Abstract
Background
Acute eosinophilic pneumonia (AEP) is a rare inflammatory lung disease. Previous studies have shown that most patients with AEP are aged 20 to 40 years, whereas several case studies have included older patients with AEP. These studies also suggested that AEP is more prevalent in summer, but they were limited due to their small sample sizes. We therefore investigated the age distribution and seasonality among patients with AEP using a national inpatient database.
Methods
Using the Japanese Diagnosis Procedure Combination database, we identified patients with a recorded diagnosis of AEP from 1 July 2010 to 31 March 2015. We examined patient characteristics and clinical practices including age, sex, seasonal variation, length of stay, use of corticosteroids, use of mechanical ventilation, and in-hospital mortality.
Results
During the 57-month study period, we identified 213 inpatients with AEP. The age distribution of AEP peaked twice: at 15 to 24 years and 65 to 79 years. The proportion of patients with AEP was highest in summer for those aged < 40 years, whereas it was distributed evenly throughout the year for those aged ≥ 40 years. The interval from hospital admission to corticosteroid administration and the duration of corticosteroid use were significantly longer in the older than younger age group.
Conclusions
The age distribution of patients with AEP was bimodal, and seasonality was undetected in older patients. Older patients may be more likely to have delayed and prolonged treatment.
Similar content being viewed by others
Background
Acute eosinophilic pneumonia (AEP) is a rare disease that was originally reported by Badesch et al. [1] and Allen et al. [2] in 1989. Patients with AEP frequently show hypoxaemic respiratory dysfunction and often require mechanical ventilation [3, 4]. Previous studies have indicated that patients with AEP have a rapid response to corticosteroid treatment [1, 2, 4, 5] and low mortality. However, a delay in diagnosis and treatment may result in increased mortality [6,7,8,9].
Most patients with AEP in previous studies were aged 20 to 40 years [3, 5, 8, 10,11,12,13,14], but several case reports and case series have included older patients [15,16,17,18]. However, these previous studies were limited due to their small number of patients. Studies regarding the seasonality of AEP occurrence included only young healthy military personnel [5, 8, 10, 11].
We therefore investigated the age distribution and seasonality among patients with AEP who required hospitalization using a nationwide inpatient database in Japan. We also examined clinical practices for patients with AEP and compared them between young and older patients.
Methods
Data source
For this study, we used the Diagnosis Procedure Combination database from 1 July 2010 to 31 March 2015. All 82 academic hospitals in Japan are obliged to participate in the database, while participation by community hospitals is voluntary. The database includes administrative claims data and some clinical data for all inpatients. The database contains the following items: unique hospital identifiers, patient age and sex, type of procedures, length of stay, and diagnoses and comorbidities recorded in Japanese text and International Classification of Diseases 10th Revision (ICD-10) codes. Dates of procedures performed and drugs prescribed are also recorded. To optimize the accuracy of diagnoses, attending physicians are required to record the diagnoses with reference to medical charts.
Given the anonymous nature of the data, informed consent was not required for this study. The research was approved by the Institutional Review Board at The University of Tokyo.
Patient selection
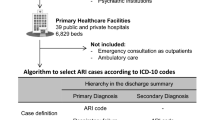
We identified patients with an ICD-10 code of J82 (pulmonary eosinophilia) and whose diagnosis in Japanese text was ‘acute eosinophilic pneumonia’. Among them, we excluded patients who also had any of the following ICD-10 codes: aspergillosis (B44), pneumocystosis (B59), pneumonia in parasitic diseases (J173), lung cancer (C34), chronic lymphocytic leukaemia (C911), eosinophilia (D721), sarcoidosis of the lung (D860), chlamydial pneumonia (J160), hypersensitivity pneumonitis (J679), pulmonary fibrosis (J841), interstitial pulmonary disease unspecified (J849), eosinophilic granulomatosis with polyangiitis (Churg–Strauss syndrome) (M301), other overlapping syndromes (M351), and colon cancer (C18). Because AEP is confirmed with bronchoscopy and corticosteroid therapy is generally provided after bronchoscopy, we excluded patients who did not undergo bronchoscopy within 7 days after admission and those who received corticosteroids before bronchoscopy to improve the specificity of the diagnosis of AEP [2, 3]. (Fig. 1).
Patient backgrounds
Patient background data included age, sex, smoking status, Charlson comorbidity index (CCI) at admission, and season of admission. The CCI was calculated as a weighted score of specific comorbid diseases based on the ICD-10 codes [19]. Seasons were defined as the following 3-month periods: spring as March to May, summer as June to August, fall as September to November, and winter as December to February [20].
Clinical practice
Data on patients’ clinical practices included length of stay after bronchoscopy, interval (days) from admission to bronchoscopy, interval (days) from admission to corticosteroid administration, duration of corticosteroid therapy, use of mechanical ventilation, and in-hospital death.
Statistical analyses
According to previous reviews of AEP [4], patients aged < 40 years were categorized as the younger age group, and those aged ≥ 40 years were categorized as the older age group. Patient backgrounds and clinical practices were compared between the younger and older age groups. Categorical variables are presented as numbers with percentages and were compared using the chi-squared test. Continuous variables are presented as median and interquartile range and were compared using the Mann–Whitney U test.
For each group (younger and older patients with AEP), we described the seasonality of AEP admissions and compared the proportions of patients with AEP among the four seasons using chi-squared tests.
A P value of < 0.05 was considered statistically significant. All statistical analyses were performed using IBM SPSS version 23 (IBM Corp., Armonk, NY, USA).
Results
During the 57-month study period, we identified 213 eligible patients. Figure 1 shows the algorithm for patient selection.
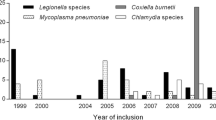
Of these, 84 patients were in the younger age group and 129 patients were in the older age group. The age distribution of all patients with AEP is shown in Fig. 2. There was a bimodal distribution peaking around age 15 to 24 and 65 to 79 years.
Table 1 shows the patient characteristics of the two age groups. Although not significant, the proportion of males was higher in the younger than older age group. The smoking status was not significantly different between the two groups. The older age group was significantly more likely to have a higher CCI. With respect to seasonality, about one-half of AEP admissions in the younger age group occurred in summer. Seasonality was significantly different between the two groups.
Figure 3 shows the seasonal distribution of hospitalized patients with AEP in the two age groups. In the younger age group, a distinct peak was observed in summer (July–August). Chi-squared tests showed a significant difference in the proportions of AEP admissions among the four seasons in the younger age group (P < 0.001), but not in the older age group (P = 0.129).
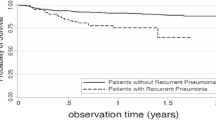
Table 2 compares the clinical practices between the younger and older age groups. The older age group showed a significantly longer length of stay after bronchoscopy, interval from admission to corticosteroid administration, and duration of corticosteroid administration compared with the younger age group. There was no significant difference in the use of mechanical ventilation or in-hospital death between the two groups.
Discussion
Using a national inpatient database in Japan, we identified two peaks in the age distribution of patients with AEP. The younger patients were hospitalized more frequently in summer, whereas there was no significant seasonal variation in hospitalization for AEP in the older patients.
Previous studies have suggested that AEP mainly occurs in younger patients [3, 5, 8, 10,11,12,13,14]. In contrast, the population in the present study included patients of all ages from the national database. Notably, most patients with AEP in our study were aged ≥ 40. In fact, the proportions of older patients in two previous small case series and one clinical study were comparable with the proportion in our study [18, 21, 22].
The sex ratio of patients with AEP was inconsistent among previous studies and understandably male-dominant in the military cohort [5, 8, 10, 11]. In several case series [3, 16, 23, 24], the occurrence of AEP was similar between male and female patients. In the present study, AEP was more common in men in the younger age group, whereas the occurrence of AEP was similar between men and women in the older age group. The reason for this remains unclear, however toxin inhalations, infections, and medications may be able to explain this [22, 25].
As in previous reports [8, 11], the occurrence of AEP in the younger age group was dominant in summer, whereas that in the older age group did not show such a trend. This may suggest a difference in causal factors of AEP between younger and older patients. Although the present study cannot clarify the causes of AEP, we speculate that several reported factors, including susceptibility to medication [22, 25], air pollution [26, 27] and viral infection [28, 29], may have differed between the younger and older patients. This might have caused the difference in their seasonal variation.
The length of stay after bronchoscopy, interval from admission to corticosteroid administration, and duration of corticosteroid therapy were significantly different between the younger and older age groups. This may suggest that older patients are more likely to have delayed and prolonged treatment.
Our study has several limitations. First, data on laboratory testing, imaging, and histopathology were not available in the database. Second, pre-admission data were also unavailable. Third, we may have overlooked some older patients with AEP, possibly because physicians may have hesitated to perform bronchoscopy in such patients.
Conclusions
In conclusion, our study showed that patients hospitalized with AEP had a bimodal age distribution. Younger patients were more prevalent in summer, but AEP in older patients did not show seasonality.
Abbreviations
- AEP:
-
Acute eosinophilic pneumonia
- CCI:
-
Charlson comorbidity index
- ICD-10:
-
International Classification of Diseases 10th Revision
References
Badesch DB, King TE Jr, Schwarz MI. Acute eosinophilic pneumonia: a hypersensitivity phenomenon? Am Rev Respir Dis. 1989;139:249–52.
Allen JN, Pacht ER, Gadek JE, Davis WB. Acute eosinophilic pneumonia as a reversible cause of noninfectious respiratory failure. N Engl J Med. 1989;321:569–74.
Philit F, Etienne-Mastroïanni B, Parrot A, Guérin C, Robert D, Cordier JF. Idiopathic acute eosinophilic pneumonia: a study of 22 patients. Am J Respir Crit Care Med. 2002;166:1235–9.
Buchheit J, Eid N, Rodgers G, Feger TIM, Yakoub O. Acute eosinophilic pneumonia with respiratory failure: a new syndrome? Am Rev Respir Dis. 1992;145:716–8.
Jhun BW, Kim SJ, Kim K, Lee JE. Outcomes of rapid corticosteroid tapering in acute eosinophilic pneumonia patients with initial eosinophilia. Respirology. 2015;20:1241–7.
Tomac N, Kuyucu N, Tezic T, Duru F, Karademir S, Gurer Y. An epidemic form of AEP. Allergy. 2002;57:1213–4.
Shin HY, Choe JW, Kwon M, Jung JW, Choi JC, Shin JW, Park IW, Choi BW, Kim JY. Acute eosinophilic pneumonia leading to acute respiratory failure in a current systemic corticosteroid user. Allergy Asthma Immunol Res. 2013;5:242–4. https://doi.org/10.4168/aair.2013.5.4.242.
Shorr AF, Scoville SL, Cersovsky SB, Shanks GD, Ockenhouse CF, Smoak BL, Carr WW, Petruccelli BP. Acute eosinophilic pneumonia among US military personnel deployed in or near Iraq. JAMA. 2004;292:2997–3005.
Kawayama T, Fujiki R, Morimitsu Y, Rikimaru T, Aizawa H. Fatal idiopathic acute eosinophilic pneumonia with acute lung injury. Respirology. 2002;7:373–5.
Rhee CK, Min KH, Yim NY, et al. Clinical characteristics and corticosteroid treatment of acute eosinophilic pneumonia. Eur Respir J. 2013;41:402–9.
Yoon CG, Kim SJ, Kim K, Lee JE, Jhun BW. Clinical characteristics and factors influencing the occurrence of acute eosinophilic pneumonia in Korean military personnel. J Korean Med Sci. 2016;31:247–53. https://doi.org/10.3346/jkms.2016.31.2.247.
Nakajima M, Matsushima T. Acute eosinophilic pneumonia following cigarette smoking. Intern Med. 2000;39:759–60.
Uchiyama H, Suda T, Nakamura Y, Shirai M, Gemma H, Shirai T, Toyoshima M, Imokawa S, Yasuda K, Ida M, Nakano Y, Inui N, Sato J, Hayakawa H, Chida K. Alterations in smoking habits are associated with acute eosinophilic pneumonia. Chest. 2008;133:1174–80.
Jhun BW, Kim SJ, Son RC, et al. Clinical outcomes in patients with acute eosinophilic pneumonia not treated with corticosteroids. Lung. 2015;193:361–7.
Larranaga JM, Marcos PJ, Pombo F, Otero-Gonzalez I. Acute eosinophilic pneumonia as a complication of influenza a (H1N1) pulmonary infection. Sarcoidosis Vasc Diffuse Lung Dis. 2016;33:95–7.
Daimon T, Johkoh T, Sumikawa H, Honda O, Fujimoto K, Koga T, Arakawa H, Yanagawa M, Inoue A, Mihara N, Tomiyama N, Nakamura H, Sugiyama Y. Acute eosinophilic pneumonia: thin-section CT findings in 29 patients. Eur J Radiol. 2008;65:462–7.
Pornsuriyasak P, Suwatanapongched T, Klaewsongkram J, Buranapraditkun S, Rotjanapan P. Acute respiratory failure secondary to eosinophilic pneumonia following influenza vaccination in an elderly man with chronic obstructive pulmonary disease. Int J Infect Dis. 2014;26:14–6.
Ajani S, Kennedy CC. Idiopathic acute eosinophilic pneumonia: a retrospective case series and review of the literature. Respir Med Case Rep. 2013;10:43–7.
Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43:1130–9.
Chen R, Peng RD, Meng X, Zhou Z, Chen B, Kan H. Seasonal variation in the acute effect of particulate air pollution on mortality in the China air pollution and health effects study (CAPES). Sci Total Environ. 2013;450–1:259–65.
Tazelaar HD, Linz LJ, Colby TV, Myers JL, Limper AH. Acute eosinophilic pneumonia: histopathologic findings in nine patients. Am J Respir Crit Care Med. 1997;155:296–302.
De Giacomi F, Decker PA, Vassallo R, Ryu JH. Acute Eosinophilic Pneumonia. Chest. 2017;152:379–85.
Pope-Harman AL, Davis WB, Allen ED, Christoforidis AJ, Allen JN. Acute eosinophilic pneumonia. A summary of 15 cases and review of the literature. Medicine (Baltimore). 1996;75:334–42.
Mochimaru H, Fukuda Y, Azuma A, Osanai K, Saito Y, Mochimaru T, Gemma A. Reconsideration of discrepancies between clinical and histopathological features in acute eosinophilic pneumonia. Sarcoidosis Vasc Diffuse Lung Dis. 2015;31:325–35.
De Giacomi F, Vassallo R, Yi ES, Ryu JH. Acute eosinophilic pneumonia. Causes, diagnosis, and management. Am J Respir Crit Care Med. 2018;197:728–36.
Bentayeb M, Simoni M, Baiz N, Norback D, Baldacci S, Maio S, Viegi G, Annesi-Maesano I. Adverse respiratory effects of outdoor air pollution in the elderly. Int J Tuberc Lung Dis. 2012;16:1149–61.
Boezen HM, Vonk JM, van der Zee SC, Gerritsen J, Hoek G, Brunekreef B, Schouten JP, Postma DS. Susceptibility to air pollution in elderly males and females. Eur Respir J. 2005;25:1018–24.
Jeon EJ, Kim KH, Min KH. Acute eosinophilic pneumonia associated with 2009 influenza a (H1N1). Thorax. 2010;65:268–70.
Fleming DM, Taylor RJ, Lustig RL, Schuck-Paim C, Haguinet F, Webb DJ, Logie J, Matias G, Taylor S. Modelling estimates of the burden of respiratory syncytial virus infection in adults and the elderly in the United Kingdom. BMC Infect Dis. 2015;15:443.
Funding
This work was supported by grants from the Ministry of Health, Labour and Welfare, Japan (H29-Policy-Designated-009 and H29-ICT-General-004); Ministry of Education, Culture, Sports, Science and Technology, Japan (17H04141); and the Japan Agency for Medical Research and Development (AMED).
Funding body did not contribute to the work in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Contributions
KO designed the study, and wrote the initial draft of the manuscript. YS, TJ, and HY contributed to analysis and interpretation of data, and assisted in the preparation of the manuscript. All other authors have contributed to data collection and interpretation, and critically reviewed the manuscript. All authors approved the final version of the manuscript, and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The research was approved and consent to participate was obtained by the Institutional Review Board at The University of Tokyo. (number 3501).
Consent for publication
Not applicable. Given the anonymous nature of the data, informed consent was not required for this study.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Ota, K., Sasabuchi, Y., Matsui, H. et al. Age distribution and seasonality in acute eosinophilic pneumonia: analysis using a national inpatient database. BMC Pulm Med 19, 38 (2019). https://doi.org/10.1186/s12890-019-0800-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12890-019-0800-3