Abstract
The COVID-19 pandemic has resulted in more than 282 million cases and almost 5.5 million deaths (WHO Coronavirus Disease (COVID-19) Dashboard, 2022). Its impact, however, has not been uniform. This analysis examines differences in COVID-19 cases and mortality rates amongst different welfare states within the first three waves of the pandemic using repeated measures Multivariate Analysis of Covariance (MANCOVA). Liberal states fared much better on the number of COVID-19 cases, deaths, and excess deaths than the Conservative/Corporatist welfare democracies. Social Democratic countries, in turn, did not fare any better than their Conservative/Corporatist counterparts once potential confounding economic and political variables were accounted for: countries’ economic status, healthcare spending, availability of medical personnel, hospital beds, pandemic-related income support and debt relief, electoral events, and left-power mobilization. The pandemic-related welfare responses after the first wave were similar across all three types of western democracies, but the differences in pandemic outcomes remained. The somewhat better outlook of the Liberal states could be attributed to the so-called social democratization of the Anglo-American democracies, but also to the fact that neoliberalism could have flattened the previous differences between the welfare states typologies and could have brought states closer to each other, ideologically speaking, in terms of welfare provision.
Similar content being viewed by others
Introduction
Once the World Health Organization (WHO) declared COVID-19 a pandemic on March 11, 2020, infection numbers climbed globally (WHO 2022). In a matter of days, Italy reached thousands of cases (Mayberry et al. 2020) and the Italian medical staff was asked to triage cases on a utilitarian basis (Romeo 2020). By the end of March 2020, most continental European states, Belgium, Germany, France, and Spain, were implementing strict lockdown measures. Through the month of May, Italy and Spain were battling over 200,000 cases each, and Germany and France were closely following suit. The Scandinavian nations showed a better outlook: from a low number of cases in Iceland, to moderate numbers in Denmark, with the highest numbers being reported in Sweden: over 84,300 confirmed cases. The pandemic seemed to have spared the Mediterranean region during these initial months. Greece for example, reported just over 6,600 cases and Croatia just over 6200 by mid-August 2020. The UK initially refused to impose restrictions on the freedom of movement and delayed a compulsory lockdown. Cases started to escalate and so did the mortality rate before any measures were issued (Burn-Murdoch and Giles 2020; Siddique 2020). At almost 14.5 million confirmed cases and 150,000 deaths as of January 2022, the UK has remained one of the worst affected countries in Europe (WHO 2022). Outside Europe, the US has reported one of the highest confirmed case counts, sitting at approximately 59 million. Canada had just over 2.4 million cases by early January 2022. Australia and New Zealand had over 922,000 and 14,000 cases, respectively.
It is difficult to adopt a one-size-fits-all interpretation as to why certain states experienced higher numbers of infections during the beginning of the pandemic while others kept theirs in check. For instance, Greece’s initial success was attributed to its capacity to implement timely and stringent lockdown measures (Labropoulou 2020). Greece closed all schools when less than 100 cases were reported in the country, it restricted domestic traveling on proof of residency, and required dwellers to either use a text messaging service or to complete, sign, and print a declaration indicating their reason for venturing outside (Ekathimerini News 2020; Labropoulou 2020; Wiley 2020). Germany was quickly branded as the ‘global leader’ on COVID-19 response (Evans 2020) as it initially reported a lower death rate, in comparison with other nations reporting similar infection numbers (Reisinger 2020). In recording higher deaths than the neighboring Denmark, Sweden was blamed for its softer, no-lockdown measures. While the country banned gatherings of more than 50 people, closed educational institutions and encouraged older citizens to stay indoors, the Swedish society and economy remained open overall (Jackson 2020). South Korea was applauded on its wide-ranging testing capability (Kim 2020), while Hong Kong’s success was largely attributed to its citizens’ vigilance (Wong et al. 2020).
The end of 2020 was marked by the US Food and Drug Administration (FDA) emergency approval of Pfizer’s and Moderna’s COVID-19 vaccines (Bryson Taylor 2021), turning most of 2021 into a global race to vaccinate. Most vaccine orders have been procured by Western states with little regard for the epidemiological needs of Global South countries. By the end of August 2021, more than three quarters of the COVID-19 vaccine doses have been used by Canada, the US, the UK, Switzerland, and the EU member states (Bejan 2021a). Canada, for example, ordered several times the doses it needed to fully immunize its 37 million population, as the country signed supplier agreements for 180 million double doses for Moderna, Pfizer-Biontech, AstraZeneca and Johnson & Johnson (Government of Canada 2021). Despite the massive vaccination campaigns conducted in the West, most countries continued to report high levels of infections, particularly due to the emergence of new variants, such as the outburst of the Delta variant in the UK that drove most cases in the country during the Third Wave (Bejan and Nikolova 2021).
In trying to make sense of such differences in cases, deaths, vaccination rates and overall state-supported pandemic responses, this analysis examines the variation of COVID-19 numbers and mortality rates from the beginning of the pandemic and until the end of the Third Wave, in a sample of countries with strong welfare policies yet different welfare regime orientations.
A welfare-state approach to COVID-19
Comparing nations has always been a difficult task in the social policy field. Starting from a political economy approach, this analysis uses the classic welfare state typology developed by Esping-Andersen (1990) as comparative grounds. A welfare regime, philosophically speaking, aims to mediate the negative consequences of the primary economic distribution that takes place through the market, hence it places the state ‘in charge’ of the secondary distribution of societal resources. Through complex programs of benefit provision, such as sick days, maternity leave, unemployment support and social assistance, welfare provision becomes about the state’s ability to assist in the delivery of well-being across various social aspects: health care, old age, family matters; as well as to correct and re-order unequal social relations (Esping-Andersen, 1990).
The idea of welfare is a Western product. It materialized, at the end of the nineteenth century, with the German social insurance model under Otto von Bismarck, which introduced coverage for sickness (1883), accident (1884) and old age and invalidity (1889). These programs were quickly copied by Denmark and the neighbouring Nordic states (Kuhnle and Sander 2010). In the interwar period, social security principles started to take ground, and with the beginning of the Great Depression, universalistic ideas started to embody a social citizenship/social rights model of guaranteeing economic security (Asatiani and Verulava 2017; Castles et al. 2012; Lightman and Lightman 2017). The expansion of social benefits started from 1945 and lasted until about the 1973 oil crisis, when a retraction in general support for public services followed (Castles et al. 2012; Lightman and Lightman 2017). It was during this time that most Western democracies established their national health care, family allowances and old age security programs (Lightman and Lightman 2017). The idea of welfare translated into health care through the reasoning that health provision, delivery and regulation determine health outcomes within national borders (Freeman and Rothgang 2012).
Public policy scholars, economists, and political scientists have taken great interest in analyzing variations of welfare provision in the Western world. The classic typology of the welfare states, and the one most often referenced in the field, was developed by Dutch sociologist Gøsta Esping-Andersen (1990). In moving away from a narrow ideological view that sees welfare provision in terms of tokenistic social amelioration and limits it to income transfers and social services, Esping-Andersen (1990) brought into focus political economy questions about the state’s role in relation to employment, wages, and macro-economics and the state’s role in de-commodifying the individuals from their dependence on the labour market. Considering a diverse set of criteria related to social rights, social stratification, and their distribution across the market, the family, and the state, and focusing on unique variables, such as decommodification (one’s standard of living independently accounted from labour market participation or the so called degree of labour decommodification); social stratification (the role of the state institutions in structuring social order or the distribution of public entitlements based on needs, social contributions, or citizenship regimes); and the public–private nexus (the role of the state, family, and the market in welfare provision) (Van Voorhis 2002; Esping-Andersen 1990); ; proposed three main types of welfare provision: liberal, social democratic, and conservative.
The Liberal states loosely correspond to the Anglo-Saxon regimes: Canada, the US, Ireland, the UK, Australia, New Zealand; and Japan, as the only liberal non-Western state. The Social Democratic states encapsulate the Northern European region: Sweden, Norway, Denmark, Finland, Iceland and the Netherlands. The Conservative/Corporatist ones are mainly in continental Europe: Italy, Greece, France, Germany, Austria, Switzerland, and Belgium.
Generally speaking, the Liberal systems of welfare provision are characterized by minimalist governmental intervention, modest benefits and social insurance plans that perpetuate class distinctions, a guaranteed support of the market, and an increased focus on individualizing personal responsibility for societal troubles. In turn, the Social Democratic regimes are invested in universal coverage, a strong focus on government intervention, and centered on principles of middle-class universalism and social equality in welfare distribution. The Conservative states tend to be characterized by a minimum level of welfare provision, usually negligible in impacting status differentials and mainly allocated on means-tested measures (Asatiani and Verulava 2017; Esping-Andersen 1990; Van Voorhis 2002). Also named Corporatist by Esping-Andersen (1990), the Conservative states preserve the centrality of family in providing well-being. Metaphorically speaking, the Social Democratic models respond to a range of social needs; the Conservative regimes condition welfare provision on social insurance principles; and, the Liberal states filter societal well-being through minimum public intervention.
Esping-Andersen’s typology insists on western democracies and pays little attention to the newly established democratic states from the former socialist and communist bloc; nor to hybrid regimes, such as China, officially a communist, or better said, a state capitalist regime, yet one that established several welfare policies, such as compulsory education; nor to South Korea, which managed, for example, to achieve universal coverage for a variety of health benefits, from physician and specialist care to drug prescriptions (Chaskin et al. 2019).
Esping-Andersen (1990) also considered the southern European states of Greece, Spain, and Italy as immature continental welfare democracies. In fact, Esping-Andersen conceptualized any unorthodox state, that would not easily fit into his classification, as unstable. The steady regimes were only those adaptable under the Liberal, Social Democratic, and Conservative types.
Despite methodological and conceptual inconstancies, Esping-Anderson’s typology has been the most influential within the field of comparative research linking social policy and public health. In fact, alternative welfare typologies seem to be conventional derivations from Esping-Anderson’s model. Most contain similar countries yet divided into sub-groups. For instance, Leibfried (1993) split the Conservative states into a ‘Bismarck’ type and a ‘Latin rim’; Ferrera (1996) included a distinct Southern category (i.e., Greece, Italy, Portugal, Spain) and excluded Australia, Canada and the US from the Anglo-Saxon type; Navarro and Shi (2001) labelled the Conservative states as Christian Democrat and divided some of them into an ex-fascist group containing Spain, Greece and Portugal; and Bambra (2005a) included a subgroup amongst the Liberal states which included Ireland, the UK and New Zealand, while the ‘main liberal group’ was limited to Australia, Japan and the US. Moreover, a recent systematic review (Powell et al. 2020) showed a lack of consensus on updating Esping-Anderson’s archetype.
Countries in this analysis fit Esping Anderson’s model. South Korea was the only additional country included and it was added to the analysis because of the latest developments in its national welfare policies. South Korea fits under the Liberal type, due to its socio-political similarity to other states in this typology: a highly urbanized mixed-market economy, with an expanding welfare system which includes various social insurance and means-tested benefit schemes (Chaskin et al. 2019). While Esping-Anderson placed Japan into the Conservative/Corporatist type, Japan could also fit under the Liberal type. First, Esping-Anderson considered Japan a hybrid state. Second, a study replicating Esping-Anderson’s decommodification index found that Japan scored in the middle of the Liberal group (Scruggs and Allan 2006). Third, one of the most recent welfare state typologies developed by Bambra (2005a, b) also includes Japan amongst the Liberal states.
No other countries from the Global South or the former Soviet Bloc were included in this analysis. The intention here was not to draw a global portrait of how countries fared on COVID-19 cases and mortality rates, but rather to explore if typical strong welfare regimes, with well-developed systems of welfare provision had superior outcomes in managing the pandemic.
Similar to other systems of classification, Esping-Andersen’s typology does not and cannot capture all distinctions between individual states. Yet, a welfare state framework to examine differences on COVID-19 cases and mortality rates sheds light on how certain ideals of welfare provision translate in health care delivery amongst comparable countries and impact pandemic related health outcomes. Health care is distributed amongst several societal actors and this distribution is political. It depends on macro-economics, political systems, and ideas about what should be publicly provided. Welfare provision includes health care systems of managing and regulating health outcomes. Think about hospital beds for example. An adequate number of hospital beds will constitute, during a pandemic, a form of welfare provision that reflects the care of the state for its most vulnerable citizens. Beliefs about welfare provision trickle down through health policy, determine the type of care offered to the vulnerable and the sick, and materialize into national disease statistics, from routine mortality rates to infectious disease numbers in case of a pandemic. Concerned with questions of political economy, heath systems then are intrinsically connected with the welfare state. As Freeman and Rothgang (2012) put it: “It is the state, then, at least in advanced industrial countries […] which processes competing, sometimes complementary, and sometimes contradictory demands for health and health care” (p. 368).
Or think about income supports. COVID-19 has been branded an occupational disease (Bejan, Allain, Glynn, Wheatley and Soto Flores 2021b; Bejan, Allain and Glynn 2021c) mostly affecting essential workers, those unable to survive without subtracting themselves from a labour market which requires workers to be in proximity to one another, such as meat packers, fruit pickers or supermarket workers. It is a state’s welfare provision through pandemic related income supports, such as lockdown benefits, unemployment supports, wage subsidies, paid sick leave etc., that could lift workers from their dependency on the labour market, and support their well-being, hence protecting them from getting infected. The more generous an income replacement support and the higher the benefit level, the higher the decommodification potential of such benefits, the higher the welfare interventionism of a state, and in turn, the lower the COVID-19 infection rates.
Ideas about population health, medicare, subsidizing health care through redistributive taxation systems, social transfers and subsequent health expenditures, as well as ideas about protecting the most vulnerable subjects during a pandemic such as the COVID-19, are all emanating from philosophies of welfare provision and state responsibility. There would be no institutional response to a pandemic if societies would not have evolved, in the modern era, from the idea that health was the responsibility of churches and charitable institutions to health being seen as a form of welfare provision (i.e., the health care state) (Freeman and Rothgang 2012). More so, the entire social determinants of health framework, which is now a staple theory in social policy, is based on distributive welfare ideas. The social determinants of health (i.e., income and social status, education, employment and working conditions), whose provision constitute the raison d’être of the western welfare state, are the strongest predictors of individual health throughout one’s lifetime (Author 2013).
Welfare states have been considered health-stratifying factors, especially through mediating the distribution of social determinants of health (Bambra 2007, 2011). Literature has linked differences in health outcomes to different types of welfare regimes and showed that welfare interventions are effective in targeting health-related aspects and equalizing health outcomes, by levelling socioeconomic positions and decreasing social marginalization (Kaplan 2007; Olafsdottir 2007). Strong welfare states, with universal health care systems, robust family policies and social supports, tend to reduce the relationship between class stratification and health disparities (Bambra 2007; Kaplan 2007; Olafsdottir 2007).
Social epidemiology has long been using welfare state variables to analyze cross-national differences in population health. For instance, public medical coverage was found to be the most significant predictor of mortality and generous family supports were associated with lower infant mortality (Chung and Muntaner 2006; Lundberg 2010). Unequal societies, those where the state has failed to equitably re-distribute wealth and to invest in public systems of service provision, have much higher mortality rates than those societies that rely on strong public sectors and equitable taxation systems for wealth re-distribution. A recent study conducted by the Institute for Public Policy Research North in the UK is particularly telling in this regard: mortality rates were found to be higher in certain regions in Blackpool, Manchester and Hull, than in some of the most underdeveloped regions of Romania (Raikes et al. 2019). This despite the fact that the UK’s GDP is about eleven times higher than that of Romania. Yet, the UK has one of the highest inequality rates amongst developed nations (Bejan 2019). There is no doubt that welfare provision trickles down through health policy, determines the type of care provided to the vulnerable and the sick, and materializes into national disease statistics, from routine mortality rates to infectious disease numbers in case of a pandemic.
Welfare state typologies have been critiqued on erasing important policy differences between nations; however, comparative social epidemiology expanded them to theorize population health and health distribution (Bambra 2011). A welfare state lens is congruent to understanding how disparities in COVID-19 infections and mortality rates are distributed amongst similar states. If routine mortality rates can be analyzed through a welfare state approach, there are no reasons as to why COVID-19 mortality cannot.
It is from within this context that this paper has taken the welfare regimes as proxies for managing pandemic related outcomes. We hypothesize that the stronger a welfare democracy, the stronger their system of health care provision, as in the greater their level of health coverage, and the higher their numbers of doctors and nurses; the higher their left-power mobilization; the higher their provision of pandemic-related income supports, the higher the decommodification of people from the labour market; hence the lower their COVID-19 cases, mortality and overall excess death rates. In other words, we expect the Social Democratic states to have lower levels of societal inequality, to have better prepared health care systems, to provide comprehensive pandemic-relates benefits, as well as to have higher testing and vaccination rates, stringent lockdown measures and required mask policies, due to the nature of their strong state and mediated through strong trust in national government; hence we expect them to experience much lower COVID-19 rates than the Corporatist regimes whose benefit provision tends to be reliant on actuarial, social insurance principles or the Liberal states who tend to rely on means-tested, selective benefit schemes and overall on low state interventionism within public matters.
Methods and measures
Gathering data on COVID-19 before the end of the pandemic comes with limitations. First, the numbers included in the sample are by no means the final figures. Second, since a cross-country, universal benchmark for testing is nonexistent, it proves difficult to know if the reported cases represent an accurate number of infections. For example, cases can be high because they directly reflect sizable testing efforts undertaken in a country or cases can be low because of underreporting. Death rates based on the total number of cases are subsequently unreliable as such figures depend on the number of tests. Reporting on COVID-19 deaths and the completion of COVID-19 death certificates depend on national legislative frameworks, making it difficult to have a universal benchmark of measuring deaths directly connected with the virus (West et al. 2020).
To account for differences in reporting and testing, this analysis uses the following measures to assess cross-national differentiations: (1) the number of cases per 100,000; (2) the number of deaths per 100,000; and (3) the number of excess deaths per 100,000. High excess mortality is a common aftereffect of low reporting (Dyer 2021), which is why exploring the number of deaths within a timeframe compared to how many deaths would be expected had there been no pandemic, can provide a more accurate estimate of pandemic-related mortality. These numbers allow for comparisons across countries as they permit per capita estimates of the impact of COVID-19 while accounting for COVID-19 underreporting and undertesting. The countries under analysis by welfare regime are presented in Table 1.
Data was drawn from the World Health Organization (2022) and contains all officially reported COVID-19 cases and deaths until June 30, 2021, inclusive. The number of cases and deaths is broken down by wave. Average timelines for all countries in our sample were calculated to determine that Wave One of the pandemic started January 1, 2020 and ended on July 31, 2020; Wave Two started August 1, 2020 and ended on January 31, 2021; and Wave Three started February 1, 2021 and ended June 30, 2021. Population data was taken from the 2019 counts for each country to calculate per 100,000 rates for reported COVID-19 cases and deaths.
To control for differences between countries in terms of their economic status, income distribution, and healthcare capacity, the following variables were included in the analysis: gross domestic product (GDP), purchasing power parity (PPP), Gini index, inequality adjusted Human Development Index (iHDI), universal healthcare coverage, poverty gap, percent of GDP spent on health, and percent of healthcare costs as out of pocket expenses. Countries’ economic status, healthcare spending and availability of medical personnel were obtained from the OECD and the WHO. They were based on the latest year available for each country (OECD 2020a, b, c; WHO 2022). Healthcare capacity was assessed by the availability of hospital personnel (i.e., number of doctors per 10,000 people, number of nurses per 10,000 people), and the number of hospital beds per 10,000 people.
To account for different pandemic policies by type of welfare state, we included several variables related to state responses, decommodification and to what Esping-Anderson (1990) termed left-power mobilization. State-response measures included governments’ stringency index (i.e., national lockdowns taken as two weeks after the start of each wave), the implementation of mask policies (i.e., recommended, required, or no policy at all), states’ testing capacity per 1000, vaccination rates, and trust in national government.
The impact of politics in a society is crucial for what a welfare state will look like, and Esping-Anderson (1990) examined the party-composition of national cabinets to measure the effects of left-leaning electoral political power on the decommodification of individuals from the labour market. Three political power variables have been included in this analysis: each country’s ruling party’s political ideology (on a ten-point continuum from leftwing to rightwing); the personal freedom ideology of the ruling party (on a ten-point continuum from libertarian to authoritarian) and the deployment of electoral events (i.e., national elections).
The extent that states have been engaged in decommodification during the pandemic has been captured through proxy variables such as income supports, debt relief and the economic regulation of the government (on a ten-point continuum of state to market control). To account for the quality of pandemic-related welfare benefits, the income support variable was classified by level of coverage (i.e., income support covers less/more than 50% of salary). See Table 2 for a complete list of variables.
Bivariate analyses (one-way ANOVA) examined differences between the three types of welfare regimes and the continuous predictors. Fisher’s exact analyses examined differences between the welfare regimes and the categorical predictors (chi-square could not be used due to the small sample sizes). Correlation analyses examined the relationships between the continuous variables. A repeated measures Multivariate Analysis of Variance (MANOVA) assessed the relationship between time/each wave of the pandemic, the type of welfare state, and the number of COVID-19 cases, COVID-19 deaths, and excess deaths. This method considers both within-subjects factors (time) and between-subjects factors (type of welfare state) and their effect on related outcome measures (cases, deaths, and excess deaths), while also considering the effects of the outcome variables on each other. A repeated measures Multivariate Analysis of Covariance (MANCOVA) also examined the potential impact of health, economic, and policy covariates on the relationship between type of welfare state and the outcome measures (cases, deaths, and excess deaths). Bonferroni adjustments were used in all bivariate and multivariate analyses to control for experiment wise error. All statistical analyses were conducted in SPSS, Version 27.
Results
Descriptive and bivariate results
COVID-19 cases and deaths per 100,000 by wave are presented in Table 3. From the beginning of the pandemic to the end of Wave Three, there were an average of 3,423.32 (SD = 3800.90) cases per 100,000 in the Liberal states, 5297.40 (SD = 4073.46) cases per 100,000 in the Social Democratic states, and 7,299.59 (SD = 1863.30) cases per 100,000 in the Conservative states. There were no statistically significant differences by welfare state typology in the number of COVID-19 cases at Wave One (F(2, 20) = 0.02, p = 0.98) or Wave Two (F(2, 20) = 2.59, p = 0.10); however, at Wave Three, the Liberal states had on average 1,606 cases fewer than the Conservative nations (F(2, 20) = 4.04, p < 0.05). In terms of mortality, by the end of the Third Wave, there was an average of 70.05 (SD = 79.72) COVID-19 deaths per 100,000 in the Liberal states, 55.61 (SD = 56.16) deaths per 100,000 in the Social Democratic states, and 156.34 (SD = 41.29) deaths per 100,000 in the Conservative states. Again, the average number of deaths were not statistically different between the welfare regimes at Wave One (F(2, 20) = 0.83, p = 0.45), but at Wave Two and Three significant differences emerged (F(2, 20) = 8.54, p < 0.01 and F(2, 20) = 9.00, p < 0.01 respectively). At Wave Two, the Liberal states had on average 47.16 deaths fewer than the Conservative states while the Social Democratic states had on average 53.34 fewer deaths than Conservative states. At Wave Three, the Liberal states had on average 25.60 fewer deaths than the Conservative states and the Social Democratic states had on average 32.34 fewer deaths than Conservative states. There were no significant differences between the Liberal and Social Democratic states in the number of COVID-19 deaths per 100,000. Similarly, there were no differences by welfare regime in the number of excess dates during Wave One (F(2, 20) = 1.17, p = 0.33), but there were significant differences at Wave Two (F(2, 20) = 4.73, p < 0.05) and Wave Three (F(2, 20) = 5.70, p < 0.05). Liberal states had on average 86.93 and the Social Democratic states had 93.16 fewer excess deaths than the Conservative states at Wave Two and 98.16 and 113.42 fewer deaths, respectively, at Wave Three. Again, there were no significant differences in the number of excess deaths between the Liberal and the Social Democratic regimes.
The number of deaths per 100,000 and the number of cases per 100,000 were unrelated to many of the healthcare and income measures. Significant bivariate relationships are indicated in Tables 3, 4, and 5. There was a significant difference by type of welfare regime in the number of doctors per 10,000, with the Conservative states having on average more doctors than Liberal states (F(2, 20) = 9.33, p < 0.001). There was also a significant difference by welfare regime type and measures of income inequality: Gini index (F(2, 20) = 11.50, p < 0.001), iHDI (F(2, 20) = 5.63, p < 0.05), and income share held by poorest 20% of the population (F(2,20) = 10.45, p < 0.001). In all three cases, the Social Democratic countries score significantly better than the Conservative countries, while the differences between Liberal and Social Democratic countries were non-significant.
In terms of the policy variables, the type of welfare regime was significantly related to Wave One and Two mask policies and Wave One debt relief (see Table 4). There was no relationship between the type of welfare state and income support, the political ideologies of the ruling party, and the economic regulation of the ruling party at any point during the pandemic. This finding was contrary to our hypothesis that there would be significant differences in the approaches to labor decommodification based on the type of welfare state and dependent on the left-power mobilization within a state. We also tested whether the political ideologies of the ruling party were related to the type and level of income support, mask policies, trust in government, the economic regulation of the market, and testing and vaccination rates. Contrary to our expectations, which were based on Esping-Anderson’s conceptualization of leftwing mobilization, there was no relationship between the political ideology of the ruling party and either the labour decommodification variables or the testing/vaccination rates. The only significant relationship was between political ideology and the economic regulation approach of the ruling party; the more leftwing the ruling party, the greater state control of the economy (r = 0.88, p < 0.001). We also found a moderate relationship between trust in government and testing rates at Wave One and Wave Two (r = 0.33 and r = 0.34, respectively), but there was no relationship at Wave Three.
Significant correlations between the outcome variables and the continuous predictors are presented in Table 5. Only Wave One COVID-19 cases were significantly associated with any of the predictors. Higher numbers of tests per 1,000 and higher percentages of the population over the age of 65 were associated with higher cases per 100,000 at Wave One. Higher Wave One deaths were associated with more stringent restrictions at Wave Three, lower numbers of hospital beds, and higher percent of GDP spent on health. Lower numbers of Wave Three COVID-19 deaths were associated with more trust in the government, more nurses per 10,000, greater health coverage by the state, higher PPP, and higher iHDI. There were no significant correlates of excess deaths at Wave One, but higher numbers of Wave Two excess deaths and Wave Three excess deaths were associated with less stringent government restrictions at Wave Three, lower numbers of nurses per 10,000, less health coverage by the state, higher out of pocket health expenses, and lower iHDI and PPP.
Multivariate results
The repeated measures MANOVA results indicate there was a significant main effect of time/wave and the outcome variables: COVID-19 cases per 100,000 (F(1.5, 31) = 34.12, p < 0.001), COVID-19 deaths per 100,000 (F(2, 40) = 13.32, p < 0.001), and the number of excess deaths (F(1.3, 26.2) = 32.50, p < 0.001). Wave Two had significantly higher numbers of cases, deaths, and excess deaths compared to Waves One and Three. There were on average 2730 fewer cases per 100,000 during Wave One compared to Wave Two (p < 0.001), and 1535 fewer cases during Wave One compared to Wave Three (p < 0.001). There were also 1195 more cases during Wave Two compared to Wave Three (p < 0.01). There were on average 20 more deaths during Wave Two compared to Wave One (p < 0.001), and 21 more deaths during Wave Two compared to Wave Three (p < 0.001). There was no significant difference in the number of deaths between Waves One and Wave Three. There were an additional 48 excess deaths at Wave Two (p < 0.001) and an additional 53 excess deaths at Wave Three compared to Wave One (p < 0.001). There were no significant differences in excess deaths between Waves Two and Three.
The repeated measures MANOVA also indicated that the type of welfare regime had a significant main effect of the number of COVID-19 deaths per 100,000 (F(2, 20) = 6.44, p < 0.01) and the number of excess deaths per 100,000 (F(2, 20) = 4.31, p < 0.05), but not on the number of COVID-19 cases per 100,000 (F(2, 20) = 3.01, p = 0.07). Liberal states and the Social Democratic states had on average 28.8 (p < 0.05) and 33.6 (p < 0.05) fewer deaths, respectively, than the Conservative states. Liberal states and the Social Democratic states also had fewer excess deaths compared to the Conservative states, but these differences were only approaching significance (MD = 69.2, p = 0.07 and MD = 77.7, p = 0.06).
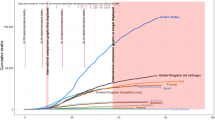
Lastly, there was a significant interaction between wave and the type of welfare regime in the number of deaths (F(4, 40) = 3.62, p < 0.05), and excess deaths (F(2.6, 26,2) = 8.58, p < 0.001), but not in the number of cases (F(3.1, 31) = 2.74, p = 0.058). A significant interaction indicates that the relationship between the outcome variables and the pandemic wave is dependent on the type of welfare state. A graphical representation of these interactions is presented in Fig. 1. As evidenced in the charts, Wave Two had a bigger impact on the number of deaths and excess deaths within the Conservative states compared to either the Liberal or the Social Democratic regimes.
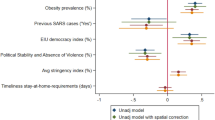
Once covariates were added to the model, the differences between Liberal and Social Democratic states in the number of cases and excess deaths at Waves Two and Three become more pronounced, while the differences between Social Democratic states and Corporatist states became non-significant when looking at the number of cases and excess deaths (see Fig. 2). Significant covariates of the relationships between welfare regime, wave, and the number of COVID-19 cases per 100,000 were the amount of GDP spent on health (F(1, 17) = 7.98, p < 0.05) and the stringency of restrictions at Wave Two (F(1, 17) = 6.18, p < 0.05). Significant covariates of the number of COVID-19 deaths per 100,000 were vaccination rate at Wave Three (F(1, 17) = 5.54, p < 0.05) and the stringency of restrictions at Wave Two (F(1, 17) = 9.27, p < 0.01). The only significant covariate of the number of excess deaths per 100,000 was the stringency of restrictions at Wave Two (F(1, 17) = 7.66, p < 0.05). No other health, economic, or policy predictors were significantly related to the three outcome variables. For all three outcome variables, the more stringent the restrictions during Wave Two, the fewer cases/deaths reported.
Discussion
The analyses indicate that overall, the examined welfare regimes are a lot more similar than expected. Very few significant differences exist in their health infrastructure (only the difference in number of doctors per 10,000 was significant between Liberal and Conservative/Corporatist states) or in their characteristics of the ruling party and their pandemic policy responses (Social Democratic states were the only ones not to issue mandatory mask policies and debt relief at the beginning of Wave One). Stringency of government restrictions, testing and vaccination rates were similar across the three welfare regimes. Meanwhile, the measures of economic inequality (Gini index, iHDI, and income share held by poorest 20%) continue to indicate that Liberal and Corporatist states have significantly more income inequality than Social Democracies. There were some interesting correlations between the predictors that might obscure some of the inter-regime differences in pandemic outcomes. For instance, testing was related to trust in government at Wave One, and generally, people in Social Democratic countries had more trust in their governments than people in Conservative countries, but this difference was only approaching significance. Similarly, the political leanings of the ruling party (left/right ideology, market/state approach to economic regulation, etc.) did not differ significantly by welfare regime and were not associated in bivariate analyses with public policy or economic policy responses at any point during the pandemic. The small number of countries analyzed could partially explain some of these non-significant findings, and future analyses could well expand the sample to include additional welfare states.
This paper started from the premise that Western democracies, those with strong welfare principles, established systems of welfare provision and robust investments in health care, would be better prepared to fight the COVID-19 pandemic. Our analysis started from the assumption that there will be differences between the Nordic states and continental Europe, as well as the Anglo-Saxon Liberal states on the number of COVID-19 infections and subsequent mortality rates during all three waves of the pandemic. The Nordic States have always served as distinct welfare archetypes, as their universal social programs, extensive state transfers and generous social policies have been improving population health, particularly through reducing mortality (Bambra 2011; Lundberg 2010; Lundberg et al. 2008). Social Democracies tend to subtract the commodifying value of goods and services weighed on the free market and to re-frame them, through redistributive welfare policies, as state benefits and services (Esping-Andersen 1990). After all, the distribution of health care is continually negotiated in societies, in exchange for cash in strong market economies (i.e., the US) or provided as a state benefit (i.e., Sweden).
The Scandinavian countries, however, despite their welfare investments within the field of public health, with strong, national health care systems, publicly owned hospitals, hence wider access to hospital beds and testing, and despite their lower income inequality rates, did not fare better than the Liberal nor the Corporatist/Conservative nations at decreasing COVID-19 deaths during First Wave. They did however, fare better, but only than the Conservative/ Corporatist states during Waves Two and Three of the pandemic.
A possible explanation for the similar higher COVID-19 rates in some of the heavily impacted states at Wave One could be connected to the outbreaks in long-term care facilities. A report published in the beginning of the pandemic, in May 2020, by the International Long-Term Care Policy Network, found that several countries, such as Canada for instance, registered the highest number of care home resident deaths (3566) as a proportion of all COVID-19 deaths (62 percent), followed by Ireland (60%) (Comas-Herrera et al. 2020). While Canada has a single-payer, universal healthcare system, long-term residential care is not covered under the national health-care plan but purchased on the private market (Armstrong and Armstrong 2016). And with privatization comes de-regulation. A recent analysis conducted by the Canadian Institute for Health Information (CIHI) found that the lack of governmental regulation in Canada was manifested in loose institutional policy responses in long-term care facilities, such as the lack of mandatory prevention measures and stay-at-home orders, as well as low monitoring compliance with immediate infection control measures, such as testing, staff training, and use of personal protective equipment (CIHI 2020). By contrast, countries with centralized regulation of long-term care homes, such as Australia, had lower numbers of COVID-19 cases and deaths (CIHI 2020). Australia had implemented isolation wards in care homes, conducted broad testing, implemented infection control training, conducted audits and provided rapid response control (CIHI 2020). While it appears that the differences in the management of long terms care homes played a large role in determining COVID-19 spread within the high-risk, older population it is important to note the overall underreporting of care home mortality in many countries. For instance, in the US, it is estimated that within the first three months of the pandemic, about 44.7% of COVID-19 cases and 40.0% of COVID-19 deaths were unaccounted for, until May 24, when the federal guidelines started to require facilities to report such cases to the National Healthcare Safety Network (Shen et al. 2021). In the UK, it is estimated that the number of people who died in care homes was above the expected mortality level by 134% at the end of the First Wave in the pandemic (O’Donnell et al. 2021). However, the underreporting of COVID-19 rates in care homes decreased by the Second and Third Waves. For instance, the number of people in England, Wales, Scotland and Northern Ireland that died in care homes only increased above expected levels by 10% in the Second Wave and later dropped to 3% by the Third Wave (O’Donnell et al. 2021). It is difficult to include a universal, valid measure that counts nursing home deaths due to national variations in reporting and across different points in time, yet as the care homes underreporting was only higher during the First Wave of the pandemic compared to the Second and Third waves, such underreporting only constitutes a minor limitation of the data.
Moreover, despite accounts of underreporting and cross-national differences in recording COVID-19 cases and deaths, Western democracies have been leading in reporting when compared to other states on a global scale. It is the countries in sub-Saharan Africa and several nations within Central and Eastern Europe as well as some of the former Soviet Republics, such as Belarus, Azerbaijan and Kazakhstan, that have recorded the highest differences between excess deaths and COVID-19 mortality (Dyer 2021; Karlinksy and Kobak 2021; Rangachev et al. 2021). The inclusion of the excess deaths variable as an outcome variable minimizes this limitation as it accounts for possible variations in underreporting.
Our analysis shows that different stories unfold within the Second and Third Waves in the pandemic compared to the First. Data indicates that welfare style state measures, such as more trust in government, more nurses per 10,000 and greater health coverage were associated with lower COVID-19 deaths at Wave Three. Yet despite the expected differences between welfare regimes in the number of COVID-19 cases and deaths, namely that Social Democracies would have the social and economic infrastructure to bear the pandemic outcomes with the least impacts, it was actually the Liberal states that performed better as a welfare group in the number of cases once the covariates were taken into account. Both Liberal and Social Democratic states had significantly lower deaths and excess deaths at Waves Two and Three than the Conservative states. These differences also cannot be attributed to differences in testing rates, because as shown in Table 3, there were no significant differences between the three regimes in the number of tests per capita performed at any point during the pandemic.
Cumulative data from all three waves shows the Corporatist states to have had the highest numbers of COVID-19 infections, mortality, and excess mortality rates out of all three welfare regimes even though the Conservative states had, on average, more doctors than the Liberal nations. The question, however, is not so much about why the Conservative/Corporatist states fared the worst. These democracies are heavily based on social insurance principles and generally only provide benefits on actuarial principles, hence they tend to restrict welfare eligibility on former contributions, forcing many to venture into the labour market and to risk infection exposures. The question is why the Liberal states fared better than the Corporatist states on all outcomes and on par with their Social Democratic counterparts. The authors’ initial assumption was that the Liberal states, whose distributive policies are based on means-tested benefits will leave many already living on the margins unprotected, hence the expectation was for these states to reach some of the highest infection and mortality rates. It was assumed that the Social Democratic regimes will show the lowest epidemiological spread of COVID-19 particularly though the provision of high pandemic benefit levels, according to need and irrespective of former participation in the labour market, as well as the provision of strong healthcare access and distribution. Theoretically speaking, the Nordic countries should have been at the top in terms of their performance vis-à-vis the COVID-19 numbers and excess mortality; the Corporatist/Conservative states somewhere in the middle; and the Liberal states last, considering the historical low-level of decommodification of these nations (Esping-Anderson 1990).
There are two possible explanations for the lack of differences between the Social Democratic and the Liberal States.
On the one hand, the low performance of the Social Democratic welfare regimes could be attributed to the rise in global neoliberalism which untied, after 1980s, a period of limited health care investment in many countries. In other words, neoliberalism could have flattened the previous differences between the welfare regimes and could have brought welfare state clusters closer to each other, ideologically speaking, in terms of welfare provision: the welfare of the market nowadays universally prevails over people’s welfare. This is evident in the lack of significant differences in the political ideologies of the ruling party and the economic regulation of the ruling party at any point during the pandemic across the three welfare types. In welfare regime theory, left-wing electoral party politics tend to shape various political outcomes in society; however, in this case, left-power mobilization, as measured by the left-wing ideological orientation of the ruling parties, was irrelevant in relation to the provision of income supports, but also irrelevant as a proxy for the reported COVID-19 rates and excess mortality numbers.
The flattening of the left–right electoral ideology is particularly important. Regardless of the strong positive correlation of leftist politics with the economic regulation of the ruling party variable (meaning the more leftist oriented ideological leaning of the ruling party the more state control), there was no difference in relation to how states with leftist orientated electoral parties have provided income support. This lack of an ideological boundary between the ‘left’ and ‘right’ indicates a fusion between the state and the market and implies a ‘left-power’ mobilization devoid of actual power; partially resulting from cross-ideological government coalitions wherein the ruling party’s political ideology gets pulled towards the center. In other words, leftist politics seem to have little capacity to mobilize state decommodification efforts in welfare provision. Benefits no longer serve the purpose of de-commodifying individuals from the labour market, the raison d’être of a welfare regime. For instance, the income support for workers unable to work due to COVID-19 lockdowns is a welfare measure that intends to emancipate workers from market dependency and to protect them from getting infected, hence a measure of help from the state geared towards its citizens. By contrast, wage subsidies for businesses or employers that had COVID-19 revenue losses is a measure that primarily supports the market and does little to reduce workers’ dependency on the labor market nor to increase their socio-economic security. Examining if the pandemic supports benefited more the market than its workers and citizens goes beyond the scope of this paper. Further research is needed to assess how welfare states have stratified COVID-19 infection and mortality rates numbers by examining pandemic-related benefit levels on ideological principles (as a matter of rights or on actuarial basis), on accessibility (universality versus selectivity), or on the strength of the benefit (i.e., the number of waiting days before benefits are paid or the maximum duration of a benefit).
Future research propositions, however, do not take away that, within the last decades, government cutbacks, decreased public spending, deregulation, diminished barriers to trade and the implementation of an ideology centered on the values of limited state intervention and unrestrained freedom of the market, have all globally residualized welfare provision on deserving/underserving criteria all over the world (Graham et al. 2012). In turn, former ideas of the state envisioning itself as responsible for citizens’ assistance, shifted towards principles of individual responsibility, productivity and economic self-sufficiency, which resulted in increased inequality within western countries (Hunter 2010; Lightman and Lightman 2017). While this analysis included indicators of inequality (i.e., Gini index, poverty gap, equality adjusted HDI, universal healthcare coverage), none of them were associated with COVID-19 cases or deaths in the cross-country multivariate analyses. The small number of countries in the sample underpowered the analyses and it is possible that a larger sample might yield different results. Yet this lack of variation could also show that welfare regimes are much more similar nowadays in terms of their unequal stratification mechanisms and irrespective of their welfare outlook.
On the other hand, the high performance of the Liberal states could be attributable to this cluster of regimes coming closer, ideologically speaking, to Social Democracy. In other words, one could argue that the pandemic has served as a catalyst for the provision of welfare through income supports, lockdown benefits, wage supports and other emergency benefits in the case of the Liberal welfare regimes. This is evidenced by the lack of differences between the three regimes in the income support levels and benefit levels offered at each wave of the pandemic (see Table 4), except Wave One when, in an unusual manner, the Social Democratic states were slower to implement income support and debt relief benefits compared to the Liberal states.
If such COVID-19 benefits are to be provided as a matter of rights rather than on actuarial principles, on universal rather than on selective basis, with no restrictive conditions on eligibility, these will all lead to decommodification, a staple feature of social democratism. Yet, the social-democratization explanation for the Liberal regimes gets further complicated when looking back again at the ideological leaning of the ruling party variable. Esping-Anderson (1990) has for long argued that left power mobilization is a precondition for social democratization, particularly in relation to the liberal welfare regimes. In Three Worlds of Welfare Capitalism, Esping-Anderson (1990) showed that if within Corporatist regimes, left-wing parties have been unable to alter the inherent etatism from the strong catholic parties and absolutist heritage, in the Liberal regimes, the left-wing parties have had very strong effects. Left-power mobilization lessens the Liberal welfare states’ attributes, meaning is it more effective in eradicating means-tested, liberal stratification effects. In other words, the influence of left-wing power politics in a state is generally associated with a higher provision of welfare. Left political power tends to marginalize the residual poor relief that is so common in the Liberal states and tends to have a very strong effect on decommodification. However, in adding the ideological leaning of the ruling party (left wing versus right wing) and the personal freedom ideology of the ruling party (libertarian versus authoritarian) as covariates, no differences were observed between the welfare states. It appears that the three types of welfare regimes are becoming more and more similar in terms of their ideological outlook and subsequent welfare approaches than ever before. Despite the limitations of our tests, which are underpowered due to the small number of countries, the averages are closer together than one would ever expect.
Is it a matter of an ideological erasure of left-wing/right-wing politics that flattened the differences between the Social Democratic and the Liberal states? Or a matter of a social-democratization of liberal residualism? Are we bearing witness to a mainstreaming of social democracy? A mainstreaming of global liberalism? Whereas all parliamentary parties, from center-right to center-left preserve the market’s dominance? Or are we bearing witness to a softening of the liberal principles towards social protectionism? Time will only tell.
References
Asatiani, M., and T. Verulava. 2017. Georgian welfare state: Preliminary study based on Esping-Andersen’s typology. Economics and Sociology 10 (4): 21–28.
Bejan, R. 2019. The collapse of social welfarism is lethal. rabble.ca. December 2: https://dalspace.library.dal.ca/handle/10222/79000.
Bejan, R., Allain, KA., Glynn, T. 2021. COVID-19 has exacerbated migrant workers’ conditions and enforced distinctions on national lines. COMPAS, University of Oxford, UK. July 2: https://dalspace.library.dal.ca/handle/10222/80574.
Bejan, R., and Nikolova, K. 2021. How Canada compares to welfare states in COVID-19 cases and deaths. The Conversation. October 5: https://dalspace.library.dal.ca/handle/10222/80919.
Bejan, R., Allain, K.A., Glynn, T., Wheatley, A. & Soto Flores, P. 2021. Safe at Work, Unsafe at Home COVID-19 and Temporary Foreign Workers in Prince Edward Island. TFW Maritimes. Halifax, NS: https://dalspace.library.dal.ca/handle/10222/80526.
Bejan, R. 2021a. The progressive case against mandatory vaccination. rabble.ca. August 17: https://dalspace.library.dal.ca/handle/10222/80918.
Bambra, C. 2011. Health inequalities and welfare state regimes: Theoretical insights on a public health ‘puzzle.’ Journal of Epidemiology and Community Health 65 (9): 740–745.
Bambra, C. 2007. Going beyond ‘The three worlds of welfare capitalism’: Regime theory and public health research. Journal of Epidemiology and Community Health 61 (12): 1098–1102.
Bambra, C. 2005a. Cash versus services: ‘worlds of welfare’ and the decommodification of cash benefits and health care services. Journal of Social Policy 34 (2): 195–213.
Bambra, C. 2005b. Worlds of welfare and the health care discrepancy. Social Policy and Society 4 (1): 31–41.
Bryson Taylor, D. 2021. A Timeline of the Coronavirus Pandemic, March 17 https://www.nytimes.com/article/coronavirus-timeline.html.
Burn-Murdoch, J., and C. Giles. 2020. UK suffers second-highest death rate from coronavirus. Financial Times, 28 May: https://www.ft.com/content/6b4c784e-c259-4ca4-9a82-648ffde71bf0.
Castles, F.G., S. Leibfried, J. Lewis, H. Obinger, and C. Pierson, eds. 2012. The Oxford Handbook of the Welfare State. Oxford: Oxford University Press.
Canadian Institute for Health Information. 2020. Pandemic Experience in the Long-Term Care Sector: How Does Canada Compare With Other Countries. Ottawa, ON: CIHI.
Chaskin, R.J., B. Lee, and S. Jaswal. 2019. Social exclusion in cross national perspective: Actors, actions, and impacts from above and below. New York, NY: Oxford University Press.
Chung, H., and C. Muntaner. 2006. Political and welfare state determinants of infant and child health indicators: An analysis of wealthy countries. Social Science and Medicine 63 (3): 829–842.
Craig, S.L., Bejan, R. and Muskat, B., 2013. Making the invisible visible: Are health social workers addressing the social determinants of health?. Social Work in Health Care 52(4): 311–331.
Comas-Herrera A., J. Zalakaín, C. Litwin, A.T. Hsu, N. Lane, and J.-L. Fernández. 2020. Mortality associated with COVID19 outbreaks in care homes: Early international evidence. International Long-Term Care Policy Network, CPEC-LSE, 3 May: https://ltccovid.org/wp-content/uploads/2020/05/Mortality-associated-with-COVID-3-May-final-5.pdf.
Dyer, O. 2021. Covid-19: Study claims real global deaths are twice official figures. British Medical Journal 373: 4–86.
Ekathimerini News. 2020. Greeks sent 110 million texts to leave house during lockdown. Ekathimerini News, 29 May: https://www.ekathimerini.com/252308/article/ekathimerini/news/greeks-sent-110-million-texts-to-leave-house-during-lockdown.
Esping-Andersen, G. 1990. The three worlds of welfare capitalism. Princeton: Princeton University Press.
Evans, M. 2020. Germany, a global leader on COVID-19 response, cautiously comes out of lockdown. CBC News, 30 May: https://www.cbc.ca/news/world/germany-coronavirus-covid-lockdown-merkel-1.5590731.
Ferrera, M. 1996. The ‘Southern model’ of welfare in social Europe. Journal of European Social Policy 6 (1): 17–37.
Freeman, R., and H. Rothgan. 2012. Health. In The Oxford handbook of the welfare state: Oxford, UK. Oxford University Press.
Government of Canada. 2021. Procuring vaccines for COVID-19. https://www.canada.ca/en/public-services-procurement/services/procuring-vaccines-covid19.html.
Graham, J., K. Swift, and R. Delaney. 2012. Canadian social policy: An introduction. North York: Pearson Education Canada.
Hunter, G. 2010. Child poverty and the Canadian welfare state. In Canadian Social Policy: Issues and Perspectives, ed. Anne Westhues. Waterloo, ON: Wilfried Laurier Press.
Jackson, H. 2020. Sweden took a softer COVID-19 approach. Has it been effective? Global News, 4 May: https://globalnews.ca/news/6901068/coronavirus-sweden-approach/.
Kaplan, G.A. 2007. Health inequalities and the welfare state: Perspectives from social epidemiology. Norsk Epidemiologi 17 (1): 9–20.
Karlinsky, A., and D. Kobak. 2021. Tracking excess mortality across countries during the COVID-19 pandemic with the World Mortality Dataset. eLife 10: 69336.
Kim, H. 2020. World watches as South Korea cautiously returns to life. CTV News, 27 May: https://www.ctvnews.ca/world/world-watches-as-south-korea-cautiously-returns-to-life-1.4956307.
Kuhnle, S., and A. Sander. 2010. The emergence of the western welfare state. In The Oxford handbook of the welfare state. Oxford, UK: Oxford University Press
Labropoulou, E. 2020. Greece has been a coronavirus success, but it will be hit economically anyway. The Washington Post, 22 April: https://www.washingtonpost.com/world/europe/greece-coronavirus-success/2020/04/22/47e018ee-7f38-11ea-84c2-0792d8591911_story.html.
Leibfried, S. 1993. Towards a European welfare state. New Perspectives on the Welfare State in Europe 133: 15.
Lightman, E.S., and N. Lightman. 2017. Social policy in Canada. Don Mills, ON: Oxford University Press.
Lundberg, O. 2010. Politics and public health—some conceptual considerations concerning welfare state characteristics and public health outcomes. International Journal of Epidemiology 39 (2): 632–634.
Lundberg, O., Yngwe, M. Å., Stjärne, M. K., Elstad, J. I., Ferrarini, T., Kangas, O., … and News Nordic Group. 2008. in social policy programmes for public health: An international comparative study. Lancet 372: 1633–1640.
Mayberry K., G. Mersiha, and J. Stepansky. 2020. Italy reports 602 new coronavirus deaths: Live updates. Al Jazeera, 23 March: https://www.aljazeera.com/news/2020/03/italy-bans-internal-travel-stop-virus-spread-live-updates-200322235532945.html.
Navarro, V., and L. Shi. 2001. The political context of social inequalities and health. International Journal of Health Services 31: 1–21.
OECD. 2020a. Health LTC. https://stats.oecd.org/Index.aspx?DataSetCode=HEALTH_LTCR.
OECD. 2020b. Healthcare Resources. https://data.oecd.org/healthres/doctors.htm#indicator-chart.
OECD. 2020c. Poverty rate (indicator). https://data.oecd.org/inequality/poverty-rate.htm.
OECD. 2018. Hospital beds (indicator). https://data.oecd.org/healtheqt/hospital-beds.htm.
O’Donnell, S.B., A.E. Bone, A.M. Finucane, J. McAleese, I.J. Higginson, S. Barclay, K.E. Sleemna, and F.E. Murtagh. 2021. Changes in mortality patterns and place of death during the COVID-19 pandemic: A descriptive analysis of mortality data across four nations. Palliative Medicine 35 (10): 1975–1984.
Olafsdottir, S. 2007. Fundamental causes of health disparities: Stratification, the welfare state, and health in the United States and Iceland. Journal of Health and Social Behavior 48 (3): 239–253.
Our World in Data. 2018. Trust, https://ourworldindata.org/trust Accessed 14 December 2021
Our World in Data. 2021a. Estimated cumulative excess deaths per 100,000 people during COVID-19, (https://ourworldindata.org/grapher/excess-deaths-cumulative-per-100k-economist?time=2020-06-29&country=PAN~TGO~SWZ~GBR~MNG~MAC~COM~LBN Accessed 14 December 2021a
Our World in Data. 2021a. COVID 19 Stringency Index, https://ourworldindata.org/grapher/covid-stringency-index?country=IRN~TWN~PRY Accessed 14 December 2021b
Our World in Data. 2021b. Face covering policies during the COVID-19 pandemic, https://ourworldindata.org/grapher/face-covering-policies-covid Accessed 14 December 2021c
Our World in Data. 2021c. Debt or contract relief during the COVID-19 pandemic, https://ourworldindata.org/grapher/debt-relief-covid?time=2021d-02-28 Accessed 15 December 2021d
Our World in Data. 2021d. Income support during the COVID-19 pandemic, https://ourworldindata.org/grapher/income-support-covid?time=2020-05-03 Accessed 15 December 2021e
Our World in Data. 2021e. Share of the population fully vaccinated against COVID 19, https://ourworldindata.org/grapher/share-people-fully-vaccinated-covid?tab=map&country=LSO~LCA~TTO~TUR~Northern+Ireland~Africa Accessed 18 December 2021f
Powell, M., E. Yoruk, and A. Bargu. 2019. Thirty years of the three worlds of welfare capitalism: A review of reviews. Social Policy and Administration 54: 60–87.
Raikes, L., Giovannini, A. and Getzel, B. (2019) Divided and Connected: Regional Inequalities in the North, the UK and the Developed World – State of the North. 2019. London. UK: Institute for Public Policy Research.
Rangachev, A., Marinov, G. K., and Mladenov, M. 2021. The demographic and geographic impact of the COVID pandemic in Bulgaria and Eastern Europe in 2020. medRxiv.
Reisinger, D. 2020. Germany has remarkably few COVID-19 deaths. Its healthcare system shows how Germany prevented a runaway death toll. Business Insider, 2 April: https://www.businessinsider.com/why-germany-has-a-low-covid-19-mortality-rate-2020-4.
Romeo, N. 2020. The grim ethical dilemma of rationing medical care, explained. Vox, 31 March: https://www.vox.com/coronavirus-covid19/2020/3/31/21199721/coronavirus-covid-19-hospitals-triage-rationing-italy-new-york.
Scruggs, L., and J. Allan. 2006. Welfare-state decommodification in 18 OECD countries: A replication and revision. Journal of European Social Policy 16 (1): 55–72.
Shen, K., L. Loomer, H. Abrams, D.C. Grabowski, and A. Gandhi. 2021. Estimates of COVID-19 cases and deaths among nursing home residents not reported in federal data. JAMA Network Open 4 (9): 1–11.
Siddique, H. 2020. Coronavirus deaths in UK hospitals surpass 10,000. The Guardian, 12 April: https://www.theguardian.com/world/2020/apr/12/coronavirus-deaths-in-uk-hospitals-surpass-10000.
Van Voorhis, R.A. 2002. Different types of welfare states-A methodological deconstruction of comparative research. Journal of Sociology and Social Welfare 29 (4): 3–18.
West, A., Czypionka, T., Steffen, M., Ettelt, S., Ghislandi, S., & Mateus, C. 2020. Reporting COVID-19 deaths in Austria, France, Germany, Italy, Portugal and the UK. Department of Social Policy, London School of Economics and Political Science.
Wiley, M. 2020. Greece is banning non-residents from flocking to their second homes on local islands in a desperate bid to prevent the spread of the coronavirus. Business Insider, 24 May: https://www.businessinsider.com/greece-bans-leisure-travel-to-islands-during-coronavirus-lockdown-2020-3.
Wong, S., K. Kwok, and F. Chan. 2020. What can countries learn from Hong Kong’s response to the COVID-19 pandemic? CMAJ 192 (19): E511–E515.
World Health Organization. 2022. WHO Coronavirus Disease (COVID-19) Dashboard. https://covid19.who.int/.
WHO. 2020a. UHC Index of service coverage. https://www.who.int/data/gho/data/indicators/indicator-details/GHO/uhc-index-of-service-coverage Accessed: 26 December 2020a.
WHO. 2020b. Nursing and midwifery personnel (per 10,000 population). https://www.who.int/data/gho/data/indicators/indicator-details/GHO/nursing-and-midwifery-personnel-(per-10-000-population) Accessed: 26 December 2020b.
WHO. 2020c. Medical doctors (per 10,000 population). https://www.who.int/data/gho/data/indicators/indicator-details/GHO/medical-doctors-(per-10-000-population) Accessed: 26 December 2020c.
WHO. 2020d. Hospital beds (per 10,000 population). https://www.who.int/data/gho/data/indicators/indicator-details/GHO/hospital-beds-(per-10-000-population) Accessed: 26 December 2020d.
WHO. 2020e. Current health expenditure (CHE) as percentage of gross domestic product (GDP, %). https://www.who.int/data/gho/data/indicators/indicator-details/GHO/current-health-expenditure-(che)-as-percentage-of-gross-domestic-product-(gdp)-(-) Accessed: 26 December 2020e.
WHO. 2020f. Out-of-pocket expenditure as a percentage of total expenditure on health. https://www.who.int/data/gho/data/indicators/indicator-details/GHO/out-of-pocket-expenditure-on-health-as-percentage-of-total-health-expenditure Accessed: 26 December 2020f.
World Bank. 2020a. Proportion of population spending more than 10% of household consumption or income on out-of-pocket health care expenditure (%). https://data.worldbank.org/indicator/SH.UHC.OOPC.10.ZS Accessed: 26 December 2020a.
World Bank. 2020b. Gini Index (World Bank estimate). https://data.worldbank.org/indicator/SI.POV.GINI Accessed: 26 December 2020b.
World Bank. 2020c. Income share held by lowest 20%. https://data.worldbank.org/indicator/SI.DST.FRST.20 Accessed: 26 December 2020c.
World Bank. 2020d. GDP, PPP (current international $). https://data.worldbank.org/indicator/NY.GDP.MKTP.PP.CD Accessed: 26 December 2020d.
World Bank. 2020e. Proportion of population over 65. https://data.worldbank.org/indicator/SP.POP.65UP.TO.ZS Accessed: 26 December 2020e.
Funding
This study was unfunded.
Author information
Authors and Affiliations
Contributions
RB and KN contributed to the study conception and design. RB contributed to the introduction, discussion and conclusion. KN contributed to the methods and results.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest or competing interests to disclose.
Ethical approval
This article does not contain any studies with human participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bejan, R., Nikolova, K. COVID-19 amongst western democracies: A welfare state analysis. Soc Theory Health 20, 123–151 (2022). https://doi.org/10.1057/s41285-022-00178-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1057/s41285-022-00178-4