Abstract
Understanding vaccine hesitancy has become increasingly important during the COVID-19 pandemic as governments around the globe have been struggling to convince portions of their populations to participate in vaccination protocols. Here we report on a nationally representative survey of the United Kingdom in which data revealed that individuals showed more willingness to take fictitious vaccines (putatively produced by the US government Medicare program and the now defunct healthcare company Theranos) than to take the Sputnik and Sinovac vaccines (developed by the Russian and Chinese governments respectively). The data indicate that the critical factor in vaccine hesitancy among the respondents was anxiety rather than familiarity with vaccines.
Similar content being viewed by others
Background
The novel coronavirus (SARS-CoV-2) is a highly contagious virus that was first identified in Wuhan, China in December 2019. The newly discovered virus causes the COVID-19 disease, which spreads rapidly within and across borders. In March 2020 the World Health Organization (WHO) assessed COVID-19 “as a pandemic… and called every day for countries to take urgent and aggressive action” (WHO, 2020). The pandemic has had a devastating effect worldwide (Johns Hopkins Coronavirus Resource Center, 2022). Early in the pandemic there was no proven method of treatment, and governments had to scramble to provide supportive care, with older people and those with underlying health conditions being more susceptible to serious illness. In the absence of effective treatment, countries around the world attempted to contain the spread of the virus by issuing travel bans, enforcing quarantines and lockdowns, and developing social distancing and mask-usage protocols. In response to the need for an effective treatment to combat the virus, the world’s scientific community mobilized and we witnessed a ‘generation’s Sputnik moment’ (Johnson and Dou, 2020) as leading pharmaceutical companies and scientists raced to develop and test vaccines through rigorous (but rushed) clinical trials (Murphy et al., 2021).
However, this sense of urgency in finding a vaccine was not shared across all demographics. False information and homemade remedies were increasingly shared online, and sometimes promoted by conservative politicians (BBC News, 2020). As an anti-vaxxer movement mobilized and spread utilizing social media platforms, administrators of such platforms found themselves “struggling to control online health dis- and misinformation” that threatened to dominate online discourse (Johnson et al., 2020). The SAGE working group on “vaccine hesitancy” defined the latter as “delay in acceptance or refusal of vaccination despite availability of vaccination services,” noting that this complex problem is context specific and “influenced by factors such as complacency, convenience and confidence” (MacDonald et al., 2015). Research on the factors influencing vaccine hesitancy and strategies for mitigating it predates the emergence of COVID-19 is not new (Bianco et al., 2019; Guay et al., 2019; MacDonald et al., 2018), but it took centre stage as the pandemic progressed (Dror et al., 2020; Puri et al., 2020).
A systematic review of existing peer-reviewed research using key search terms “Vaccine hesitancy AND COVID-19” found lower acceptance of vaccines among women, Blacks/Africans, unemployed people, and lower income, lower education, lower age cohorts (Troiano and Nardi, 2021). Religiosity was also negatively correlated with willingness to take a COVID-19 vaccine, while declared democratic political support was positively correlated. This review of fifteen studies found that the most common reasons given for refusal were: “being against vaccines in general, concerns about safety/thinking that a vaccine produced in a rush is too dangerous, considering the vaccine useless because of the harmless nature of COVID-19, general lack of trust, doubts about the efficiency of the vaccine, belief to be already immunized, doubt about the provenience of vaccine” (Troiano and Nardi, 2021).
Previous research during the pandemic has found a variety of factors influencing vaccine hesitancy or refusal in different contexts, some of which are particularly relevant for our study. Concern about the safety of vaccines or their potential side-effects was the most common reason expressed for vaccine hesitancy in both a study of Chinese adults (Liu et al., 2021) and a study of low to middle income countries (Solís Arce et al., 2021). Anxiety about the efficacy and safety of eventual COVID-19 vaccines was also a predictor of vaccine hesitancy in populations surveyed in Portugal and Italy (di Giuseppe et al., 2021; Soares et al., 2021). Studies in the US found that hesitancy about future COVID-19 vaccines was associated with factors, such as younger age, lower educational attainment, and conservative political ideology, and common reasons given for hesitation included need for more information and lack of trust (Fisher et al., 2020; Fridman et al., 2021). A study using a representative sample of Ireland (N = 1041) and the UK (N = 2025) explored the psychological characteristics associated with COVID-19 for vaccine hesitancy and resistance and found that in both countries the latter were significantly associated with three demographic factors: sex, age, and income level. Women, younger age cohorts, and individuals with lower income levels were more likely to be hesitant or resistant to vaccination (Murphy et al., 2021).
The United Kingdom was the first country to approve a COVID-19 vaccine tested in a large clinical trial. On December 2, 2020, UK regulators granted emergency-use authorization of the Pfizer-BioNTech vaccine, seven months after the start of clinical trials (Ledford et al., 2020). Shortly afterward, on December 30, the Oxford-AstraZeneca vaccine was approved for first use (AstraZeneca’s COVID-19 Vaccine Shows Effectiveness against Indian Variants of SARS-CoV-2 Virus, 2021). As of December 15, 2021, more than 43 million people in the UK have had at least one dose (population of 67.61 million), 39.2 million have received a second dose and a further 20.7 million have received a booster/third dose (Morgan, 2021). A recent survey (Office for National Statistics, 2021) found that, as of December 3, 2021, most (90%) double-vaccinated adults would likely accept a booster Covid-19 vaccine. However, within the double-vaccinated category 1 in 20 were very unlikely or fairly unlikely to have a booster if offered. Common reasons for booster refusal included belief that the second vaccine is enough to keep them safe (59%) or that the booster will not offer any further protection (49%). Additionally, respondents expressed concerns about long-term effects on health (33%) and about whether the booster should be offered to others instead of themselves (22%). This study sought to explore knowledge and willingness to take Pfizer-BioNTech and other vaccines developed in the West, e.g., Moderna (US) and Janssen-J&J (The Netherlands), as well as vaccine programs developed in Russia and China. Russia’s Sputnik vaccine reported 91.4% efficacy for its vaccine (COVID-19 Sputnik V); however, these figures have been contested because only 39 of the 18,000 people in the trial tested positive for COVID-19 (Ling, 2021). China’s Sinovac phase three trials conducted in Brazil, Chile, Indonesia, Turkey and the Philippines have given disparate unpublished results (Dyer, 2021). Researchers in Brazil have found Sinovac to have a 50.7% efficacy which increases to 62.3% with longer dosing intervals, while Turkish researchers have reported a much higher 83.5% efficacy (Dyer, 2021).
Vaccine hesitancy, which can be driven by conspiracy theories, fear, doubt, distrust of scientific expertise, and lack of information (Haerlin and Parr, 1999; Larson, 2020), puts lives at risk. The stakes are high. In order to contribute to a better understanding of the factors influencing vaccine hesitancy, we investigated a representative UK sample and explored the link between knowledge about vaccines and willingness to become vaccinated.
Methods
The sample consisted of N = 537 UK adults who completed a survey on their religious and political beliefs as well as their eagerness, willingness, and hesitance to take various global COVID-19 vaccines—with two vaccines “Theranos” and “Medicare” being fake. The survey was piloted with a soft-launch on social media (which had 37 respondents, who were included in the final sample) followed by a representative sample recruited via Prolific in March 2021. Using the Prolific platform, participants were directed to an online survey. The first information presented to the participant was informed consent. Informed consent was provided by all participants, at the informed consent prompt, the participant was informed about the use and anonymization of the data and that survey responses guarantee the anonymity of each participant. The study was done in line with the ethical guidelines and approval of Kingston University. Participants were compensated £1.29 for their participation.
The survey started by asking about the participant’s level of education, age, gender, race/ethnicity, religious and spiritual identity (asking specifically with which group they align themselves), what region from the UK they are from, annual income, relationship status, frequency of social media use (focusing on Twitter, Reddit, Facebook, and Instagram specifically), whether they are in a risk population for COVID, and their political beliefs. The measure of political beliefs used a scale that presented the participant with two sliders where they can rate their political beliefs, one slider for economic beliefs and one slider for social beliefs. The sliders are anchored with “very liberal” (0) and “very conservative” (100).
The survey then asked if the participant had been vaccinated. If they had been vaccinated, they were asked how anxious they felt about taking the vaccine. If not, they were asked if they would take the vaccine if offered and whether they would get it immediately when offered, delay, or refuse to get it. They were also asked to report their feelings toward receiving the vaccine (on a scale from very positive to very negative), what they would do if the vaccine was available at their local pharmacy, whether they would encourage their friends or family to get the vaccine, whether they are encouraged by friends or family to get the vaccine, whether they find taking the vaccine important, and whether they would describe themselves as eager to get the vaccine or were against vaccination for COVID-19.
Participants were then asked to rate how knowledgeable they are (on a scale of “I have never heard of this vaccine” to “I know a lot about this vaccine”) about the following vaccines: Novavax, Janssen-J&J, Theranos, Medicare, Moderna, Pfizer-BioNTech, Oxford-AstraZeneca, Sinovac, and Sputnik V. They were then asked to rate if they would take a vaccine developed by the companies on a scale from “Strongly disagree” to “Strongly agree”.
Participants were also asked whether they would take a vaccine given at a hospital, church, mobile ambulance, pharmacy, university, mosque, Jewish temple, Hindu temple, other religious location, or be willing to take it if self-administered. They were then asked if community leaders and religious/spiritual leaders in their community supported the vaccine, whether they trust religious/spiritual leaders in health-related matters and whether they would listen to the suggestion of religious/spiritual leaders regarding the vaccination. This was followed by a self-report rating (from 0 to 100) of their view of the severity of the risks of COVID-19.
These questions were then followed by questions about their beliefs and identity. First, participants were presented with the 7-item verbal fusion scale to measure fusion with their nation. They were also given the 7-item verbal fusion scale to measure fusion with their religion (Gómez et al., 2011). Lastly, for tracking and renumeration, participants were asked how they found out about the survey. Overall, we found that the survey had a high completion rate. Most participants who did drop out did so at the informed consent page (3.2%), the rest (1.6%) dropped out at page 4. We believe the latter was due to survey fatigue since this was the longest page of the 4-page survey.
Analysis of the data was performed in R and relied heavily on OLS regression techniques. All p values utilized an α = 0.95 and assumed two-tailed tests, which were used to investigate: (1) what demographic factors, i.e., income, age, gender, religious and political beliefs affect vaccine hesitancy, and (2) how much knowledge participants felt they had about various global vaccines and whether this knowledge impacted their willingness to become vaccinated.
As with all studies of this kind there are inherent limitations. The use of a survey methodology limited our ability to cross-check the self-report measures of social media use. Ideally, in future research data from the users themselves would be collected in cooperation with the social media sites themselves to ensure data protection. In addition, future research should utilize a manipulation check to approximate any confounding effects of using the names of “Theranos” and “Medicare” in the research. While the names of the approved and (at the time of research) unapproved vaccines were already well known during the data collection period, future research could utilize other names that are not pre-existing institutions or organizations. Future research could also assess social and economic political beliefs using additional multi-dimensional measurements in order to determine whether particular social or economic beliefs or ideologies underly vaccine hesitancy.
Results
We found that 89.22% of participants would take the Oxford-AstraZeneca vaccine, while 88.24% would take the Pfizer-BioNTech vaccine. These are substantially higher than those who would take the Sinovac vaccine (37.65%) or Sputnik vaccine (37.25%). The results also showed that most individuals would take a vaccine that was listed in the survey but that does not actually exist (allegedly produced by Medicare or Theranos in the USA). 57.65% stated they are willing to take a vaccine made by Medicare and 55.10% stated that they are willing to take a vaccine made by Theranos.
There is a significant difference in eagerness by age group [F(2, 502) = 6.614, p = 0.001]. A post hoc analysis reveals this is driven by a difference between the 18–34 cohort and the 35–54 and 55+ cohorts (but not the 35–54 and 55+ cohort) with the youngest group having the lowest eagerness to take the vaccine and people in the older cohorts being more eager.
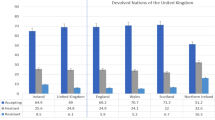
Most respondents were able to differentiate between the fictive and non-fictive vaccines: 10–15% of the population stated that they are “knowledgeable” about these vaccines, while 85–90% of the population stated that they had never heard of these vaccines (Fig. 1).
Despite the vast majority saying that they had never heard of the (fictive) Medicare and Theranos vaccines, 55–58% of participants indicated they would be willing to take them. It is important to note that Theranos, a US company that is now defunct, was involved in one of the largest medical frauds in US history.
To better understand the effects of information flow and trust in these (fictive and non-fictive) vaccines, we investigated the potential role of social media and political ideology. Participants were asked to estimate how frequently they used Twitter, Facebook, Reddit, and Instagram. They were also asked to report how conservative or liberal they are on social and economic issues (on a scale of 0—very liberal to 100—very conservative). We then created regressions where these variables were used to predict (1) how knowledgeable they felt about each vaccine and (2) whether the participants would take each of the vaccines.
When it comes to what predicted knowledge about the available vaccines (Table 1), we found that the more participants reported being more knowledgeable about Janssen-J&J and Moderna the more they used Twitter. In addition, we found a positive effect of economic conservatism and feeling knowledgeable about the Oxford-AstraZeneca vaccine, while there were negative effects of social conservatism for Moderna and Oxford-AstraZeneca. This suggests that the more liberal you are, the less you feel you know about Moderna and Oxford-AstraZeneca, while the more socially conservative, the more you know. Further, the more economically conservative you are, the more you know about Oxford-AstraZeneca, while the more economically liberal, the less you know.
Investigating the same effects among unavailable vaccines (Table 2) we found that Twitter use increased your knowledge about Sputnik. In addition, the more economically conservative you are, the more you felt you knew about Sputnik.
Regarding an individual’s willingness to be vaccinated using the available vaccines (Table 3), the study found that Frequency of using Twitter had a positive effect on willingness to take Janssen-J&J, Moderna, and Novavax. Interestingly, Frequency of Instagram use had a negative effect on willingness to take any of the approved vaccines except Oxford-AstraZeneca (for which we found no statistically significant effect). In addition, we also found that there is a negative effect on social politics and willingness to take Pfizer-BioNTech’s vaccine.
Finally, given the global discussion of misinformation on online social networks, we also investigated the willingness to take unavailable or fake vaccines using the same measures (Table 4). We found that Frequency of Twitter use had a positive effect on willingness to take both unavailable vaccines developed by Russia (Sputnik) and China (Sinovac) as well as non-existent vaccines developed by Medicare (a US government program) and Theranos (a now-defunct fraudulent healthcare company). In addition, Frequency of Instagram use had a negative effect on willingness to take the fictitious vaccines (Medicare and Theranos) but no effect on taking unavailable or poorly tested vaccines of Sputnik and Sinovac. We found no significant effects of social or economic-political leanings on willingness to take fictitious or unavailable vaccines.
Discussion
The key finding of this study is that social media use does have an effect on perceived knowledge about vaccines as well as on vaccine hesitancy. However, this effect is largely limited to the negative impact of Twitter use and a general anti-vax stance detected in relation to Instagram use. Despite Facebook’s attempts to heavily regulate and fact-check information on their system, it had no discernible effect on vaccine hesitancy in our sample. This is interesting when compared to Reddit, which has taken a more community-based approach to censorship of misinformation and has come under fire for doing so (Taylor, 2021). Nevertheless, we found no evidence that frequency of Reddit use was related to vaccine knowledge or vaccine hesitancy, which is noteworthy because users of Reddit (compared to users of other social media) spend more time on the site and are more likely to interact intensely with materials on the site (Chritine, 2018; C. Liu et al., 2010). However, Twitter use had particularly concerning effects. Its users felt as if they were more knowledgeable about several vaccines. This sounds like a good thing, but they also indicated more willingness to take fictive or fraudulent vaccines that had not in fact been approved. Moreover, respondents indicated more willingness to take fake vaccines than those tested and deployed in countries outside of the US or Europe. This suggests that one of the effects of Twitter use may have been the promotion of acceptance for Chinese and Russian vaccines. No other platform had such wide-ranging effects in either direction, which suggests that Frequency of Twitter use is the most likely factor influencing the finding that people, in general, found the fake vaccines more acceptable than the Chinese or Russian vaccines.
Our findings indicate that concern about the trustworthiness of foreign vaccine production and testing protocols may be playing an important role in vaccine hesitancy. It could be that respondents assumed that if the (fake) US-based vaccines were real, they would have gone through the relevant rigorous trials. It seems that anxiety surrounding the COVID-19 pandemic makes people willing to take vaccines they actually know nothing about (because they do not exist), but wary of taking real vaccines produced by countries with which the UK is currently entangled in geopolitical tension (Russia and China). We conclude that there is not a strong relationship between willingness to take a fake vaccine and knowledge about those vaccines. Nevertheless, we did find a relationship between willingness to take fake vaccines and anxiety about getting the vaccine. However, the fact that this anxiety is not related to eagerness to take the vaccine suggests that anxiety and fear, rather than hope, may be driving the trends revealed in this study.
Data availability
The datasets generated during and/or analyzed during the current study are available in the GitHub repository: https://github.com/culturepulse/vaccinehesitancy
References
AstraZeneca’s COVID-19 vaccine shows effectiveness against Indian variants of SARS-CoV-2 virus (2021) https://www.astrazeneca.com/media-centre/articles/2021/astrazenecas-covid-19-vaccine-shows-effectiveness-against-indian-variants-of-sars-cov-2-virus.html Accessed 15 Dec 2021.
Bianco A, Mascaro V, Zucco R, Pavia M (2019) Parent perspectives on childhood vaccination: how to deal with vaccine hesitancy and refusal? Vaccine 37(7):984–990. https://doi.org/10.1016/J.VACCINE.2018.12.062
BBC News (2020) Coronavirus: Outcry after Trump suggests injecting disinfectant as treatment. https://www.bbc.co.uk/news/world-us-canada-52407177 Accessed 15 Dec 2021.
Chritine C (2018) Holiday on Reddit—upvoted. https://redditblog.com/2018/11/13/holiday-on-reddit/ Accessed 15 Dec 2021
Coronavirus (COVID-19) latest insights—Office for National Statistics. https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/articles/coronaviruscovid19latestinsights/vaccines Accessed 15 Dec 2021.
Johns Hopkins Coronavirus Resource Center (2022) https://coronavirus.jhu.edu/map.html Accessed 15 Dec 2021
di Giuseppe G, Pelullo CP, della Polla G, Pavia M, Angelillo IF (2021) Exploring the willingness to accept SARS-CoV-2 vaccine in a University Population in Southern Italy, September to November 2020. Vaccines 9(3). https://doi.org/10.3390/VACCINES9030275
Dror AA, Eisenbach N, Taiber S, Morozov NG, Mizrachi M, Zigron A, Srouji S, Sela E (2020) Vaccine hesitancy: the next challenge in the fight against COVID-19. Eur J Epidemiol 35(8):775–779. https://doi.org/10.1007/S10654-020-00671-Y/FIGURES/3
Dyer O (2021) Covid-19: Chinese vaccines may need changes to improve efficacy, admits official. BMJ 373:n969. https://doi.org/10.1136/BMJ.N969
Fisher KA, Bloomstone SJ, Walder J, Crawford S, Fouayzi H, Mazor KM (2020) Attitudes toward a potential SARS-CoV-2 vaccine: a survey of U.S. adults. Ann Intern Med 173(12):964–973. https://doi.org/10.7326/M20-3569
Fridman A, Gershon R, Gneezy A (2021) COVID-19 and vaccine hesitancy: a longitudinal study. PLoS ONE 16(4). https://doi.org/10.1371/JOURNAL.PONE.0250123
Gómez Á, Brooks ML, Buhrmester MD, Vázquez A, Jetten J, Swann WB (2011) On the nature of identity fusion: insights into the construct and a new measure. J Pers Soc Psychol 100(5):918–933. https://doi.org/10.1037/A0022642
Guay M, Gosselin V, Petit G, Baron G, Gagneur A (2019) Determinants of vaccine hesitancy in Quebec: a large population-based survey. Hum Vaccines Immunother 15(11):2527–2533. https://doi.org/10.1080/21645515.2019.1603563
Haerlin B, Parr D (1999) How to restore public trust in science Nature 400(6744):499–499. https://doi.org/10.1038/22867
Johnson NF, Velásquez N, Restrepo NJ, Leahy R, Gabriel N, Oud S, el, Zheng M, Manrique P, Wuchty S, Lupu Y (2020) The online competition between pro- and anti-vaccination views Nature 582(7811):230–233. https://doi.org/10.1038/s41586-020-2281-1
Johnson YC, Dou E (2020) The global race for a coronavirus vaccine could lead to this generation’s Sputnik moment. Wash Post. https://www.washingtonpost.com/health/2020/06/03/coronavirus-vaccine-global-race/ Accessed 15 Dec 2021
Larson HJ (2020) Blocking information on COVID-19 can fuel the spread of misinformation. Nature 580(7803):306. https://doi.org/10.1038/D41586-020-00920-W
Ledford H, Cyranoski D, van Noorden R (2020) The UK has approved a COVID vaccine—here’s what scientists now want to know. Nature 588(7837):205–206. https://doi.org/10.1038/D41586-020-03441-8
Ling T (2021) COVID vaccine UK: what vaccines are there? When will they be ready? BBC Sci Focus Mag. https://www.sciencefocus.com/news/covid-vaccine-uk/ Accessed 15 Dec 2021
Liu C, White RW, Dumais S (2010) Understanding web browsing behaviors through weibull analysis of dwell time. In: Crestani F, Marchand-Maillet S, Chen H-H, Efthimiadis EN (eds.) SIGIR 2010 Proceedings—33rd annual international ACM SIGIR conference on research and development in information retrieval. Association for Computing Machinery, New York, NY, US, pp. 379–386
Liu R, Zhang Y, Nicholas S, Leng A, Maitland, E, Wang J (2021) COVID-19 vaccination willingness among Chinese adults under the free vaccination policy. Vaccines 9(3). https://doi.org/10.3390/VACCINES9030292
MacDonald NE, Butler R, Dubé E (2018) Addressing barriers to vaccine acceptance: an overview. Hum Vaccines Immunother 14(1):218–224. https://doi.org/10.1080/21645515.2017.1394533
MacDonald NE, Eskola J, Liang X, Chaudhuri M, Dube E, Gellin B, Goldstein S, Larson H, Manzo ML, Reingold A, Tshering K, Zhou Y, Duclos P, Guirguis S, Hickler B, Schuster M (2015) Vaccine hesitancy: definition, scope and determinants. Vaccine 33(34):4161–4164. https://doi.org/10.1016/J.VACCINE.2015.04.036
Morgan E (2021) Written statement: COVID-19 vaccination—JCVI announcement on vaccinating Children & Young People (19 July 2021) | GOV.WALES. https://gov.wales/written-statement-covid-19-vaccination-jcvi-announcement-vaccinating-children-young-people Accessed 15 Dec 2021
Murphy J, Vallières F, Bentall RP, Shevlin M, McBride O, Hartman TK, McKay R, Bennett K, Mason L, Gibson-Miller J, Levita L, Martinez AP, Stocks, TVA, Karatzias T, Hyland P (2021) Psychological characteristics associated with COVID-19 vaccine hesitancy and resistance in Ireland and the United Kingdom. Nat Commun 12(1). https://doi.org/10.1038/s41467-020-20226-9
Puri N, Coomes EA, Haghbayan H, Gunaratne K (2020) Social media and vaccine hesitancy: new updates for the era of COVID-19 and globalized infectious diseases. Hum Vaccines Immunother 16(11):2586–2593. https://doi.org/10.1080/21645515.2020.1780846
Sputnik V. Second interim analysis of clinical trial data showed a 91.4% efficacy for the Sputnik V vaccine on day 28 after the first dose; vaccine efficacy is over 95% 42 days after the first dose. https://sputnikvaccine.com/newsroom/pressreleases/second-interim-analysis-of-clinical-trial-data-showed-a-91-4-efficacy-for-the-sputnik-v-vaccine-on-d/ Accessed 15 Dec 2021
Soares, P, Rocha JV, Moniz M, Gama A, Laires PA, Pedro AR, Dias S, Leite A, Nunes C (2021) Factors associated with COVID-19 vaccine hesitancy. Vaccines 9(3). https://doi.org/10.3390/VACCINES9030300
Solís Arce JS, Warren SS, Meriggi NF, Scacco A, McMurry N, Voors M, Syunyaev G, Malik AA, Aboutajdine S, Adeojo O, Anigo D, Armand A, Asad S, Atyera M, Augsburg B, Awasthi M, Ayesiga GE, Bancalari A, Björkman Nyqvist M, Omer SB (2021) COVID-19 vaccine acceptance and hesitancy in low- and middle-income countries Nat Med 27(8):1385–1394. https://doi.org/10.1038/s41591-021-01454-y 27:8
Taylor J (2021) Reddit defends how it tackles misinformation as it opens Australian office | Reddit | The Guardian. https://www.theguardian.com/technology/2021/jul/14/reddit-defends-how-it-tackles-misinformation-as-it-opens-australian-office Accessed 15 Dec 2021
Troiano G, Nardi A (2021) Vaccine hesitancy in the era of COVID-19. Public Health 194:245–251. https://doi.org/10.1016/J.PUHE.2021.02.025
WHO (2020) Director-General’s opening remarks at the media briefing on COVID-19. https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 Accessed 15 Dec 2021
Acknowledgements
The authors are grateful to Kingston University, London, for funding the data collection, and to the Research Council of Norway for funding the “Emotional Contagion: Predicting and Preventing the Spread of Misinformation, Stigma, and Anxiety During a Pandemic” (EmotiCon) project, which partially supported the research time for FLS and JEL during the writing of this paper.
Author information
Authors and Affiliations
Contributions
Conception/design of the work (all authors); acquisition of data (JEL); analysis of data (JEL); interpretation of findings (all authors); drafted and revised the work (all authors).
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
All participants and their data are assumed to have the widest data rights in accordance with The Data Protection Act 2018 (UK); GDRP rights are also extended to non-UK citizens regardless of location or residency and data can be deleted (right to be forgotten) at the request of a participant at any time. All research was limited to anonymous survey information with no additional personal information recorded or analyzed beyond that shown in the survey to the participants. All research was performed in accordance with the Declaration of Helsinki. This research was approved by the internal ethical review board at ALAN Analytics s.r.o., in agreement with the University of Kingston. All research was performed in accordance with the relevant guidelines and regulations and data is made open source for future use in the electronic appendix.
Informed consent
Informed consent was obtained from all participants.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bullock, J., Lane, J.E. & Shults, F.L. What causes COVID-19 vaccine hesitancy? Ignorance and the lack of bliss in the United Kingdom. Humanit Soc Sci Commun 9, 87 (2022). https://doi.org/10.1057/s41599-022-01092-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1057/s41599-022-01092-w
- Springer Nature Limited
This article is cited by
-
A synthesis of evidence for policy from behavioural science during COVID-19
Nature (2024)
-
Determinants of COVID-19 vaccine uptake among Nigerians: evidence from a cross-sectional national survey
Archives of Public Health (2023)
-
Experiences and perceptions of COVID-19 infection and vaccination among Palestinian refugees in Jerash camp and Jordanian citizens: a comparative cross-sectional study by face-to-face interviews
Infectious Diseases of Poverty (2022)
-
Vaccine Hesitancy: Obstacles and Challenges
Current Pediatrics Reports (2022)