Abstract
In Korea, patients with stroke are commonly treated using traditional Korean medicine (TKM). The aim of this study was to provide information on the clinical characteristics of the pattern identification (PI) of stroke used in TKM. Stroke patients admitted to 15 TKM university hospitals from April 2005 through December 2013 were evaluated. The measured variables included the following factors as they related to the PI: (a) stroke etiology; (b) distribution of symptoms/signs; (c) physical characteristics and lifestyle parameters; (d) medical history; and (e) stroke-related laboratory results. Among 4912 stroke patients, 3466 patients received the same PI by two experts with the following distribution: Qi-Deficiency pattern (n = 810), Fire-Heat (FH) pattern (n = 1031), Dampness-Phlegm (DP) pattern (n = 1127), and Yin-Deficiency pattern (n = 498). Approximately 89.9% of subjects enrolled in this study had cerebral infarction. Some of specific symptoms were related to each type of PI, and obese phenotypes and blood lipids were significantly related to DP and FH. These results showed the characteristics of each type of PI and should lead to the standardization of diagnosis for stroke in TKM.
Similar content being viewed by others
Introduction
In Korea, the second most common cause of death is stroke, and the treatment and management of cerebrovascular diseases incurs a large financial burden1,2. Many stroke patients receive traditional medical care in Korea. According to a recent report from the Korean Ministry of Health and Welfare, stroke inpatients comprise the largest proportion of inpatients in traditional Korean medicine (TKM) hospitals3.
PI is a traditional diagnostic system characterized by its own theoretical basis and practical experience in traditional Eastern-Asian medicine (TEAM), which is practiced in China, Korea and Japan4,5,6,7. PI is the foundation of the treatment disease in TEAM. In traditional Chinese medicine (TCM), stroke is classified into six subtypes according to PI, and Zhou et al. reported the efficacy of therapies based on PI among patients with cerebral infarction8.
PI diagnosis is processed by the combination of signs and symptoms that are, specific and/or non-specific for diseases through observation, listening, questioning and feeling the pulse9.
However, the PI diagnosis exhibits limited objectivity and reproducibility due to the lack of standardized measurement indices, and it is difficult to objectify a diagnosis among physicians due to variations in their knowledge and experience4,5,6,10. As the demand for the reestablishment and development of TKM has increased, studies on the establishment of a scientific basis for and the standardization of PI have been actively conducted7.
The Korea Institute of Oriental Medicine (KIOM) conducted the project “Fundamental study for the standardization and objectification of pattern identification in TKM for stroke (SOPI-Stroke)” over the course of nine years from April 2005 to December 20135,6.
The purpose of this paper was to evaluate the distribution and characteristics of several key factors, including demographic parameters, lifestyle factors, symptoms/signs, stroke etiology, medical history, and laboratory results, in relation to the PI of stroke patients in TKM according to the results of the SOPI-Stroke project.
Results
Stroke etiology in relation to PI
Of the 4921 stroke patients collected over nine years, 3466 patients received the same PI diagnosis by two TKM experts with the following distribution: Qi-Deficiency (QD) pattern (n = 810, 23.37%), Fire-Heat (FH) pattern (n = 1031, 29.75%), Dampness-Phlegm (DP) pattern (n = 1127, 32.52%), and Yin-Deficiency (YD) pattern (n = 498, 14.37%). The different stroke types and NIHSS scores in relation to PI are presented in Table 1. Approximately 89.9% of subjects enrolled in this study had cerebral infarction (CI). In the TOAST classification of CI type, many subjects exhibited small vessel occlusion (SVO) rather than large artery atherosclerosis (LAA). The NIHSS score of the majority of patients was below 15. Among PI, the frequency of CI and SVO in the DP pattern was slightly higher than the YD pattern, but the NIHSS score among PI was not different.
Distribution of symptoms/signs in relation to PI
The Korean standard PI (K-SPI) of stroke consists of four PIs (QD, FH, DP, and YP pattern), and a total of 44 symptoms/signs for determining PI were reported in a previous study6. Variables are classified into four types: 19 FH variables, 7 DP variables, 11 QD variables, and 11 YD variables. Table 2 shows the distribution of the variables according to PI. In the FH pattern, headache-like flush, red tongue and strong pulse were the major symptoms. In the DP pattern, obesity (bi-sup) and a white “fur” on the tongue were common. Appearing powerless and lethargic and weak pulse symptoms were commonly observed in the QD pattern. Tidal fever, dry mouth and gauntness were more common in the YD pattern than in other PIs.
Physical characteristics and lifestyle parameters in relation to PI
Table 3 shows the physical characteristics and lifestyle patterns in relation to PIs. The BMI and WHR, which are related with obesity, were higher in the DP pattern than in other PIs. For lifestyle patterns, subjects that were currently smokers and drinkers were more likely to exhibit the FH pattern than the QD or YD pattern. Food preferences were also different according to PI.
Medical history in relation to PI
The subjects’ medical histories are presented in Table 4. With regard to past medical history, more than 58% of the patterns showed hypertension, which was the most common (58.43–63.35%) disease. A stroke-related history of diseases such as hypertension, DM, and heart attack was observed. However, the distribution among PIs was not different.
Blood parameters in relation to PI
The subjects’ blood parameters are presented in Table 5. In the haematology category, the levels of WBC, hemoglobin and hematocrit were higher in the FH pattern than in the other PIs. The platelet level was higher in the DP pattern, and the serum levels of lipids, including total cholesterol and triglycerides, were higher in the DP pattern compared to the other groups. Homocysteine and vitamin B12, which are indirect indicators of stroke, showed a different tendency among the pattern groups. The levels of homocysteine were higher in the FH group compared to the other groups, but the level of vitamin B12 was higher in the YD group.
Discussion
In the practice of TEAM, including TCM and TKM, a unique decision-making process called Bian Zheng Lun Zhi (PI or syndrome differentiation followed by treatment) is widely used11. This method, also called traditional Chinese medical diagnostics, is the procedure and practice of examining patients, determining diseases and differentiating syndromes/identifying patterns of signs and symptoms of diseases4. Through the comprehensive analysis of symptoms and signs, which has implications in determining the cause, nature and location of the illness and the patient’s physical condition, their treatment is determined and confirmed4,11. According to TEAM theory, even patients with the same disease receive different treatments based on PI results. Although this diagnostic system has many advantages in that it uses a comprehensive analysis of symptoms and signs to assess the cause of the diseases, there are many variations in the diagnostic process7,12.
KIOM focuses on the importance of standardization in PI and has been engaged in relevant research7. The SOPI-Stroke project was conducted by KIOM from April 2005 to December 2013 to standardize and objectify PI for stroke through a scientific process5,6,10. In a previous study, our team described the four standard patterns, FH pattern, DP pattern, YD pattern, and QD pattern, in stroke and the forty-four indices used to determine the pattern6. This paper provides the characteristics, laboratory results and symptoms and signs of stroke patients who were treated according to TKM in the SOPI-Stroke project.
Among the symptoms/signs for PI diagnosis, some were common in each of the types of PI (Table 2). Over 80% of subjects with the FH pattern exhibited a reddened complexion, red tongue and a strong pulse. A white “fur” on the tongue and obesity (bi-sup) were major symptoms in the DP pattern, and many patients with the QD pattern appeared powerless and lethargic and had a weak pulse pattern. The YD pattern was associated with paleness, a red zygomatic site and dry mouth. These results were similar to other studies presented by our team and other TCM researchers13,14.
Many previous studies were performed to evaluate the relationship between Western indicators, such as body composition or blood parameters, and PI patterns15,16,17,18,19. Tables 3 and 5, respectively, show the distribution of body composition and blood parameters among PI. Among these, the level of obesity indices, including BMI and waist circumference, were significantly higher in the DP and FH patterns than in the QD and YD patterns (Table 3). Total cholesterol, triglycerides and total lipids, which are blood parameters positively related to obesity, were also higher in the DP and FH (Table 5). These results are similar to those previously reported by Min et al.15, and other studies showed that DP was significantly related to the obese phenotype16,17,18.
Genetic studies showed that many of the gene polymorphisms were related to obesity and obese phenotypes20,21,22,23. Similar studies that show the association between genetic polymorphisms and PI were performed in TKM and TCM17,24,25,26. Specifically, the polymorphisms in UCP2 and UCP3, which were significantly associated with BMI and serum cholesterol in Korean female subjects, were also associated with DP pattern24,27,28. Some studies showed controversial results. For example, Kim et al. reported that subjects with the C allele of −607 G > C in wnt10b had lower BMI levels than subject with the GG type29, but Ko et al. showed that the −607 G > C polymorphism was related to the YD pattern, not DP pattern25. Those results suggested that the PI, a diagnostic system used in TEAM, exhibited similar or different phenotypes compared to the phenotypes discussed in Western medicine.
There are some limitations to our study. To obtain the characteristics of stroke patients treated with TKM, observational studies are very important. This is a potentially interesting observational study because it provided evidence for clinical practice. This paper describes the baseline characteristics of stroke according to PI but there is no follow-up data describing long-term outcomes. Therefore, it is necessary to conduct improved randomized controlled trial studies or cohort studies to obtain reliable results on PI phenotypes and the effect of treatment based on PI compared with Western medicine. Second, the population enrolled in this study focused on the CI type and SVO type according to the TOAST classification. Additionally, the severity of stroke in the enrolled patients was lower than that of stroke patients visiting Western medical hospitals. For this reason, it is difficult to generalize the characteristics of PI. TKM uses four methods of diagnosis, which include diagnosis by observation, hearing and smelling, interrogation, and palpation. Diagnosis depends on the clinician’s experience and knowledge, along with a variety of environmental factors. It is essential to establish an objective diagnostic standard for tongue and pulse measurements, along with other reliable diagnostic tools.
Although this study had some limitations, the significance of our study was to show the characteristics of the patients receiving TKM treatment. In TKM treatment, PI comprises a series of processes that involve not only identifying specific neurological symptoms but also unspecific symptoms and indicators with four examinations, as well as determining treatment goals after integrating all the data for stroke diagnosis. These results should to lead to the standardization of PI for stroke in TKM.
Methods
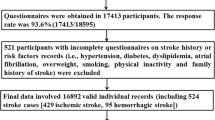
Subjects
This study was a community-based multicentre trial that was part of the SOPI-Stroke project5,6. Stroke patients who were admitted to 15 TKM university hospitals participated in this study from 2005 through 2013 (The entire list of hospitals can be found as Supplementary Table S1). Each patient provided written informed consent to undergo procedures that were approved by the respective institutions’ Institutional Review Boards (IRB). This study was conducted in accordance with approved guidelines by the IRB of the KIOM and by each TKM university hospital’s IRB. All patients provided informed consent after a thorough explanation of the details. Figure 1 shows the PI distribution among stroke patients by gender according to region.
(A) Capital (n = 1865): Gachon University Gil Korean Medical Hospital, Kyung Hee Korean Medical Center, Kyung Hee University Hospital at Gangdong, Dong Guk University Hospital, Dong Seo Medical Center; (B) Kwang won/Chung cheong(n = 930): Dae Jeon Korean Medical Hospital, Sang Ji Korean Medical Hospital; (C) Yeong nam(n = 228): Dae Gu Hanny University Medical Center, Dong Eui Hospital; (D) Honam(n = 443): Dong Sin Korean Medical Hospital, Woo Suk University Korean Hospital(Jeonju),Won Kwang Korean Medical Hospital; QD: qi deficiency pattern. FH: fire-heat pattern. YD: yin deficiency pattern. DP: dampness phlegm pattern.
Inclusion/exclusion criteria
We enrolled stroke patients within 30 days of the onset of their symptoms if their diagnosis was confirmed by an imaging diagnosis such as computerized tomography (CT) or magnetic resonance imaging (MRI)5,6. Patients with traumatic stroke such as subarachnoid, subdural, and epidural haemorrhage were excluded from the study. This study was approved by the IRB of the KIOM and by each TKM university hospital’s IRB.
Measured variables
Each patient was seen by two experts in the same department within each site. All experts were well trained in standard operation procedures (SOPs). The experts had at least three years of clinical experience with stroke after finishing a regular college education of TKM for six years. The examination parameters were extracted from parts of a case report form (CRF) for the standardization of stroke diagnosis developed by an expert committee organized by the KIOM. The measured variables used included the following key subjects in relation to PI: (a) stroke etiology; (b) distribution of signs/symptoms; (c) physical characteristics and lifestyle parameters; (d) medical history; and (e) laboratory results. Specifically, as suggested by the KIOM, the clinicians were required to measure the stroke PI of each patient according to the FH pattern, DP pattern, QD pattern, or YD pattern.
Statistics
Data were statistically analysed with SAS software, version 9.1.3 (SAS Institute Inc., Cary, NC, USA). Categorical variables were compared with the chi-square test or Fisher’s exact test, and differences in continuous variables were determined by one-way analysis of variance (ANOVA). Statistical significance was set at P < 0.05.
Additional Information
How to cite this article: Ko, M. M. et al. Stroke in Traditional Korean Medicine: A Nine-Year Multicentre Community-Based Study in South Korea. Sci. Rep. 6, 28286; doi: 10.1038/srep28286 (2016).
References
Social Statistics Bureau in Korea National Statistical Office. Causes of death statistics in 2013. Annual report. Available at: http://kostat.go.kr/portal/eng/pressReleases/1/index.board?bmode=read&aSeq=330671 (Accessed: 4th March 2016) (2014).
Division of Statistical Analysis in Korean National Health Insurance Cooperation. Annual report of national health insurance statistics. Annual report. Available at: http://www.hira.or.kr/dummy.do?pgmid=HIRAA020045010000&cmsurl=/cms/medi_info/07/03/02/1204381_27401.html&subject=2009%eb%85%84+%ea%b1%b4%ea%b0%95%eb%b3%b4%ed%97%98%ed%86%b5%ea%b3%84%ec%97%b0%eb%b3%b4 (Accessed: 4th March 2016) (2010).
Ministry of Health and Welfare. The third utilization of oriental medical services survey 2014. Available at: http://www.mohw.go.kr/front_new/al/sal0301vw.jsp?PAR_MENU_ID=04&MENU_ID=0403&CONT_SEQ=317464&page=1 (Accessed: 4th March 2016) (2015).
WHO Regional Office for the Western Pacific, WHO International Standard Terminologies on Traditional Medicine in the Western Pacific Region. Geneva. Available at: http://www.wpro.who.int/publications/who_istrm_file.pdf?ua=1 (Accessed: 4th March 2016) (2007).
Park, T. Y. et al. The fundamental study for the standardization and objectification of pattern identification in Traditional Korean medicine for stroke: an overview of phase I. Eur J Integr Med 4, e125–e131 (2014).
Lee, J. A. et al. Fundamental study for the standardization and objectification of pattern identification in traditional Korean medicine for stroke: An overview of the second and third stages. Eur J Integr Med 7, 378–383 (2015).
Ko, M. M., Lee, J. A., Yun, K. J., You, S. S. & Lee, M. S. Perception of pattern identification in traditional medicine: a survey of Korean medical practitioners. J Tradit Chin Med 34, 369–372 (2014).
Working Group on Cerebrovascular Diseases, Chinese Society of Neurology. Chinese guidelines for diagnosis and treatment of acute ischemic stroke 2010 edition. Chin J Neurol 43, 146–152 (2010).
Li, Z., Chen, Y., Liu, J., Liu, Z.-l. & Gao, Y. Evaluating the implementation of evidence-based TCM Clinical Practice Guidelines for Cerebral Infarction. Eur J Integr Med 6, 147–155 (2014).
Lee, J. A. et al. Developing indicators of pattern identification in patients with stroke using traditional Korean medicine. BMC Res Notes 5, 136 (2012).
Wu, H. Z., Fang, Z. Q. & Cheng, P. J. Introduction to diagnosis in traditional Chinese Medicine. World Century Publishing Corporation, Singapore (2013).
Man, Y. N., Liu, X. H. & Wu, X. Z. Chinese medicine herbal treatment based on syndrome differentiation improves the overall survival of patients with unresectable hepatocellular carcinoma. Chin J Integr Med 21, 49–57 (2015).
Cheng, S. C. et al. Fire-Heat and Qi Deficiency Syndromes as Predictors of Short-term Prognosis of Acute Ischemic Stroke. J Altern Complement Med 19, 721–728 (2012).
Cao, K. G. et al. Y. A new prognostic scale for the early prediction of ischemic stroke recovery mainly based on traditional Chinese medicine symptoms and NIHSS score: a retrospective cohort study. BMC Complement Altern Med 15, 407 (2015).
Min, I. K. et al. The relation of dampness-phlegm and metabolic syndrome in acute stroke patients [in Korean]. J Korean Oriental Med 30, 109–119 (2009).
Ko, M. M., Kang, B. K., Lim, J. H., Lee, M. S. & Cha, M. H. Genetic association of NPY gene polymorphisms with dampness-phlegm pattern in Korean stroke patients. Evid Based Complement Alternat Med 2012, 109796 (2012).
Lim, J. H., Ko, M. M., Moon, T. W., Cha, M. H. & Lee, M. S. Association of the UCP-1 single nucleotide polymorphism A-3826G with the dampness-phlegm pattern among Korean stroke patients. BMC Complement Altern Med 12, 180 (2012).
Cha, M. H., Jones, A. D., Ko, M. M., Zhang, C. & Lee, M. S. Metabolic profiles distinguish non-dampness-phlegm and dampness-phlegm patterns among Korean patients with acute cerebral infarction. Evid Based Complement Alternat Med 2013, 517018 (2013).
Cha, M. H. et al. Study on the Obesity and Blood parameters Differences between Fire/Heat and Qi-deficiency Pattern Identification/Syndrome Differentiation among Acute Stroke Patient. Korean J Orient Int Med 30, 772–779 (2009).
Yako, Y. Y. et al. Genetic association studies of obesity in Africa: a systematic review. Obes Rev 16, 259–272 (2015).
Zhang, M., Wang, M. & Zhao, Z. T. Uncoupling protein 2 gene polymorphisms in association with overweight and obesity susceptibility: A meta-analysis. Meta Gene 2, 143–159 (2014).
Taylor, J. Y. et al. An overview of the genomics of metabolic syndrome. J Nurs Scholarsh 45, 52–59 (2013).
Rankinen, T. et al. The human obesity gene map: the 2005 update. Obesity (Silver Spring) 14, 529–644 (2006).
Lim, J. H. et al. Differential Association of Uncoupling Protein 2 Polymorphisms with Pattern Identification among Korean Stroke Patients: A Diagnostic System in Traditional Korean Medicine. Evid Based Complement Alternat Med 2012, 532078 (2012).
Ko, M. M., Park, T. Y., Lim, J. H., Cha, M. H. & Lee, M. S. WNT10B Polymorphism in Korean Stroke Patients with Yin Deficiency Pattern. Evid Based Complement Alternat Med 2012, 798131 (2012).
Guo, J. et al. Syndrome Differentiation of Diabetes by the Traditional Chinese Medicine according to Evidence-Based Medicine and Expert Consensus Opinion. Evid Based Complement Alternat Med 2014, 492193 (2014).
Cha, M. H. et al. Association of UCP2 and UCP3 gene polymorphisms with serum high-density lipoprotein cholesterol among Korean women. Metabolism 56, 806–813 (2007).
Cha, M. H., Shin, H. D., Kim, K. S., Lee, B. H. & Yoon, Y. The effects of uncoupling protein 3 haplotypes on obesity phenotypes and very low-energy diet–induced changes among overweight Korean female subjects. Metabolism 55, 579–586 (2006).
Kim, I. C. et al. functional promoter polymorphism −607G > C of WNT10B is associated with abdominal fat in Korean female subjects. J Nutr Biochem 22, 252–258 (2010).
Acknowledgements
Thanks for many supports in this study as collaborator by Bo Young Kim (Korea Institute of Oriental Medicine), Dr. Bongki Park (Dongguk University Medical Center), Byeong Chan Yu, Prof. Chang-Ho Han (Dongguk University), Prof. Chang-nam Ko (Kyung Hee University Hospital at Gangdong), Prof. Chan-yong Chen (Gachon University Korean Medicine Hospital), Prof. Dong-Eog Kim (Dongguk University Ilsan Hospital), Eun Hyoung Shim (Korea Institute of Oriental Medicine), Prof. Gil-Cho Shin (Dongguk University), Prof. Ho-Yeon Go (Semyung University), Hoyoung Lee (Korea Institute of Oriental Medicine), Prof. In Chan Seol (Daejeon University Hospital ar Dunsan), Prof. In Lee (Pusan National University Korean Medicine Hospital), Dr. Jeeyoun Jung (Korea Institute of Oriental Medicine), Jeong-Cheol Kim, Ji Hee Jun (Korea Institute of Oriental Medicine), Ji Hye Lim, Jiae Choi (Korea Institute of Oriental Medicine), Jin-Seok Moon (Korea Institute of Oriental Medicine), Dr. Joong Kil Kim, Dr. Jungsup Lee (Korean National Rehabilitation Center), Prof. Ki-Ho Cho (Kyung Hee University), Kyung Won Kang, Kyung-Jin Yun, Dr. No Soo Kim (Korea Institute of Oriental Medicine), Dr. Ok-Sun Bang (Korea Institute of Oriental Medicine), Dr. Sae-Wook Park, Se-Mi Oh, Seon Hwa Shin, Prof. Seong-Gyu Ko (Kyung Hee University), Dr. Sooseong You (Korea Institute of Oriental Medicine), Prof. So-Yeon Kim (Pusan National University Korean Medicine Hospital), Executive director of R&D Sun Mi Choi (Korea Institute of Oriental Medicine), Dr. Tae-Woog Moon (Jaseng Oriental Hospital), Prof. Tae-Yong Park (Catholic Kwandong University), Dr. Tae-Young Choi (Korea Institute of Oriental Medicine), Prof. Yoon Sik Kim (Daejeon University Hospital at Cheonan), Prof. Yoosik Yoon (Chung-Ang University), Prof. Young Kyun Kim (Dong-Eui University Korean Medicine Hospital). Orders of all co-authors are followed alphabetical order. This research was supported by a grant from the Korea Institute of Oriental Medicine (no. K13130, no. K16111).
Author information
Authors and Affiliations
Contributions
M.M.K., J.A.L. and M.S.L. designed the study. M.M.K., M.H.C. and B.-K.K. participated in the design of the study and performed the statistical analysis. M.S.L. and J.A.L. conceived of the study, and participated in its design and coordination and helped to draft the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Supplementary information
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Ko, M., Lee, J., Cha, M. et al. Stroke in Traditional Korean Medicine: A Nine-Year Multicentre Community-Based Study in South Korea. Sci Rep 6, 28286 (2016). https://doi.org/10.1038/srep28286
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep28286
- Springer Nature Limited