Abstract
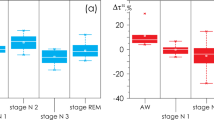
We performed a wavelet analysis of oscillatory dynamics in brain activity of patients with obstructive sleep apnoea (OSA) (\(N=10\), age \(52.8\pm 13\) years, median 49 years; male/female ratio: 73), compared with a group of apparently healthy participants (\(N=15\), age \(51. 5\pm 29.5\) years, median 42 years; malefemale ratio: 87), based on the calculation of patterns from electroencephalographic (EEG) signals of ***nighttime polysomnography (PSG) recordings. It was shown that there were no statistical differences in the number and duration of nocturnal sleep stages in patients of the two groups. The distributions of the number N and duration T of oscillatory wavelet patterns of EEG signals in bands \(\Delta f_i = [i; i+2]\), where i takes values from 2 to 38, have been estimated. Statistically significant differences in the characteristics of the distributions of the number and duration of patterns for the high-frequency bands \(\Delta f_{17}\) – \(\Delta f_{19}\) (32 – 38 Hz) are shown. It is demonstrated that estimation of the coordinates of the height and the value of the maximum point of the distribution of the considered quantitative characteristics of the patterns allows clustering of the EEG processing results and demonstrates the separation of the nocturnal sleep characteristics of OSA patients and healthy volunteers. Evaluation based on the Mann–Whitney U-test shows statistically significant differences between N and T patterns assessed from nocturnal EEG recordings. The number and duration of high-frequency patterns are significantly reduced in the EEG of OSA patients compared to essentially healthy participants. It is possible that such a change in high-frequency activity is related to known structural changes in the brain.





Similar content being viewed by others
Data availability
The datasets generated during and analysed during the current study are available from the corresponding author on reasonable request.
References
A. Babloyantz, J. Salazar, C. Nicolis, Evidence of chaotic dynamics of brain activity during the sleep cycle. Physics letters A 111(3), 152–156 (1985)
L. Ramlow, J. Sawicki, A. Zakharova, J. Hlinka, J.C. Claussen, E. Schöll, Partial synchronization in empirical brain networks as a model for unihemispheric sleep. Europhysics Letters 126(5), 50007 (2019)
Z. Zhou, B. Cai, G. Zhang, A. Zhang, V.D. Calhoun, Y.-P. Wang, Prediction and classification of sleep quality based on phase synchronization related whole-brain dynamic connectivity using resting state fMRI. NeuroImage 221, 117190 (2020)
A.I. Pack, U.J. Magalang, B. Singh, S.T. Kuna, B.T. Keenan, G. Maislin, Randomized clinical trials of cardiovascular disease in obstructive sleep apnea: understanding and overcoming bias. Sleep 44(2), 229 (2021)
C. André, S. Rehel, E. Kuhn, B. Landeau, I. Moulinet, E. Touron, V. Ourry, G. Le Du, F. Mézenge, C. Tomadesso et al., Association of sleep-disordered breathing with Alzheimer disease biomarkers in community-dwelling older adults: a secondary analysis of a randomized clinical trial. JAMA neurology 77(6), 716–724 (2020)
A.H. Babiloni, A. Bellemare, G. Beetz, S.-A. Vinet, M.O. Martel, G.J. Lavigne, L. De Beaumont, The effects of non-invasive brain stimulation on sleep disturbances among different neurological and neuropsychiatric conditions: A systematic review. Sleep medicine reviews 55, 101381 (2021)
L.D. Lisabeth, B.N. Sánchez, D. Lim, R.D. Chervin, E. Case, L.B. Morgenstern, S. Tower, D.L. Brown, Sleep-disordered breathing and poststroke outcomes. Annals of neurology 86(2), 241–250 (2019)
S. Baillieul, B. Revol, I. Jullian-Desayes, M. Joyeux-Faure, R. Tamisier, J.-L. Pépin, Diagnosis and management of central sleep apnea syndrome. Expert review of respiratory medicine 13(6), 545–557 (2019)
Y. Yeghiazarians, H. Jneid, J.R. Tietjens, S. Redline, D.L. Brown, N. El-Sherif, R. Mehra, B. Bozkurt, C.E. Ndumele, V.K. Somers et al., Obstructive sleep apnea and cardiovascular disease: a scientific statement from the American Heart Association. Circulation 144(3), 56–67 (2021)
M. Rodriguez-Fernandez, Circadian rhythm in metabolism and endocrinology. Frontiers in Endocrinology 14, 1263823 (2023)
M. Fusetti, A. Fioretti, M. Valenti, F. Masedu, M. Lauriello, M. Pagliarella, Cardiovascular and metabolic comorbidities in patients with obstructive sleep apnoea syndrome. Acta Otorhinolaryngologica Italica 32(5), 320 (2012)
M.T. Smith, J.A. Haythornthwaite, How do sleep disturbance and chronic pain inter-relate? Insights from the longitudinal and cognitive-behavioral clinical trials literature. Sleep medicine reviews 8(2), 119–132 (2004)
J.C. Cole, D. Dubois, M. Kosinski, Use of patient-reported sleep measures in clinical trials of pain treatment: a literature review and synthesis of current sleep measures and a conceptual model of sleep disturbance in pain. Clinical therapeutics 29(11), 2580–2588 (2007)
I.E.R. Marta, S.S. Baldan, A.F. Berton, M. Pavam, M.J.P.d. Silva, The effectiveness of therapeutic touch on pain, depression and sleep in patients with chronic pain: clinical trial. Revista da Escola de Enfermagem da USP 44, 1100–1106 (2010)
S. Redline, A. Azarbarzin, Y. Peker, Obstructive sleep apnoea heterogeneity and cardiovascular disease. Nature Reviews Cardiology, 1–14 (2023)
Z. Xu, Y. Wu, J. Tai, G. Feng, W. Ge, L. Zheng, Z. Zhou, X. Ni, Risk factors of obstructive sleep apnea syndrome in children. Journal of Otolaryngology-Head & Neck Surgery 49(1), 1–7 (2020)
E. Simou, J. Britton, J. Leonardi-Bee, Alcohol and the risk of sleep apnoea: A systematic review and meta-analysis. Sleep medicine 42, 38–46 (2018)
S. Jin, S. Jiang, A. Hu, Association between obstructive sleep apnea and non-alcoholic fatty liver disease: A systematic review and meta-analysis. Sleep and Breathing 22, 841–851 (2018)
C.W. Ong, D.M. O’Driscoll, H. Truby, M.T. Naughton, G.S. Hamilton, The reciprocal interaction between obesity and obstructive sleep apnoea. Sleep medicine reviews 17(2), 123–131 (2013)
G. Magliulo, G. Iannella, A. Ciofalo, A. Polimeni, M. De Vincentiis, B. Pasquariello, F. Montevecchi, C. Vicini, Nasal pathologies in patients with obstructive sleep apnoea. Acta Otorhinolaryngologica Italica 39(4), 250 (2019)
H.J. Münch, P. O’Leary, J. Bille, T. Kjaergaard, Oropharyngeal rhabdomyoma: the cause of severe sleep apnoea? BMJ Case Reports CP 13(2), 230949 (2020)
C.M. Cielo, C.L. Marcus, Obstructive sleep apnoea in children with craniofacial syndromes. Paediatric respiratory reviews 16(3), 189–196 (2015)
I. Alfonso, R. Luzondo, O. Papazian, Sleep disorders in the newborn. Medicina 67(6 Pt 1), 556–560 (2007)
J. Coleman, Disordered breathing during sleep in newborns, infants, and children: symptoms, diagnosis, and treatment. Otolaryngologic Clinics of North America 32(2), 211–222 (1999)
M.R. Mannarino, F. Di Filippo, M. Pirro, Obstructive sleep apnea syndrome. European journal of internal medicine 23(7), 586–593 (2012)
G. Andreou, F. Vlachos, K. Makanikas, Neurocognitive deficits in patients with obstructive sleep apnea syndrome (OSAS). Neuroscience, 93–114 (2012)
C. Lal, C. Strange, D. Bachman, Neurocognitive impairment in obstructive sleep apnea. Chest 141(6), 1601–1610 (2012)
H.K. Yaggi, J. Concato, W.N. Kernan, J.H. Lichtman, L.M. Brass, V. Mohsenin, Obstructive sleep apnea as a risk factor for stroke and death. New England Journal of Medicine 353(19), 2034–2041 (2005)
P. Mone, U. Kansakar, F. Varzideh, E. Boccalone, A. Lombardi, A. Pansini, G. Santulli, Epidemiology of obstructive sleep apnea: What is the contribution of hypertension and arterial stiffness? The Journal of Clinical Hypertension 24(4), 395 (2022)
S. Jehan, F. Zizi, S.R. Pandi-Perumal, S. Wall, E. Auguste, A.K. Myers, G. Jean-Louis, S.I. McFarlane, Obstructive sleep apnea and obesity: implications for public health. Sleep medicine and disorders: international journal 1(4) (2017)
A.U. Din, Z. Iqbal, M. Imran, Epidemiology of obstructive sleep apnea: A decade Long experience of Polysomnography in tertiary care hospital of Peshawar. Eur Respiratory Soc (2023)
B.J. Swihart, B. Caffo, K. Bandeen-Roche, N.M. Punjabi, Characterizing sleep structure using the hypnogram. Journal of Clinical Sleep Medicine 04(04), 349–355 (2008). https://doi.org/10.5664/jcsm.27236
P. Manjunatha, V.C. Rangappa, A. Varati, C.K. Narayanappa, Automatic detection of sleep stages using Deep Learning Algorithm. In: 2022 4th International Conference on Circuits, Control, Communication and Computing (I4C), pp. 436–439 (2022). https://doi.org/10.1109/I4C57141.2022.10057685
R.S. Rosenberg, S. Van Hout, The American Academy of Sleep Medicine inter-scorer reliability program: respiratory events. Journal of clinical sleep medicine 10(4), 447–454 (2014)
S. Chokroverty, Overview of sleep & sleep disorders. Indian Journal of Medical Research 131(2), 126–140 (2010)
J. Zhang, R. Yao, W. Ge, J. Gao, Orthogonal convolutional neural networks for automatic sleep stage classification based on single-channel EEG. Computer Methods and Programs in Biomedicine 183, 105089 (2020). https://doi.org/10.1016/j.cmpb.2019.105089
V.K. Kapur, D.H. Auckley, S. Chowdhuri, D.C. Kuhlmann, R. Mehra, K. Ramar, C.G. Harrod, Clinical practice guideline for diagnostic testing for adult obstructive sleep apnea: an American Academy of Sleep Medicine clinical practice guideline. Journal of clinical sleep medicine 13(3), 479–504 (2017)
N. Nachar et al., The Mann-Whitney U: A test for assessing whether two independent samples come from the same distribution. Tutorials in quantitative Methods for Psychology 4(1), 13–20 (2008)
A. Runnova, M. Zhuravlev, R. Ukolov, I. Blokhina, A. Dubrovski, N. Lezhnev, E. Sitnikova, E. Saranceva, A. Kiselev, A. Karavaev et al., Modified wavelet analysis of ECoG-pattern as promising tool for detection of the blood-brain barrier leakage. Scientific reports 11(1), 1–8 (2021)
M. Simonyan, A. Fisun, G. Afanaseva, O. Glushkovskaya-Semyachkina, I. Blokhina, A. Selskii, M. Zhuravlev, A. Runnova, Oscillatory wavelet-patterns in complex data: mutual estimation of frequencies and energy dynamics. The European Physical Journal Special Topics 232(5), 595–603 (2023)
M.O. Zhuravlev, A.O. Kiselev, A.E. Runnova, Study of the characteristics of EEG frequency patterns: the automatic marking of sleep stage without additional physiological signals. In: 2022 International Conference on Quality Management, Transport and Information Security, Information Technologies (IT &QM &IS), pp. 352–355 (2022). IEEE
K. Sergeev, A. Runnova, M. Zhuravlev, O. Kolokolov, N. Akimova, A. Kiselev, A. Titova, A. Slepnev, N. Semenova, T. Penzel, Wavelet skeletons in sleep eeg-monitoring as biomarkers of early diagnostics of mild cognitive impairment. Chaos: An Interdisciplinary Journal of Nonlinear Science 31(7) (2021)
P.J. Arnal, V. Thorey, E. Debellemaniere, M.E. Ballard, A. Bou Hernandez, A. Guillot, H. Jourde, M. Harris, M. Guillard, P. Van Beers, M. Chennaoui, F. Sauvet, The Dreem Headband compared to polysomnography for electroencephalographic signal acquisition and sleep staging. Sleep 43(11), 097 (2020) https://arxiv.org/abs/https://academic.oup.com/sleep/article-pdf/43/11/zsaa097/34499353/zsaa097.pdf. https://doi.org/10.1093/sleep/zsaa097
L.H. White, O.D. Lyons, A. Yadollahi, C.M. Ryan, T.D. Bradley, Night-to-night variability in obstructive sleep apnea severity: relationship to overnight rostral fluid shift. Journal of Clinical Sleep Medicine 11(2), 149–156 (2015)
L.R.A. Bittencourt, D. Suchecki, S. Tufik, C. Peres, S.M. Togeiro, M.D.C. Bagnato, L.E. Nery, The variability of the apnoea-hypopnoea index. Journal of sleep research 10(3), 245–251 (2001)
H. Danker-hopfe, P. Anderer, J. Zeitlhofer, M. Boeck, H. Dorn, G. Gruber, E. Heller, E. Loretz, D. Moser, S. Parapatics et al., Interrater reliability for sleep scoring according to the rechtschaffen & kales and the new AASM standard. Journal of sleep research 18(1), 74–84 (2009)
S. Saha, A. Bhattacharjee, S.A. Fattah, Automatic detection of sleep apnea events based on inter-band energy ratio obtained from multi-band EEG signal. Healthcare technology letters 6(3), 82–86 (2019)
H. Abdullah, G. Holland, I. Cosic, D. Cvetkovic, Correlation of sleep EEG frequency bands and heart rate variability. In: 2009 Annual International Conference of the IEEE Engineering in Medicine and Biology Society, pp. 5014–5017 (2009). IEEE
D. Alvarez, R. Hornero, J.V. Marcos, F. Del Campo, M. Lopez, Spectral analysis of electroencephalogram and oximetric signals in obstructive sleep apnea diagnosis. In: 2009 Annual International Conference of the IEEE Engineering in Medicine and Biology Society, pp. 400–403 (2009). IEEE
H.P. Bandla, D. Gozal, Dynamic changes in EEG spectra during obstructive apnea in children. Pediatric pulmonology 29(5), 359–365 (2000)
P.M. Macey, R. Kumar, M.A. Woo, E.M. Valladares, F.L. Yan-Go, R.M. Harper, Brain structural changes in obstructive sleep apnea. Sleep 31(7), 967–977 (2008)
M.E. Zimmerman, M.S. Aloia, A review of neuroimaging in obstructive sleep apnea. Journal of Clinical Sleep Medicine 2(04), 461–471 (2006)
M. Morrell, M. Jackson, G. Twigg, R. Ghiassi, D. McRobbie, R. Quest, H. Pardoe, G. Pell, D. Abbott, P. Rochford et al., Changes in brain morphology in patients with obstructive sleep apnoea. Thorax 65(10), 908–914 (2010)
Acknowledgements
Study has been supported by of the Government Procurement of the Russian Federation Ministry of Healthcare within the state assignment “Development of algorithms for recognising markers of breathing disorders during sleep in patients with various forms of cardiovascular pathology” No 122013100209-5 (2022–2024), performed in National Medical Research Center for Therapy and Preventive Medicine.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Runnova, A., Zhuravlev, M., Orlova, A. et al. Structural abnormalities of brain electrical activity during night sleep in patients with obstructive apnoea syndrome. Eur. Phys. J. Spec. Top. (2023). https://doi.org/10.1140/epjs/s11734-023-01056-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1140/epjs/s11734-023-01056-4