Abstract—
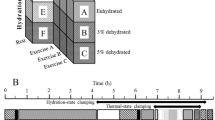
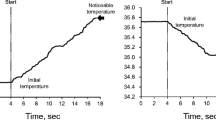
Adaptive shifts in systemic hemodynamic parameters and energy consumption were evaluated in 15 healthy young men in response to a single procedure of passive hyperthermia (PH) and during a course of ten such procedures. PH procedures with a duration of 40 min were performed in an infrared body heating capsule at 65–80°C, with the head remaining outside the capsule. Heart rate, blood pressure, and SрО2 were analyzed. Oxygen and energy consumption were measured by indirect calorimetry. The sweating rate and the physiological strain index (PSI) were calculated. It was found that PH procedures were accompanied by an increase in energy consumption (in comparison with placebo procedures), but without a pronounced stress response of systemic hemodynamics. PSI values during PH corresponded to moderate heat stress. During the course, adaptive shifts occurred in the form of a decrease in energy consumption and an increase in the sweating rate. In the tenth procedure the relationship between the degree of increase in body temperature and the level of energy consumption was revealed.




Similar content being viewed by others
REFERENCES
Cohen, M., Turning up the heat on COVID-19: heat as a therapeutic intervention, F1000Research, 2020, vol. 9, p. 292.
Heathcote, S.L., Hassmén, P., Zhou, S., and Stevens, C.J., Passive heating: reviewing practical heat acclimation strategies for endurance athletes, Front. Physiol., 2018, vol. 9, p. 1851.
Ihsan, M., Périard, J.D., and Racinais, S., Integrating heat training in the rehabilitation toolbox for the injured athlete, Front. Physiol., 2019, vol. 10, p. 1488.
Glazachev, O.S., Kofler, W., Dudnik, E.N., et al., Impact of adaptation to passive hyperthermia on aerobic performance and cardio-respiratory endurance in amateur athletes, Hum. Physiol., 2020, vol. 46, no. 1, p. 66.
Hussain, J. and Cohen, M., Clinical effects of regular dry sauna bathing: a systematic review, Evidence-Based Complementary Altern. Med., 2018, vol. 2018, art. ID 1857413.
Brunt, V.E., Howard, M.J., Francisco, M.A., et al., Passive heat therapy improves endothelial function, arterial stiffness and blood pressure in sedentary humans, J. Physiol., 2016, vol. 594, no. 18, p. 5329.
Gravel, H., Behzadi, P., Cardinal, S., et al., Acute vascular benefits of Finnish sauna bathing in patients with stable coronary artery disease, Can. J. Cardiol., 2021, vol. 37, no. 3, p. 493.
Kampmann, B. and Bröde, P., Heat acclimation does not modify Q10 and thermal cardiac reactivity, Front. Physiol., 2019, vol. 10, p. 1524.
Podstawski, R., Borysławski, K., Clark, C.C.T., et al., Correlations between repeated use of dry sauna for 4 × 10 min, physiological parameters, anthropometric features, and body composition in young sedentary and overweight men: health implications, Biomed. Res. Int., 2019, vol. 2019, art. ID 7535140.
Kim, K., Monroe, J.C., Gavin, T.P., and Roseguini, B.T., Skeletal muscle adaptations to heat therapy, J. Appl. Physiol., 2020, vol. 128, no. 6, p. 1635.
Gryka, D., Pilch, W.B., Czerwińska-Ledwig, O.M., et al., The influence of Finnish sauna treatments on the concentrations of nitric oxide, 3-nitrotyrosine and selected markers of oxidative status in training and non-training men, Int. J. Occup. Med. Environ. Health, 2020, vol. 33, no. 2, p. 173.
Pilch, W., Szyguła, Z., Klimek, A., et al., Changes in the lipid profile of blood serum in women taking sauna baths of various duration, Int. J. Occup. Med. Environ. Health, 2010, vol. 23, no. 2, p. 167.
Bakulin, V.S., Makarov, V.I., Bogomolova, M.M., and Panina, N.G., Physiological criteria for regulation of the level of hyperthermic effects of the sauna, Vestn. Volgograd. Gos. Med. Univ., 2007, vol. 3, no. 23, p. 6.
Glazachev, O.S., Kryzhanovskaya, S.Yu., Dud-nik, E.N., et al., Passive heat acclimation: influence on the subjective quality of life, anxiety, and the level of the brain-derived neurotrophic factor (BDNF), Ross. Fiziol. Zh. im. I.M. Sechenova, 2019, vol. 105, no. 5, p. 544.
Nakata, H., Namba, M., Kakigi, R., and Shibasaki, M., Effects of face/head and whole-body cooling during passive heat stress on human somatosensory processing, Am. J. Physiol.: Regul. Integr. Comp Physiol., 2017, vol. 312, no. 6, p. 996.
Ketelhut, S. and Ketelhut, R.G., The blood pressure and heart rate during sauna bath correspond to cardiac responses during submaximal dynamic exercise, Complementary Ther. Med., 2019, vol. 44, p. 218.
Li, Z., Jiang, W., Chen, Y., et al., Acute and short-term efficacy of sauna treatment on cardiovascular function: a meta-analysis, Eur. J. Cardiovasc. Nurs., 2020, vol. 20, no. 2, p. 96.
Mang, Z.A., Fennel, Z.I., Realzola, R.A., et al., Heat acclimation during low-intensity exercise increases V O2max and Hsp72, but not markers of mitochondrial biogenesis and oxidative phosphorylation in skeletal tissue, Exp. Physiol., 2021, vol. 106, no. 1. P. 290.
Pallubinsky, H., Phielix, E., Dautzenberg, B., et al., Passive exposure to heat improves glucose metabolism in overweight humans, Acta Physiol., 2020, vol. 229, no. 4, p. 1.
Pallubinsky, H., Schellen, L., Kingma, B.R.M., et al., Thermophysiological adaptations to passive mild heat acclimation, Temperature, 2017, vol. 4, no. 2, p. 176.
Moran, D.S., Shitzer, A., and Pandolf, K.B., A physiological strain index to evaluate heat stress, Am. J. Physiol.: Regul. Integr. Comp. Physiol., 1998, vol. 275, no. 1, p. R129.
Périard, J.D., Travers, G.J.S., Racinais, S., and Sawka, M.N., Cardiovascular adaptations supporting human exercise-heat acclimation, Auton. Neurosci., 2016, vol. 196, p. 52.
Zinchuk, V.V. and Zhadko, D.D., The effect of a sauna on blood oxygen transport and the prooxidant-antioxidant balance in untrained subjects, Hum. Physiol., 2012, vol. 38, no. 5, p. 548.
Litvitskii, P.F., Thermal dysbalance of the body: hyperthermia, hyperthermic reactions, heat stroke, and sunstroke, Vopr. Sovrem. Pediatrii, 2010, vol. 9, no. 1, p. 96.
Laukkanen, T., Kunutsor, S.K., Zaccardi, F., et al., Acute effects of sauna bathing on cardiovascular function, J. Hum. Hypertens., 2018, vol. 32, no. 2, p. 129.
Dubé, P.-A., Imbeau, D., Dubeau, D., and Auger, I., Worker heat stress prevention and work metabolism estimation: comparing two assessment methods of the heart rate thermal component, Ergonomics, 2019, vol. 62, no. 8, p. 1066.
Kampmann, B. and Bröde, P., Metabolic costs of physiological heat stress responses—Q10 coefficients relating oxygen consumption to body temperature, Extreme Physiol. Med., 2015, vol. 4, p. A103.
Tomiyama, C., Watanabe, M., Honma, T., et al., The effect of repetitive mild hyperthermia on body temperature, the autonomic nervous system, and innate and adaptive immunity, Biomed. Res., 2015, vol. 36, no. 2, p. 135.
Klous, L., De Ruiter, C., Alkemade, P., et al., Sweat rate and sweat composition during heat acclimation, J. Therm. Biol., 2020, vol. 93, p. 102697.
ACKNOWLEDGMENTS
We are grateful to all the volunteers who participating in the study, as well as Sybaritic Inc. (United States) for the Alfa Basic thermal capsules provided free of charge for hyperthermic procedures. The company and its representatives were not involved in the study design, data collection, analysis and interpretation, and preparation of the publication.
Funding
This work was in part supported by the Russian Foundation for Basic Research, project no. 19-013-00465 A “Direct and Crossover Effects of Adaptation to Systemic Hyperthermia: Influence on the Quality of Life, Neurohormonal and Psychophysiological Status of a Person.”
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
All procedures performed in studies involving human participants were in accordance with the biomedical ethics principles formulated in the 1964 Helsinki Declaration and its later amendments and approved by the local bioethical committee of the Sechenov First Moscow State Medical University (Sechenov University) (Moscow).
Conflict of interests. The authors declare that they have no conflict of interest.
Informed consent. Each study participant provided a voluntary written informed consent signed by him after explaining to him the potential risks and benefits, as well as the nature of the upcoming study.
Additional information
Translated by E. Babchenko
Rights and permissions
About this article
Cite this article
Kryzhanovskaya, S.Y., Zapara, M.A., Dudnik, E.N. et al. Adaptive Changes in the Indicators of Systemic Hemodynamics and Energy Consumption by Young Men during Passive Hyperthermia Procedures. Hum Physiol 48, 161–169 (2022). https://doi.org/10.1134/S0362119722020104
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1134/S0362119722020104