Abstract
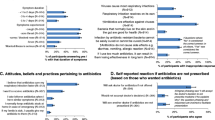
Children with upper respiratory tract infections (URTIs) are among the highest receivers of antibiotics. Using a retrospective cross-sectional study, we described clinical management in rural China of recent URTIs in children. We explored antibiotics using behaviors and associations of caregivers’ variables and children’s symptoms. Children with URTIs had a high consultation rate and a high prescription rate of antibiotics. For the children, some caregivers adopted, without rationale, ‘self-medication’ with antibiotics. Children with fever were more likely to be taken to a doctor; among those, children with particular symptoms were more likely to receive a prescription for antibiotics. Disseminating knowledge on antibiotics, and on interpretation and management of URTI symptoms will be important targets for caregiver and physician education and should become routine in training for physicians. Our findings also suggest the need to improve communication between doctors and caregivers, to strengthen regulation of drug sales, and to help caregivers learn when over-the-counter drug purchase without medical consultation is reasonable. These activities can help to improve health of a vast population of children in rural China.




Similar content being viewed by others
References
Bauman KA. The family physician’s reasonable approach to upper respiratory tract infection care for this century. Arch Fam Med. 2000;9(7):596–7.
Fleming DM, Smith GE, Charlton JR, Charlton J, Nicoll A. Impact of infections on primary care—greater than expected. Commun Dis Public Health. 2002;5(1):7–12.
Hak E, Rovers MM, Kuyvenhoven MM, Schellevis FG, Verheij TJ. Incidence of GP-diagnosed respiratory tract infections according to age, gender and high-risk co-morbidity: the Second Dutch National Survey of General Practice. Fam Pract. 2006;23(3):291–4.
Arroll B. Antibiotics for upper respiratory tract infections: an overview of Cochrane reviews. Respir Med. 2005;99(3):255–61.
Spinks A, Glasziou PP, Mar CBD. Antibiotics for sore throat. New York: Wiley; 2013.
Lee GM, Friedman JF, Ross-Degnan D, Hibberd PL, Goldmann DA. Misconceptions about colds and predictors of health service utilization. Pediatrics. 2003;111(2):231–6.
Nash DR, Harman J, Wald ER, Kelleher KJ. Antibiotic prescribing by primary care physicians for children with upper respiratory tract infections. Arch Pediatr Adolesc Med. 2002;156(11):1114.
Nasrin D, Collignon PJ, Roberts L, Wilson EJ, Pilotto LS, Douglas RM. Effect of βlactam antibiotic use in children on pneumococcal resistance to penicillin: prospective cohort study. BMJ Clin Res. 2002;324(7328):28–30.
Mcnulty CAM, Johnson AP. The European antibiotic awareness day. J Antimicrob Chemother. 2008;62(5):853–4.
Costelloe C, Metcalfe C, Lovering A, Mant D, Hay AD. Effect of antibiotic prescribing in primary care on antimicrobial resistance in individual patients: systematic review and meta-analysis. BMJ. 2010;340(10):688.
China NHaFPCotPsRo. The stewardship strategies for the clinical antimicrobial use. 2012. http://www.nhfpc.gov.cn/fzs/s3576/201205/2f773c2ddbd84e19aab0b4b2d9741900.shtml. Accessed 29 March 2018.
Li J, Song X, Yang T, Chen Y, Gong Y, Yin X, et al. A systematic review of antibiotic prescription associated with upper respiratory tract infections in China. Medicine (Baltimore). 2016;95(19):e3587.
Zhang Z, Hu Y, Zou G, Lin M, Zeng J, Deng S, et al. Antibiotic prescribing for upper respiratory infections among children in rural China: a cross-sectional study of outpatient prescriptions. Glob Health Action. 2017;10(1):1287334.
Yang L, Liu C, Wang L, Yin X, Zhang X. Public reporting improves antibiotic prescribing for upper respiratory tract infections in primary care: a matched-pair cluster-randomized trial in China. Health Res Policy Syst. 2014;12:61.
Mangionesmith R, Mcglynn EA, Elliott MN, Mcdonald L, Franz CE, Kravitz RL. Parent expectations for antibiotics, physician-parent communication, and satisfaction. Arch Pediatr Adolesc Med. 2001;155(7):800.
Friedman JF, Lee GM, Kleinman KP, Finkelstein JA. Acute care and antibiotic seeking for upper respiratory tract infections for children in day care: parental knowledge and day care center policies. Arch Pediatr Adolesc Med. 2003;157(4):369–74.
Ding L, Sun Q, Sun W, Du Y, Li Y, Bian X, et al. Antibiotic use in rural China: a cross-sectional survey of knowledge, attitudes and self-reported practices among caregivers in Shandong province. BMC Infect Dis. 2015;15:576.
Yu M, Zhao G, Stalsby Lundborg C, Zhu Y, Zhao Q, Xu B. Knowledge, attitudes, and practices of parents in rural China on the use of antibiotics in children: a cross-sectional study. BMC Infect Dis. 2014;14:112.
Zou G, Wei X, Hicks JP, Hu Y, Walley J, Zeng J, et al. Protocol for a pragmatic cluster randomised controlled trial for reducing irrational antibiotic prescribing among children with upper respiratory infections in rural China. BMJ Open. 2016;6(5):e010544.
Wei X, Zhang Z, Walley JD, Hicks JP, Zeng J, Deng S, et al. Effect of a training and educational intervention for physicians and caregivers on antibiotic prescribing for upper respiratory tract infections in children at primary care facilities in rural China: a cluster-randomised controlled trial. The Lancet Global Health. 2017;5(12):e1258–67.
Kung K, Wong CKM, Wong SYS, Lam A, Chan CKY, Griffiths S, et al. Patient presentation and physician management of upper respiratory tract infections: a retrospective review of over 5 million primary clinic consultations in Hong Kong. BMC Family Practice. 2014;15(1):95.
Gonzales R Jr, Barrett PH, Steiner JF. The relation between purulent manifestations and antibiotic treatment of upper respiratory tract infections. J Gen Intern Med. 1999;14(3):151–6.
Murray S, Del Mar C, O’Rourke P. Predictors of an antibiotic prescription by GPs for respiratory tract infections: a pilot. Fam Pract. 2000;17(5):386–8.
McNulty CA, Nichols T, French DP, Joshi P, Butler CC. Expectations for consultations and antibiotics for respiratory tract infection in primary care: the RTI clinical iceberg. Br J Gen Pract. 2013;63(612):e429–36.
Hou D, Wang Q, Jiang C, Tian C, Li H, Ji B. Evaluation of the short-term effects of antimicrobial stewardship in the intensive care unit at a tertiary hospital in China. PLoS ONE. 2014;9(7):e101447.
Butler CC, Kinnersley P, Prout H, Rollnick S, Edwards A, Elwyn G. Antibiotics and shared decision-making in primary care. J Antimicrob Chemother. 2001;48(3):435–40.
Administration CFaD. Provisions for supervision of drug distribution. 2007. http://eng.sfda.gov.cn/WS03/CL0768/61650.html.
Grigoryan L, Burgerhof JG, Degener JE, Deschepper R, Lundborg CS, Monnet DL, et al. Attitudes, beliefs and knowledge concerning antibiotic use and self-medication: a comparative European study. Pharmacoepidemiol Drug Saf. 2007;16(11):1234–43.
André M, Vernby Å, Berg J, Lundborg CS. A survey of public knowledge and awareness related to antibiotic use and resistance in Sweden. J Antimicrob Chemother. 2010;65(6):1292–6.
Mainous AG, Hueston WJ, Eberlein C. Colour of respiratory discharge and antibiotic use. The Lancet. 1997;350(9084):1077.
Heald A, Auckenthaler R, Borst F, Delaspre O, Germann D, Matter L, et al. Adult bacterial nasopharyngitis: a clinical entity? J Gen Intern Med. 1993;8(12):667–73.
Acknowledgements
The study was funded by the National Nature Science Foundation of China (NSFC 71704003). The authors thank the local health and family planning commission at each study site for their field coordination and support throughout the study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cheng, J., Chai, J., Sun, Y. et al. Antibiotics use for upper respiratory tract infections among children in rural Anhui: children’s presentations, caregivers’ management, and implications for public health policy. J Public Health Pol 40, 236–252 (2019). https://doi.org/10.1057/s41271-019-00161-w
Published:
Issue Date:
DOI: https://doi.org/10.1057/s41271-019-00161-w