Abstract
This review is the second part of the critical analysis of recent papers of Russian and other authors devoted to the study of the stabilometric parameters in postural control biofeedback training and rehabilitation, associated with psychological functions. The review presents the studies of postural control features in chronic pain syndrome, chronic fatigue syndrome, Parkinson’s disease, multiple sclerosis, and depression. The leading role of Russian researchers in the development and application of stabilometric biofeedback in the training of optimal functioning, rehabilitation, and correction of neurological disorders is noted. The paradigm of stabilometric biofeedback training of the cognitive and affective functions is offered.
Similar content being viewed by others
The key mechanism of postural control as one of the most common examples of sensorimotor integration is adaptive feedback [1, 2]. Hence it follows that the disruption of the connections between the perception and the processing of information during the execution of motor or cognitive tasks, causes disorders of central genesis. This determines the fundamental significance of studying the interrelationship between the impairments of perception (vestibular, visual, proprioceptive and support afferentation) and CNS (cognitive and affective functions) of postural control processes. In the past 30 years the study of this relationship has gained new relevance due to the development of informative technologies presupposing the use of more and more electronic gadgets in everyday life, which leads to a reduction in physical activity and changes in the pattern of cognitive activity [3]. In addition to the negative consequences of sedentary lifestyle, long-term sitting position or weakened support afferentation per se impairs not only physical musculoskeletal [4, 5], cardio-respiratory and vegetative [6], but also cognitive [7–9] and psychoemotional functions [10–12]. At the same time, if we take into account the negative effects of high-frequency electromagnetic waves caused by electronic devices and gadgets [8, 9], which are also associated with cognitive and psychoemotional disorders and even with the appearance of depressive symptoms as early as in the childhood and adolescence [13], the study of techniques for correcting impaired postural control as a result of weakened support afferentation in sedentary lifestyle becomes particularly important [4]. In addition, the relevance of studying the interrelationship between stabilometric and psychological parameters is due to the fact that balance training and posture control can be highly effective for elderly people, the relative number of which has been steadily increasing over the past 20 years, and the problem acquires global significance [14–81]. Finally, in the recent two years of the COVID-19 pandemic, a new need has arisen to investigate the interrelationship between impaired postural control (as a result of sedentary lifestyle), being a consequence of isolation and a complication of neurochemical processes in the brain after coronavirus infection [19, 20].
It is known that one of the most efficient approaches to neurophysiological nonmanipulative rehabilitation of impaired regulatory processes is to use the biofeedback technology as learning to recognize the state of optimal functioning [21]. Stabilometric biofeedback (BFB) presupposes postural control training with the involvement of feedback from the parameters of the center of pressure deviations (CoPD). We assume that stabilometric BFB will favor the correction and rehabilitation of not only biomechanical functions of equilibrium but also the cognitive and affective functions associated with impaired sensorimotor integration. However, the problems of using the objectively measured stabilometric characteristics of sensorimotor integration as BFB aimed at overcoming psychoemotional disorders and cognitive deficit have not yet been sufficiently investigated.
The present article continues the review of research into the psychophysiological mechanisms of postural control. The second part of this review presents the published data on the relationship between the impairments of postural stability and the disorders of psychological functions in chronic pain syndrome (such as fibromyalgia), chronic fatigue syndrome, multiple sclerosis, depressive states and disorders of cognitive functions. The review includes the currently known data on the efficiency of using stabilometric BFB aimed at the correction of neurological disorders and affecting psychoemotional functions.
Literature on the impact of impaired postural functions rehabilitation, as well as influence of postural control training with stabilometric biofeedback, on psychological characteristics was searched for by the following keywords: “postural control,” “stabilometry,” “sensorimotor integration,” “afferentation,” in combination with the words “cognitive functions,” “memory,” “attention,” “anxiety,” “depression,” “biofeedback,” “training,” and “rehabilitation.”
A literature search was conducted according to the recommendations of “Preferred Reporting Items for Systematic Reviews and Meta-Analyses” PRISMA and relied on the literature search described in the RELISH (RElevant LIterature SearcH) consensus [22]. The following databases were used: Web of Science, PubMed, Scopus and RSCI (to report on the results of Russian studies). The present review includes the results published in the articles with DOI (digital object identifier), completely corresponding to the keywords (Table 1). The review does not include the results of studies without psychological measurements or investigating individual cases without the control, as well as those published as abstracts only.
Psychophysiological Mechanisms of Postural Control Impairment
One of the methodological techniques used in the framework of cognitive neurosciences to study psychophysiological mechanisms is to compare the postural control variables under the normal conditions and their values in patients with CNS disorders [23–26] or dysfunction of sensory inputs [27], as well as with the borderline mental [28], phobic [29], anxiety and depressive disorders [30, 31].
Chronic pain syndrome and chronic fatigue syndrome. Chronic pain syndrome and chronic fatigue syndrome are overlapping and can influence disease etiology by involving the same regulatory mechanisms in CNS [32, 33]. This may have an effect on the central mechanisms, because motor learning requires the maintenance and renewal of internal psychomotor models [34]. Pain and fatigue perception can interfere with postural control. For example, the problems with maintaining balance have been found in patients with fibromyalgia and/or chronic fatigue syndrome [35, 36]. In patients suffering from chronic pain and fatigue, cognitive problems are combined with postural deficits [35–37]. Such patients often complain that they have to make more efforts to perform the common cognitive tasks [38, 39]. The possible consequences of chronic pain and fatigue with respect to motor functions are often underestimated but must be taken into consideration. In particular, E. Peper et al. and W.C. Tsai et al. have noted that the maintenance of correct upright posture with the support on the feet is associated not only with reduction of painful sensations in the neck, shoulders and back, but also with mood improvement, confidence, greater strength compared to the hunched sitting posture, which is associated, in addition to painful and unpleasant bodily sensations, with depressive state and negative emotions [40, 41].
In the work of O. Rasouli et al., the effects of adding cognitive task performance to the maintenance of the upright posture were compared in the groups of patients with chronic fatigue and fibromyalgia, as well as in the healthy participants group [42]. In patients, the frequency of CoPD proved to be lower compared to the control, demonstrating predominance of the involuntary component of postural control. While performing a competing cognitive task, the patients showed worse postural control parameters compared to healthy persons: the higher amplitudes and the lower frequencies of CoPD. At the same time, the differences in stabilometric parameters in the chronic fatigue compared to the control group were more marked [42]. The fact that the present study has revealed correlations between fatigue and postural control, but not pain, suggests the predominance of psychological but not reflex mechanism of impaired postural control in the chronic fatigue syndrome.
Attention deficit. Attention is an important factor in adequate motor commands organization, in particular, while maintaining balance [43]. This fact is confirmed by the proven deterioration of postural control in children with attention deficit [44]. The role of voluntary attention in postural control is studied using the “separated attention” models with the addition of a competing cognitive task, e.g., conversation while walking [45]. It would be logical to assume that the addition of a cognitive task while maintaining the upright posture will enhance the load of information processing in the CNS [46] and thereby reduce the ability to control balance. Such effect has been demonstrated in the study of elderly people with the increased risk of falling (the increase in the area of CoPD while performing a competing cognitive task) [47]. The increase in energy demand for simultaneous dual (motor + cognitive) tasks performance demonstrates that walking or maintaining postural stability requires the involvement of considerable cognitive resources in healthy elderly people [48] and/or in case of mental disorders with the early Alzheimer’s disease [49]. In the meantime, B. Kerr et al. [50] have established that postural control is impaired only when solving a spatial task but not a working memory task. These results suggest that the cognitive processing of precisely spatial tasks depends on the neuronal mechanisms of the vestibular but not on the nonspecific cortical activation in postural control [50]. The results of our study in patients with major depressive disorder [31] also showed that performance of a dual postural–psychomotor task not associated with spatial imagination was accompanied by postural control improvement with respect to the parameters of energy demands for balance maintenance, while in healthy persons it was unchanged or even reduced in case of task complication. It can be supposed that, in case of depression, the attention required to maintain balance was focused on the process of rumination (“preoccupation with negative thoughts”) instead of postural control; when performing a simple cognitive task, the attention was switched over to task performance, while balance was maintained automatically [31]. We assume that such attention switching technique can be useful for balance training in order to overcome depressive rumination.
Affective disorders. The studies with the involvement of psychiatric patients and patients with the vestibular disorder report the high comorbidity of vestibular dysfunctions and the symptoms of agoraphobia [51], panic attacks [52], and anxiety [53]. The results of M.S. Redfern et al. show that patients with anxiety disorders, especially with the space and motion phobia, are more dependent on visual afferentation while maintaining balance than in the absence of phobia [54]. This subgroup of patients can be exposed to the therapy with the involvement of stabilometric biofeedback, which uses visual inputs as a feedback signal.
The studies of the role of vestibular afferentation make it possible to reveal, at least partially, various neuronal mechanisms. C.D. Balaban et al. assume that the area of the parabrachial nucleus receiving afferent inputs from vestibular receptors contains the cells that respond to rotation of the body relative to the force of gravity. The parabrachial nucleus, with its reciprocal relationships with the central nucleus of the amygdala, the infralimbic cortex and the hypothalamus [53], is an important node in the primary network that processes the convergent vestibular, somatic and visceral information in order to mediate avoidance conditioning, anxiety and conditioned fear responses [55].
The noradrenergic and serotoninergic projections of vestibular nuclei also have parallel connections with the pathways of anxiety. The ceruleovestibular pathway originates in the locus coeruleus (LC) and provides regionally specialized noradrenergic input to the vestibular nuclei, which probably mediates the effects of alerting and vigilance on the sensitivity of vestibule–motor circuits. Both serotonergic and nonserotonergic pathways from the dorsal raphe nucleus also project differentially to the vestibular nuclei, while 5-HT (2A) receptors are expressed in amygdaloid and cortical targets of the parabrachial nucleus. It is proposed that the dorsal raphe nucleus pathway contributes to both the tradeoff between the motor and sensory (information gathering) aspects of responses to self-motion and the calibration of sensitivity of affective responses to aversive aspects of motion [56]. F. Mast et al. believe that the described neurophysiological model is a synthetic scheme for studying the neuromorphological and neurochemical bases of comorbidity of balance and anxiety disorders. Spatial transformations affect the parietal regions, body representation is associated with the somatosensory regions, and affective processes involve the insular and cingulated cortex, each of them receiving a vestibular signal [57]. Under certain circumstances, visual, vestibular and postural interactions act as a signal causing fear, similarly to what takes place in motion sickness, which then may be associated with particular stimuli or a situation, creating an association (e.g., phobia), or without association with any particular concomitant event (e.g., panic) [58]. Following this rationale, C.M. Coelho and C.D. Balaban have proposed to consider this subcategory of anxiety disorders as the one induced by visual-vestibular disorders and fears in the framework of DSM-V diagnostic criteria [59]. In the meantime, in spite of establishing the broad range of various vestibular cortical projections, their functions have yet been poorly studied.
Depression. The relationship between postural control and depression deserves special attention, as it was noted long ago that the major depressive disorder has a negative effect on the entire organism but not only on the psyche. Among the most severe manifestations of depression, there are motor symptoms; nevertheless, they are often ignored both in research and in clinical practice [60]. In spite of the fact that motor disorders attract much less attention in the assessment of depression, often they are a self-sufficient factor independent of affective, cognitive and neurovegetative components of this disorder [61–63]. The existing estimates of motor symptoms usually rely on subjective judgments made by physicians on the basis of observed or recalled behavior [64, 65]. In some studies, they begin to use more objective tools such as Timed Up and Go Test (TUGT) or dual motor-cognitive tasks [66–68].
At present, it is only known about single studies devoted to the relationship between the severity of depression and stabilometrically measured postural impairments [30, 31, 69]. However, such relationship has its neurobiological basis: postural control, similar to the regulation of emotional state, depends on the complex mechanisms of sensorimotor regulation involving the dopaminergic pathways, as well as the links between the basal ganglia and the prefrontal cortex [70], and the same mechanisms are involved in the development of major depressive disorder [71]. In addition, recent studies of the consequences of sedentary lifestyle (i.e., the weakened support afferentation) and isolation under conditions of the COVID-19 pandemic demonstrate an increase the number of depressive disorders, probably due to the impaired neurochemical and postural mechanisms of sensorimotor integration, which complement each other [19, 20].
Parkinson’s disease. Parkinson’s disease is also characterized by a combination of motor and nonmotor disorders, which affect life quality. Nonmotor symptoms such as apathy and depression are associated with locomotion problems, in particular, postural instability [72]. Apathy and depression have a clear anatomical link to cerebral structures and are usually manifested in case of damage to the prefrontal cortical areas and the cingulate gyrus [73]. The neuroanatomical bases of postural instability in Parkinson’s disease are less studied. However, all these manifestations (apathy, depression and postural instability) are related actually to the same neuronal pathways as depression. These are the pathways through the basal ganglia associated with dopamine deficiency. These manifestations are usually resistant to the L-DOPA therapy [74, 75]. Other common neurotransmitter pathways involve cholinergic and catecholaminergic fibers [76, 77].
Multiple sclerosis. In patients with multiple sclerosis, locomotor disorders are also combined with anxiety and depressive symptoms. Depression develops in almost half of multiple sclerosis patients at a particular stage of their lives [78]. According to the American Academy of Neurology, the efficacy of antidepressant therapy and/or group therapy in such patients is insufficient [79]. The meta-analysis performed by I. Ensari et al., reporting on the effects of physical exercise in depression, showed that such exposure had a slight but statistically significant effect with respect to reduction of depressive symptoms in multiple sclerosis patients [80]. Later, several reviews presented evidence in favor of the fact that the efficiency of nonpharmacological techniques aimed at an increase in physical activity for rehabilitation and prevention of depressive disorders did not reach a significant level [81, 82].
The available studies show that affective and cognitive disorders are invariably accompanied by impaired balance, posture and gait, when they are assessed by objective stabilometric methods [30, 31]. Impaired postural control probably passes from the main component of affective disorder (among young people) to the epiphenomenon of concomitant physical and cognitive decline (among elderly people).
Thus, disorders of attention, spatial memory, mood, and other cognitive and affective functions, which could be targets for stabilometric biofeedback, are described in literature as the psychophysiological correlates of impaired postural control. Among the stabilometric indices of these psychological functions, particular attention is focused on the rate of oscillations in the foot center of pressure in high-frequency bands as most predictive, with the possibility of using them for cognitive function training.
The above data suggest that the training of the voluntary element of postural control, i.e., performance of simple cognitive or psychomotor tasks while maintaining balance, can be appropriate for overcoming attention deficit, psychomotor retardation and psychoemotional disorders.
Application of Stabilometry in Affective Disorders Rehabilitation
The previous section of this review demonstrated the interrelationship between stabilometric, psychological and neurobiological characteristics of postural control under normal conditions and in differentent kind of disorders. However, in rehabilitation, emphasis is usually placed only on one sphere: either motor or emotional. Both Russian and foreign literature sources describe different approaches to postural rehabilitation. Most often, the efficiency of a set of physical exercises is investigated [30, 81–85], while stabilometry is used in combination with other motor tests only for diagnosing disorders.
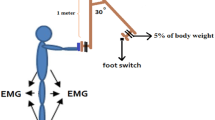
It is known that the biofeedback technology, due to neurophysiological principles of its organization, is the most efficient technique for regulation impairments correction and for training the optimal functioning [21, 86]. The neurophysiological basis of biofeedback procedure is related to anticipation, considered by Bernstein as a structural element of any human activity organization , which is closely associated with planning or creating a model that can be used in future reality [1, 34]. The result of the execution plan is presented in signs of the visual, acoustic, proprioceptive or even tactile feedback. These signals are a stimulus for training sensory awareness of a correctly performed activity, similar to motor training on the basis of sensory corrections [87]. Mental training with the involvement of feedback is aimed to activation of the brain integrative functions. As it has been mentioned previously, psychoemotional disorders have the sensorimotor disintegration origin, and postural disbalance is a particular case of sensorimotor disintegration. Therefore, the stabilometric biofeedback task must include the training of sensorimotor integration.
There is an interesting example of training the maintenance of the upright posture with biofeedback, using a head tilt sensor attached on the lower part of the neck. The sensor generates a feedback signal based on the changing tilt and curvature of the spine as vibration in case of hunching and tilting the head downward [88]. The authors have noted the efficiency of such training with respect to the quality of life, stress reduction and mood improvement in the group of healthy volunteers using this gadget. An important practical aspect of its application can be the convenience and simplicity of using it in the sitting position, which is especially relevant for people who actively use computers, pads, smartphones, etc.
Meantime, the literature search using simultaneously the keywords “depression,” “stabilometry,” and “biofeedback” did not yield any results (Table 2).
In Russian studies, the stabilometry method is actively used not only for diagnosing the balance function but also for its correction in the framework of neurological rehabilitation [28, 89–92], as well as for increasing efficiency in high performance sport [93, 94]. It should be noted that Russian authors very rarely take into account the psychoemotional state and peculiarities of cognitive functions of patients exposed to postural stability training. Quite often, the detailed descriptions of stabilometric parameters and training devices used, the presence of a control group of healthy subjects, the peculiarities of psychological examination are either not presented at all or described as secondary (e.g., a kind of neuropsychological examination without indicating the tests and assessing the dynamics of their changes as in [89], or assessment of the higher psychological functions in [90]). Therefore, researchers indicate the need for the common and strict methodological standards to overcome the deficiency of well-controlled studies and heterogeneity of electrophysiological and stabilometric data [21].
For example, high quality design and detailed description of techniques and results are presented by I.V. Krivoshey et al. [28] in the work with two control groups (healthy volunteers and patients with neuroses receiving no treatment), as well as three experimental groups of patients with neuroses undergoing rehabilitation with three different combinations of measures: the course of stabilometric biofeedback, the “Balance” course of specifically designed therapeutic exercises, and the course of stabilometric training with BFB and the “Balance” course of therapeutic exercises simultaneously. This study confirms the efficiency of the used correction techniques, which not only lead to functional motor changes but also have a psychotherapeutic effect, reduce anxiety and depression and are a guide to recovery. The results of clinical testing of patients from the BFB subgroup by the CoPD coordinates demonstrate the higher efficiency of biofeedback compared to the conventional training of postural control by physical exercise for improving mental health [28].
CONCLUSIONS
Thus, the analysis of Russian and foreign studies of the impaired postural control rehabilitation suggests that the improvement of qualitative and quantitative indices of the maintaining posture function with the use of stabilometric biofeedback and/or physical exercises aimed at postural control training is also accompanied by improvement of the psychoemotional state (reduced anxiety, depression, fatigue, apathy, and decrease in pain score) and, in general, the quality of life improvement. However, in these studies authors mostly did not take into account or did not present the data on the factors influencing the efficiency of biofeedback [21]: the initial individual neuroendophenotype, using dual tasks for redistribution of attention, the threshold level for feedback presentation, the time of feedback presentation delay, the available information on the progress and monitoring. Consequently, the efficiency of stabilometric biofeedback is determined by several psychophysiological mechanisms and situational circumstances that should be controlled and modified by researchers and experts.
REFERENCES
Bernshtein, N.A., New trends in physiology and their relationship with cybernetics, in Filosofskie voprosy fiziologii vysshei nervnoi deyatel’nosti i psikhologii (Philosophical Problems in Physiology of Higher Nervous Activity and Psychology), Moscow: Akad. Nauk SSSR, 1963, p. 299.
Anokhin, P.K., Sistemnye mekhanizmy vysshei nervnoi deyatel’nosti (System Mechanisms of Higher Nervous Activity), Moscow: Nauka, 1979.
Leiva, A.M., Martínez, M.A., Cristi-Montero, C., et al., Sedentary lifestyle is associated with metabolic and cardiovascular risk factors independent of physical activity, Rev. Med. Chil., 2017, vol. 145, no. 4, p. 458.
Arocha Rodulfo, J.I., Sedentary lifestyle a disease from XXI century, Clin. Invest. Arterioscler., 2019, vol. 31, no. 5, p. 233.
Amirova, L.E., Plehuna, A., Rukavishnikov, I.V., et al., Sharp changes in muscle tone in humans under simulated microgravity, Front. Physiol., 2021, vol. 12, art. ID 661922.
Mac Giollabhui, N., Alloy, L.B., Schweren, L.J.S., and Hartman, C.A., Investigating whether a combination of higher CRP and depression is differentially associated with worse executive functioning in a cohort of 43,896 adults, Brain Behav. Immun., 2021, vol. 96, p. 127.
Rodriguez-Ayllon, M., Cadenas-Sánchez, C., Estévez-López, F., et al., Role of physical activity and sedentary behavior in the mental health of preschoolers, children and adolescents: a systematic review and meta-analysis, Sports Med., 2019, vol. 49, no. 9, p. 1383.
Abou Khalil, G., Doré-Mazars, K., Senot, P., et al., Is it better to sit down, stand up or walk when performing memory and arithmetic activities? Exp. Brain Res., 2020, vol. 238, no. 11, p. 2487.
Hoare, E., Milton, K., Foster, C., and Allender, S., The associations between sedentary behavior and mental health among adolescents: a systematic review, Int. J. Behav. Nutr. Phys. Act., 2016, vol. 13, no. 1, p. 108.
Bickham, D.S., Hswen, Y., and Rich, M., Media use and depression: exposure, household rules, and symptoms among young adolescents in the USA, Int. J. Publ. Health, 2015, vol. 60, no. 2, p. 147.
Lee, E. and Kim, Y., Effect of university students’ sedentary behavior on stress, anxiety, and depression, Perspect. Psychiatr. Care, 2019, vol. 55, no. 2, p. 164.
Murri, M.B., Instrumental assessment of balance and gait in depression: a systematic review, Psychiatry Res., 2020, vol. 284, p. 112687.
Goldfield, G.S., Murray, M., Maras, D., et al., Screen time is associated with depressive symptomatology among obese adolescents: a HEARTY study, Eur. J. Pediatr., 2016, vol. 175, no. 7, p. 909.
Collado-Mateo, D., Lavín-Pérez, A.M., Peñacoba, C., et al., Key factors associated with adherence to physical exercise in patients with chronic diseases and older adults: an umbrella review, Int. J. Environ. Res. Publ. Health, 2021, vol. 18, no. 4, p. 2023.
Kim, S., Nussbaum, M.A., and Madigan, M.L., Direct parameterization of postural stability during quiet upright stance: effects of age and altered sensory conditions, J. Biomech., 2008, vol. 41, no. 2, p. 406.
Mehdizadeh, S., van Ooteghem, K., Gulka, H., et al., A systematic review of center of pressure measures to quantify gait changes in older adults, Exp. Gerontol., 2021, vol. 143, art. ID 111170.
Brauer, S.G., Woollacott, M., and Shumway-Cook, A., The influence of a concurrent cognitive task on the compensatory stepping response to a perturbation in balance-impaired and healthy elders, Gait Posture, 2002, vol. 15, no. 1, p. 83.
Kvelde, T., McVeigh, C., Toson, B., et al., Depressive symptomatology as a risk factor for falls in older people: Systematic review and meta-analysis, J. Am. Geriatr. Soc., 2013, vol. 61, no. 5, p. 694.
Schuch, F.B., Bulzing, R.A., Meyer, J., et al., Associations of moderate to vigorous physical activity and sedentary behavior with depressive and anxiety symptoms in self-isolating people during the COVID-19 pandemic: a cross-sectional survey in Brazil, Psychiatry Res., 2020, vol. 292, art. ID 113339.
Zheng, C., Huang, W.Y., Sheridan, S., et al., COVID‑19 pandemic brings a sedentary lifestyle in young adults: a cross-sectional and longitudinal study, Int. J. Environ. Res. Publ. Health, 2020, vol. 17, no. 17, p. 6035.
Ros, T., Enriquez-Geppert, S., Zotev, V., et al., Consensus on the reporting and experimental design of clinical and cognitive-behavioural neurofeedback studies (CRED-nf checklist), Brain, 2020, vol. 143, no. 6, p. 1674.
Brown, P., Tan, A.C., El-Esawi, M.A., et al., Large expert-curated database for benchmarking document similarity detection in biomedical literature search, Database, 2019, vol. 2019, p. baz085.
Zhavoronkova, L.A., Zharikova, A.V., and Maksakova, O.A., Integrating role of voluntary postural control recovery during rehabilitation of patients with traumatic brain injury, Neurosci. Behav. Physiol., 2012, vol. 42, no. 5, p. 486.
Chernikova, L.A., Ustinova, K.I., Ioffe, M.E., et al., The postural sway biofeedback in neurology, Sib. Nauchn. Med. Zh., 2004, vol. 24, no. 3, p. 85.
Shapovalenko, T.V., Sidyakina, I.V., Lyadov, K.V., and Ivanov, V.V., Prospective use of innovative BFB (biofeedback) technologies for the rehabilitation of patients after a stroke, Vestn. Vosstanov. Med., 2011, no. 3 (43), p. 2.
Mikhailova, L.V., Stabilometrics using biological feedback in medical rehabilitation of patients with cerebrovascular disease, Kurortnaya Med., 2018, no. 4, p. 57.
Zhutikov, D.L. and Usachev, V.I., Stabilometric diagnosis of ataxias caused by dysfunction of sensory inputs of the postural system, Manual’naya Ter., 2013, no. 3 (51), p. 28.
Krivoshei, I.V., Shinaev, N.N., Skvortsov, D.V., et al., Postural balance of patients with borderline mental disorders and its correction by biofeedback and exercise therapy, Ross. Psikhiatr. Zh., 2008, no. 1, p. 59.
Bronstein, A. and Lempert, T., Dizziness: A Practical Approach to Diagnosis and Management, New York: Cambridge Univ. Press, 2007.
Deschamps, T., Sauvaget, A., Pichot, A., et al., Posture-cognitive dual-tasking: A relevant marker of depression-related psychomotor retardation. An illustration of the positive impact of repetitive transcranial magnetic stimulation in patients with major depressive disorder, J. Psychiatr. Res., 2016, vol. 83, p. 86.
Aftanas, L.I., Bazanova, O.M., and Novozhilova, N.V., Posture-motor and posture-ideomotor dual-tasking: a putative marker of psychomotor retardation and depressive rumination in patients with major depressive disorder, Front. Hum. Neurosci., 2018, vol. 12, p. 108.
Ingvar, M., Learning mechanisms in pain chronification–teachings from placebo research, Pain, 2015, vol. 156, no. 1 (4), p. S18.
Öncü, J., Başoğlu, F., and Kuran, B., A comparison of impact of fatigue on cognitive, physical, and psychosocial status in patients with fibromyalgia and rheumatoid arthritis, Rheumatol. Int., 2013, vol. 33, no. 12, p. 3031.
Bernshtein, N.A., Ocherki po fiziologii dvizhenii i fiziologii aktivnosti (Essays on Physiology of Movement and Physiology of Activity), Moscow: Meditsina, 1966, p. 39.
da Silva Costa, I., Gamundí, A., Vivas Miranda, J.G., et al., Altered functional performance in patients with fibromyalgia, Front. Hum. Neurosci., 2017, vol. 11, p. 14.
Ash-Bernal, R., Wall, C., Komaroff, A.L., et al., Vestibular function test anomalies in patients with chronic fatigue syndrome, Acta Otolaryngol., 1995, vol. 115, no. 1, p. 9.
Neu, D., Mairesse, O., Montana, X., et al., Dimensions of pure chronic fatigue: psychophysical, cognitive and biological correlates in the chronic fatigue syndrome, Eur. J. Appl. Physiol., 2014, vol. 114, no. 9, p. 1841.
Capuron, L., Welberg, L., Heim, C., et al., Cognitive dysfunction relates to subjective report of mental fatigue in patients with chronic fatigue syndrome, Neuropsychopharmacology, 2006, vol. 31, no. 8, p. 1777.
Gelonch, O., Garolera, M., Valls, J., et al., Cognitive complaints in women with fibromyalgia: are they due to depression or to objective cognitive dysfunction? J. Clin. Exp. Neuropsychol., 2017, vol. 39, no. 10, p. 1013.
Peper, E., Booiman, A., Lin, I.M., and Harvey, R., Increase strength and mood with posture, Biofeedback, 2016, vol. 44, no. 2, p. 66.
Tsai, W.C., Lien, H.Y., Liu, W.Y., et al., Early and anticipatory postural adjustments in healthy subjects under stable and unstable sitting conditions, J. Electromyogr. Kinesiol., 2018, vol. 43, p. 21.
Rasouli, O., Fors, E.A., Vasseljen, O., and Stensdotter, A.K., A concurrent cognitive task does not perturb quiet standing in fibromyalgia and chronic fatigue syndrome, Pain Res. Manage., 2018, vol. 2018, art. ID 9014232.
Fraizer, E.V. and Mitra, S., Methodological and interpretive issues in posture-cognition dual-tasking in upright stance, Gait Posture, 2008, vol. 27, no. 2, p. 271.
Isaac, V., Olmedo, D., Aboitiz, F., and Delano, P.H., Altered cervical vestibular-evoked myogenic potential in children with attention deficit and hyperactivity disorder, Front. Neurol., 2017, vol. 8, p. 90.
Beauchet, O., Annweiler, C., Dubost, V., et al., Stops walking when talking: a predictor of falls in older adults? Eur. J. Neurol., 2009, vol. 16, no. 7, p. 786.
Slobounov, S., Hallett, M., Stanhope, S., and Shibasaki, H., Role of cerebral cortex in human postural control: an EEG study, Clin. Neurophysiol., 2005, vol. 116, no. 2, p. 315.
Kang, H.G. and Lipsitz, L.A., Stiffness control of balance during quiet standing and dual task in older adults: the MOBILIZE Boston Study, J. Neurophysiol., 2010, vol. 104, no. 6, p. 3510.
Woollacott, M. and Shumway-Cook, A., Attention and the control of posture and gait: a review of an emerging area of research, Gait Posture, 2002, vol. 16, no. 1, p. 1.
Rapp, T., Apouey, B.H., Senik, C., et al., The impact of institution use on the wellbeing of Alzheimer’s disease patients and their caregivers, Soc. Sci. Med., 2018, vol. 207, p. 1.
Kerr, B., Condon, S.M., and McDonald, L.A., Cognitive spatial processing and the regulation of posture, J. Exp. Psychol.: Hum. Percept. Perform., 1985, vol. 11, no. 5, p. 617.
Indovina, I., Conti, A., Lacquaniti, F., et al., Lower functional connectivity in vestibular-limbic networks in individuals with subclinical agoraphobia, Front. Neurol., 2019, vol. 10, p. 874.
Lilienfeld, S.O., Jacob, R.G., and Furman, J.M., Vestibular dysfunction followed by panic disorder with agoraphobia, J. Nerv. Ment. Dis., 1989, vol. 177, no. 11, p. 700.
Balaban, C.D., Neural substrates linking balance control and anxiety, Physiol. Behav., 2002, vol. 77, nos. 4–5, p. 469.
Redfern, M.S., Furman, J.M., and Jacob, R.G., Visually induced postural sway in anxiety disorders, J. Anxiety Disord., 2007, vol. 21, no. 5, p. 704.
McCandless, C.H. and Balaban, C.D., Parabrachial nucleus neuronal responses to off-vertical axis rotation in macaques, Exp. Brain Res., 2010, vol. 202, no. 2, p. 271.
McCall, A.A., Miller, D.M., and Balaban, C.D., Integration of vestibular and hindlimb inputs by vestibular nucleus neurons: multisensory influences on postural control, J. Neurophysiol., 2021, vol. 125, no. 4, p. 1095.
Mast, F.W., Preuss, N., Hartmann, M., and Grabherr, L., Spatial cognition, body representation and affective processes: the role of vestibular information beyond ocular reflexes and control of posture, Front. Integr. Neurosci., 2014, vol. 8, p. 44.
Meehan, A., Lewandowski, A., Weaver, L.K., et al., Prospective study of anxiety, post-traumatic stress and depression on postural control, gait, otolith and visuospatial function in military service members with persistent post-concussive symptoms, Undersea Hyperbaric Med., 2019, vol. 46, no. 3, p. 271.
Coelho, C.M. and Balaban, C.D., Visuo-vestibular contributions to anxiety and fear, Neurosci. Biobehav. Rev., 2015, vol. 48, p. 148.
Fried, E.I. and Nesse, R.M., The impact of individual depressive symptoms on impairment of psychosocial functioning, PLoS One, 2014, vol. 9, no. 2, p. e90311.
Drysdale, A.T., Grosenick, L., Downar, J., et al., Resting-state connectivity biomarkers define neurophysiological subtypes of depression, Nat. Med., 2017, vol. 23, no. 1, p. 28.
Rosenström, T. and Jokela, M., Reconsidering the definition of major depression based on collaborative psychiatric epidemiology surveys, J. Affective Disord., 2017, vol. 207, p. 38.
Vrieze, E., Demyttenaere, K., Bruffaerts, R., et al., Dimensions in major depressive disorder and their relevance for treatment outcome, J. Affective Disord., 2014, vol. 155, p. 35.
Fried, E.I., The 52 symptoms of major depression: Lack of content overlap among seven common depression scales, J. Affective Disord., 2017, vol. 208, p. 191.
Kendler, K.S., The genealogy of major depression: symptoms and signs of melancholia from 1880 to 1900, Mol. Psychiatry, 2017, vol. 22, no. 11, p. 1539.
Bayot, M., Dujardin, K., Tard, C., et al., The interaction between cognition and motor control: a theoretical framework for dual-task interference effects on posture, gait initiation, gait and turning, Neurophysiol. Clin., 2018, vol. 48, no. 6, p. 361.
Coni, A., Mellone, S., Colpo, M., et al., A factor analysis model of the instrumented Timed Up and Go test for physical capability assessment, Gait Posture, 2018, vol. 66, p. S11.
Schrijvers, D., Hulstijn, W., and Sabbe, B.G.C., Psychomotor symptoms in depression: a diagnostic, pathophysiological and therapeutic tool, J. Affective Disord., 2008, vol. 109, nos. 1–2, p. 1.
Doumas, M., Smolders, C., Brunfaut, E., et al., Dual task performance of working memory and postural control in major depressive disorder, Neuropsychology, 2012, vol. 26, no. 1, p. 110.
Takakusaki, K., Functional neuroanatomy for posture and gait control, J. Mov. Disord., 2017, vol. 10, no. 1, p. 1.
Walther, S., Bernard, J.A., Mittal, V.A., and Shankman, S.A., The utility of an RDoC motor domain to understand psychomotor symptoms in depression, Psychol. Med., 2019, vol. 49, no. 5, p. 212.
Martinez-Martin, P., Rodriguez-Blazquez, C., Kurtis, M.M., et al., The impact of non-motor symptoms on health related quality of life of patients with Parkinson’s disease, Mov. Disord., 2011, vol. 26, no. 3, p. 399.
Reijnders, J.S., Ehrt, U., Lousberg, R., et al., The association between motor subtypes and psychopathology in Parkinson’s disease, Parkinsonism Relat. Disord., 2009, vol. 15, no. 5, p. 379.
Gallagher, D.A. and Schrag, A., Psychosis, apathy, depression and anxiety in Parkinson’s disease, Neurobiol. Dis., 2012, vol. 46, no. 3, p. 581.
Beuter, A., Hernandez, R., Rigal, R., et al., Postural sway and effect of levodopa in early Parkinson’s disease, Can. J. Neurol. Sci., 2008, vol. 35, no. 1, p. 65.
Yarnall, A., Rochester, L., and Burn, D.J., The interplay of cholinergic function, attention, and falls in Parkinson’s disease, Mov. Disord., 2011, vol. 26, no. 14, p. 2496.
Grimbergen, Y.A., Langston, J.W., Roos, R.A., and Bloem, B.R., Postural instability in Parkinson’s disease: the adrenergic hypothesis and the locus coeruleus, Expert Rev. Neurother., 2009, vol. 9, no. 2, p. 279.
Tauil, C.B., Ramari, C., Da Silva, F.M., et al., The impact of physical functions on depressive symptoms in people with multiple sclerosis, Arq. Neuro-Psiquiatr., 2021, vol. 79, no. 1, p. 44.
Minden, S.L., Feinstein, A., Kalb, R.C., et al., Evidence-based guideline: assessment and management of psychiatric disorders in individuals with MS: report of the Guideline Development Subcommittee of the American Academy of Neurology, Neurology, 2014, vol. 82, no. 2, p. 174.
Ensari, I., Motl, R.W., and Pilutti, L.A., Exercise training improves depressive symptoms in people with multiple sclerosis: results of a meta-analysis, J. Psychosomatic Res., 2014, vol. 76, no. 6, p. 465.
Gul’tyaeva, V.V., Zinchenko, M.I., Uryumtsev, D.Yu., et al., Exercise for depression treatment. Physiological mechanisms, Zh. Nevrol. Psikhiatr. im. S.S. Korsakova, 2019, vol. 119, no. 7, p. 112.
Kandola, A., Ashdown-Franks, G., Hendrikse, J., et al., Physical activity and depression: Towards understanding the antidepressant mechanisms of physical activity, Neurosci. Biobehav. Rev., 2019, vol. 107, p. 525.
Ozgen, G., Karapolat, H., Akkoc, Y., and Yuceyar, N., Is customized vestibular rehabilitation effective in patients with multiple sclerosis? A randomized controlled trial, Eur. J. Phys. Rehabil. Med., 2016, vol. 52, no. 4, p. 466.
Sepúlveda de Andrade Mesquita, L., Texeira de Carvalho, F., Sepúlveda de Andrade Freire, L., et al., Effects of two exercise protocols on postural balance of elderly women: a randomized controlled trial, BMC Geriatr., 2015, vol. 15, p. 61.
Hebert, J.R., Corboy, J.R., Manago, M.M., and Schenkman, M., Effects of vestibular rehabilitation on multiple sclerosis–related fatigue and upright postural control: a randomized controlled trial, Phys. Ther., 2011, vol. 91, no. 8, p. 1166.
Sitaram, R., Ros, T., Stoeckel, L., et al., Closed-loop brain training: the science of neurofeedback, Nat. Rev. Neurosci., 2017, vol. 18, no. 2, p. 86.
Bernshtein, N.A., The relationship between coordination and localization, Arkh. Biol. Nauk, 1935, vol. 38, no. 1, p. 18.
Harvey, R.H., Peper, E., Mason, L., and Joy, M., Effect of posture feedback training on health, Appl. Psychophysiol. Biofeedback, 2020, vol. 45, no. 2, p. 59.
Bofanova, N.S., Diagnostics of movement disorders and the rehabilitation of patients with the consequences of traumatic brain injury using the stabilometric method, Vestn. Nov. Med. Tekhnol., 2013, no. 1, p. 118.
Mel’nikova, E.A., Rud’, I.M., and Rassulova, M.A., Stabilization training with biofeedback in the rehabilitation of patients with diseases of the musculoskeletal system, Doktor.Ru, 2019, no. 1 (156), p. 53.
Kubryak, O.V., Grokhovskii, S.S., Isakova, E.V., and Kotov, S.V., Biologicheskaya obratnaya svyaz’ po opornoi reaktsii: metodologiya i terapevticheskie aspekty (Support Response Biofeedback: Methods and Therapeutic Aspects), Moscow: Maska, 2015.
Sliva, A.S., Voinov, I.D., and Sliva, S.S., Development of methods and means of computer stabilography, Izv. Yuzh. Fed. Univ., Tekh. Nauki, 2010, no. 9 (110), p. 158.
Napalkov, D.A., Ratmanova, P.O., and Kolikov, M.B., Apparatnye metody diagnostiki i korrektsii funktsional’nogo sostoyaniya strelka (Machine Methods for Diagnostics and Correction of the Functional State of the Shooter), Moscow: MAKS Press, 2009.
Shilenok, V.V., Training of stability in the shooter-weapon-target system in young bullet shooters based on operational stabilometry data, Uch. Zap. Univ. im. P.F. Lesgafta, 2019, no. 4 (170), p. 367.
Funding
The work was supported by the federal budget for fundamental research works (no. AAAA-A21-121011990039-2) and partially by the Russian Foundation for Basic Research (projects no. 19-013-00317a and no. 20-113-50129\20).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
CONFLICT OF INTERESTS
The authors declare that they have no conflict of interest.
COMPLIANCE WITH ETHICAL STANDARDS
This work does not contain any studies involving animals or human subjects performed by any of the authors.
Additional information
Translated by E. Makeeva
Rights and permissions
About this article
Cite this article
Bazanova, O.M., Kovaleva, A.V. Stabilometric Biofeedback Training in Cognitive and Affective Function Improvement. Contribution of the Russian Scientific School. Part II. Hum Physiol 48, 271–284 (2022). https://doi.org/10.1134/S0362119722030021
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1134/S0362119722030021