Abstract
High-fidelity simulation-based training, such as those aimed at teaching the management of medical crises, constitutes a highly complex learning task. To be effective, its design must be guided by sound learning principles. Cognitive load theory is a well-developed framework and has been extensively used in other settings to improve instructional designs in medical education. We explain this theoretical framework and its relevance to the educational design of high-fidelity simulation using as an exemplar the McGill University internal medicine crisis resource management learning activity. We then conclude with a few practical suggestions on how to apply cognitive load theory in the design of high-fidelity simulation-based learning activities.

Similar content being viewed by others
References
Alessi SM (2000). Simulation design for training and assessment. Aircrew training and assessment, pp 197–222.
Allen J, Buffardi L, and Hays R (1991). The Relationship of Simulator Fidelity to Task and Performance Variables. DTIC Document.
Bradley P (2006). The history of simulation in medical education and possible future directions. Medical education 40(3): 254–262.
Gaba DM, Howard SK, Fish KJ, Smith BE and Sowb YA (2001). Simulation-based training in anesthesia crisis resource management (ACRM): A decade of experience. Simulation & Gaming 32(2): 175–193.
Gaba DM, Howard SK, Flanagan B, Smith BE, Fish KJ and Botney R (1998). Assessment of clinical performance during simulated crises using both technical and behavioral ratings. Anesthesiology 89(1): 8.
Grunwald T and Corsbie-Massay C (2006). Guidelines for cognitively efficient multimedia learning tools: educational strategies, cognitive load, and interface design. Academic Medicine 81(3): 213–223.
Haji FA, Rojas D, Childs R, Ribaupierre S and Dubrowski A (2015). Measuring cognitive load: performance, mental effort and simulation task complexity. Medical Education 49(8): 815–827.
Harrison TK, Manser T, Howard SK and Gaba DM (2006). Use of cognitive aids in a simulated anesthetic crisis. Anesthesia & Analgesia 103(3): 551–556.
Hayes CW, Rhee A, Detsky ME, Leblanc VR and Wax RS (2007). Residents feel unprepared and unsupervised as leaders of cardiac arrest teams in teaching hospitals: A survey of internal medicine residents*. Critical Care Medicine 35(7): 1668–1672.
Kim J, Neilipovitz D, Cardinal P and Chiu M (2009). A comparison of global rating scale and checklist scores in the validation of an evaluation tool to assess performance in the resuscitation of critically ill patients during simulated emergencies (abbreviated as” CRM simulator study IB”). Simulation in Healthcare 4(1): 6.
Kim J, Neilipovitz D, Cardinal P, Chiu M and Clinch J (2006). A pilot study using high-fidelity simulation to formally evaluate performance in the resuscitation of critically ill patients: The University of Ottawa Critical Care Medicine, High-Fidelity Simulation, and Crisis Resource Management I Study. Critical Care Medicine 34(8): 2167–2174.
Kirschner PA (2002). Cognitive load theory: Implications of cognitive load theory on the design of learning. Learning and Instruction 12(1): 1–10.
Lane NE and Alluisi EA (1992). Fidelity and Validity in Distributed Interactive Simulation: Questions and Answers. DTIC Document.
Naismith LM, Cheung JJ, Ringsted C and Cavalcanti RB (2015). Limitations of subjective cognitive load measures in simulation-based procedural training. Medical Education 49(8): 805–814.
Nishisaki A, Keren R and Nadkarni V (2007). Does simulation improve patient safety?: Self-efficacy, competence, operational performance, and patient safety. Anesthesiology Clinics 25(2): 225–236.
Riem N, Boet S, Bould M, Tavares W and Naik V (2012). Do technical skills correlate with non-technical skills in crisis resource management: a simulation study. British Journal of Anaesthesia.
Sweller J (2010). Element interactivity and intrinsic, extraneous, and germane cognitive load. Educational Psychology Review 22(2): 123–138.
Sweller JJJ, Van Merrienboer G and Paas FGWC (1998). Cognitive architecture and instructional design. Educational Psychology Review 10(3): 251–296.
Van Merriënboer JJ, Kirschner PA and Kester L (2003). Taking the load off a learner’s mind: Instructional design for complex learning. Educational Psychologist 38(1): 5–13.
Van Merriënboer JJG and Sweller J (2005). Cognitive load theory and complex learning: Recent developments and future directions. Educational Psychology Review 17(2): 147–177.
Van Merriënboer JJG and Sweller J (2010). Cognitive load theory in health professional education: design principles and strategies. Medical Education 44(1): 85–93.
Young JQ, Van Merrienboer J, Durning S and Ten Cate O (2014). Cognitive Load Theory: Implications for medical education: AMEE Guide No. 86. Medical Teacher 36(5): 371–384.
Financial disclosure
The authors report no conflict of interest, financial or otherwise.
Authors contribution
Simulation has been increasingly used in health professions education and is rapidly gaining traction as the preferred instructional methods for team training for high-stake situations such as response to medical emergencies. High-fidelity simulation allows training to occur in authentic context without harm to patients. However, the complexity of such authentic learning activity can be overwhelming for learners if it is not designed based on sound adult learning principles. Cognitive load theory is a well-known framework that has commonly be used to guide instructional designs in order to maximize learning. Though it can also be used to optimize learning outcome in simulation-based activities, example of its formal application to this setting is lacking in the literature. Our article explains the key principles of cognitive load theory, walks the readers through an exemplar application to these in real life, and then concludes with a brief list of practical suggestions on how to optimize simulation-based learning using this theoretical framework. Even though the exemplar we describe is one of health professions education, the principles of cognitive load theory can be applied to simulation-based learning in any discipline and setting.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
1.1 Description of the pulmonary embolism scenario
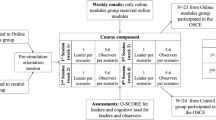
Four first to third year internal medicine residents are selected to form the team who will manage this medical emergency. Three more residents will be observing the case from outside the room through a one-way mirror. Two faculty debriefers will also be observing from outside the room. The case facilitator will be in the room when the scenario begins and will also role play the obstetrical nurse.
A sign is placed at the entrance to the simulation room with the following information: ‘You are the internal medicine residents on the Rapid Response Team in a community hospital. You are called to see a 32 year-old pregnant lady on the pre-partum unit.’ A high-fidelity mannequin (either Laerdal or METI) is used to simulate a 32 year-old female who is 29-week pregnant and critically ill from a massive pulmonary embolism (i.e. large blood clot in the pulmonary blood vessels obstructing blood flow). The simulation room is set up to mirror a typical obstetrical patient room and the resident team has access to the standard hospital equipment including the necessary equipment and medication for monitoring and stabilization of a critically ill patient. To better simulate real life practice, the resident team are also allowed to contact consultants in subspecialties (e.g. anesthesia) by phone. Standardized responses to these are designed to provide just-in-time procedural information (e.g. drug dosage).
As the resident team enter the room and engage in conversation with the obstetrical nurse, they learn that this patient was admitted 1 week ago for management of hypertension of pregnancy, and that they were called in because she was found by the nurse to have very low blood pressure. More information about the patient’s medical history, current symptoms and recent clinical progression are provided by the obstetrical nurse (i.e. the facilitator) and the patient (i.e. the simulation controller via speaker on the mannequin).
As soon as the residents attach the right monitoring device to the patient, vital signs appear on a screen next to the patient. All vital signs were pre-programmed to change in response to interventions by residents on a background of steady deterioration reflective of the natural progression of the disease process should there be no intervention.
The resident team have to seek and interpret information (e.g. blood test results, electrocardiogram tracings, chest X-ray film…) to arrive at the correct diagnosis of pulmonary embolism while working on stabilize the patient (e.g. giving intravenous fluid to increase blood pressure, intubating to protect airway as patient’s level of consciousness declines…). In addition to these technical skills, the team also has to demonstrate the crisis resource management (CRM) skills of leadership, problem solving, situational awareness, resource utilization and communication. An additional level of difficulty can achieved by introducing a standardized distractor whereby the obstetrical nurse draws the residents’ attention to deteriorations in fetal heart rate tracing and insists with increasing alarm on the need for urgent caesarian section.
Rights and permissions
About this article
Cite this article
Sun, N.Z., Anand, P.A. & Snell, L. Optimizing the design of high-fidelity simulation-based training activities using cognitive load theory – lessons learned from a real-life experience. J Simulation 11, 151–158 (2017). https://doi.org/10.1057/s41273-016-0001-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1057/s41273-016-0001-5