Abstract
Diabetes mellitus (DM) increases the risk of sudden cardiac death, which suggests the involvement of arrhythmogenic mechanisms. Among other changes, DM causes cardiac autonomic neuropathy (CAN), but its role in electrophysiological myocardial remodeling is unclear. The objective of the present study was to test the effects of β-adrenergic blockade regarding ventricular spatiotemporal electrophysiological properties in an experimental DM model. Epicardial mapping (64-lead sock electrode array) was done in 13 control and 11 alloxan-induced DM rabbits. Activation times (AT), end of repolarization times (RT), and activation-repolarization intervals (ARI) were determined as dV/dt min during QRS, dV/dt max during T-wave, and RT-AT difference, respectively. The β-adrenergic blockade was produced by esmolol infusion (0.5 mg/kg, i.v.). It was found that the early-stage DM in rabbits was characterized by relatively mild changes in ventricular myocardium, which did not involve ventricular activation and the average duration of repolarization. The signature of this stage was the local prolongation of repolarization, which pertained to the RV apical region. The blockade of β-adrenergic receptors in healthy animals produced a ventricular spatiotemporal repolarization pattern similar to that observed in diabetic rabbits with the local apical prolongation of repolarization. On the other hand, the blockade of β-adrenergic receptors in diabetics prolonged the relatively short basal repolarization. It can be concluded that β-adrenergic blockade in healthy animals reproduced the early-stage DM effects on the spatiotemporal electrophysiological properties of the ventricular myocardium. This demonstrated the role which CAN could play in the electrical remodeling of ventricular myocardium in early-stage DM.
Similar content being viewed by others
INTRODUCTION
The prevalence of diabetes mellitus (DM) is approaching 10% of the Earth’s population [1]. Even in the presence of its modern age notorious rival COVID-19, the DM pandemic presents a major medical problem. Among other complications, DM increases the risks of sudden cardiac death [2] that suggests involvement of arrhythmogenic mechanisms [3]. However, the latter remain largely unclear. Moreover, some experimental studies reported that susceptibility to arrhythmias in the diabetic hearts can even be decreased [4–9].
Such a controversy warrants further studies of cardiotropic effects of DM. At the organ level, the electrophysiological effects of DM include activation delay, prolongation of QT interval and redistribution of repolarization gradients, which manifests as T-wave flattening in the body surface ECG [10]. At the cellular level, the targets of DM effects are ion channels for INa [11], Ito [12], IKr [13], IKs [14] currents. DM can either affect cardiomyocytes directly via modification of insulin-dependent signaling pathways and abnormal metabolism or change myocardial properties via abnormal sympathetic regulation, a so-called diabetic cardiac autonomic neuropathy [15–17]. Involvement of sympathetic regulation might have different effects on cardiac electrophysiology, including arrhythmogenic consequences. Major electrophysiological effects of the sympathetic system in the ventricular myocardium are the augmentation of ICa-L [18, 19] and IKs [20], and the enhancement of conduction via gap junctions [21]. The overall effect of sympathetic stimulation is repolarization shortening and increase of conduction velocity [22]. Therefore, it can be expected that attenuation of sympathetic effects might result in the opposite changes. Since sympathetic activation in ischemic conditions has proarrhythmic effects [23], suppression of autonomic effects in DM might partly counterbalance the otherwise adverse electrophysiological effects of DM especially at the early stages of its progression.
We hypothesized that at least part of the electrophysiological effects of DM are due to the suppression of sympathetic influences on the heart. If this is true, then the β-adrenergic blockade might reproduce these effects of DM. On the other hand, the effects of β-adrenergic blockade might be modified in the animals with DM since diabetic conditions might mask the effects of adrenergic blockade. To test this hypothesis in the present study, we evaluated the effect of the β-adrenergic blocker esmolol on a spatiotemporal pattern of ventricular electrophysiological properties, namely propagation via conduction system and contractile myocardium, average duration of ventricular repolarization, dispersion of repolarization and ventricular repolarization gradients in healthy and diabetic rabbits.
METHODS
The investigation conforms with the Guide for the Care and Use of Laboratory Animals, 8th Edition published by the National Academies Press (US) 2011. Experiments were conducted on Chinchilla rabbits (either sex, age 6 months). 13 animals served as controls (6 males, 7 females) and DM was induced in 11 animals (4 males, 7 females) by a single dose of alloxan (120 mg/kg body weight, i.v.). The DM diagnosis was confirmed with the fasting plasma glucose concentration being higher than 7 mmol/L measured once a week with a One Touch glucometer (LifeScan Inc, USA). Electrophysiological studies were done 4–5 weeks after DM induction.
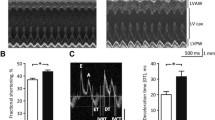
The open-chest experiments were carried out on anaesthetized rabbits (zoletil, 15 mg/kg, i.m.). The measurements were done prior to and after the injection of the β1-blocker esmolol (0.5 mg/kg, i.v.). Unipolar electrograms were recorded in reference to Wilson’s central terminal from 64 ventricular epicardial leads at spontaneous sinus rhythm. Electrophysiological data were recorded by means of a custom-designed mapping system (16 bits; bandwidth 0.05 to 1000 Hz; sampling rate 4000 Hz). In each epicardial lead, activation time (AT), end of repolarization time (RT), and activation–repolarization interval (ARI) were determined as dV/dt min during QRS complex, dV/dt max during T-wave, and the difference between the latter and the former, respectively [24]. The values were determined automatically, inspected by the observer, and corrected manually if necessary. Corrected ARI (ARIc) were calculated by Bazett’s equation [25] to exclude the influence of heart rate: ARI (corrected) = ARI (measured) / RR1/2. The time measurements were done with respect to the QRS onset in the I limb lead. ARIs were assessed in the left ventricular (LV) base and apex, and in the LV and right ventricle (RV) in order to evaluate apicobasal and interventricular repolarization gradients, respectively. Duration of activation propagation via the ventricular conduction system, total ventricular activation and activation of contractile myocardium were measured as the minimal AT throughout all epicardial leads (time of epicardial activation breakthrough), maximal AT throughout all epicardial leads and the difference between maximal and minimal ATs, respectively.
After the electrophysiological measurements, the animals were euthanized during deep anesthesia and the hearts were excised. The light microscopy of Van Gieson and hematoxylin-eosin-stained sections of the left ventricle was conducted to find out the DM-induced inflammatory changes in myocardium. The histopathological changes were interpreted by the investigator who was blinded to the evaluated groups.
Statistical analysis was performed with IBM SPSS Statistics 23.0. The data are presented here as median and interquartile range (IQR). Wilcoxon and Mann–Whitney tests were used for paired comparisons and for the comparisons between the diabetic and control groups, respectively. The differences were considered significant at p ≤ 0.05.
RESULTS
As expected, the median blood glucose level was significantly higher in the diabetic rabbits as compared to the controls (27.3 (IQR 18.1–27.6) mM vs. 5.7 (IQR 5.1–6.0) mM, p < 0.001, respectively). The median body weight of animals from the diabetic group did not change during the course of the disease (2.9 (IQR 2.7–3.1) kg vs. 3.0 (2.7–3.3) kg, p > 0.05, at the time of DM induction and immediately before the electrophysiological experiment, respectively). The lack of weight gain in 6-month-old rabbits for 1 month of observation may be one of the signs of DM. The histological examination demonstrated lypomatosis, disarrangement of the cardiomyocytes, the increase of collagen content and microvascular damage in diabetic hearts (Fig. 1) providing evidence in support of the presence of inflammatory changes in the myocardium at 1 month follow-up.
The median heart rate was lower in the DM group as compared to control (259 (IQR 212–270) beats per minute vs 277 (IQR 238–291), p = 0.018, respectively). The parameters of ventricular activation (duration of activation propagation via ventricular conduction system, duration of contractile myocardium activation, and duration of total ventricular activation) did not differ between the groups and did not change with esmolol administration. The average ARIc duration was similar in the control and DM groups both in the baseline state and after esmolol infusion (Table 1). In the normal rabbits, the apicobasal and interventricular ARI distribution was rather uniform, whereas in the diabetics ARIs were longer in the apex than in the base, and in the RV than the LV (Fig. 2a). The measured and rate-corrected ARIs demonstrated the similar gradients.
β1-blockade resulted in the heart rate slowing both in the control and DM groups (from 277 (IQR 238–291) to 258 (IQR 222–269) and from 259 (IQR 212–270) to 226 (IQR 202–243) beats per min, respectively, p < 0.050) and changed the spatial repolarization distributions in both groups. In the control group, esmolol treatment led to the development of the area of prolonged repolarization on the heart apex and adjacent anterior surface and the significant apicobasal difference in ARI durations (Table 2). In the diabetic hearts, esmolol treatment did not significantly affect apical regions but preferentially prolonged the initially shorter repolarization in the LV base (Fig. 2b). As a result, esmolol application abrogated the apicobasal repolarization gradient in the diabetic ventricles. There was no difference in the duration of repolarization between the control group with the application of esmolol and the DM group at baseline, both at the apex (p = 0.98) and at the base of the left ventricle (p = 0.97).
Pathological changes in the left ventricular myocardium of the diabetic rabbits. (a) Hematoxylin-eosin stain, original magnification 200 times, scale bar 20 µm, wide arrows point at disarray of cardiomyocytes, narrow arrows show lipid accumulation. (b) van Gieson stain, original magnification 200 times, scale bar 50 µm, demonstrates connective tissue development in ventricular myocardium.
DISCUSSION
In this study, we demonstrated that the early stage of DM in rabbits was characterized by relatively mild changes, which did not involve ventricular activation and the average duration of repolarization. The activation times in the diabetic rabbits were similar to those in controls in contrast to data obtained from measurements in diabetic mice [26] and rats [27, 28]; however, the distribution of repolarization durations in diabetic animals differed from that in the control group. In diabetic animals, we did not observe the prolongation of the absolute durations of repolarization which have been found in a number of investigations [14, 29] and which is probably a characteristic of a longer DM duration [30]. However, the rabbits from the DM group had a distinct “inverted” apicobasal repolarization gradient with ARIs increasing as one moved from the base to the apex. This observation could be explained by the short-term follow-up which was not sufficient enough to influence the average duration of repolarization, but rather affected repolarization duration only in the apical region.
The demonstrated pathological myocardial alterations, i.e. the lypomatosis, disarrangement of the myocytes, connective tissue enlargement and microvascular damage were consistent with the previous data [31] showing that fibrosis could serve as a relatively early marker of the DM-induced inflammation. However, the observed differences in the repolarization pattern between normal and diabetic rabbits could hardly be exclusively ascribed to the myocardial inflammatory changes evidenced by fibrosis since the blockade of β-adrenoreceptors in diabetic animals with esmolol abolished the DM-induced repolarization gradients.
The findings of the present study can be interpreted as follows. At the follow-up of 1 month, DM conditions affected repolarization duration predominantly in the apex. The same apical region is affected by the inhibition of sympathetic influences. It was shown in our previous investigation [32] with β-adrenergic blockade with propranolol and in the present investigation with esmolol in the control animals. Similar to DM, β-adrenergic blockade resulted in the prolongation of repolarization. If the DM-induced changes were independent of adrenergic regulation, one might expect the similar effect of β-adrenergic blockade with apical prolongation of repolarization both in the control and diabetic animals. However, adrenergic inhibition in the diabetic rabbits produced different effects, instead of repolarization prolongation in the apex we observed repolarization prolongation in the base. The presumable cause of the effect of esmolol on the diabetic hearts could be the preferential inhibition of sympathetic influence (and prolongation of repolarization) in the areas with the still preserved sympathetic innervation, that produced the rather uniform ARI distribution in the hearts of DM group.
Limitations of the study
In the present study we investigated the contribution of sympathetic dysfunction to the electrical remodeling in DM. On the other hand, different mechanisms of electrophysiological alterations related to DM could also be suggested. Moreover, our data imply that DM-induced disturbance of sympathetic innervation develop in a spatially heterogeneous manner that might be based on a corresponding heterogeneity of sympathetic innervation. In the present study, we could not test this suggestion, and direct data concerning this issue are also lacking in the literature. However, we demonstrated that on the background of various DM-induced myocardial alterations, the sympathetic function/dysfunction appeared essential for the development of repolarization gradients in DM and the elimination of the sympathetic influence abrogated these gradients even in the presence of structural changes of an inflammatory nature. The data presented here concerned the very early stages of the DM development. The prolongation of the follow-up could provide different results on the mechanisms of myocardial electrical remodeling in DM.
CONCLUSIONS
The present study demonstrated that β-adrenergic blockade in healthy animals reproduced the early-stage DM effects on the spatiotemporal electrophysiological properties of ventricular myocardium. This demonstrated a role CAN could play in electrical remodeling of ventricular myocardium in the early-stage DM.
REFERENCES
Saeedi P, Petersohn I, Salpea P, Malanda B, Karuranga S, Unwin N, Colagiuri S, Guariguata L, Motala AA, Ogurtsova K, Shaw JE, Bright D, Williams R (2019) Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: Results from the international diabetes federation diabetes atlas, 9th edition. Diab Res Clin Pract 157: 107843. https://doi.org/10.1016/j.diabres.2019.107843
Aune D, Schlesinge S, Norat T, Riboli E (2018) Diabetes mellitus and the risk of sudden cardiac death: A systematic review and meta-analysis of prospective studies. Nutr Metab Cardiovasc Dis 28: 543–556. https://doi.org/10.1016/j.numecd.2018.02.011
Spooner P (2008) Sudden cardiac death: Influence of diabetes. Diabetes Obes Metab 10: 523–532. https://doi.org/10.1111/j.1463-1326.2007.00723.x
Ravingerova T, Stetka R, Pancza D, Ulicna O, Ziegelhoffer A, Styk J (2000) Susceptibility to ischemia-induced arrhythmias and the effect of preconditioning in the diabetic rat heart. Physiol Res 49: 607–616.
Matejikova J, Kucharska J, Pancza D, Ravingerova T (2008) The effect of antioxidant treatment and nos inhibition on the incidence of ischemia-induced arrhythmias in the diabetic rat heart. Physiol Res 57 (Suppl 2): S55–S60.
Beatch G, McNeill J (1988) Ventricular arrhythmias following coronary artery occlusion in the streptozotocin diabetic rat. Can J Physiol Pharmacol 66: 312–317. https://doi.org/10.1139/y88-053
Kusama Y, Hearse D, Avkiran M (1992) Diabetes and susceptibility to reperfusion-induced ventricular arrhythmias. J Mol Cell Cardiol 24: 411–421. https://doi.org/10.1016/0022-2828(92)93195-p
Zhang L, Parratt J, Beastall G, Pyne N, Furman B (2002) Streptozotocin diabetes protects against arrhythmias in rat isolated hearts: Role of hypothyroidism. Eur J Pharmacol 435: 269–276. https://doi.org/10.1016/s0014-2999(01)01398-x
Belkina LM, Terekhina OL, Smirnova EA, Usacheva MA, Kruglov SV, Saltykova VA (2011) Effect of acute alloxan diabetes on ischemic and reperfusion arrhythmias in rats with different activity of nitric oxide system. Bull Exp Biol Med 150: 299–303. https://doi.org/10.1007/s10517-011-1127-0
Sedova KA, Azarov JE, Arteyeva NV, Ovechkin AO, Vaykshnorayte MA, Vityazev VA, Bernikova OG, Shmakov DN, Kneppo P (2017) Mechanism of electrocardiographic t-wave flattening in diabetes mellitus: Experimental and simulation study. Physiol Res 66: 781–789. https://doi.org/10.33549/physiolres.933494
Stables CL, Musa H, Mitra A, Bhushal S, Deo M, Guerrero-Serna G, Mironov S, Zarzoso M, Vikstrom KL, Cawthorn W, Pandit SV (2014) Reduced na(+) current density underlies impaired propagation in the diabetic rabbit ventricle. J Mol Cell Cardiol 69: 24–31. https://doi.org/10.1016/j.yjmcc.2013.12.031
Gallego M, Alday A, Urrutia J, Casis O (2019) Transient outward potassium channel regulation in healthy and diabetic hearts. Can J Physiol Pharmacol 87: 77–83. https://doi.org/10.1139/y08-106
Zhang Y, Xiao J, Lin H, Luo X, Wang H, Bai Y, Wang J, Zhang H, Yang B, Wang Z (2007) Ionic mechanisms underlying abnormal qt prolongation and the associated arrhythmias in diabetic rabbits: A role of rapid delayed rectifier k+ current. Cell Physiol Biochem 19: 225–238. https://doi.org/10.1159/000100642
Lengyel C, Virág L, Kovács PP, Kristóf A, Pacher P, Kocsis E, Koltay ZM, Nánási PP, Tóth M, Kecskeméti V, Papp JG, Varró A, Jost N (2008) Role of slow delayed rectifier k+-current in qt prolongation in the alloxan-induced diabetic rabbit heart. Acta Physiol 192: 359–368. https://doi.org/10.1111/j.1748-1716.2007.01753.x
Vinik AI, Casellini C, Parson HK, Colberg SR, Nevoret ML (2018) Cardiac autonomic neuropathy in diabetes: A predictor of cardiometabolic events. Front Neurosci 12: 591. https://doi.org/10.3389/fnins.2018.00591
Bissinger A (2017) Cardiac autonomic neuropathy: Why should cardiologists care about that? J Diabetes Res 2017: 5374176. https://doi.org/10.1155/2017/5374176
Stables CL, Glasser RL, Feldman EL (2013) Diabetic cardiac autonomic neuropathy: Insights from animal models. Auton Neurosci 177: 74–80. https://doi.org/10.1016/j.autneu.2013.03.001
Dixon RE (2021) Nanoscale organization, regulation, and dynamic reorganization of cardiac calcium channels. Front Physiol 12: 810408. https://doi.org/10.3389/fphys.2021.810408
Reuter H, Scholz H (1977) The regulation of the calcium conductance of cardiac muscle by adrenaline. J Physiol 264: 49–62. https://doi.org/10.1113/jphysiol.1977.sp011657
Sanguinetti MC, Jurkiewicz NK, Scott A, Siegl PK (1991) Isoproterenol antagonizes prolongation of refractory period by the class iii antiarrhythmic agent e-4031 in guinea pig myocytes. Mechanism of action. Circ Res 68: 77–84. https://doi.org/10.1161/01.res.68.1.77
Campbell AS, Johnstone SR, Baillie GS, Smith G (2014) Β-adrenergic modulation of myocardial conduction velocity: Connexins vs. Sodium current. J Mol Cell Cardiol 77: 147–154. https://doi.org/10.1016/j.yjmcc.2014.09.030
Ajijola OA, Lux RL, Khahera A, Kwon O, Aliotta E, Ennis DB, Fishbein MC, Ardell JL, Shivkumar K (2017) Sympathetic modulation of electrical activation in normal and infarcted myocardium: Implications for arrhythmogenesis. Am J Physiol Heart Circ Physiol 312: H608–H621. https://doi.org/10.1152/ajpheart.00575.2016
Shen MJ, Zipes DP (2014) Role of the autonomic nervous system in modulating cardiac arrhythmias. Circ Res 114: 1004–1021. https://doi.org/10.1161/circresaha.113.302549
Coronel R, de Bakker JMT, Wilms-Schopman FJG, Opthof T, Linnenbank AC, Belterman CN, Janse MJ (2006) Monophasic action potentials and activation recovery intervals as measures of ventricular action potential duration: Experimental evidence to resolve some controversies. Heart Rhythm 3: 1043–1050. https://doi.org/10.1016/j.hrthm.2006.05.027
Bazett H (1920) An analysis of the time-relations of еlectrocardiograms. Heart 7:353–367.
Vaykshnorayte MA, Ovechkin AO, Azarov JE (2012) The effect of diabetes mellitus on the ventricular epicardial activation and repolarization in mice. Physiol Res 61: 363–370.
Axelsen LN, Calloe K, Braunstein TH, Riemann M, Hofgaard JP, Liang B, Jensen CF, Olsen KB, Bartels ED, Baandrup U, Jespersen T, Nielsen LB, Holstein-Rathlou N-H, Nielsen MS (2015) Diet-induced pre-diabetes slows cardiac conductance and promotes arrhythmogenesis. Cardiovasc Diabetol 14: 87. https://doi.org/10.1186/s12933-015-0246-8
Olsen KB, Axelsen LN, Braunstein TH, Sorensen CM, Andersen CB, Ploug T, Holstein-Rathlou NH, Nielsen MS (2013) Myocardial impulse propagation is impaired in right ventricular tissue of zucker diabetic fatty (zdf) rats. Cardiovasc Diabetol 12: 19. https://doi.org/10.1186/1475-2840-12-19
Magyar J, Rusznák Z, Szentesi P, Szûcs G, Kovács L (1992) Action potentials and potassium currents in rat ventricular muscle during experimental diabetes. J Mol Cell Cardiol 24: 841–853. https://doi.org/10.1016/0022-2828(92)91098-P
Pershina E, Azarov J, Vaykshnorayte M, Bernikova O, Ovechkin A (2021) Prolongation of experimental diabetes mellitus increased susceptibility to reperfusion ventricular tachyarrhythmias. Can J Physiol Pharmacol 99: 1097–1101. https://doi.org/10.1139/cjpp-2020-0743
Ares-Carrasco S, Picatoste B, Benito-Martín A, Zubiri I, Sanz AB, Sánchez-Niño MD, Ortiz A, Egido J, Tuñón J, Lorenzo O (2009) Myocardial fibrosis and apoptosis, but not inflammation, are present in long-term experimental diabetes. Am J Physiol Heart Circ Physiol 297: H2109–H2119. https://doi.org/10.1152/ajpheart.00157.2009
Sedova KA, Goshka SL, Vityazev VA, Shmakov DN, Azarov JE (2011) Load-induced changes in ventricular repolarization: Evidence of autonomic modulation. Can J Physiol Pharmacol 89: 935–944. https://doi.org/10.1139/y11-098
Funding
The study was supported by the Program for Fundamental Research of the Russian Academy of Sciences, project number 1021052404529-3-3.1.8.
Author information
Authors and Affiliations
Contributions
Conceptualization, AOO, DNS, JEA; experimental design, AOO, MAV, KAS, IGD, JEA; conducting experiments, AOO, MAV, KAS, KVS, SYM, IGD, JEA; data processing and analysis, AOO, MAV, KAS, KVS, SYM, IGD, JEA, drafting the manuscript, AOO; editing the manuscript, AOO, MAV, KAS, DNS, KVS, SYM, IGD, JEA.
Corresponding author
Ethics declarations
CONFLICT OF INTEREST
The authors declare that they have no conflicts of interest.
Additional information
Translated by A. Polyanovsky
Rights and permissions
About this article
Cite this article
Ovechkin, A.O., Vaykshnorayte, M.A., Sedova, K.A. et al. Beta-Receptor Blockade Reproduces Electrophysiological Effects of Early Diabetes Mellitus in Ventricular Myocardium. J Evol Biochem Phys 58 (Suppl 1), S74–S81 (2022). https://doi.org/10.1134/S0022093022070080
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1134/S0022093022070080