Abstract
Enhancing the pooling level of medical insurance is an inevitable requirement to strengthen the mutual assistance capability of funds and achieving national health. In China, with the continuous expansion of the migrant population seeking medical treatment in other regions, the role of provincial-pooling of basic medical insurance is becoming increasingly prominent. While there is limited research on the impact and mechanism of provincial-pooling of basic medical insurance on the health of migrant population. Therefore, this study aims to explore the impact of provincial-pooling of basic medical insurance on the health performance of migrant population and analyze the mediating role of social integration. Using data of three waves (2014, 2016 and 2018) of the China Labor force Dynamics Survey, this study focuses on a sample of migrant population enrolled in Urban and Rural Resident Basic Medical Insurance and employs the estimation methods of time-varying difference-in-difference and mediating effect model. The results of time-varying difference-in-difference show that provincial-pooling of basic medical insurance improves the health performance of migrant population by 9.6% (p < 0.05), and the event study method and placebo test all indicate that the research results are robust. The mediating effect analysis demonstrates that the provincial-pooling of basic medical insurance enhances health performance by fostering the subjective and objective social integration, and neighbourhood assistance, social equity, life happiness and trust in the majority are specific intermediary channels. The results of heterogeneity analysis indicates that provincial-pooling of basic medical insurance is more effective in improving the health performance of high-income (β = −0.090; P < 0.05), new-generation (β = −0.116; P < 0.1) and highly-educated (β = 0.130; p < 0.05) migrant population. Our results call for accelerating the promotion of provincial-pooling of basic medical insurance to improve health performance of migrant population.
Similar content being viewed by others
Introduction
The most important indicator of Chinese path to modernization is health. Migrant population is undoubtedly an important force for creating miracles of economic growth, but due to the long-term separation between household registered and actual residences, the health issues of this group have emerged as a significant global concern, and China is no exception. The mobility characteristics inherent to the migrant population exposes them to an elevated susceptibility to infectious diseases, reproductive system ailments and mental health disorders (Liu and Wang 2022). In addition, the dual institutional barriers of outflow and inflow areas make this group more susceptible to suffer health losses due to difficulties in accessing fair health services and delayed treatment (Li et al. 2022). Prolonged low-level social integration may also lead to psychological health risks such as anxiety and depression, and even lead to physical diseases such as malignant tumors (Latinsky-Ortiz and Strober 2022; Xia and Shen 2022).
Internationally, countries are dedicated to strengthen the fund’s capability of resilience to risks, promote social equity and improve the overall operational efficiency of the healthcare system by elevating pooling level of medical insurance (Harlock et al. 2019; Gu and Wu 2021). Fund risk pools are usually classified by the level of administrative management, population and geographical coverage, and the higher pooling level means government departments at higher levels disperse health risks for insured individuals on a larger scale (Mathauer et al. 2019). In practice, two kinds of integration, horizontal and vertical, have been formed to enhance the degree of pooling. For instance, Thailand has horizontally integrated the Medical Benefit Scheme and the Voluntary Health Insurance into Universal Coverage Scheme (Hsu et al. 2015). Korea has also integrated over 300 insurance projects into a single national health insurance fund (Kwon 2010). In China, due to the large population base and significant differences of socioeconomic development between urban and rural areas, the basic medical insurance has been divided based on population since its establishment, initially including the Urban Employee Basic Medical Insurance (UEBMI), Urban Resident Basic Medical Insurance (URBMI) and New Cooperative Medical Scheme (NCMS). With the continuous improvement of fairness and treatment level of institution, China integrated the latter two insurances into the Urban and Rural Resident Basic Medical Insurance (URRBMI) in 2016. Meanwhile, the level of basic medical insurance fund management has also been elevated from the county-level to the city level, and has developed towards provincial-level, which vertically enhances the level of medical insurance pooling.
Nevertheless, limited by various factors such as economic development, policy system and digital platform, the current pooling level of basic medical insurance in China is still mainly at the city level. In fact, in order to strengthen the fund’s capability of resilience to risks and meet social mobility needs, some provinces and cities have been actively promoting provincial- pooling of basic medical insurance since 2000. However, due to differences in the management difficulty of UEBMI and URRBMI, some regions firstly implemented the provincial-pooling of UEBMI, such as Shanghai, Beijing and Tianjin, while other regions firstly implemented the provincial-pooling of URRBMI, such as Chongqing, Qinghai, Hainan. Undoubtedly, with the construction of a more fair and sustainable medical security system, more and more provinces will implement the provincial-pooling of basic medical insurance. Will it impact the health performance of migrant population? Does it help them integrate into the destination and achieve a positive interaction between social integration and health performance? This is the important issue that this study aims to explore.
This study refers to the substantive impact of provincial-pooling of basic medical on the health of migrant population as health performance. Although limited scholars have studied the relationship between provincial-pooling of medical insurance and individual health, no consensus has been reached. Some scholars hold a positive attitude, advocating that the provincial-pooling of basic medical insurance can increase residents’ willingness to seek medical treatment and better maintain their health (Li et al. 2020). Wu et al. (2022) found that the provincial-pooling of UEBMI can alleviate health inequality caused by income disparity, reducing the probability of suffering from chronic diseases among low-income groups by about 6.80%. However, some scholars hold different opinions, arguing that although the provincial-pooling of UEBMI significantly increased the utilization of medical services, it didn’t bring health benefits (Shen 2022). Regarding research subjects, previous studies mainly focused on the insured population of UEBMI. Only Zhang and Wu 2022 analyzed the impact of the elevation of the pooling level of medical insurance on the utilization of health service for the elderly migrant population, which indicated that the provincial-pooling can increase their possibility of seeking medical treatment and enjoying instant settlement in the inflow area.
Research on the social integration of migrant population first appeared in the attention to the integration of international immigrants (Park 1928). Social integration refers to the process in which migrant population gradually adapt to inflow area across cultural, psychological and other dimensions through a complex interplay of interaction and collision, and enjoy the same welfare benefits as the citizens of the destination (Liang 2016). Correspondingly, the measurement of social integration is also multidimensional, which mainly divided into subjective social integration and objective social integration. The former mainly refers to social integration related to value concept, psychological satisfaction and identity recognition, while the latter mainly refers to social integration related to economic integration, behavioral adaptation and social welfare benefits (Yang 2010; Liu et al. 2020; Xiao et al. 2021). As an important institutional factor, previous research indicated that the provincial-pooling of medical insurance can increase the possibility of equal access to medical services between migrant population and local residents, and create a strong institutional pull force to promote the integration of migrant population into destination (Li and Dou 2022; Cao et al. 2022). What’s more, economic integration, cultural integration and psychological integration all have a significant positive impact on the health of migrant population (Chen et al. 2017; Hao et al. 2018). Nevertheless, few studies have systematically analyzed the provincial-pooling of basic medical insurance, social integration and the health performance of migrant population within one framework.
In summary, existing studies on the provincial-pooling of basic medical insurance, social integration and the health of migrant population furnishes valuable insights for our study. But they have not reached a consensus on the relationship between provincial-pooling of basic medical insurance and health performance and doesn’t include the key element of social integration into mechanism analysis. Few studies focus on migrant population with characteristics of health vulnerabilities and unequal medical security. Furthermore, existing studies lack rigorous empirical analysis and the effectiveness of identifying the causal effects of policies remains to be discussed. Based on this, this study explores the impact of provincial-pooling of basic medical insurance on the health performance using time-varying difference-in-difference (DID) approach and test the mediating role of social integration. The main contributions of this study are as follows: firstly, this study takes the URRBMI which covers the widest range of migrant population as an example to explore the impact of provincial-pooling of basic medical insurance on the health performance of migrant population, the results are of great significance for accelerating the promotion of provincial-pooling of basic medical insurance. Secondly, this study examines the mediating role of social integration between the provincial-pooling of basic medical insurance and the health performance of migrant population, which provides data support for achieving a positive interaction between new urbanization and the construction of a healthy China. Thirdly, this study uses time-varying DID approach to mitigate potential endogeneity concerns, such as unobserved variables and bidirectional causality, thereby augmenting the credibility of the research results. Fourthly, this study explores the heterogeneous characteristics of the impact of provincial-pooling of basic medical insurance on the health performance in terms of income, age and education, so as to comprehensively examine the policy effects and improve the precision of the implementation of policy.
Policy background and hypotheses
Policy background
Elevating the level of basic medical insurance, also referring to elevating the management level of medical insurance fund, has always been an important means for China to strengthen the fund’s capabilities of resilience to risks and co-payment (Yuan 2022). At the beginning of the establishment of the basic medical insurance system, the State Council issued the “Decision on Establishing the Urban Employee Basic Medical Insurance” and announced that employees should participate in basic medical insurance with their local city or county as the pooling unit. However, in the process of development, the low pooling level of basic medical insurance successively led to the imbalances of regional policy, the dispersion of fund management, the difficulties in seeking health services across different regions and the negligence in fund supervision. Therefore, some regions began to elevate the pooling level of basic medical insurance from county-level to city-level. In 2009, the Ministry of Human Resources and Social Security and the Ministry of Finance issued the “Guiding Opinions on Further Strengthening the Management of Basic Medical Insurance Funds” and announced that China would basically achieve the city-pooling of basic medical insurance by 2011. Subsequently, in 2010, the Social Insurance Law firstly proposed the implementation of provincial-pooling of basic medical insurance at the national level. In 2020, the Communist Party of China Central Committee and the State Council of the People’s Republic of China issued “Opinions on Deepening the Reform of the Medical Security System” and emphasized the importance of the promotion of provincial-pooling of basic medical insurance. In 2022, the report to the 20th National Congress of the Communist Party of China further clarified the requirement of promoting provincial-pooling of basic medical insurance, unemployment insurance and work-related injury insurance. From 2000 to 2023, 8 provinces (municipalities) have implemented provincial-pooling of UEBMI and 7 provinces (municipalities) have implemented provincial-pooling of URRBMI in China, forming the unified revenue and expenditure model and the risk adjustment fund model (as shown in Table 1). The former is to centralize the rights of the formulation of medical insurance policies and the management of medical insurance funds of the cities under the province’s jurisdiction to provincial-level institutions, achieving the unification of financing, security benefits and management service standards within the provincial region. The latter is to collect a certain proportion of the adjustment funds from cities by the provincial-level medical insurance departments every year without changing the original policy formulation, administrative supervision and handling services of the cities under the province’s jurisdiction, which will be used to fill the possible gap in revenue and expenditure of the medical insurance fund.
Compared to the risk adjustment fund model, the unified revenue and expenditure model is a truly unified model for medical insurance fund pooling. The former has relatively less resistance to reform and is often considered a transitional measure for the latter. Nevertheless, due to the incompatibility of the unified revenue and expenditure model with traditional medical insurance management and fiscal responsibility mechanisms, as well as the long-standing and widespread economic imbalances, financing and treatment disparities within provincial regions, it is difficult to reach a consensus on whether to implement the provincial-pooling of basic medical insurance and what model to adopt. But there is no doubt that the implementation of the provincial-pooling of basic medical insurance, especially the adoption of the unified revenue and expenditure model, is more conducive to enhancing the capabilities of risk resistance of funds and promoting social equity.
Hypotheses
Due to the long-standing dual institutional barriers between outflow and inflow areas, a large number of migrants face problems such as large medical insurance treatment disparities and difficulties in transferring social insurance relationships during the process of seeking health service. This may not only inhibit their health needs, but also delay disease treatment (Liu 2020). Therefore, higher requirements have been put forward for the accessibility of health service and the improvement of medical insurance benefits in inflow areas. Based on the law of large numbers theory, on one hand, the provincial-pooling of basic medical insurance can enhance the fund’s capability of resilience to risks by expanding insurance coverage. On the other hand, it can also reduce regional differences and improve institutional equity by unifying management systems, financing mechanisms and security benefits within the province (Jia et al. 2023), so as to improve the utilization of medical services and health performance of migrant population. Moreover, the publicity of the provincial-pooling of basic medical insurance may also help migrant population acquire health knowledge and improve health literacy, so as to reduce and prevent the occurrence of diseases. Based on this analysis, we propose hypothesis 1:
Hypothesis 1: Provincial-pooling of basic medical insurance has a significant positive impact on the health performance of migrant population.
Based on the equal opportunity theory by John Romer, it is unequal for migrant population to be unable to enjoy the same medical security benefits as residents of the destination due to factors of identity and environment (Ma et al. 2018; Zhou et al. 2016). The provincial-pooling of basic medical insurance is a relatively equal policy design for migrant population and local residents in the inflow area. Subjectively, it is beneficial to enhance the sense of identity recognition and belonging of the migrant population (Zhu et al. 2022). Objectively, it is helpful for migrant population to obtain equal medical services and higher levels of medical insurance benefits (Cao et al. 2022), thus promoting the free mobility of labor across regions and social integration into the inflow area. Furthermore, existing research indicated that the social integration has a positive impact on the mental health of migrant population, and the stronger their cultural adaptability and willingness to integrate, the higher their health performance (Miao and Xiao 2020; Lin et al. 2017). On the contrary, the opposition and separation of social psychology may exacerbate the phenomenon of migrant population being deprived of various public service resources, which has a negative impact on their health (Cheng et al. 2021). In other words, the lower the level of social integration, the higher the degree of inequality between migrant population and the local residents in accessing social security and health services, and the more limited the social support they may receive in the face of health shocks (Zhang et al. 2020). Based on this analysis, we propose hypothesis 2:
Hypothesis 2: Provincial-pooling of basic medical insurance improves the health performance of migrant population by fostering their social integration.
Consequently, we systematically examine the relationship among provincial-pooling of basic medical insurance, social integration and the health performance of migrant population within one analytical framework. Provincial-pooling of basic medical insurance may not only directly improve the health performance of migrant population by strengthening the fund’s capability of resilience to risks and narrowing the disparities of regional medical insurance benefits, but also indirectly improve the health performance by enhancing the subjective social integration characterized by value identification and objective social integration characterized by social equity. In addition, considering that personal, environmental and social factors may also have impacts on the social integration and health performance of migrant population, we incorporate control variables at the individual, family and regional levels. The theoretical analysis framework constructed in this study is shown in Fig. 1.
Data and methods
Data source
This study used data of three waves (2014, 2016 and 2018) of the China Labor Force Dynamic Survey (CLDS). This survey covers diverse information of the labor force population aged 15–64, including basic demographics, education background, migration experience, social support and health status, which meets the research needs of our study. The sample covers 29 provinces/cities/autonomous regions in China (except Hong Kong, Macao, Taiwan, Xizang and Hainan) and is nationally representative. To obtain an appropriate sample, several data handling steps were taken. Firstly, according to the definition of migrant population by the National Bureau of Statistics, this study selected samples with registered residence outside the county where they live and with experience of moving across counties for more than half a year as research objects. Secondly, considering only individuals who participate in basic medical insurance are likely to be covered by the provincial-pooling of basic medical insurance, we retained the basic medical insurance participant samples for urban and rural residents, so as to exclude the research bias caused by uninsured samples. Finally, after deleting the samples with missing key variable information, 7719 participants were included in the analysis.
Variables
The dependent variable in this study is the health performance of migrant population. Self-rated health is a comprehensive indicator reflecting the health status of individuals and is widely used by scholars to measure the health performance of migrant population (Wei et al. 2021; Henriksson et al. 2020). This study also selected self-rated health as a proxy variable for health performance. Based on the respondents’ answers to the question of “What do you think of your current health status?” over a period of time with clear memory, we assigned a value of 1 to responses of “very healthy” and “healthy” and a value of 0 to responses of “average”, “relatively unhealthy” and “very unhealthy”.
The independent variable in this study is the provincial-pooling of URRBMI, measured by whether the household registration region of migrant population implements the provincial-pooling of URRBMI. Based on the policy documents published on the official websites of provincial governments, health insurance bureaus, or human resources and social security bureaus, this study obtained the year in which provincial-pooling of URRBMI was implemented in each province. If the year of policy release before or equal to the survey year, it will be classified into the treatment group, with a value of 1. Otherwise, it will be classified into the control group, with a value of 0.
The mediating variable in this study is the social integration of migrant population. Based on previous literature and data availability, we measured the social integration from both objective and subjective perspectives. Objective social integration refers to the behaviour adaptation of migrant population and the degree to which they enjoy the same social welfare as locals. It is measured by the respondents’ answers to the questions of “Do you have mutual assistance with your neighbours?” and “Do you think your current living standard is fair compared to your efforts at work?”. Subjective social integration refers to the subjective evaluation of migrant population in the process of interacting with the city, often manifested as a sense of belonging, identification and happiness at the psychological level (Xia and Shen 2022; Liang 2020). It is measured by the respondents’ answers to the questions of “Do you think you are living a happy life?” and “Do you agree that most people can be trusted?”. All the above answers are the respondents’ perceptions of social integration during a period of time with clear memory before the interview. This study used principal component analysis to measure the variance contribution rates of four basic indicators, and then weighted them separately to obtain the indicators of subjective and objective social integration.
Referring to the previous literature (Yuan and Deng 2021; Zheng et al. 2022), this study selects control variables at the individual, family and regional levels. Personal characteristics include age, gender, marriage, education, social status, income, whether to smoke, drink and exercise. Family characteristics mainly refers to the number of siblings. Regional characteristics include the per capita Gross Domestic Product (GDP) of each province and the region they belong to, which are matched according to the province ID and economic region classification standards published by the National Bureau of Statistics.
Study model
Time-varying DID model
The elevation in the pooling level of basic medical insurance is an incremental process marked by variation in the year for implementing provincial-pooling of URRBMI across provinces. Referring to the previous literature (Hoynes et al. 2016; Guo and Xiong 2018), this study used a time-varying DID model to estimate the effect of provincial-pooling of URRBMI on the health performance of migrant population. The model is set as Eq. (1):
The subscripts i, k and t correspond to individual, province and time, respectively. \({H}_{{ikt}}\) represents the health performance of individual i in province k during period t. \({{Policy}}_{{ikt}}\) represents the implementation of the policy of provincial-pooling of URRBMI. If province k where individual i is located implements the provincial-pooling of URRBMI in period t, a value of 1 will be assigned, otherwise, a value of 0 will be assigned. \({X}_{{ikt}}^{m}\) is a control variable group that includes variables at the individual, family and regional levels. \({{\rm{\beta }}}_{1}\) is the coefficient of the independent variable, \({{\rm{\beta }}}_{1}\)> 0 indicates that the provincial-pooling of URRBMI will improve the health performance of migrant population. \({\beta }_{m}\) is the coefficient of the control variables. \({{\rm{\lambda }}}_{k}\) and \({{\rm{\gamma }}}_{t}\) refer to region and time fixed effect, respectively. \({{\rm{\beta }}}_{0}\) is a constant term. \({{\rm{\mu }}}_{{ikt}}\) is a random error term.
Mediating effect model
Social integration plays a vital role in improving the health conditions. In order to further examine the mediating role of social integration in the process of provincial-pooling of URRBMI affecting the health performance of migrant population, this study constructed a mediating effect model. The model is set as Eqs. (2)–(4):
\({M}_{{ikt}}\) represents the level of social integration of individual i in province k during period t, including objective and subjective social integration. The setting of independent variable, dependent variable and control variables is consistent with the time-varying DID model.
Results
Descriptive analysis
The results of descriptive analysis are shown in Table 2. It can be found that 3.7% of the migrant population are covered by the policy of provincial-pooling of URRBMI in the survey year, which is consistent with the fact that China’s provincial-pooling of URRBMI is still in the pilot stage. Compared with the control group (M = 0.598, SD = 0.490) that was not covered by the policy of provincial-pooling of URRBMI, the self-rated health of the treatment group (M = 0.671, SD = 0.471) significantly improves by 7.3%. The level of life happiness in the treatment group (M = 3.753, SD = 0.954) is 9.9% higher than that in the control group (M = 3.653, SD = 0.925). The level of trust in the majority in the treatment group (M = 2.841, SD = 0.532) is 7.6% higher than that in the control group (M = 2.765, SD = 0.560). The probability of marriage for the treatment group (M = 0.760, SD = 0.428) is 8.0% lower than that of the control group (M = 0.839, SD = 0.367). The probability of having an agricultural household registration in the treatment group (M = 0.781, SD = 0.414) is 15% lower than that of the control group (M = 0.931, SD = 0.253). The highest educational level of the treatment group (M = 2.322, SD = 1.191) is 35.1% higher than that of the control group (M = 1.970, SD = 0.936). The annual income of the treatment group (M = 10.026, SD = 2.125) is 52.4% higher than that of the control group (M = 9.502, SD = 2.434). The probability of smoking in the treatment group (M = 0.417, SD = 0.494) is 6.6% higher than that of the control group (M = 0.351, SD = 0.477). The probability of physical exercise in the treatment group (M = 0.329, SD = 0.471) is 10.4% higher than that of the control group (M = 0.225, SD = 0.418). The number of siblings in the treatment group (M = 2.459, SD = 1.759) is 49.3% less than that in the control group (M = 2.953, SD = 1.835). The per capita GDP of the treatment group (M = 11.201, SD = 0.372) significantly increases by 33.8% compared to the control group (M = 10.863, SD = 0.372). The probability of living in economically underdeveloped areas in the treatment group (M = 2.286, SD = 0.960) is 38% higher than that in the control group (M = 1.906, SD = 0.916). In addition, there are no significant differences between the treatment group and the control group in terms of neighbourhood assistance, social equity, age, gender, social status and whether to drink.
Time-varying DID analysis
Considering that the self-rated health is a binary dummy variable, the Logit model was employed to estimate the average marginal effect of provincial-pooling of URRBMI on the health performance of migrant population. The results of time-varying DID analysis are shown in Table 3. Without adding any control variables and only controlling for the fixed effects of region and time, the provincial-pooling of URRBMI significantly increases the health performance of migrant population by 9.8% (P < 0.01). After adding the control variables, the provincial-pooling of URRBMI still increases the health performance of migrant population by 9.6% (P < 0.05), thus verifying hypothesis 1.
This study also evaluated the impact of individual, family and regional characteristics on the health performance of migrant population. The health performance of migrant population decreases by 0.9% (P < 0.01) with every one-year increase in age. Men’s health performance is 5.1% (P < 0.01) higher than that of women’s. Higher level of education, income and social status increase the health performance of migrant population by 2.9%, 0.8%, and 3.7% (P < 0.01). This may be related to their ability to access more medical resources. Participation in physical exercise can also increase the health performance of migrant population by 4.0% (P < 0.01).
Mechanism analysis
This study used stepwise regression to test the mediating effect. Firstly, the results of time-varying DID have indicated that provincial-pooling of URRBMI significantly enhances the health performance of migrant population. Secondly, this study examines the impact of provincial-pooling of URRBMI on the social integration of migrant population. As shown in Table 4, the provincial-pooling of URRBMI increases the level of objective social integration by 16.5%, which is significant at a statistical level of 5%. The provincial-pooling of URRBMI also increases the level of subjective social integration by 20.6%, which is significant at a statistical level of 1%. Finally, this study examines the impact of provincial-pooling of URRBMI and social integration on the health performance of migrant population. As shown in Table 5, after adding objective social integration into the benchmark regression, the positive effect of provincial-pooling of URRBMI on health performance decreases to 8.5%, and objective social integration significantly enhances the health performance by 6.8%. After adding subjective social integration into the benchmark regression, the positive effect of provincial-pooling of URRBMI on health performance decreases to 8.3%, and subjective social integration significantly improves the health performance by 6.6%. The above results indicate that both objective and subjective social integration play a partial mediating role, thus verifying hypothesis 2.
Heterogeneity analysis
Heterogeneity analysis plays an important role in comprehensively examining the impact of provincial-pooling of URRBMI on the health performance of migrant population. Firstly, the heterogeneity of different income groups is analysed. Referring to the classification criteria of the National Bureau of Statistics for the low-income group and considering the actual income distribution of respondents in the CLDS, this study defines the low-income group with a monthly average income of less than or equal to 700 yuan, and the high-income group with a monthly average income of more than 700 yuan. The results of heterogeneity analysis in Table 6 show that the provincial-pooling of URRBMI improves the health performance of high-income group by 9%, while the impact on the health performance of low-income group is not significant. High-income migrant population is the main beneficiary of the provincial-pooling of URRBMI.
Secondly, this study analyses the heterogeneity of different age groups. Referring to the general classification standards of previous literature, this study divides migrant population into the old-generation and new-generation based on their birth years, with the year 1980 as the boundary. The results of heterogeneity analysis in Table 6 show that the provincial-pooling of URRBMI significantly enhances the health performance of the old-generation group and the new-generation group by 9% and 11.6%, respectively. In comparison, the positive effect on the new-generation migrant population is much higher.
Thirdly, the heterogeneity of different education groups is analysed. The study further divides migrant population into low-education group and high-education group, with middle school education as the boundary. The results of heterogeneity analysis in Table 6 show that the provincial-pooling of URRBMI significantly improves the health performance of the high-education group by 13%, while the impact on the low-education group is not significant. High-education migrant population is more likely to benefit from the provincial-pooling of URRBMI.
Robustness test
Event study
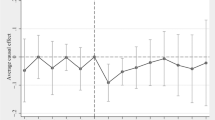
To verify the robustness of the results, three strategies are adopted. The first is the event study method. Given the variation in the year of implementing provincial-pooling of URRBMI across provinces, we employed event study method to test parallel trend (Pilvar and Yousefi 2021), which means that the treatment group and the control group exhibit similar time trends in the absence of policy shocks. Meanwhile, this method can also examine the dynamic effects of the provincial-pooling of URRBMI. The model of event study is set as Eq. (5):
To order to exclude the influence of unobservable factors, this study constrained the event window to two periods before the implementation of the policy and four periods after the implementation of the policy, and used the first period before the implementation of the policy as the benchmark group for prior trend test. When m = −2, for the individual i in province k which implemented provincial-pooling of URRBMI in year t + 2, the dummy variable \({{policy}}_{{ikt}}=1\), otherwise \({{policy}}_{{ikt}}=0\). When m = 0, for the individual i in province k which implemented provincial-pooling of URRBMI in year t, the dummy variable \({{policy}}_{{ikt}}=1\), otherwise \({{policy}}_{{ikt}}=0\), and so on. \({\alpha }_{m}\) is the core coefficient that the event study method focuses on, if the value of \({\alpha }_{-2}\) is significantly 0, the prior parallel trend passes.
The dynamic effects of the provincial-pooling of URRBMI on the health performance of migrant population are shown in Fig. 2. During the two periods preceding the implementation of the policy, the coefficient of \({{policy}}_{{ikt}}\) is not significant, thus passing the parallel trend test. In the first period after the implementation of the policy, the provincial-pooling of URRBMI significantly enhances the health performance of migrant population by 24.5%, which is consistent with the results of logit regression. However, the coefficient is not significant and the impact direction shifts from positive to negative since the second period after the implementation of the policy. This indicates that the provincial-pooling of URRBMI only plays a short-term role in enhancing the health performance of migrant population, and fails to fundamentally solve the difficulties of migrant population in accessing health services.
Placebo test
The second is the placebo test. To exclude the influence of other random confounding factors on the health performance of the migrant population, we conducted a placebo test by randomly generating time for the implementation of provincial-pooling of URRBMI in different regions. This study randomly divided provinces into treatment and control groups based on the actual number of provinces implementing provincial-pooling of URRBMI. Then, this study randomly generated the time for the implementation of the policy for each treatment group. The dummy variable signifying the implementation of the policy was regenerated to replace the original one, adhering to the definition of whether to implement provincial-pooling of URRBMI in the time-varying DID model. Finally, this study repeated the above process 500 times and compared the obtained 500 sets of regression results with the results of time-varying DID. If most of the p-values in these 500 sets of regression results are not significant, the improvement in the health performance is indeed caused by the provincial-pooling of URRBMI.
The results of placebo test are shown in Fig. 3. The vertical dotted line represents the p-value corresponding to the time-varying DID, the value of which is 0.011. It can be seen that after randomization, the p-values of most estimates are greater than the true value of 0.011 and aren’t significant at the 5% level of significance. Consequently, the interference of other random factors can be excluded, indicating that the results of time-varying DID are robust.
Expand sample size
The third robustness test is to expand sample size. To reduce the interference of outliers, this study further included the data of the 2012 wave of CLDS on top of the original samples. Since the questionnaire in the 2012 wave of CLDS did not investigate the marriage, whether to exercise and the number of siblings, the three variables were excluded from the set of control variables here, and the set of other variables were consistent with the benchmark regression.
The results of robustness test after expanding the sample size are shown in Table 7. After adding control variables, the provincial-pooling of URRBMI significantly enhances the health performance of migrant population by 8.4%, which is close to the results of benchmark regression, thus verifying the reliability of the results.
Discussion
This study finds that the provincial-pooling of URRBMI significantly enhances the health performance of migrant population. The elevation in the pooling level of medical insurance enables migrant population to enjoy more medical security benefits and reduces their behavior of self-treatment, thus promoting the health performance of migrant population. This is consistent with existing research (Wu et al. 2022; Li et al. 2022). The added value of this study lies in providing empirical evidence for the impact of the provincial-pooling of URRBMI on the health performance of migrant population which is a broad and special group. In addition, this study also finds that the provincial-pooling of URRBMI only has a significant positive impact on the health performance of migrant population in the first year after the implementation of the policy. Based on the the equal opportunity theory, in the early stages of the implementation of the policy, the provincial-pooling of URRBMI signifies an improvement in the medical security benefits, which can motivate migrant population to seek health services in a timely manner (Ma et al. 2018). Nevertheless, owing to the lower payment capacity of migrant population compared to local residents with stable employment and economic sources, it is less likely for them to continue enhancing the utilization of medical service over time, which affects the continuous enhancement of health performance. This suggests that except promoting the provincial-pooling of basic medical insurance, we should also focus on enhancing the capacity of endogenous development of the migrant population, such as providing them with education, work and medical care. Such endeavors can enhance their ability to translate the opportunity equity presented by provincial-pooling of basic medical insurance into substantive equity of health.
Meanwhile, the provincial-pooling of URRBMI enhances the health performance of migrant population by fostering the subjective and objective social integration. Neighbourhood assistance, social equity, life happiness and trust in the majority are important intermediary channels. Previous literatures have found that social integration is an important factor in promoting the health of migrants (Lu et al. 2022; Zhou et al. 2022), but they didn’t explore the relationship between provincial-pooling of basic medical insurance, social integration and the health of migrants within one analytical framework. This study addresses this gap. On one hand, the provincial-pooling of URRBMI improves the convenience of migrant population seeking medical services out of hometown and ensures their fairness in accessing medical security, thus improving their health performance by fostering the objective social integration. On the other hand, the provincial-pooling of URRBMI enhances the sense of belonging and identification among the migrant population towards the city and encourages them to learn health-related knowledge, thus improving their health performance by fostering the subjective social integration.
In addition, this study finds that the beneficiaries of the provincial-pooling of URRBMI are mainly high-income, new-generation and high-education migrant population. The possible reasons are that high-income group exhibits a stronger capacity of economic payment and are more inclined to enhance their utilization of medical services following the provincial-pooling of URRBMI. The convenience of accessing medical resources makes new-generation group more likely to benefit from the provincial-pooling of URRBMI. High-education group usually has higher health literacy, which can help them absorb health information and using health services efficiently. These findings provide reference for the precise implementation of the provincial-pooling of medical insurance.
Although this study has deepened the understanding of the relationship between the provincial-pooling of URRBMI and the health performance of migrant population, there are still two limitations. Firstly, this study used data of three waves (2014, 2016 and 2018) of the CLDS, limited by the disclosure time of public database, this study did not observe the long-term effects of the provincial-pooling of basic medical insurance after 2018. In this regard, we will conduct further in-depth research after the release of tracking data in the future. Secondly, health is a multidimensional concept that encompasses physical health, mental health and social adaptation. This study selected self-rated health to measure the health performance of migrant population, with a certain degree of subjectivity. In future research, more health indicators can be considered for a more comprehensive evaluation.
Conclusion and policy recommendation
In summary, this study concludes that the provincial-pooling of URRBMI can improve the health performance of migrant population, and the result passes robustness tests of event study method, placebo test and expanding sample size. Mechanism analysis shows that the provincial-pooling of URRBMI can enhance health performance of migrant people by fostering the subjective and objective social integration. Heterogeneity analysis shows that the beneficiaries of provincial-pooling of URRBMI are high-income, new-generation and high-education migrant population.
Based on these findings, the following recommendations are made to policymakers. Firstly, it is imperative to accelerate the promotion of the provincial-pooling of URRBMI, so as to enhance the fund’s capability of resilience to risks on a larger scale and narrow the gap in medical service accessibility between the migrant population and local residents. Secondly, it is necessary to leverage the intermediary function of social integration between the provincial-pooling of basic medical insurance and the enhancement of health performance, such as holding various cultural and recreational activities in the community, strengthening the interaction between migrant population and local residents. Thirdly, it is suggested that the medical security benefits should be appropriately tilted towards vulnerable groups, for instance, granting lower deductible line, higher reimbursement ratio and higher cap line to low-income group. Community doctors and volunteers should also hold health lectures to help low-education group improve their health literacy.
Data availability
We used a secondary data from the China Labor Force Dynamic Survey (CLDS), which was conducted in 2014, 2016 and 2018. The data that support the findings of this study are not publicly available due to the ownership of the data belonging to the Social Science Survey Center of Sun Yat-sen University. We have applied for the data by sending email to [cssdata@mail.sysu.edu.cn], and the data can be accessed in Sun Yat-sen University at [http://css.sysu.edu.cn] within the university IP coverage. The data analysed during the current study are provided in the supplementary file and can be obtained from the corresponding author on reasonable request.
References
Cao ZJ, Chen ZF, Chen SJ (2022) Research on the impact of access to public health services on social integration among migrant elderly—Based on the data of national dynamic survey of health and family planning of migrant population in 2017. Health Econ Res 39(2):35–39
Cheng HB, Tian M, Li ZG (2021) The impact of multidimensional integration on migrants’ health in transitional urban China. Modern Urban Res 36(12):96–102
Chen W, Ling L, Renzaho A (2017) Building a new life in Australia: An analysis of the first wave of the longitudinal study of humanitarian migrants in Australia to assess the association between social integration and self-rated health. BMJ Open 7(3):e014313
Gu H, Wu D (2021) Connotation and strategic conceptualization of the high-quality development of the essential healthcare security system during the 14th Five-Year plan period. J Manag World 37(9):158–167
Guo F, Xiong RX (2018) Local financial institutions and regional economic growth: A quasi-natural experiment of city commercial banks in China. China Econ Q 17(1):221–246
Hao XN, Sun JY, Bo T (2018) Study of the effect of the social integration on health among floating people—Based on the test of the dynamic monitoring data of the national floating population in 2014. Popul Dev 24(4):14–23
Harlock J, Caiels J, Marczak J, Peters M, Fitzpatrick R, Wistow G et al. (2019) Challenges in integrating health and social care: The better care fund in England. J Health Serv Res Policy 25(2):86–93
Henriksson P, Sderstrm E, Blomberg M, Nowicka P, Petersson K, Thomas K, Bendtsen M, Esteyez-Lopez F, Lof M (2020) Self-rated health in migrant and non-migrant women before, during and after pregnancy: A population-based study of 0.5 million pregnancies from the Swedish pregnancy register. J Clin Med 9(6):1764
Hoynes HW, Schanzenbach DW, Almond D (2016) Long run impacts of childhood access to the safety net. Am Econ Rev 106(4):903–934
Hsu MC, Huang XG, Yupho S (2015) The development of universal health insurance coverage in Thailand: Challenges of population aging and informal economy. Soc Sci Med 2015(145):227–236
Jia XY, Zhang XW, Zhou M (2023) In the context of common prosperity the impact of provincial overall planning of basic medical insurance on the burden of medical expenditure. J Xi’ Univ Financ Econ 36(3):76–86
Kwon S (2010) Healthcare financing reform and the new single payer system in the Republic of Korea: Social solidarity or efficiency? Int Soc Security Rev 56(1):75–94
Latinsky-Ortiz EM, Strober LB (2022) Keeping it together: The role of social integration on health and psychological well-being among individuals with multiple sclerosis. Health Soc Care Community 30(6):E4074–E4085
Liang TK (2020) Residence certificate system, life course and psychological integration of new generation migrant population. J Public Manag 17(1):96–109
Liang Z (2016) China’s great migration and the prospects of a more integrated society. Annu Rev 42(1):451–471
Li R, Wu J, Yang HL (2022) The impact of provincial pooling of the basic medical insurance for employees on medical expenditures—An investigation based on CFPS data. Insurance Stud 43(6):83–98
Liu KH, Wang YJ (2022) Does trade openness affect migrant’s health? Evidence from China migrant dynamic survey. Soc Sci Guangdong 215(3):27–38
Liu T, Wei CC, Tong D (2020) Human capital, social support and social assimilation of floating population: A case study of Beijing. Popul Dev 26(2):11–22
Lin Y, Zhang Q, Chen W, Ling L (2017) The social income inequality, social integration and health status of internal migrants in China. Int J Equity Health 16(1):1–11
Liu LC (2020) The dilemma of the cross-provincial medical treatment of migrant population: The origin, policy analysis and removal of institutional barriers. J Sichuan Univ Sci Eng (Soc Sci Ed) 35(5):31–47
Li Y, Dou D (2022) The influence of medical insurance on the use of basic public health services for the floating population: The mediating effect of social integration. Int J Equity Health 21(1):1–15
Li YH, Liu NN, Chen HS, Shen BL (2022) Has the integrated medical insurance relieved the overwork of migrant workers? Chin Rural Econ 451(7):124–144
Lu HY, Kandilov IT, Nie P (2022) Heterogeneous impact of social integration on the health of rural-to-urban migrants in China. Int J Environ Res Public Health 19(16):1–14
Ma C, Qu ZP, Song Z (2018) Inequality of opportunity of floating population’s health care under the integrated medical insurance system—Paradox of the ex-ante or ex-post compensation principle. China Industrial Econ 36(2):100–117
Mathauer I, Saksena P, Kutzin J (2019) Pooling arrangements in health financing systems: A proposed classification. Int J Equity Health 18(1):1–11
Miao SY, Xiao Y (2020) Effects of social integration, sense of belonging on migrants’ mental health—Based on 2014 internal migrant dynamic monitoring survey data. J Soc Dev 7(2):110–127
Park RE (1928) Human migration and the marginal man. Am J Sociol 33(6):881–893
Pilvar H, Yousefi K (2021) Changing physicians’ incentives to control the c-section rate: evidence from a major health care reform in Iran J Health Econ 79(1):1–25
Shen YP (2022) Medical insurance pooling, utilization and welfare: Intervening mechanisms of the rise in medical expenses with pooling at the provincial level. Chin Soc Security Rev 6(4):83–101
Wei SQ, Kong FL, Li SX (2021) The effects of social support and morbidities on self-rated health among migrant elderly following children to Jinan, China. Healthcare 9(6):686
Wu J, Li R, Lu JQ (2022) Can basic insurance equalization alleviate health inequality—Evidence from the provincial coordination of employee insurance. China Health Insurance 15(18):43–52
Xia L, Shen HL (2022) Has the floating population really integrated into the society? —Research on social integration of floating population based on structural equation model. Popul Dev 28(2):138–151
Xiao BY, Zhu Y, Lin LY (2021) The subjective social integration of migrants from the perspective of multidimensional coupling: A case study of Fuzhou-Xiamen-Guangzhou urban cluster. Hum Geogr 36(2):120–126
Yang JH (2010) Index of assimilation for rural-to-urban migrants: A future analysis of the conceptual framework of assimilation theory. Popul Econ 179(2):64–70
Yuan HB, Deng HL (2021) Impact of basic public health services on health of floating population—Empirical analysis based on CMDS2018 data. Soc Scientist 292(8):104–107
Yuan T (2022) Scientific connotation and path optimization of provincial overall planning of basic medical insurance. Acad J Zhongzhou 44(12):85–94
Zhang GY, Wu SL (2022) Migration, insurance and utilization: An empirical study of the elderly migrant population —On the paths and goals of health insurance integration. Soc Sci Guangdong 39(6):199–211
Zhang KZ, Gao ZB, Zhang LN, Cheng Q (2020) Migratory-bird flow or permanent migration? —Public services accessibility and population migration options based on the perspective of social integration. Res Econ Manag 41(7):112–133
Zheng C, Wang XJ, Sun Q (2022) The integrated urban-rural medical insurance, health shocks and targeted poverty alleviation. J Public Manag 19(1):146–158
Zhou JJ, Zhu L, Zhang JW (2022) Social integration and health among young migrants in China: mediated by social mentality and moderated by gender. Front Psychol 13:1–12
Zhou Q, Tian S, Pan J (2016) Inequity of equalization—Theoretical and empirical analysis on beneficial equity of the urban resident basic medical insurance in China. Econ Res J 51(6):172–185
Zhu ZK, Zheng YX, Chen SL, Leng CX (2022) Equalization of public health services and social integration of migrant workers. Public Finan Res 43(7):52–65
Acknowledgements
We would like to thank Jiangsu University, School of Management, Department of Public Administration, and Nanjing University, School of Government, Department of Social Medicine and Health Administration, and other colleagues for their support and help in this study. Without their timely help, this study would not have been finished successfully.
Funding
This work was supported by the National Natural Science Foundation of China (Grant No. 72174078 to Xinjie Zhang), the National Natural Science Foundation of China (Grant No. 71804061 to Xinjie Zhang) and A Project Funded by Jiangsu University “Blue Project” (2022). There was no role of this funding agency in this study except the provision of funds.
Author information
Authors and Affiliations
Contributions
Xinjie Zhang is responsible for conceptualization, methodology, formal analysis, writing-original draft. Wei Chen is responsible for data curation, formal analysis, writing-original draft, writing-review & editing, supervision.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
The data used in this paper is based on secondary data, which has already collected by Center for Social Survey, Sun Yat-sen University and is available in public domain for research purpose. Therefore, no ethics approval was required from any institutional review board.
Informed consent
The data used in this paper is based on secondary data, which has already collected by Center for Social Survey, Sun Yat-sen University. Therefore, I do not have any informed consent.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhang, X., Chen, W. Can provincial-pooling of urban and rural resident basic medical insurance improve the health performance of migrant population?. Humanit Soc Sci Commun 11, 983 (2024). https://doi.org/10.1057/s41599-024-03476-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1057/s41599-024-03476-6
- Springer Nature Limited