Abstract
A critical issue in the management of chronic kidney disease (CKD) is to prevent patients from the progression to end-stage kidney disease (ESKD), however, there is only limited number of biomarkers for the discrimination of the high-risk CKD patients. We aimed to identify the metabolites which possess the ability to predict the earlier kidney deterioration. We performed capillary electrophoresis and liquid chromatography mass spectrometry (CE-MS)-based metabolic profiling in a prospective cohort, which consisted of referred 112 CKD patients with median follow-up period of 4.4 years. The association between the levels of candidate metabolites and the outcomes (progression to ESKD alone or in combination with death before ESKD) were assessed by multivariate Cox proportional hazard models after adjusting for the baseline covariates. A total of 218 metabolites were detected in the plasma of CKD patients. We identified 16 metabolites which have predictive values for the composite outcome: The risk for composite outcome was elevated from 2.0- to 8.0-fold in those with higher levels of 16 plasma metabolites. Our results suggest that the measurement of these metabolites may facilitate CKD management by predicting the risk of progression to ESKD.
Similar content being viewed by others
Introduction
Chronic kidney disease (CKD) is a global health problem1. CKD patients are widely prevalent, and the number of end-stage kidney disease (ESKD) patients is still increasing. ESKD patients requires cost-prohibitive kidney replacement therapy2. Moreover, CKD patients are highly vulnerable, and the risk of cardiovascular events and death increases with the progression of CKD stages3,4,5,6. Thus, it is critical to predict their risk for the progression to ESKD in CKD patients to avoid these unfavorable situations.
Taking the fact that kidney is one of metabolically-active organs7,8, the metabolic profiling of CKD patients is a promising method to identify new biomarkers for the prognoses of CKD patients. Recent cross-sectional studies have demonstrated the correlations between kidney function and the levels of certain metabolites in CKD patients9,10,11,12,13. The presence or altered levels of certain metabolites was also suggested in ESKD patients14. Population-based studies also demonstrated that the levels of some metabolites were associated with the incidence of CKD15,16 or with the worsening of kidney function, i.e., the decrease in estimated glomerular filtration ratio (eGFR, a calculated product of creatinine, sex, and age)17,18. A nested-cohort study in diabetic patients with early stages of CKD (mainly stage 1 and 2) showed a specific metabolomic profile in those who progressed to ESKD within an observational period19. The importance of metabolic profiling and the aberrance of metabolism in CKD patients have been emphasized20, however, the number of prospective metabolomic studies is limited thus far. Thus, whether certain metabolic changes could predict rapid progression of ESKD in referred CKD patients is largely unknown.
We conducted capillary electrophoresis and liquid chromatography mass spectrometry (CE-MS)-based metabolic profiling21,22 in a prospective longitudinal cohort, which was composed of referred CKD patients who were not on dialysis at entry. We aimed to prove that the levels of a subset of blood metabolites would predict the further worsening of kidney function, with the goal to raise the possibility that the measurements of these metabolites will facilitate the management of referred CKD patients.
Results
We performed a metabolic profiling from a prospective cohort, which consisted of referred CKD patients. Data were generated from 112 participants with median follow-up period of 4.4 years (IQR, 2.4–5.5). The baseline characteristic is shown in Table 1. None of the participants were lost to follow-up. Among these patients, 61 started kidney replacement therapy and 17 died, including 4 who died before initiating kidney replacement therapy.
Metabolomic analyses were performed using the plasma samples of this cohort. Out of 579 metabolites in the library, a total of 218 metabolites were detected in the plasma of CKD patients. Among them, 129 metabolites, including creatinine and urea nitrogen, were above the detection limits in at least 40% of study subjects and were subjected to the rest of the analyses. The levels of 73 out of 129 metabolites were significantly correlated with eGFR (Figs S1–3): the increased levels of urea and creatinine, which represent kidney function, showed the strongest correlation with the decreased level of eGFR, whereas the levels of the rest of metabolites variably, but less strongly, correlated.
The levels of metabolites were divided into three tertiles and were subjected to the Cox regression analyses. The Holm-corrected multiple testing revealed that the levels of 26 out of 127 metabolites (creatinine and urea were excluded) had predictive values on the composite outcome (a combination of end-stage kidney disease requiring replacement therapy and all-cause of death, Table S1). These metabolites were detected in more than 80% of patients except for 2-hydroxyisobutyrate (67.5%), cytidine (56.4%), and 3-hydroxy-3-methylglutarate (53.0%). We fitted multiple Cox regression analyses to assess the predictive value of the levels of these metabolites by adjusting for eGFR, the level of urinary protein, and other clinical covariates such as the presence of diabetes. After adjustment for the clinical covariates, the levels of 16 out of 26 metabolites remained as significant predictors of the composite outcome when tertiles were analyzed as continuous variables (Table 2). The results were largely similar when analyzed for ESKD (Table S2). Patients in the top tertile of these metabolites had 2.0- to 8.0- fold higher adjusted hazard ratios for the composite outcomes, compared with those in the lowest tertile (Fig. 1 and Tables 2 and S2).
Kaplan-Meier curve analyses demonstrated that patients with the higher levels of 58 metabolites including creatinine and urea, and the lower levels of 4 metabolites, more frequently reached the composite outcome (Figs 2 and S4). Among them, 16 metabolites identified in the analysis above robustly divided the likelihood of reaching the composite outcome (Fig. 2). Because not a small fraction of this cohort is diabetic patients, we stratified the analyses by its presence (Table S3 and Fig. S5). The levels of some metabolites showed good predictive values specifically in the presence (4-oxopentanoate, glucoronate, 2-hydroxyisobutyrate, 5-oxoproline, pimelate, N-acetylneuraminate, 3-methylhistidine, phthalate, trp, hippurate, and 3-hydroxy-3-methylglutarate) or absence (citramalate and 2,3-pyrinedicarboxylate) of diabetes, although the levels of some showed the predictive values regardless of the presence or the absence of diabetes (isethionate, saccharate, trimethylamine N-oxide, cytidine, gluconate, guanidinosuccinate, and uridine).
Discussion
By applying CE-MS-based metabolic profiling, we identified 16 prognostic metabolites in CKD patients. The risk of developing ESKD was elevated from 2.0- to 8.0-fold in those with higher or lower levels of plasma metabolites. Although the levels of some of the metabolites identified in this study correlated with eGFR, these metabolites are associated with kidney deterioration even when they were adjusted for the baseline kidney function. These findings may support the notion that measurement of these metabolites in CKD patients would be a useful tool to assess the risk of progression to ESKD.
The number of studies using metabolomics in CKD studies as a tool is increasing, which strongly suggests the growing interests of this field9,10,11,12,14,15,16,17,18,19. In their first application of metabolomics on CKD study, Toyohara et al. demonstrated correlations between the levels of 64 plasma metabolites and that of eGFR in CKD patients9. Rhee et al. showed that the levels of 49 metabolites were altered in ESKD patients on hemodialysis compared with age-matched control14. Shah et al. showed significant differences in the levels of some plasma metabolites among various stages of CKD 2–410. Hirayama et al. identified some metabolites whose levels were associated with the presence of nephropathy (assessed by the presence of macroalbuminuria) in diabetic patients11, while Sharma et al. demonstrated that the levels of 12 metabolites were associated with the presence of diabetes in CKD12. By nested-cohort study, Niewczas et al. demonstrated that the levels of some plasma metabolites had significant odds ratios for the incidence of ESKD during the observational period in diabetes patients (CKD stage 1–2, 78%; stage 3, 22%)19. In population-based studies, Rhee et al. and Yu et al. demonstrated that a subset of blood metabolites in study participants (eGFR ≥60 mL/min/1.73 m2) were associated with the onset of incident CKD (defined by eGFR of <60)15,16. Geok et al. demonstated that the levels or the combined ratios of some serum metabolites were associated with the decreased ratio of eGFR17,18. The present study added the important prognostic notion that patients with advanced CKD stages have particular metabolomic profiles that are associated with worse prognoses.
The 16 metabolites identified in the present cohort are located on widely variable metabolic pathways. These pathways include nucleotides (cytidine and uridine), glycolysis (gluconate [also known as gluconic acid] and saccharate [glucaric acid]), amino acids (guanidinosuccinate [guanidinosuccinic acid] and 3-methylhistidine), amino sugar (N-acetylneuramine [N-acetylneuraminic acid] and glucoronate [glucuronic acid]), biotin (pimelate [heptanedioic acid]), glutathione (5-oxoproline [pyroglutamic acid]), and taurine (isethionate [2-hydroxyethanesulfonate]). In addition, the origins or pathways of some metabolites are unidentified (4-Oxopentanoate [levulinic acid, 4-ketovalerate], trimethylamine N-oxide [TMAO], citramalate, 2-hydroxyisobutyrate [alpha-hydroxyisobutyric acid, acetonate], and phthalate [Alizarinate, Naphthalinate]). These metabolites might be originated from extracorporeal metabolisms such as gut flora, dietary, and environmental chemicals, whose importance in CKD patients are rediscovered recently23. The presence of broad pathways behind the identified metabolites in our study may reflect the complicated process of kidney deterioration24.
The association with kidney function have been demonstrated in some of metabolites identified in this study. Guanidinosuccinate, trimethylamine N-oxide, 3-methylhistidine25, cytidine26, and uridine27 are ones of the earliest uremic toxins whose toxicity are identified28,29. Trimethylamine N-oxide is also associated with onset of CKD15. Both cytidine and uridine are pyrimidine-derived nucleosides, and the level of cytidine is known to decrease in kidney from drug-induced kidney injury model rats30. Guanidinosuccinate is an acetyl derivative of the amino sugar neuraminic acid, whereas N-acetylneuramine, another metabolite identified in this study, is a major component of glycoconjugates, including glycoproteins which resides on cellular membranes to mediate several cellular functions. The fact that both guanidinosuccinate and N-acetylneuramine were identified as predictors for kidney deterioration in this study may suggest the potential roles of glycomodulation in the progression of kidney diseases. The fact that the level of 3-Methylhistidine, a component of actin and myosin, is associated with muscle protein breakdown31 may reflect muscle-wasting in kidney diseases32. 5-Oxoproline is known to increase its level in response to worsened kidney function9,33. 5-oxoproline is involved in the metabolism of glutathione, a major antioxidant, in both synthetic and degradative pathways. While our study is in revision, Yu et al. reported that lower levels 5-oxoproline was associated with incidence of CKD16, whereas our data suggested that its higher level was a risk for earlier kidney deterioration. The regulation of 5-oxoproline seems to be complicated and its level should be understood based on their kidney function and other underlying comorbidities. Interestingly, the levels of some metabolites have the potentials to predict prognosis in specific patients (i.e., in the presence or absence of diabetes). Whether these metabolites may reflect prognosis synergically or through specific association with certain underlying pathophysiology needs to be studied.
This study has some limitations that need to be addressed in further studies. Although the present study was strengthened by the longitudinal observation, the limitations exist on relatively small number of the cohort and the dependence only on the baseline characteristics. We performed power analyses using a type I error of 5% and 80% power. These analyses revealed that 19 or 65 patients would be needed for the median (3.62 for uridine) or lowest hazard ratios (2.01 for phthalate) of the selected metabolites in the prediction set, respectively. Therefore, we had enough sample size to determine the association between composite outcomes and these metabolites, though the effects of unselected metabolites might be underestimated. This is especially the case in the presence of statistical processes of multiple comparison or adjustments. The correlations between the metabolites identified in this study and eGFR also complicated the results. Although our results were achieved by adjusting for eGFR, we could not completely rule out residual confounding due to kidney function. We considered that the levels of these metabolites in CKD patients may not be simple reflections of the decreased level of eGFR based on the following observations34,35. First, the Spearman correlation coefficients for the selected metabolites with eGFR were not always the highest ones as shown in Fig. S2. Second, one metabolite (phthalate) was not significantly correlated with eGFR. Third, the coefficients of most of the metabolites were lower than that of hemoglobin (r = 0.58), which is used as a prognostic factor of CKD patients. Therefore, the metabolic profile of CKD patients identified in the present study may rather provide additional information for the progression of kidney disease. The importance of the identified metabolites and the variance in the concentrations of these metabolites need to be validated in future studies. Statistical multiple-comparison might have obscured the true relationship. Finally, we have no mechanistic data to demonstrate the reasons for the changes of the levels of these metabolites. Further mechanistic and causal studies together with validation studies will support our comprehensiveness and clinical application.
In summary, 16 metabolites were related to higher risk of the deterioration of kidney function in advanced CKD patients. Our studied population is based on referred CKD patients, who need immediate and impeding improvement of medical care. Measurement of the metabolites identified herein may facilitate our management of advanced CKD patients through the additional information on the clinical parameters, such as eGFR and urinary protein level. We propose that the metabolomic profiling of CKD patients will potentiate us to perform tailored management of CKD.
Methods
Study population and samples
We prospectively enrolled 118 consecutive patients with CKD stages 3, 4 and 5, who were not on dialysis, from a single nephrology department at Rinku General Medical Centre between August 2005 and January 2009. Baseline blood samples from patients after an overnight fast were collected. Patients with insufficient blood samples were excluded beforehand. This study was approved by the institutional ethics committees of Rinku General Medical Centre and Osaka General Medical Centre, and was adherent to the Declaration of Helsinki. All patients provided written informed consent to participate in the study.
Baseline inclusion criteria included age less than 90 years, no complication of malignancy, and no active infection. Patients with incomplete baseline data (n = 2) and started kidney replacement therapy within 1 month after the enrollment (n = 4) were excluded. Final analysis covered the remaining 112 patients.
Kidney function was evaluated from baseline data at the first visit to our outpatient clinic using the estimated glomerular filtration rate (eGFR) based on the equation for Japanese population36. The formula is as follows: eGFR = 194 × serum creatinine (SCr)−1.094 × age−0.287, where age is in years, SCr is in mg/dL and the glomerular filtration rate (GFR) is in mL/min/1.73 m2 body surface area. The product of this equation for women was multiplied by a correction factor of 0.739. Serum creatinine was measured by enzymatic methods in the same laboratory. Random urine samples (10 mL) were also collected at baseline to measure the ratio of urinary protein to creatinine. Other baseline variables included age, sex, diabetes defined according to the International Classification of Diseases, Tenth Revision (ICD-10) codes E10-E14, systolic blood pressure, diastolic blood pressure, hemoglobin, albumin, calcium, phosphate, and use of renin-angiotensin system inhibitor, beta-blocker, and calcium blocker. Cardiovascular disease included ischemic heart disease (ICD-10 codes I20-I25), heart failure (ICD-10 code I50), and stroke (ICD-10 codes I60-I67).
The primary end points were end-stage kidney disease (ESKD) requiring kidney replacement therapy and a composite of ESKD and all-cause of death.
Patients received regular follow-up care in the outpatient ward. Data were collected from source documentation at the end of 2011. The baseline and follow-up data were collected from hospital medical records and discharge abstracts, outpatient visit records, contact with primary and dialysis care physicians and death certificates. End points were validated by at least two physicians. The follow-up of patients is available with accuracy because i) this facility is the central hospital of the southern area of Osaka prefecture, and there is no other central hospital in this region, and ii) regional partnership with the primary and dialysis care physicians has been well-established.
Metabolite extraction and measurement
Metabolites were measured as previously reported with modification21,37. Briefly, plasma samples (40 μl) were put into 360 μl of methanol which contained internal standards [20 μmol/L each of methionine sulfone and 2-(N-morpholino)-ethanesul-fonic acid]. The homogenate was then mixed with 160 μl of Milli-Q water and 400 μl chloroform and centrifuged at 10,000 g for 5 min at 4 °C. Subsequently, the aqueous 300 μl solution was centrifugally filtered through a 5-kDa cutoff filter (Millipore) to remove proteins. The filtrate was centrifugally concentrated and dissolved in 50 μl Milli-Q water that contained reference compounds (200 μmol/L each of 3-aminopyrrolidine and trimesate) immediately before CE-TOFMS analysis.
Measurement of metabolites was performed using CE-TOMFS21,37. Briefly, CE-TOFMS was carried out using an Agilent CE Capillary Electrophoresis System equipped with 6210 Time-of-Flight mass spectrometer, 1100 isocratic HPLC pump, G1603A CE-MS adapter kit, and G1607A CE-ESI-MS sprayer kit. The system was controlled by Agilent G2201AA ChemStation software version B.03.01 for CE. Data acquisition was performed by Analyst QS Build: 7222 software for Agilent TOF (Applied Biosystems). For cationic metabolites, capillary electrophoreses were performed using a fused silica capillary. The electrolyte was 1 M formic acid. For anionic metabolites, a polymer coated COSMO (+) capillary (Nacalai, 07584-44i) was used. The electrolyte was 50 mM ammonium acetate (pH 8.5). For all analytical modes, inner diameter and total length of capillary are 50 μm and 100 cm, respectively. The applied voltage was set at +30 kV and −30 kV for cation and anion modes and nucleotide mode, respectively. Electrosplay ionisation-TOFMS was operated in the positive ion mode (4 kV), the negative ion mode (3.5 kV), and the negative ion mode (3.5 kV) for cationic metabolites, anionic metabolites, and nucleotides, respectively. Exact mass data were acquired over a 50–1000 m/z range. A mixed solution of the standards were prepared immediately before CE-TOFMS analysis as previously described22. The measured metabolite included amino acids, glycolysis intermediates, nucleotides, and their derivatives. CE exhibits extremely high resolution for charged species and its injection volume is quite low (3–30 nl). Therefore, matrix effects are hardly observed in CE-MS system38,39.
Data processing
Raw data were processed using software (MasterHands) developed in-house as previously described22. The data processing flow consisted of noise filtering, baseline correction, peak detection, and integration of the peak areas from 0.02 m/z-wide sections of the electropherograms. The accurate m/z of each peak was calculated by Gaussian curve-fitting on the m/z domain, and the migration times were normalized to match the detected peaks among the multiple datasets. The peaks were identified by matching m/z values and normalized migration times of corresponding authentic standard compounds. Quantification was performed by comparing the peak areas against a calibration curves generated using internal standardization-techniques to eliminate systematic bias which was derived from injection volume variance and MS sensitivity. Metabolites that were above the detection limit in at least 40% of study subjects were analyzed. We set this cut-off value for two reasons. First, we were afraid higher cut-off value may lead us to underestimate the effects of metabolites, which is against the screening-nature of this study. Second, we consider the possibility that the detection of a certain metabolite in itself may provide a valuable information for the prognosis. The levels of metabolites under detection limits were imputed with minimal value of each metabolite. The levels of metabolites collected here were exposed to the Holm’s multiple comparison as described below.
Statistical analysis
We constructed multivariate Cox proportional hazard models to assess an association between each candidate metabolite and the outcome after adjusting for the baseline covariates. Multiple comparison of the hazard models were performed with the Holm method. Log-rank test was used to assess the equality of survival distribution stratified by the median values. Statistical significance was defined as P < 0.05. Statistical analyses were performed using R environment for statistical computing, version 2.15.240, and STATA statistical software version 11 (STATA Corporation, College Station, TX, USA).
Additional Information
How to cite this article: Kimura, T. et al. Identification of biomarkers for development of end-stage kidney disease in chronic kidney disease by metabolomic profiling. Sci. Rep. 6, 26138; doi: 10.1038/srep26138 (2016).
References
Levey, A. S. et al. Chronic kidney disease as a global public health problem: approaches and initiatives-a position statement from Kidney Disease Improving Global Outcomes. Kidney Int 72, 247–259 (2007).
Coresh, J., Astor, B. C., Greene, T., Eknoyan, G. & Levey, A. S. Prevalence of chronic kidney disease and decreased kidney function in the adult US population: Third National Health and Nutrition Examination Survey. Am J Kidney Dis 41, 1–12 (2003).
Sarnak, M. J. et al. Kidney disease as a risk factor for development of cardiovascular disease: a statement from the American Heart Association Councils on Kidney in Cardiovascular Disease, High Blood Pressure Research, Clinical Cardiology, and Epidemiology and Prevention. Hypertension 42, 1050–1065 (2003).
Kimura, T. et al. Effects of chronic kidney disease and post-angiographic acute kidney injury on long-term prognosis after coronary artery angiography. Nephrol Dial Transplant 26, 1838–1846 (2011).
Yasuda, K. et al. Plasma B-type natriuretic peptide level predicts kidney prognosis in patients with predialysis chronic kidney disease. Nephrol Dial Transplant 27, 3885–3891 (2012).
Obi, Y. et al. Impact of age and overt proteinuria on outcomes of stage 3 to 5 chronic kidney disease in a referred cohort. Clin J Am Soc Nephrol 5, 1558–1565 (2010).
Kimura, T. et al. Autophagy protects kidney proximal tubule epithelial cells from mitochondrial metabolic stress. Autophagy 9, 1876–1886 (2013).
Namba, T. et al. Autophagic Clearance of Mitochondria in the Kidney Copes with Metabolic Acidosis. J Am Soc Nephrol 25, 2254–2266 (2014).
Toyohara, T. et al. Metabolomic profiling of uremic solutes in CKD patients. Hypertens Res 33, 944–952 (2010).
Shah, V. O. et al. Plasma metabolomic profiles in different stages of CKD. Clin J Am Soc Nephrol 8, 363–370 (2013).
Hirayama, A. et al. Metabolic profiling reveals new serum biomarkers for differentiating diabetic nephropathy. Anal Bioanal Chem 404, 3101–3109 (2012).
Sharma, K. et al. Metabolomics reveals signature of mitochondrial dysfunction in diabetic kidney disease. J Am Soc Nephrol 24, 1901–1912 (2013).
Nkuipou-Kenfack, E. et al. Assessment of metabolomic and proteomic biomarkers in detection and prognosis of progression of renal function in chronic kidney disease. PLoS One 9, e96955 (2014).
Rhee, E. P. et al. Metabolite profiling identifies markers of uremia. J Am Soc Nephrol 21, 1041–1051 (2010).
Rhee, E. P. et al. A combined epidemiologic and metabolomic approach improves CKD prediction. J Am Soc Nephrol 24, 1330–1338 (2013).
Yu, B. et al. Serum metabolomic profiling and incident CKD among African Americans. Clin J Am Soc Nephrol 9, 1410–1417 (2014).
Goek, O. N. et al. Serum metabolite concentrations and decreased GFR in the general population. Am J Kidney Dis 60, 197–206 (2012).
Goek, O. N. et al. Metabolites associate with kidney function decline and incident chronic kidney disease in the general population. Nephrol Dial Transplant 28, 2131–2138 (2013).
Niewczas, M. A. et al. Uremic solutes and risk of end-stage renal disease in type 2 diabetes: metabolomic study. Kidney Int 85, 1214–1224 (2014).
Breit, M. & Weinberger, K. M. Metabolic biomarkers for chronic kidney disease. Arch Biochem Biophys 589, 62–80 (2016).
Soga, T. et al. Differential metabolomics reveals ophthalmic acid as an oxidative stress biomarker indicating hepatic glutathione consumption. J Biol Chem 281, 16768–16776 (2006).
Hirayama, A. et al. Quantitative metabolome profiling of colon and stomach cancer microenvironment by capillary electrophoresis time-of-flight mass spectrometry. Cancer Res 69, 4918–4925 (2009).
Vaziri, N. D. CKD impairs barrier function and alters microbial flora of the intestine: a major link to inflammation and uremic toxicity. Curr Opin Nephrol Hypertens 21, 587–592 (2012).
Nangaku, M. Chronic hypoxia and tubulointerstitial injury: a final common pathway to end-stage renal failure. J Am Soc Nephrol 17, 17–25 (2006).
Counahan, R., El-Bishti, M., Cox, B. D. & Ogg, C. S. Plasma amino acids in children and adolescents on hemodialysis. Kidney Int 10, 471–477 (1976).
Gerrits, G. P. et al. Disturbances of cerebral purine and pyrimidine metabolism in young children with chronic renal failure. Nephron 58, 310–314 (1991).
Daniels, J. C. et al. Altered nucleic acid synthesis patterns in lymphocytes from patients with chronic uremia. Am J Med Sci 259, 214–227 (1970).
Kikuchi, T. et al. Liquid-chromatographic determination of guanidino compounds in plasma and erythrocyte of normal persons and uremic patients. Clin Chem 27, 1899–1902 (1981).
Simenhoff, M. L., Burke, J. F., Saukkonen, J. J., Ordinario, A. T. & Doty, R. Biochemical profile or uremic breath. N Engl J Med 297, 132–135 (1977).
Boudonck, K. J. et al. Discovery of metabolomics biomarkers for early detection of nephrotoxicity. Toxicol Pathol 37, 280–292 (2009).
Asatoor, A. M. & Armstrong, M. D. 3-methylhistidine, a component of actin. Biochem Biophys Res Commun 26, 168–174 (1967).
Kopple, J. D. McCollum Award Lecture, 1996: protein-energy malnutrition in maintenance dialysis patients. Am J Clin Nutr 65, 1544–1557 (1997).
Humphreys, B. D. et al. Acetaminophen-Induced Anion Gap Metabolic Acidosis and 5-Oxoprolinuria (Pyroglutamic Aciduria) Acquired in Hospital. American Journal of Kidney Diseases 46, 143–146 (2005).
Eloot, S. et al. Estimated glomerular filtration rate is a poor predictor of concentration for a broad range of uremic toxins. Clin J Am Soc Nephrol 6, 1266–1273 (2011).
Aronov, P. A. et al. Colonic contribution to uremic solutes. J Am Soc Nephrol 22, 1769–1776 (2011).
Matsuo, S. et al. Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis 53, 982–992 (2009).
Soga, T. et al. Quantitative metabolome analysis using capillary electrophoresis mass spectrometry. J Proteome Res 2, 488–494 (2003).
Hirayama, A., Igarashi, K., Tomita, M. & Soga, T. Development of quantitative method for determination of gamma-glutamyl peptides by capillary electrophoresis tandem mass spectrometry: an efficient approach avoiding matrix effect. J Chromatogr A 1369, 161–169 (2014).
Soga, T. et al. Metabolomic profiling of anionic metabolites by capillary electrophoresis mass spectrometry. Anal Chem 81, 6165–6174 (2009).
R Development Core Team. R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing. Vienna, Austria, 2005. http://www.R-project.org (12 Dec 2012, date last accessed).
Acknowledgements
We thank M. Ohishi, K. Endoh, S. Ohta for technical assistance, K. Ikemoto and K. Shibayama for secretary assistance, and the doctors and coworkers of the Department of Nephrology at Rinku General Medical Centre, Izumisano Municipal Hospital for clinical assistance. TK was supported from Manpei Suzuki Diabetes Foundation and Uehara Memorial Foundation. KY is a research fellow of Japan Society for the Promotion of Science.
Author information
Authors and Affiliations
Contributions
T.K. and T.H. designed research, K.Y. collected clinical data, T.K. and K.Y. performed statistical analysis, T.S. measured metabolites, H.R. and Y.I. provided scientific advice, and T.K., K.Y., R.Y. and Y.I. wrote the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Supplementary information
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Kimura, T., Yasuda, K., Yamamoto, R. et al. Identification of biomarkers for development of end-stage kidney disease in chronic kidney disease by metabolomic profiling. Sci Rep 6, 26138 (2016). https://doi.org/10.1038/srep26138
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep26138
- Springer Nature Limited
This article is cited by
-
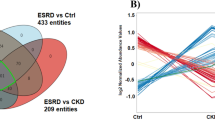
Metabolomics profiling distinctively identified end-stage renal disease patients from chronic kidney disease patients
Scientific Reports (2023)
-
Metabolomic Analysis Reveals the Adaptation in the P. przewalskii to Se-Deprived Environment
Biological Trace Element Research (2022)
-
DBnorm as an R package for the comparison and selection of appropriate statistical methods for batch effect correction in metabolomic studies
Scientific Reports (2021)
-
Data-dependent normalization strategies for untargeted metabolomics—a case study
Analytical and Bioanalytical Chemistry (2020)
-
Reverse translational research of autophagy and metabolism in kidney disease: Oshima Award Address 2018
Clinical and Experimental Nephrology (2019)