Abstract
Introduction
Obesity is an epidemic affecting more than one-third of adults in the United States. Obese women experience decreased fertility, explained in part by oocyte quality. Since follicular fluid (FF) provides an important microenvironment for oocyte growth, we sought to evaluate the effect of increased body weight on FF levels of 11 metabolic hormones and fatty acid metabolism.
Methods
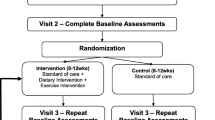
The FF was collected from 25 women (10 normal weight, 10 overweight, and 5 obese) with diminished ovarian reserve undergoing in vitro fertilization (IVF) following a minimal stimulation protocol. Hormone levels were determined by multiplex immunoassay using the MAGPIX (Luminex, Austin, Texas) instrument. Fatty acid metabolites were determined using gas and ultra-high pressure liquid chromatography coupled with mass spectrometry.
Results
Levels of hormones related to glucose and energy homeostasis and regulation of fat stores (insulin, glucagon, glucagon-like peptide-1, C-peptide, and leptin) were increased significantly in FF from obese women compared to FF from nonobese(normal weight and overweight) women. Interestingly, FF levels of branched-chain amino acids (BCAA) isoleucine, leucine, and valine as well as uric acid, isocaproic acid, butanoic acid, tyrosine, threonine, glycine, and methionine correlated positively with body mass index.
Conclusion
This pilot study demonstrates significant alterations in the FF milieu of obese women undergoing IVF, which may contribute to the decreased fecundity of obese women. Although the impact of this environment on oocyte and embryo development is not fully realized, these changes may also lead to imprinting at the genomic level and long-term sequelae on offspring.
Similar content being viewed by others
References
Adult Obesity Facts ∣ Overweight & Obesity ∣ CDC. https://www.cdc.gov/obesity/data/adult.html. Accessed March 5, 2018
Practice Committee of the American Society for Reproductive Medicine. Obesity and reproduction: a committee opinion. Fertil Steril. 2015;104(5):1116–1126. doi:https://doi.org/10.1016/j.fertnstert.2015.08.018
Kumbak B, Oral E, Bukulmez O. Female obesity and assisted reproductive technologies. Semin Reprod Med. 2012;30(6):507–516. doi:https://doi.org/10.1055/s-0032-1328879
Luke B, Brown M, Missmer S, Bukulmez O, Leach R, Stern J. The effect of increasing obesity on the response to and outcome of assisted reproductive technology: a national study. Fertil Steril. 2011;96(4):820–825. doi:https://doi.org/10.1016/J.FERTNSTERT.2011.07.1100
Fortune JE. Ovarian follicular growth and development in mammals. Biol Reprod. 1994;50(2):225–232. http://www.ncbi.nlm.nih.gov/pubmed/8142540. Accessed August 14, 2017
Revelli A, Delle Piane L, Casano S, Molinari E, Massobrio M, Rinaudo P. Follicular fluid content and oocyte quality: from single biochemical markers to metabolomics. Reprod Biol Endocrinol. 2009;7(1):40. doi:https://doi.org/10.1186/1477-7827-7-40
Ferraretti AP, La Marca A, Fauser BC, Tarlatzis B, Nargund G, Gianaroli L; ESHRE working group on Poor Ovarian Response Definition. ESHRE consensus on the definition of “poor response” to ovarian stimulation for in vitro fertilization: the Bologna criteria. Hum Reprod. 2011;26(7):1616–1624. doi:https://doi.org/10.1093/humrep/der092
Reed B, Babayev S, Bukulmez O. Shifting paradigms in diminished ovarian reserve and advanced reproductive age in assisted reproduction: customization instead of conformity. Semin Reprod Med. 2015;33(3):169–178. doi:https://doi.org/10.1055/s-0035-1552585
Xu YW, Peng YT, Wang B, Zeng YH, Zhuang GL, Zhou CQ. High follicle-stimulating hormone increases aneuploidy in human oocytes matured in vitro. Fertil Steril. 2011;95(1):99–104. doi:https://doi.org/10.1016/j.fertnstert.2010.04.037
Roberts R, Iatropoulou A, Ciantar D, et al. Follicle-stimulating hormone affects metaphase i chromosome alignment and increases aneuploidy in mouse oocytes matured in vitro1. Biol Reprod. 2005;72(1):107–118. doi:https://doi.org/10.1095/biolreprod.104.032003
Bou Nemer L, Weitzman VN, Arheart KL, et al. In vitro fertilization versus mild stimulation intrauterine insemination in women aged 40 and older. Reprod Sci. 2017;24(4):609–612. doi:https://doi.org/10.1177/1933719116667215
Wang QS, Zhou H, Yeung D, Ma L, Geng W. Development and validation of multiplex assays for human diabetes biomarkers. 2010. http://www.bio-rad.com/webroot/web/pdf/lsr/literature/Bulletin_5985A.pdf. Accessed January 17, 2018
Sessions-Bresnahan DR, Schauer KL, Heuberger AL, Carnevale EM. Effect of obesity on the preovulatory follicle and lipid fingerprint of equine oocytes. Biol Reprod. 2016;94(1):15. doi:https://doi.org/10.1095/biolreprod.115.130187
Laskowski D, Båge R, Humblot P, Andersson G, Sirard MA, Sjunnesson Y. Insulin during in vitro oocyte maturation has an impact on development, mitochondria, and cytoskeleton in bovine day 8 blastocysts. Theriogenology. 2017;101:15–25. doi:https://doi.org/10.1016/j.theriogenology.2017.06.002
Laskowski D, Sjunnesson Y, Humblot P, et al. Insulin exposure during in vitro bovine oocyte maturation changes blastocyst gene expression and developmental potential. Reprod Fertil Dev. 2016. doi:https://doi.org/10.1071/RD15315
Campbell BK, Scaramuzzi RJ, Webb R. Control of antral follicle development and selection in sheep and cattle. Journal of Reproduction and Fertility Supplement. 1995;49:335–350. http://www.ncbi.nlm.nih.gov/pubmed/7623325. Accessed September 19, 2017
Maruthini D, Harris SE, Barth JH, Balen AH, Campbell BK, Picton HM. The effect of metformin treatment in vivo on acute and long-term energy metabolism and progesterone production in vitro by granulosa cells from women with polycystic ovary syndrome. Hum Reprod. 2014;29(10):2302–2316. doi:https://doi.org/10.1093/humrep/deu187
Bhatia B, Price CA. Insulin alters the effects of follicle stimulating hormone on aromatase in bovine granulosa cells in vitro. Steroids. 2001;66(6):511–519. http://www.ncbi.nlm.nih.gov/pubmed/11182140. Accessed September 19, 2017
Dupont J, Scaramuzzi RJ. Insulin signalling and glucose transport in the ovary and ovarian function during the ovarian cycle. Biochem J. 2016;473(11):1483–1501. doi:https://doi.org/10.1042/BCJ20160124
Klok MD, Jakobsdottir S, Drent ML. The role of leptin and ghrelin in the regulation of food intake and body weight in humans: a review. Obes Rev. 2007;8(1):21–34. doi:https://doi.org/10.1111/j.1467-789X.2006.00270.x
Kamyabi Z, Gholamalizade T. A comparative study of serum and follicular fluid leptin concentrations among explained infertile, unexplained infertile and fertile women. Int J Fertil Steril. 2015;9(2):150–156. doi:https://doi.org/10.22074/ijfs.2015.4235
Várnagy A, Bódis J, Kovács GL, Sulyok E, Rauh M, Rascher W. Metabolic hormones in follicular fluid in women undergoing in vitro fertilization. J Reprod Med. 58(7–8):305–311. http://www.ncbi.nlm.nih.gov/pubmed/23947080. Accessed August 14, 2017
Anifandis G, Koutselini E, Stefanidis I, et al. Serum and follicular fluid leptin levels are correlated with human embryo quality. Reproduction. 2005;130(6):917–921. doi:https://doi.org/10.1530/rep.1.00705
Bützow TL, Moilanen JM, Lehtovirta M, et al. Serum and follicular fluid leptin during in vitro fertilization: relationship among leptin increase, body fat mass, and reduced ovarian response. J Clin Endocrinol Metab. 1999;84(9):3135–3139. doi:https://doi.org/10.1210/jcem.84.9.6004
Catteau A, Caillon H, Barrière P, Denis MG, Masson D, Fréour T. Leptin and its potential interest in assisted reproduction cycles. Hum Reprod Update. 2016;22(3):320–341. doi:https://doi.org/10.1093/humupd/dmv057
Zhang S, Zeng X, Ren M, Mao X, Qiao S. Novel metabolic and physiological functions of branched chain amino acids: a review. J Anim Sci Biotechnol. 2017;8:10. doi:https://doi.org/10.1186/s40104-016-0139-z
González IM, Martin PM, Burdsal C, et al. Leucine and arginine regulate trophoblast motility through mTOR-dependent and independent pathways in the preimplantation mouse embryo. Dev Biol. 2012;361(2):286–300. doi:https://doi.org/10.1016/j.ydbio.2011.10.021
Gangloff YG, Mueller M, Dann SG, et al. Disruption of the mouse mTOR gene leads to early postimplantation lethality and prohibits embryonic stem cell development. Mol Cell Biol. 2004;24(21):9508–9516. doi:https://doi.org/10.1128/MCB.24.21.9508-9516.2004
Martin PM, Sutherland AE. Exogenous amino acids regulate trophectoderm differentiation in the mouse blastocyst through an mTOR-dependent pathway. Dev Biol. 2001;240(1):182–193. doi:https://doi.org/10.1006/dbio.2001.0461
Spindle A. An improved culture medium for mouse blastocysts. In Vitro. 1980;16(8):669–674. http://www.ncbi.nlm.nih.gov/pubmed/7419236. Accessed August 21, 2017
Guertin DA, Stevens DM, Thoreen CC, et al. Ablation in mice of the mTORC components raptor, rictor, or mLST8 reveals that mTORC2 is required for signaling to Akt-FOXO and PKCalpha, but not S6K1. Dev Cell. 2006;11(6):859–871. doi:https://doi.org/10.1016/j.devcel.2006.10.007
Van Winkle LJ. Amino acid transport regulation and early embryo development. Biol Reprod. 2001;64(1):1–12. http://www.ncbi.nlm.nih.gov/pubmed/11133652. Accessed August 21, 2017
Zhang C, Zhao Y, Li R, et al. Metabolic heterogeneity of follicular amino acids in polycystic ovary syndrome is affected by obesity and related to pregnancy outcome. BMC Pregnancy Childbirth. 2014;14(1):11. doi:https://doi.org/10.1186/1471-2393-14-11
Stöger R. The thrifty epigenotype: an acquired and heritable predisposition for obesity and diabetes? BioEssays. 2008;30(2):156–166. doi:https://doi.org/10.1002/bies.20700
Aiken CE, Ozanne SE. Transgenerational developmental programming. Hum Reprod Update. 2014;20(1):63–75. doi:https://doi.org/10.1093/humupd/dmt043
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bou Nemer, L., Shi, H., Carr, B.R. et al. Effect of Body Weight on Metabolic Hormones and Fatty Acid Metabolism in Follicular Fluid of Women Undergoing In Vitro Fertilization: A Pilot Study. Reprod. Sci. 26, 404–411 (2019). https://doi.org/10.1177/1933719118776787
Published:
Issue Date:
DOI: https://doi.org/10.1177/1933719118776787