Abstract
Approximately 20% of pregnant women smoke despite intentions to quit. Smoking cessation drugs, such as nicotine replacement therapy (NRT) and bupropion, are recommended treatments. Adverse cardiovascular outcomes in offspring have raised concerns about NRT’s safety during pregnancy. However, the effect of bupropion is unknown. Using a rat model, we determined whether NRT and bupropion interventions during pregnancy are safer than continued smoking on offspring’s cardiovascular function. Male offspring of controls and dams exposed to cigarette smoke (1.6 packs/day, inhalation), nicotine (2 mg/kg/d subcutaneously), and bupropion (13 mg/kg twice daily orally) were assessed for fetoplacental weight, cardiac function, blood pressure, and vascular reactivity. Fetoplacental weights were decreased and spontaneous beating and intracellular calcium in neonatal cardiomyocytes were increased in smoking, nicotine, and bupropion offspring; however, these effects were more accentuated in smoking followed by nicotine and bupropion offspring. Increased heart rate and decreased cardiac output, stroke volume, and left ventricular percent posterior wall thickening were observed in smoking, nicotine, and bupropion offspring. The left ventricular mass was reduced in smoking and nicotine but not in bupropion offspring. Blood pressure was higher with decreased endothelium-dependent relaxation and exaggerated vascular contraction to angiotensin II in smoking and nicotine offspring, with more pronounced dysfunctions in smoking than nicotine offspring. Maternal bupropion did not impact offspring’s blood pressure, endothelium-dependent relaxation, and vascular contraction. In conclusion, maternal nicotine intervention adversely affects offspring’s cardiovascular outcomes, albeit less severely than continued smoking. However, bupropion causes cardiac derangement in offspring but does not adversely affect blood pressure and vascular function.
Similar content being viewed by others
References
Einarson A, Riordan S. Smoking in pregnancy and lactation: a review of risks and cessation strategies. Eur J Clin Pharmacol. 2009;65(4):325–330.
Rogers J. Tobacco and pregnancy. Reprod Toxicol. 2009;28(2):152–160.
Horta BL, Victora CG, Menezes AM, Halpern R, Barros FC. Low birthweight, preterm births and intrauterine growth retardation in relation to maternal smoking. Paediatr Perinat Epidemiol. 1997;11(2):140–151.
Antonopoulos CN, Sergentanis TN, Papadopoulou C, et al. Maternal smoking during pregnancy and childhood lymphoma: a metaanalysis. M J Cancer. 2011;129(11):2694–2703.
Durmus B, Kruithof CJ, Gillman MH, et al. Parental smoking during pregnancy, early growth, and risk of obesity in preschool children: the Generation R Study. Am J Clin Nutr. 2011;94(1):164–171.
Haynes A, Cooper MN, Bower C, Jones TW, Davis EA. Maternal smoking during pregnancy and the risk of childhood type 1 diabetes in Western Australia. Diabetologia. 2014;57(3):469–472.
Blake KV, Gurrin LC, Evans SF, et al. Maternal cigarette smoking during pregnancy, low birth weight and subsequent blood pressure in early childhood. Early Hum Dev. 2000;57(2):137–147.
Lawlor DA, Najman JM, Sterne J, Williams GM, Ebrahim S, Davey SG. Associations of parental, birth, and early life characteristics with systolic blood pressure at 5 years of age: findings from the Mater-University study of pregnancy and its outcomes. Circulation. 2004;110(16):2417–2423.
Oken E, Huh SY, Taveras EM, Rich-Edwards JW, Gillman MW. Associations of maternal prenatal smoking with child adiposity and blood pressure. Obes Res. 2005;13(11):2021–2028.
Lawlor DA, Smith GD. Early life determinants of adult blood pressure. Curr Opin Nephrol Hypertens. 2005;14(3):259–264.
Geerts CC, Grobbee DE, van der Ent CK, et al. Tobacco smoke exposure of pregnant mothers and blood pressure in their newborns: results from the wheezing illnesses study Leidsche Rijn Birth Cohort. Hypertension. 2007;50(3):572–578.
Hogberg L, Cnattingius S, Lundholm C, D’Onofrio BM, Langstrom N, Iliadou AN. Effects of maternal smoking during pregnancy on offspring blood pressure in late adolescence. J Hypertens. 2012;30(4):693–699.
Brion MJ, Leary SD, Smith GD, Ness AR. Similar associations of parental prenatal smoking suggest child blood pressure is not influenced by intrauterine effects. Hypertension. 2007;49(6):1422–1428.
Law CM, Shiell AW. Is blood pressure inversely related to birth weight? The strength of evidence from a systematic review of the literature. J Hypertens. 1996;14(8):935–941.
Whincup PH, Cook DG, Shaper AG. Early influences on blood pressure: a study of children aged 5-7 years. BMJ. 1989;299(6699):587–591.
Morley R, Leeson PC, Lister G, Lucas A. Maternal smoking and blood pressure in 7.5 to 8 year old offspring. Arch Dis Child. 1995;72(2):120–124.
Brion MJ, Leary SD, Lawlor DA, Smith GD, Ness AR. Modifiable maternal exposures and offspring blood pressure: a review of epidemiological studies of maternal age, diet, and smoking. Pediatr Res. 2008;63(6):593–598.
Breslau N. Psychiatric comorbidity of smoking and nicotine dependence. Behav Genet. 1995;25(2):95–101.
Lumley J, Chamberlain C, Dowswell T, Oliver S, Oakley L, Watson L. Interventions for promoting smoking cessation during pregnancy. Cochrane Database Syst Rev. 2009;(3):CD001055.
Filion KB, Abenhaim HA, Mottillo S, et al. The effect of smoking cessation counselling in pregnant women: a meta-analysis of randomised controlled trials. BJOG. 2011;118(12):1422–1428.
Wong S, Ordean A, Kahan M. Substance use in pregnancy. J Obstet Gynaecol Can. 2011;33(4):367–384.
Cooper S, Lewis S, Thornton JG, et al. The SNAP trial: a randomised placebo-controlled trial of nicotine replacement therapy in pregnancy-clinical effectiveness and safety until 2 years after delivery, with economic evaluation. Health Technol Assess. 2014;18(54):1–128.
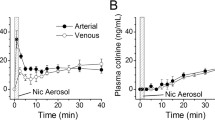
Oncken CA, Hardardottir H, Hatsukami DK, Lupo VR, Rodis JF, Smeltzer JS. Effects of transdermal nicotine or smoking on nicotine concentrations and maternal-fetal hemodynamics. Obstet Gynecol. 1997;90(4 pt 1):569–574.
Lindblad A, Marsal K, Andersson KE. Effect of nicotine on human fetal blood flow. Obstet Gynecol. 1988;72(3 pt 1): 371–382.
Windsor R, Oncken C, Henningfield J, Hartmann K, Edwards N. Behavioral and pharmacological treatment methods for pregnant smokers: issues for clinical practice. J Am Med Womens Assoc. 2000;55(5):304–310.
Swamy GK, Roelands JJ, Peterson BL, et al. Predictors of adverse events among pregnant smokers exposed in a nicotine replacement therapy trial. Am J Obstet Gynecol. 2009;201(4):354–357.
Xiao D, Xu Z, Huang X, Longo LD, Yang S, Zhang L. Prenatal gender-related nicotine exposure increases blood pressure response to angiotensin II in adult offspring. Hypertension. 2008;51(4):1239–1247.
Xiao D, Huang X, Lawrence J, Yang S, Zhang L. Fetal and neonatal nicotine exposure differentially regulates vascular contractility in adult male and female offspring. J Pharmacol Exp Ther. 2007;320(2):654–661.
Xiao D, Dasgupta C, Li Y, Huang X, Zhang L. Perinatal nicotine exposure increases angiotensin ii receptor-mediated vascular contractility in adult offspring. PLoS One. 2014;9(9):e108161.
Bruin JE, Gerstein HC, Holloway AC. Long-term consequences of fetal and neonatal nicotine exposure: a critical review. Toxicol Sci. 2010;116(2):364–374.
Xiao D, Wang L, Huang X, Li Y, Dasgupta C, Zhang L. Protective effect of antenatal antioxidant on nicotine-induced heart ischemia-sensitive phenotype in rat offspring. PLoS One. 2016;11(2):e0150557.
Xiao D, Huang X, Li Y, Dasgupta C, Wang L, Zhang L. Antenatal antioxidant prevents nicotine-mediated hypertensive response in rat adult offspring. Biol Reprod. 2015;93(3):66.
Xiao D, Huang X, Yang S, Zhang L. Direct effects of nicotine on contractility of the uterine artery in pregnancy. J Pharmacol Exp Ther. 2007;322(1):180–185.
Lawrence J, Xiao D, Xue Q, Rejali M, Yang S, Zhang L. Prenatal nicotine exposure increases heart susceptibility to ischemia/reper-fusion injury in adult offspring. J Pharmacol Exp Ther. 2008;324(1):331–341.
Stedman RL. The chemical composition of tobacco and tobacco smoke. Chem Rev. 1968;68(2):153–207.
Swauger JE, Steichen TJ, Murphy PA, Kinsler S. An analysis of the mainstream smoke chemistry of samples of the U.S. cigarette market acquired between 1995 and 2000. Regul Toxicol Pharmacol. 2002;35(2 pt 1):142–156.
Brose LS, McEwen A, West R. Association between nicotine replacement therapy use in pregnancy and smoking cessation. Drug Alcohol Depend. 2013;132(3):660–664.
Alwan S, Reefhuis J, Rasmussen SA, Friedman JM; National Birth Defects Prevention Study. Patterns of antidepressant medication use among pregnant women in a United States population. J Clin Pharmacol. 2011;51(2):264–270.
Hughes JR, Stead LF, Lancaster T. Antidepressants for smoking cessation. Cochrane Database Syst Rev. 2007;(1):CD000031.
Jorenby DE, Leischow SJ, Nides MA, et al. A controlled trial of sustained-release bupropion, a nicotine patch, or both for smoking cessation. N Engl J Med. 1999;340(9):685–691.
Chan B, Einarson A, Koren G. Effectiveness of bupropion for smoking cessation during pregnancy. J Addict Dis. 2005;24(2):19–23.
Paterson NE. Behavioural and pharmacological mechanisms of bupropion’s anti-smoking effects: recent preclinical and clinical insights. Eur J Pharmacol. 2009;603(1-3):1–11.
Slemmer JE, Martin BR, Damaj MI. Bupropion is a nicotinic antagonist. J Pharmacol Exp Ther. 2000;295(1):321–327.
Cressman AM, Pupco A, Kim E, Koren G, Bozzo P. Smoking cessation therapy during pregnancy. Can Fam Physician. 2012;58(5):525–527.
Coleman T, Chamberlain C, Davey MA, Cooper SE, LeonardiBee J. Pharmacological interventions for promoting smoking cessation during pregnancy. Cochrane Database Syst Rev. 2012;(9):CD010078.
Rigotti NA, Park ER, Chang Y, Regan S. Smoking cessation medication use among pregnant and postpartum smokers. Obstet Gynecol. 2008;111(2 pt 1):348–355.
Anderka M, Romitti PA, Sun L, Druschel C, Carmichael S, Shaw G; National Birth Defects Prevention Study. Patterns of tobacco exposure before and during pregnancy. Acta Obstet Gynecol Scand. 2010;89(4):505–514.
Nekhayeva IA, Nanovskaya TN, Pentel PR, Keyler DE, Hankins GD, Ahmed MS. Effects of nicotine-specific antibodies, Nic311 and Nic-IgG, on the transfer of nicotine across the human placenta. Biochem Pharmacol. 2005;70(11):1664–1672.
Earhart AD, Patrikeeva S, Wang X, et al. Transplacental transfer and metabolism of bupropion. J Matern Fetal Neonatal Med. 2010;23(5):409–416.
Wang X, Abdelrahman DR, Zharikova OL, et al. Bupropion metabolism by human placenta. Biochem Pharmacol. 2010;79(11):1684–1690.
Lichtensteiger W, Ribary U, Schlumpf M, Odermatt B, Widmer HR. Prenatal adverse effects of nicotine on the developing brain. Prog Brain Res. 1988;73:137–157.
Slotkin TA. Fetal nicotine or cocaine exposure: which one is worse? J Pharmacol Exp Ther. 1998;285(3):931–945.
Benowitz NL, Zevin S, Jacob P III. Sources of variability in nicotine and cotinine levels with use of nicotine nasal spray, transdermal nicotine, and cigarette smoking. Br J Clin Pharmacol. 1997;43(3):259–267.
Gariti P, Alterman AI, Barber W, Bedi N, Luck G, Cnaan A. Cotinine replacement levels for a 21 mg/day transdermal nicotine patch in an outpatient treatment setting. Drug Alcohol Depend. 1999;54(2):111–116.
Zhu AZ, Cox LS, Nollen N, et al. CYP2B6 and bupropion’s smoking-cessation pharmacology: the role of hydroxybupropion. Clin Pharmacol Ther. 2012;92(6):771–777.
Suckow RF, Smith TM, Perumal AS, Cooper TB. Pharmacokinetics of bupropion and metabolites in plasma and brain of rats, mice, and guinea pigs. Drug Metab Dispos. 1986;14(6):692–697.
Wang X, Vernikovskaya DI, Abdelrahman DR, Hankins GD, Ahmed MS, Nanovskaya TN. Simultaneous quantitative determination of bupropion and its three major metabolites in human umbilical cord plasma and placental tissue using high-performance liquid chromatography-tandem mass spectrometry. J Pharm Biomed Anal. 2012;70:320–329.
Peng M, Huang L, Xie Z, Huang WH, Askari A. Partial inhibition of Na+/K+-ATPase by ouabain induces the Ca2+-dependent expressions of early-response genes in cardiac myocytes. J Biol Chem. 1996;271(17):10372–10378.
Gopalakrishnan K, Morgan EE, Yerga-Woolwine S, et al. Augmented rififylin is a risk factor linked to aberrant cardiomyocyte function, short-QT interval and hypertension. Hypertension. 2011;57(4):764–771.
Webster DR, Patrick DL. Beating rate of isolated neonatal cardiomyocytes is regulated by the stable microtubule subset. Am J Physiol Heart Circ Physiol. 2000;278(5):H1653-H1661.
Sathishkumar K, Yallampalli U, Elkins R, Yallampalli C. Raf-1 kinase regulates smooth muscle contraction in the rat mesenteric arteries. J Vasc Res. 2010;47(5):384–398.
Poole AT, Vincent KL, Olson GL, et al. Effect of lactation on maternal postpartum cardiac function and adiposity: a murine model. Am J Obstet Gynecol. 2014;211(4):424.e1–e7.
Chinnathambi V, Yallampalli C, Sathishkumar K. Prenatal testosterone induces sex-specific dysfunction in endothelium-dependent relaxation pathways in adult male and female rats. Biol Reprod. 2013;89(4):1–9.
Chinnathambi V, Selvanesan BC, Vincent KL, et al. Elevated testosterone levels during rat pregnancy cause hypersensitivity to angiotensin II and attenuation of endothelium-dependent vasodilation in uterine arteries. Hypertension. 2014;64(2):405–414.
Andres RL, Day MC. Perinatal complications associated with maternal tobacco use. Semin Neonatol. 2000;5(3):231–241.
Abel EL. Smoking during pregnancy: a review of effects on growth and development of offspring. Hum Biol. 1980;52(4):593–625.
Perkins SL, Belcher JM, Livesey JF. A Canadian tertiary care centre study of maternal and umbilical cord cotinine levels as markers of smoking during pregnancy: relationship to neonatal effects. Can J Public Health. 1997;88(4):232–237.
De LN, Hyslop JR, Nicholson CJ, Morrison KM, Gerstein HC, Holloway AC. Postnatal metabolic and reproductive consequences of fetal and neonatal exposure to the smoking cessation drug bupropion. Reprod Sci. 2013;20(10):1156–1161.
Piasek M, Blanusa M, Kostial K, Laskey JW. Placental cadmium and progesterone concentrations in cigarette smokers. Reprod Toxicol. 2001;15(6):673–681.
Zhu BT, Cai MX, Spink DC, et al. Stimulatory effect of cigarette smoking on the 15 alpha-hydroxylation of estradiol by human term placenta. Clin Pharmacol Ther. 2002;71(5):311–324.
Pastrakuljic A, Derewlany LO, Koren G. Maternal cocaine use and cigarette smoking in pregnancy in relation to amino acid transport and fetal growth. Placenta. 1999;20(7):499–512.
Resnik R, Brink GW, Wilkes M. Catecholamine-mediated reduction in uterine blood flow after nicotine infusion in the pregnant ewe. J Clin Invest. 1979;63(6):1133–1136.
Lambers DS, Clark KE. The maternal and fetal physiologic effects of nicotine. Semin Perinatol. 1996;20(2):115–126.
Luck W, Nau H, Hansen R, Steldinger R. Extent of nicotine and cotinine transfer to the human fetus, placenta and amniotic fluid of smoking mothers. Dev Pharmacol Ther. 1985;8(6):384–395.
Fokina VM, West H, Oncken C, et al. Bupropion therapy during pregnancy: the drug and its major metabolites in umbilical cord plasma and amniotic fluid. Am J Obstet Gynecol. 2016;215(4):497.e1–7.
Quattrocki E, Baird A, Yurgelun-Todd D. Biological aspects of the link between smoking and depression. Harv Rev Psychiatry. 2000;8(3):99–110.
Pauly JR, Slotkin TA. Maternal tobacco smoking, nicotine replacement and neurobehavioural development. Acta Paediatr. 2008;97(10):1331–1337.
Janes AC, Jensen JE, Farmer SL, Frederick BD, Pizzagalli DA, Lukas SE. GABA levels in the dorsal anterior cingulate cortex associated with difficulty ignoring smoking-related cues in tobacco-dependent volunteers. Neuropsychopharmacology. 2013;38(6):1113–1120.
Oncken C, Kranzler H, O’Malley P, Gendreau P, Campbell WA. The effect of cigarette smoking on fetal heart rate characteristics. Obstet Gynecol. 2002;99(5 pt 1):751–755.
Feng Y, Caiping M, Li C, et al. Fetal and offspring arrhythmia following exposure to nicotine during pregnancy. J Appl Toxicol. 2010;30(1):53–58.
Jolma CD, Samson RA, Klewer SE, Donnerstein RL, Goldberg SJ. Acute cardiac effects of nicotine in healthy young adults. Echocardiography. 2002;19(6):443–448.
Leventhal K, Byatt N, Lundquist R. Fetal cardiac arrhythmia during bupropion use. Acta Obstet Gynecol Scand. 2010;89(7):980–981.
Bers DM. Calcium fluxes involved in control of cardiac myocyte contraction. Circ Res. 2000;87(4):275–281.
Ventura C, Zinellu E, Maninchedda E, Fadda M, Maioli M. Protein kinase C signaling transduces endorphin-primed cardiogenesis in GTR1 embryonic stem cells. Circ Res. 2003;92(6):617–622.
Steinberg SF, Goldberg M, Rybin VO. Protein kinase C isoform diversity in the heart. J Mol Cell Cardiol. 1995;27(1):141–153.
Kuwahara K, Wang Y, McAnally J, et al. TRPC6 fulfills a calcineurin signaling circuit during pathologic cardiac remodeling. J Clin Invest. 2006;116(12):3114–3126.
Wu X, Eder P, Chang B, Molkentin JD. TRPC channels are necessary mediators of pathologic cardiac hypertrophy. Proc Natl Acad Sci U S A. 2010;107(145):7000–7005.
Li N, Si B, Ju JF, et al. Nicotine induces cardiomyocyte hypertrophy through TRPC3-mediated Ca/NFAT signalling pathway. Can J Cardiol. 2016;32(10):1260.e1–1260.e10.
Brain KL, Trout SJ, Jackson VM, Dass N, Cunnane TC. Nicotine induces calcium spikes in single nerve terminal varicosities: a role for intracellular calcium stores. Neuroscience. 2001;106(2):395–403.
Abreu-Villaca Y, Seidler FJ, Slotkin TA. Does prenatal nicotine exposure sensitize the brain to nicotine-induced neurotoxicity in adolescence? Neuropsychopharmacology. 2004;29(8):1440–1450.
Chou HC, Chen CM. Maternal nicotine exposure during gestation and lactation induces cardiac remodeling in rat offspring. Reprod Toxicol. 2014;50:4–10.
Anblagan D, Jones NW, Costigan C, et al. Maternal smoking during pregnancy and fetal organ growth: a magnetic resonance imaging study. PLoS One. 2013;8(7):e67223.
Sullivan PM, Dervan LA, Reiger S, Buddhe S, Schwartz SM. Risk of congenital heart defects in the offspring of smoking mothers: a population-based study. J Pediatr. 2015;166(4):978–984.
Williams S, Poulton R. Twins and maternal smoking: ordeals for the fetal origins hypothesis? A cohort study. BMJ. 1999;318(7188):897–900.
Gao YJ, Holloway AC, Su LY, Takemori K, Lu C, Lee RM. Effects of fetal and neonatal exposure to nicotine on blood pressure and perivascular adipose tissue function in adult life. Eur J Pharmacol. 2008;590(1-3):264–268.
Pausova Z, Paus T, Sedova L, Beruhe J. Prenatal exposure to nicotine modifies kidney weight and blood pressure in genetically susceptible rats: a case of gene-environment interaction. Kidney Int. 2003;64(3):829–835.
Fox KA, Longo M, Tamayo E, et al. Sex-specific effects of nicotine exposure on developmental programming of blood pressure and vascular reactivity in the C57B1/6J mouse. Am J Obstet Gynecol. 2012;207(3):208.e1–9.
Hays JT, Ebbert JO. Bupropion for the treatment of tobacco dependence: guidelines for balancing risks and benefits. CNS Drugs. 2003;17(2):71–83.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gopalakrishnan, K., More, A.S., Hankins, G.D. et al. Postnatal Cardiovascular Consequences in the Offspring of Pregnant Rats Exposed to Smoking and Smoking Cessation Pharmacotherapies. Reprod. Sci. 24, 919–933 (2017). https://doi.org/10.1177/1933719116673199
Published:
Issue Date:
DOI: https://doi.org/10.1177/1933719116673199