KO designed the experiments and wrote the manuscript; NY, HO, KT and KO performed the experiments; and KS, KK, HM and KO analysed data and coordinated the manuscript writing. All authors reviewed the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This study was approved by the Research Ethics Committee of Tokyo University of Agriculture and Technology (0016018).
Consent for publication
Written informed consent for publication of the clinical details was obtained from the owner of the dog.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Sugita, K., Yanuma, N., Ohno, H. et al. Oral faecal microbiota transplantation for the treatment of Clostridium difficile-associated diarrhoea in a dog: a case report. BMC Vet Res 15, 11 (2019). https://doi.org/10.1186/s12917-018-1754-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12917-018-1754-z