Abstract
This article summarizes the experience of managing patients with COVID-19-associated pneumonia treated in one of the intensive care units of a multidisciplinary hospital with and without a heated oxygen–helium mixture. It has been shown that the use of a heated oxygen–helium mixture in the complex therapy of pneumonia caused by SARS-CoV-2 is effective. A comparative analysis of the clinical manifestations of the disease and the results of laboratory tests in the main and control groups of patients confirm with a high degree of reliability the improvement of blood oxygenation, the normalization of the acid–base balance and the positive dynamics of the main parameters, which ultimately increases the efficacy and reduces the time of treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
The current generation of doctors and inhabitants of planet Earth have witnessed the COVID-19 pandemic—a new coronavirus infection. The pandemic is in full swing, and we still do not understand all the possible options for the course of the disease. Taking into account the fact that we have not previously dealt with such an infection, it is sometimes necessary, to test, by trial and error, therapeutic and preventive measures in the course of daily clinical activities.
Coronaviruses represent a family of 40 viruses, 7 of which cause various pathological changes in humans. Another part of the viruses from the coronavirus family usually affected animals, but then, in the process of evolution, they began to infect humans. Presumably, the primary human contact with a new coronavirus infection occurred in the wholesale market of animals and seafood in the city of Wuhan, Hubei Province, People’s Republic of China (PRC) [1].
At the end of 2019, Chinese scientists issued a statement about the emergence in Wuhan of a new coronavirus infection that mainly affects the respiratory organs of humans and is characterized by the development of severe respiratory failure in some patients. As early as on February 11, 2020, the study group of the WHO International Committee published an official statement, where they identified the cause of the severe acute respiratory syndrome caused by coronavirus 2 (SARS-CoV-2).
The study of the viral genome revealed recombination between the bat coronavirus and another virus, most likely a snake or other reptile virus. According to Chinese experts, bats infected reptiles with their virus, resulting in a new virus. It may be suggested with high probability that the “hosts” are the South Chinese multi-banded krait and the Chinese cobra [2].
A generalization of the data obtained in the PRC led to the conclusion that 80% of hospital admissions were associated with lung damage. At the same time, the highest mortality was registered among people over 85 years old (about 30%). More than 80% of lethal outcomes were associated with lung damage occurring with hypoxemia due to acute respiratory distress syndrome. People at high risk of infection, medical workers, travelers, elderly adults with a comorbid background in the form of concomitant diseases, as a rule, cardiovascular, oncological, diabetes mellitus, and chronic lung diseases [3], appeared to be susceptible to a severe form of the disease.
The main route of infection transmission is airborne. Contact transmission through food products and contaminated objects is also possible. There is evidence that the incubation period for the SARS-CoV-2 virus is an average of 5.2 days, and the incubation period ranges from 4 to 14 days. Chinese doctors have identified a pattern that the epidemic doubled approximately every 7 days and the basic reproductive number was 2.2, i.e., each patient infected approximately 2.2 patients. Information in available sources indicates that approximately 10–12% of cases were mild, and 15–20% of severe cases became fatal. Patients with mild illness recovered within two weeks, while patients with a severe course required 3 to 6 weeks to regain health [2]. Most of the deaths in clinics in China, Italy, and Spain were reported 2–6 weeks after the first symptoms of the disease appeared. There is evidence that patients with asymptomatic disease are able to transmit the infection within 2 to 8 days from the disease onset.
After the virus enters the body through the mucous membranes of the nose, eyes, oropharynx, esophagus, stomach, and small intestine, its penetration through cell barriers is observed using transport mechanisms similar to those of the human immunodeficiency virus, including penetration through epithelial barriers by being transported by monocytes and macrophages, which is relevant when considering the pathogenesis of lung damage during the development of systemic inflammation. In this connection, the human body can be regarded as an environment of the same permeability for the virus, where it can spread regardless of the route of entry. The virus releases its DNA into the cell, begins to multiply and penetrates into the alveoli. SARS-CoV-2 is able to affect alveolar type 2 cells (having the largest number of ACE2 receptors), causing disturbances in the synthesis of surfactant, lysozyme, interferon, and neutralize oxidants, as well as disrupt the transport of water and ions. Alveolocytes-2 occupy only 1/20 of the alveolar surface; however, they determine the balance of airiness and hydration of the lung tissue, being the most metabolically active cells, which is attractive for virus reproduction [1]. It is they that ultimately appear to be the most vulnerable in the development of an infectious lesion, which is similar to the previously described respiratory distress syndrome [4]. Unlike other coronavirus pathogens that cause seasonal acute respiratory viral infections, SARS-CoV-2 replicates in the upper respiratory tract without clinical manifestations in the first days. After a few days of the latent period, disturbances of metabolic processes in alveolar type II cells begin.
According to the results of the study of the treatment of COVID-19 in China obtained by the Wuhan Medical Expert Group, the clinical picture of those infected with COVID-19 allows the most common symptoms to be determined. Thus, the sufferers were observed to have the following symptoms: fever (≥38°C), 98% of cases; dry cough, sometimes with the discharge of a small amount of sputum, 76%; shortness of breath with a respiratory rate >22 per minute, 55%; severe weakness with myalgia, 44%; headaches, sputum, and diarrhea were observed in less than 30% of patients [5]. If they developed lung damage, all patients had X-ray-positive pneumonia with a characteristic ground-glass X-ray pattern. One-third of patients developed acute respiratory distress syndrome.
Depending on the intensity of the development of the disease, several scenarios are distinguished. Thus, the slow development of the disease is accompanied by a feeling of lack of air and shortness of breath. The rapid development is accompanied by complaints of lack of air, anxiety, acrocyanosis, shortness of breath and accelerated respiratory rate up to 30 respirations per minute, a moderate rise in blood pressure, blood saturation with oxygen below 90%, and arterial oxygen tension up to 70 mmHg. With severe development, profuse sweat, cyanosis, shortness of breath with a respiratory rate of up to 40 per minute, tachycardia, arterial hypertension, a decrease in saturation below 80%, and oxygen tension in the arterial blood up to 60 mmHg were observed. In hypoxic coma, consciousness is absent; convulsions appear; the skin is cyanotic, with a marble pattern; and blood pressure drops. Gastrointestinal symptoms were the leading complaint in less than half of patients with novel coronavirus infection. The incubation period in patients with dyspeptic symptoms and diarrhea was noted to increase to 9 days, while respiratory symptoms were absent in more than half of the patients [2].
Hypoxia has been found by researchers and practitioners to be the most common symptom of lung damage done by COVID-19. According to Russian and American scientists, the cause of hypoxia during SARS-CoV-2-associated infection is not only damage to pulmonary alveoli, but also to human blood cells. Penetrating through the nonstructural proteins orf1ab, ORF10, and ORF3 through the erythrocyte cell membrane, the virus displaces the ferrous atom from the porphyrin core of the beta chain of the hemoglobin molecule. Hemoglobin is destroyed inside the erythrocyte [5]. These mechanisms contribute to the occurrence of hypoxia and hypoxemia. In patients with COVID-19-associated pneumonia, blood saturation with oxygen decreases, which also increases inflammatory foci in the lungs. Iron is deposited in the interstitial tissue of the lungs, catalyzing oxidative processes. This is confirmed by an increase in the level of ferritin and lactate denitrogenase in patients and a decrease in the level of hemoglobin and erythrocytes. According to some scientists, intravascular hemolysis stimulates intravascular coagulation. One of the markers of this process is an increase in the D-dimer content and fibrinogen degradation products. In addition, the maximum D-dimer level, in combination with the clinical picture of respiratory failure, was noted in patients with a fatal outcome [6]. Computed tomography angiography of the pulmonary artery in these patients revealed signs of acute thromboembolism of small branches. Assessment of the state of the heart, kidneys, liver, and the central nervous system in patients with COVID-19-associated pneumonia was nonspecific and consistent with hypoxic changes characteristic of the development of respiratory failure [5].
One of the effective ways to compensate for hypoxia caused by damage to the lung tissue by coronavirus is oxygen inhalation [3]. Indications for oxygen therapy are signs of developing hypoxemia accompanied by a decrease in saturation (SpO2), oxygen tension in the arterial blood (PaO2), and an increase in its carbon dioxide content (PaCO2). The response to oxygen therapy is a crucial factor in assessing the course of acute respiratory failure in patients with COVID-19-associated pneumonia. There are three types of such a response. The first is progressive improvement. This course is usually observed in patients with mild or moderately severe hypoxia. With the elimination of hypoxemia, its clinical symptoms disappear; partial carbon dioxide tension progressively decreases. The second type of response is the most frequent; oxygenation contributes to a certain decrease in hypoxemia, but is also accompanied by a slight increase in PaCO2 until equilibrium is reached at a new level. The third type of response to oxygen therapy is the rapid progression of hypercapnia, for example, in severe depression of the respiratory center. Therefore, the use of oxygen therapy requires proper control of the CO2 concentration in the alveolar gas or PaCO2. Restoration of oxygen supply to tissues is an urgent problem in modern critical care medicine. The regulation and stabilization of gas exchange has become one of the leading factors in the management of multiple organ failure that develops in patients with lung damage due to a new coronavirus infection. In viral damage to the lungs, the compensatory mechanisms of the body are not capable of coping with extreme loads, thus resulting in hypoventilation, tachypnea, a decrease in volumetric blood flow rate, and hypoxia. With this pathology, the body often loses the ability to fully supply tissues with oxygen, which contributes to the disruption of energy metabolism in cells. Due to the intensification of oxidative processes against the background of oxygen deficiency, the need for oxygen increases, and this, in turn, impairs gas exchange. Restoration of gas exchange with an oxygen–air mixture and even pure oxygen against the background of using various methods of lung ventilation is not always a successful measure [1, 2]. The latter, among other things, is associated with the complexity of pathophysiological mechanisms and the versatility of homeostatic disorders during hypoxia caused by COVID-19.
In the 1990s, the staff of the Institute of Biomedical Problems headed by B.N. Pavlov proposed to use heated oxygen–helium mixtures in the complex therapy of pneumonia and bronchial obstructive disease [7]. The first clinical trials of the Geofarm device (Special Design Bureau under the Institute of Biomedical Problems, Russian Academy of Sciences) were performed at the Kirov Military Medical Academy, Ministry of Defense of the Russian Federation, at the Research Institute of Pulmonology under the Federal Biomedical Agency, and the Central Research Institute of Tuberculosis. Further development of the technology of helium inhalations with heated oxygen–helium mixtures was associated with the devices of the Ingalit series (Special Design Bureau under the Institute of Biomedical Problems) and with the development of a methodology for their use in conjunction with the Pirogov Russian National Medical University, Ministry of Health of Russia, and with the Central Clinical Hospital, Russian Academy of Sciences [8, 9].
Currently, Ingalit and a number of other devices are used to treat patients with COVID-19, for example, in City Clinical Hospital no. 52, at the Sklifisovskii Research Institute of Emergency Medicine [10], and in the Burdenko Main Military Clinical Hospital, Ministry of Defense of the Russian Federation; the technique is being tested in a number of medical universities and medical centers [11]. According to the opinion of Academician of the Russian Academy of Sciences A.G. Chuchalin expressed in the lecture Pneumonia-2020 on March 14, 2020 and in several other speeches, the evaluation of respiratory therapy methods for severe pneumonia shows the high efficacy of using the technology of heated artificial breathing mixtures based on oxygen and helium [10] both at the initial stage of respiratory failure in patients and when they are connected to and removed from mechanical ventilation.
Helium is an inert monatomic gas without color, smell, or taste. A mixture of helium and oxygen in a proportion of 70 to 30% or 60 to 40% is called heliox. Helium improves the ventilation function of the lungs, reduces respiratory resistance and, contributing to the regression of obstructive disorders, decreases the severity of hyperinflation of the lungs. Of great importance is the high diffusion capacity of helium [7], which makes it possible to increase the diffusion capacity of the alveolocapillary membrane and the lungs as a whole [12]. Improvement in ventilation and gas exchange decreases the load on the respiratory muscles, which has a positive effect on the counteraction of the respiratory muscle fatigue syndrome and helps to reduce the feeling of shortness of breath. It is very important that heliox does not have general and specific toxicity, mutagenicity, embryotoxicity, teratogenicity, carcinogenicity, does not cause allergies, and does not disrupt reproductive function. Despite the relatively long-standing use of heliox in medicine, which began as early as the 1930s, and its widespread use in diving to great depths [13, 14], there remains a need for additional research aimed at studying the effect of a heated oxygen–helium mixture on bronchial patency, the drainage function of the bronchi, the thermal regime of the body, and the combined use of helium inhalations with various drugs [10, 15, 16].
MATERIALS AND METHODS
In the midst of the pandemic the Rozanov Moscow Regional Hospital began to use inhalations with a heated oxygen–helium mixture (heliox) using a domestic Ingalit-V2-01 device. This device was designed and manufactured by one of the divisions of the Institute of Biomedical Problems, which is confirmed by RF patents 2072241 and 2232013 dated September 20, 1995 and June 4, 2001. The equipment includes a rack with a control unit that regulates the flow of the mixture, its temperature, and the inhalation time, a face mask, and an air duct with a heating element that heats the gas mixture to 100°C, as well as a cylinder with an oxygen–helium mixture. A preliminarily prepared gas mixture for inhalation was used at a concentration of 70% helium and 30% oxygen.
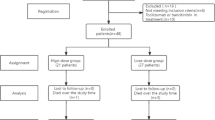
This study is based on a retrospective analysis of case histories of patients with SARS-CoV-2-associated pneumonia who were discharged from the hospital and stayed in the intensive care unit of the Center for Anesthesiology, Resuscitation, and Intensive Care. A total of 59 case histories were analyzed; the inclusion criteria were the moderate or severe condition of patients with spontaneous breathing; lesions of the lung tissue (radiological CT signs—2, 3, 4) accompanied by hyperthermia of the body; shortness of breath at rest; arterial and peripheral hypoxemia, hyperfibrinemia; and elevated acute-phase inflammatory reactions in the blood serum warranting urgent or emergency medical care. Statistical data were processed using nonparametric and parametric methods in the Statistica for Windows software v. 10. To describe quantitative features, calculations of the means and standard deviations were used. The dynamics of parameter values in the course of treatment within one group was assessed using the Wilcoxon test; intergroup differences were determined using the Mann–Whitney U-test. Differences were considered significant at p < 0.05.
The examination included the etiological diagnosis of COVID-19 made upon delivery of samples to the Rospotrebnadzor (Federal Service for Supervision of Consumer Rights Protection and Human Welfare) Vector laboratories, Mytishchi, Moscow oblast, using polymer chain reaction methods. In addition, a laboratory examination was performed, including a general (clinical) blood test with the determination of the level of erythrocytes, hemoglobin, hematocrit, leukocytes, platelets, and leukocyte formula; a biochemical blood test, including the determination of blood urea, creatinine, electrolytes, glucose, alanine aminotransferase, aspartate aminotransferase, bilirubin, albumin, lactate, lactate dehydrogenase, troponin, ferritin, and C-reactive protein (CRP); coagulogram parameters, including activated partial thromboplastin time (APTT), prothrombin time, fibrinogen, and D-dimer (quantitative method). Laboratory studies were conducted regularly with obligatory samplings on the 1st, 5th, and 10th days of therapy. To visualize the volume and degree of damage to the lung tissue, computed tomography of the lungs was performed according to a standard protocol without intravenous contrasting or radiography of the lungs in two projections.
Inhalation with heated heliox, depending on the patient’s condition, was carried out in the supine or sitting position through a mask and a mouthpiece; the temperature of the mixture at the outlet of the device heater was 95°C. Inhalations were used in accordance with the methodology developed by the Federal Department for Biomedical and Extreme Problems under the Ministry of Health of the Russian Federation: three intervals, including 5 min of inhalation and 5 min of rest [7]. Depending on the blood oxygen saturation level, up to four inhalations with a heated oxygen–helium mixture were performed daily. Subsequently, the inhalation time could be increased up to 10 min while maintaining 5-min rest intervals.
In addition, the main therapy for probable COVID-19-associated pneumonia with a verified polymerase chain reaction (PCR) was carried out in accordance with the temporary guidelines approved by the Minister of Health and the Chief Sanitary Doctor of the Russian Federation for the diagnosis, clinical symptoms, and treatment of COVID-19 [3]. The therapy included both pathogenetic and symptomatic therapy recommended by the protocols for the treatment of pulmonary coronavirus-associated lesions.
RESULTS AND DISCUSSION
All patients were divided into two groups. The first group (n = 28) included patients who received additional therapy with an oxygen–helium mixture. The second group included patients (n = 31) with viral lung damage who did not receive inhalation with heated heliox, but were treated in the intensive care unit (prior to the use of oxygen-helium therapy in the unit).
The average age of group 1 patients was 62.5 ± 18.3 years; men (15) accounted for 53.6%. Some patients had comorbidities. Thus, 32.1% (9) had type II diabetes mellitus, 57.1% (16) had stage 2–3 hypertension; 53.6% (15), coronary heart disease; 57.1% (16), signs of stage II–III chronic cardiovascular insufficiency; and 32.1% (9) had pathological changes in the kidneys with concomitant chronic renal failure.
For comparative evaluation of the effectiveness of the therapy used, complaints were monitored daily in patients with a time stamp of disappearance of symptoms from the moment they were admitted to the hospital. The most common complaints were distributed according to the severity (Table 1). Weakness and shortness of breath at rest were observed in 100%; cough, as a rule, dry or with a small amount of sputum, in 54 patients (98.3%); hyperthermia, in 50 (91.5%); chest pain (tightness), in 50 (84.7%); headaches, in 31 (52.5%); and bowel disorders, in 22 (37.3%) patients. Only the most frequent complaints and symptoms were evaluated and compared.
From the data in the table it follows that all the most frequent complaints and symptoms accompanying the disease associated with a new coronavirus infection in the first group (using heliox) were relieved significantly earlier than in the second control group.
The primary interpretation of the general blood test and coagulogram revealed that inflammatory indicators and markers of qualitative disorders of the blood coagulation system were in excess of normal values (Table 2). During the reexamination on the 5th and the 10th day, a significant decrease in the level of erythrocytes, ferritin, D-dimer, and the prothrombin index was noted, indicating the reversal of inflammatory and thrombodynamic changes under the influence of the therapy.
On admission, patients presented with hypoxemia characterized by a sharp decrease in blood oxygen tension and blood saturation with a decline in the oxygenation index (the ratio of partial oxygen pressure in the arterial blood to the oxygen fraction in the inhaled gas) (Table 3).
When treating patients using the Ingalit-2V-01 device according to the above method, we observed a distinct trend towards normalization of the above parameters by the 5th day of therapy against the background of normalization of the acid–base balance; by the 10th day, normalization of blood oxygen parameters was achieved. The average duration of the use of heliox was 5.2 ± 3.9 days, while the total treatment time in the clinical setting was 12.6 ± 4.1 days.
The average age of group 2 patients was 59.6 ± 14.1 years; men (23) in the group accounted for 79%. Some patients had comorbidities: 45.2% (14) had type I–II diabetes mellitus; 54.8% (17) were afflicted with stage 2–3 hypertension; 61.3% (19) had ischemic heart disease; 38.7% (12) had signs of stage II–III chronic cardiovascular insufficiency; and 29% (9) noted pathological changes in the urinary organs accompanied by chronic renal failure.
Changes in the general blood test and coagulogram parameter values shown in Table 4 were characteristic of a marked inflammatory process accompanied by blood coagulation disorders with manifestations of hypercoagulability. During the therapy, the intensity of the inflammatory process was observed to abate, while a significant decrease in CRP values occurred only on the 10th day of treatment compared with the data obtained on the 1st day of treatment. It should be noted that the continuing trend towards hypercoagulability persisted in most patients, despite anticoagulation therapy.
On admission, all group two patients were noted to have decreased blood oxygen tension, saturation, and oxygenation index values (Table 5). During treatment and continuous insufflation of humidified oxygen, most patients showed an increase in these parameter values. At 10 days of the therapy, they significantly differed from the data obtained during the primary examination. At the same time, the average duration of treatment for group 2 patients was longer by an average of 4 days constituting 16.7 ± 5.3 days.
When the results of the laboratory examination of patients from both groups on admission were compared, only the prothrombin index (PTI), ferritin, and D-dimer appeared to have significant differences. As an example, the PTI value was higher (p < 0.01); the ferritin value, lower (p < 0.05); and the D-dimer value, higher (p < 0.05) in group 1 patients.
On the 5th day of treatment, the results of a clinical blood test and blood oxygenation parameters showed significant differences between patients of both groups. The levels of erythrocytes, hemoglobin, and platelets in group 1 patients were significantly higher than those in group 2 patients (p < 0.05). Blood oxygenation parameters in group 1 patients with COVID-19-associated pneumonia normalized earlier than in group 2 patients. The level of arterial blood oxygen tension and the percentage of oxyhemoglobin were within the normal range and significantly higher than in group 2 (p < 0.01). The oxygenation index, being below the generally accepted norm (<350 mm Hg), was significantly higher than in group 2 patients.
On the 10th hospitalization day, significant differences were observed between patients with coronavirus-affected lung tissue receiving heliox inhalations and patients who did not receive a heated oxygen–helium mixture in the form of inhalations according to the following parameters: hemoglobin, erythrocytes, D-dimer, PTI, and oxygenation index were higher; activated partial thromboplastin time (APTT) and CRP were lower (p < 0.05), while PTI and APTT levels remained within the reference values. The persistence of the D-dimer level exceeding the reference values in patients of both groups was due to the presence of severe inflammatory manifestations and anticoagulant therapy.
CONCLUSIONS
(1) The high efficiency of the use of heated heliox in comparison with oxygen inhalations was manifested in a decrease in the severity of subjective and objective signs of the disease, such as general weakness, dyspnea and tachypnea, cough, and hyperthermia.
(2) The use of heated heliox reduced breathing resistance and improved the gas-transport function of the lungs, which was confirmed by an increase in PaO2 and an increase in SpO2.
(3) Inhalations with a heated oxygen–helium mixture during hypoxia combined with hypercapnia contributed to the normalization of the blood acid–base balance and a more marked decrease in inflammatory markers.
(4) The use of heliox in the complex therapy of patients with COVID-19 has reduced the hospital stay time not only in the intensive care unit, but also in hospital bed.
REFERENCES
Gromov, A.A., Kruchinina, M.V., and Rabko, A.V., Coronavirus disease COVID 19: unused treatment options, Ross. Med. Zh., 2020, no. 9, p. 1.
Rukovodstvo po profilaktike i lecheniyu novoi koronavirusnoi infektsii COVID-19 (Guidelines for the Prevention and Treatment of New Coronary Viral Infection COVID-19), Tingbo Liang, Ed., Moscow: The First Academic Clinic of Zhejiang University School of Medicine, 2020.
Vremennye metodicheskie rekomendatsii: profilaktika, diagnostika i lechenie novoi koronavirusnoi infektsii (COVID-19) (Temporary Methodic Guidelines: Prevention, Diagnosis and Treatment of New Coronavirus Infection (COVID-19)), Moscow, 2020. https://endoexpert.ru/ dokumenty-i-prikazy/versiya-8-ot-03-09-2020-vremennye-metodicheskie-rekomendatsii-profilaktika-diagnostika-i-lechenie-no/.
Kassil, V.L. and Savicheva, Yu.Yu., Ostryi respiratornyi distress-sindrom i gipoksemiya (Acute Respiratory Distress Syndrome and Hypoxemia), Moscow, 2016.
Cui, S., Chen, S., Li, X., et al., Prevalence of venous thromboembolism in patients with severe novel coronavirus pneumonia, J. Thromb. Haemostasis, 2020. https://doi.org/10.1111/jth.14830
Xu, Jin-fu, Wang, L., Zhao, L., et al., Risk assessment of venous thromboembolism and bleeding in COVID-19 patients, Preprint of Res. Square. https://doi.org/10.21203/rs.3.rs-18340/v1
Pavlov, B.N., Plaksin, S.E., and Boitsov, S.A., Metodika “Lechenie podogrevaemymi kislorodno-gelievymi smesyami ostrykh vospalitel’nykh i bronkhoobstruktivnykh zabolevanii legkikh s pomoshch’yu apparata “Ingalit” (Method “Treatment with Heated Oxygen–Helium Mixtures of Acute Inflammatory and Broncho-Obstructive Lung Diseases Using the “Inhalit” Device”), Approved by the Ministry of Health, RF 26.01.2001, Moscow, 2001.
Krasnovsky, A.L., Grigoriev, S.P., Alyokhin, A.I., and Potapov, V.N., Application of heated oxygen–helium mixture in the complex treatment of patients with community-acquired pneumonia, Klin. Med., 2013, no. 5, p. 38.
Krasnovsky, A.L., Grigoriev, S.P., Loshkareva, E.O., and Zolkina, I.V., Use of heliox in the treatment of patients with bronchopulmonary pathology, Ross. Med. Zh., 2012, no. 5, p. 46.
Shogenova, L.V., Varfolomeev, S.D., Bykov, V.I., et al., Effect of thermal helium–oxygen mixture on viral load in COVID-19, Pul’monologiya, 2020, vol. 30, no. 5, p. 533.
Shogenova, L.V., Effects of heliox as a working gas during inhalation of β2-agonists using a nebulizer in patients with acute bronchial asthma, Eff. Farmakoter., 2010, no. 27, p. 34.
Razumov, A.N., Ponomarenko, G.N., and Badtieva, V.A., Medical rehabilitation of patients with pneumonia associated with the new COVID-19 coronavirus infection, Vopr. Kurortol., Fizioter. Lech. Fiz. Kult., 2020, vol. 97, no. 3, p. 5.
Pavlov, B.N., D’yachenko, A.I., Shulagin, Y.A., et al., Studies of physiological effects of breathing heated oxygen—helium mixtures, Hum. Physiol., 2003, vol. 29, no. 5, p. 576. https://doi.org/10.1023/A:1025863900451
Dolina, O.A., Dubova, M.N., and Lokhvitsky, S.V., Use of helium in respiratory failure after lung surgery, Eksp. Khir. Anesteziol., 1966, no. 3, p. 77.
Pavlov, B.N., Smolin, V.V., Baranov, V.M., et al., Osnovy barofiziologii, vodolaznoi meditsiny, baroterapii i lechenie inertnymi gazami (Fundamentals of Barophysiology, Diving Medicine, Barotherapy, and Treatment with Inert Gases), Moscow, 2008.
Shogenova, L.V., Effects of heliox as a working gas during inhalation of β2-agonists using a nebulizer among patients with acute bronchial asthma, Nauka Prakt., p. 34.
Funding
Part of the study was carried out within the basic theme of the Russian Academy of Sciences, project no. 64.1.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
COMPLIANCE WITH ETHICAL STANDARDS
All procedures performed in studies involving human participants were in accordance with the biomedical ethics principles formulated in the 1964 Helsinki Declaration and its later amendments and approved by the local Bioethics Committee of the Institute of Biomedical Problems, Russian Academy of Sciences (Moscow).
CONFLICT OF INTERESTS
The authors declare that they do not have a conflict of interest.
INFORMED CONSENT
Each study participant provided a signed voluntary written informed consent after explanation of the potential risks and benefits, as well as the nature of the upcoming study to them.
Additional information
Translated by E. Babchenko
Rights and permissions
About this article
Cite this article
Manuilov, V.M., Suvorov, A.V., Kurkin, S.V. et al. Evaluation of the Efficiency of Oxygen–Helium Therapy for Patients with Covid-19-Associated Pneumonia. Hum Physiol 48, 863–870 (2022). https://doi.org/10.1134/S0362119722070143
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1134/S0362119722070143