Abstract
Chinese medicine (CM) is major form of traditional and complementary medicine used by Chinese populations. Evaluation on patients’ experience on CM service is essential for improving service quality. This cross sectional study aims (i) to assess how CM clinics with different administrative model differ in terms of quality from patients’ perspective; and (ii) to investigate how quality varies with patients’ demographic and health characteristics. Five hundred and sixteen patients were sampled from charity and semi-public CM clinics in Hong Kong and were invited to assess their experience using the Primary Care Assessment Tool (PCAT). Results indicated that overall mean PCAT scoring is satisfactory, achieving 70.7% (91.26/129) of total score. Ratings were lower in areas of “coordination of patient information”, “continuity of care” and “range of service provided”. Impact of administrative models, including involvement of tax-funded healthcare system and outreach delivery, were minimal after adjusting for patient characteristics. Demographic and health characteristics of patients did not contribute to substantial variations in scoring. To improve patient experience, policy makers should consider strengthening care coordination, continuity and comprehensiveness in CM primary care services. Sharing of electronic records and establishing referral system are potential solutions for linking CM and conventional healthcare services.
Similar content being viewed by others
Introduction
In response to patients’ choice1 and emerging clinical evidence on traditional and complementary medicine (T & CM)2,3,4, the World Health Organization (WHO) is advocating the integration of T&CM into national health system in its Traditional Medicine Strategy 2014-20235. In many national health systems, conventional medicine is the dominant type of primary care practice and patients often obtain T&CM service from the private sector simultaneously, leading to fragmentation of care6. The provision of both conventional and T&CM within the same health services delivery infrastructure can ensure orchestrated delivery of both services7. Integrative delivery echoes suggestion from the 2008 World Health Report Primary Health Care – Now More than Ever, in which health systems are encouraged to consolidate modalities of healthcare horizontally across the community - including both formal and informal providers in public and private sectors8.
In Hong Kong, Chinese medicine (CM) is the major form of T&CM and its use is popular among chronic disease patients who are already receiving conventional care9. After the reunification of Hong Kong with China in 1997, the government has implemented development plans for CM as a fulfillment to constitutional mandate. Formal regulation on CM practitioners and Chinese herbal medicines are implemented and CM practitioners are positioned as a parallel profession to conventional medical doctor. Nevertheless, bridge building and interprofessional education between the two professions have been limited10. On the service provision side, initiatives in establishing CM service beyond the private sector has started a decade ago, but it is largely positioned outside the tax funded healthcare system11. The public healthcare system is managed by the Hospital Authority, which provides conventional medical services at various levels. On the other hand, non-governmental organizations (NGOs) are the main providers of charity and semi-public CM services12.
Charity and semi-public TCM services in Hong Kong
For non-profit charity service, NGOs manage two types of CM delivery models: (i) outpatient clinics (NGOs clinics) and (ii) mobile “clinics” which provide outreach CM services via fully equipped vans (mobile clinics). The NGOs are also actively involved in the provision of semi-public CM services by managing Clinical Centers for Teaching & Research in Chinese Medicine (CCTRCM). CCTRCM are established under the tripartite collaboration between NGOs, universities providing tertiary CM education, as well as the Hospital Authority. CCTRCM distinguish themselves from NGOs and mobile clinics as they have (i) formal linkages with the tax funded healthcare system13 and (ii) consultation fee waivers mechanism for patients receiving social security14 . Regardless of their management structure, all clinics provide three types of CM services: herbal medicine, acupuncture and massage therapy.
Aim of this study
Internationally, T&CM service provision within charity and semi-public setting is a relatively new endeavor in health systems with a dominant conventional care sector. Providing quality T&CM care is challenging especially in maintaining coordination and continuity of care across T&CM and conventional care sectors for chronic disease patients, especially those with multiple morbidities15. Little is known on how these new initiatives in Hong Kong are equipped to manage these challenges and also on how different administrative and service delivery models may affect quality of care. This study aims to assess patient’s experience of primary care provided by charity and semi-public CM clinics. The objectives were (i) to assess how CCTRCM, NGOs and mobile clinics differ in terms of quality from patients’ perspective; and (ii) to investigate how quality varies with patients’ demographic and health characteristics.
Methods
Sampling and Data Collection
This study was conducted in charity and semi-public CM clinics managed by a NGO in Hong Kong. Participants were selected using stratified sampling in three types of CM clinics mentioned above. These include five NGO clinics, eighteen mobile clinics and two CCTRCM. Following the sample size requirement of 20 subjects per independent variable in conducting multiple linear regression analysis16, we estimated that the required sample size would be 500. To ensure representative recruitment of patients, we sampled 167 patients from each type of clinic. Patients who were: (i) aged 18 or above, (ii) able to provide written informed consent, (iii) able to read and write Chinese without assistance were invited to participate. Specifically, we approached thirty-four patients from each of the 5 NGO clinics, ten patients from each of the 18 mobile clinics and eighty-three patients from each of 2 CCTRCM. In each clinic, all eligible service users invited to participate in a face to face interview immediately after consultation. We invited consecutive patients who attended the clinics until the required sample size was reached. Written informed consent was obtained from patients prior to the interview. The research protocol was approved by the Joint Chinese University of Hong Kong – New Territories East Cluster Clinical Research Ethics Committee (Reference number: CRE-2012.113). The methods were carried out in accordance with the guideline approved by the Committee.
Questionnaire Design
The questionnaire used in the interview consisted of two parts. The first part aimed to collect data on respondents’ demographic and health-related characteristics, including their gender, age, employment status, education level, marital status, housing type, payment status, reason for consultation, duration of waiting time and duration of consultation. We also queried on patients’ self-perceived health status using the validated question of: “In general, how would you rate your health?” [in Cantonese] with response options of excellent, very good, good, fair, or poor17.
In the second part, we assessed patients’ experience in CM service using by using the validated Primary Care Assessment Tool (PCAT) Adult edition short version instrument. The Chinese version used in this study was found to have good reliability and validity18.
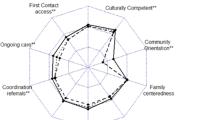
PCAT assesses patients’ experience in the following domains, which are to be key attributes of quality primary care services19: first contact accessibility and utilization, continuity of care, coordination of services and information system, comprehensiveness of services availability and provision, family centeredness, community orientation and cultural competence. Question items in each domain were rated on a 1 to 4 Likert scale. If a “not sure/cannot remember” option was chosen, scorings were imputed using method described in the statistical analysis section. Total score for each domain was calculated by summing (with reverse coding whenever appropriate) the values for all items within each domain. The overall PCAT score was derived by summing sores from each domain.
Statistical Analysis
Pearson’s Chi-square test was used to compare the socio-demographic and health related characteristics of patients in different healthcare settings. Variables with significant difference (p-value <0.15) were treated as potential confounder in the multiple regression analysis. There was 5.3% of missing values and 11.8% of “Don’t Know/Can’t Remember” options in the PCAT data and these were which imputed by the expectation-maximization (EM) algorithm with single imputation20. Subsequently, the domain and total scores of PCAT among different types of CM clinics were compared using multiple linear regression by adjusting patients’ demographic and health characteristics (independent variables included patients’ gender, age, education level, employment status, marital status, types of housing, self-perceived health status, Chinese Medicine specialty visited, reason for consultation and usage of conventional specialist services in public sector). Multiple linear regression analysis using full information maximum likelihood was performed to assess the association between PCAT total score and patients’ socio-demographic and health related characteristics20. Same regression model were used as sub-analyses for each PCAT domain score. Almost all patients from NGO or mobile clinics need to pay, but 30.7% patients sampled in the CCTRCM had their consultation fee waived. We conducted sensitivity analysis to study the potential influence of payment status on PCAT score by using CCTRCM data only. Statistical significance was set at p < 0.05. All analyses were performed using R version 2.15.221, in which the package OpenMx was used for multiple linear regression using full information maximum likelihood22,23.
Results
Characteristics of respondents
Table 1 presents the socio-demographic and health characteristics of 516 participants sampled from NGO clinics, mobile clinics and CCTRCM. The distribution of gender, age, education level, employment status, marital status, TCM specialty visited, reason for consultation, consultation payment and specialist visited experience differed significantly among three types of clinics, except for type of housing and self-perceived health status.
PCAT scorings
Results on PCAT score are reported in Table 2. Overall analysis of data from all three types of clinics showed that the PCAT total score is satisfactory, with a mean rating of 91.26 out of 129. In other words, rating achieved 70.7% of maximum possible score. Nevertheless, mean scorings in the domains of Continuity of Care (8.64 out of 16), Coordination (Information System) (6.79 out of 12), Comprehensiveness (Service provided) (12.43 out of 16) and Cultural Competence (6.11 out of 12) were lower. In these domains, ratings were below 60% of highest possible scores.
Comparison of PCAT score across CCTRCM, NGO and mobile clinics
Multiple linear regression analysis showed that, after adjusting for socio-demographic and health characteristics, all other PCAT domain scores and total score for NGO and mobile clinics differed significantly from that of CCTRCM clinics, except the first two domains in First Contact (Table 2). For Continuity of Care, CCTRCM had the highest mean score, while NGO clinics had the lowest mean score. Also, CCTRCM had higher score than that of the NGO and mobile clinics in the domain of Cultural Competence. However, when compared to CCTRCM users, both NGO and mobile clinic patients had slightly better experiences in the following domains: Coordination of Service, Coordination (information system), Comprehensiveness of Service Available and Provided, Family Centeredness and Community Orientation. Overall, NGO and mobile clinics scored slightly higher in total PCAT scores when compared to CCTRCM. The mean differences in PCAT total scores between CCTRCM and NGO / mobile clinics are less than 6 out of a total of 129, indicating that there is no substantial difference in patient experiences among the clinic types.
Association between PCAT scoring, clinic type and patients’ characteristics: Multiple linear regression analysis
Table 3 presents results from multiple linear regression analysis on total PCAT score, with clinic type as well as patients’ socio-economic and health characteristics as independent variables. Our results indicated that patients from NGO or mobile clinics reported a higher overall PCAT score when compared to those using CCTRCM. Retired patients rated a higher score than those who were employed. Magnitudes of associations described above were weak, as all the standardized β (adjusted) values are below 0.20. No other characteristics were found to be significantly associated with PCAT total score.
Association between PCAT scoring and patients’ characteristics in CCTRCM: Multiple linear regression analysis
Table 4 presents results from multiple linear regression analysis performed on data from CCTRCM, with payment of consultation fee as an extra independent variable. The results indicated that patients with primary education or below tended to rate their overall score lower than those received tertiary education. Unemployed patients rated a higher score than those who were employed. Compare to patients who consulted an herbalist, those who received acupuncture treatment reported a significantly lower score. Magnitudes of associations described above were weak, with standardized β (adjusted) values vary from 0.22 to 0.24.
Discussion
This is one of the first studies that evaluate patients’ experience of primary care provided by charity and semi-public CM clinics. While previous studies have reported poorer quality of conventional care received by Hong Kong patients with lower socioeconomic background16, in this CM focused study PCAT domain scores were largely similar across patients with different demographic characteristics. While the overall patient experience is satisfactory, ratings are lower in the three areas of “coordination of patient information”, “continuity of care” and “range of service provided”. Impact of administrative models on the results, including involvement of tax-funded healthcare system and outreach delivery, are minimal after adjusting for demographic and health characteristics of patients. When compared to a previous PCAT study that evaluated patients’ experiences in conventional public and private medical services in Hong Kong18, CM clinics fared worse than both public and private conventional care service in coordinating of patient information. For ensuring continuity of care, CM clinics were on par with public conventional clinics, but not with private primary care service. It can be speculated that lower PCAT score in CM clinics could be attributed to the lack of channels for communication and information sharing between the CM and conventional care sectors.
The need of improving information coordination and continuity across CM and conventional care
The PCAT domain of Coordination (information system) assesses three aspects: (i) readiness of patient record prior to consultation; (ii) patients’ right to examine their own record; and (iii) whether patients can own a copy of their record and bring it to the consultation. As the use of electronic health record systems is widespread in all three types of CM clinics, patients’ case notes are often ready at the consultation. Also, patients are allowed to read their record if requested. The main reason for lower score in this domain is patients’ difficulties in bringing their conventional care record to CM consultations. There is no formal referral system between CM and both public and private biomedical services24 except for certain selected diseases13. Communication across CM and conventional care providers using referral letters is uncommon. Even in CCTRCM where the Hospital Authority is involved, seamless electronic health record sharing between CM and tax-funded biomedical care are not in place. Responsibility of coordinating information flow across CM and conventional clinicians falls solely on the patients. In order to obtain their own CM and conventional health records, separate administrative fees must be paid in CM and conventional care settings respectively. The lack of communication channel with conventional health services, together with barriers for patients in obtaining their own records, has led to poor coordination of patient information in CM settings. As the government is promoting a territory wide sharing of electronic record system25, coordination of information across the two sectors may improve in the future. Unfortunately, there is no consensus between CM and conventional medicine stakeholders on whether patient record should be shared across disciplines26. Further policy research is needed for formulating informational sharing protocol that would be acceptable to both patients and professionals.
The PCAT domain of Continuity of Care assesses three aspects: (i) whether patients can consult the same CM clinician in every episode; (ii) whether patients can ask the same CM clinician questions with regards to their condition; and (iii) whether the CM clinician knows the patient well. It appears that private conventional care is performing better in these aspects. A common problem for both CM and public conventional care is that patients are often unable to see the same clinician and contacting clinician who manages their last consultation is usually not facilitated. This hinders continuity of care within CM or conventional care, not to mention fragmentation of care across two types of care27. The combined impact of poor information coordination and lack of continuity could pose risk to patients, especially when Chinese herbs and conventional drugs are prescribed by two clinicians without acknowledging each other28. For example, common Chinese herbs like Angelica sinensis or Salvia miltiorrhiza can potentiate the effect of warfarin, leading to excessive bleeding tendency among patients29. Potential threats of adverse herb-drug interaction demonstrate the need of improving coordination and continuity across CM and biomedical care at policy level30.
Beyond reducing the risk of herb-drug interaction, streamlining both services can also improve connectivity and trust between CM and biomedical clinicians. This is particularly important for policymakers who are interested in developing integrative model of care, which is gaining popularity internationally7. Successful collaboration between T&CM and conventional clinicians depends on timely information exchange and efficient referral platform. Shared electronic health record is a preferred channel for communication31,32,33 and face-to-face case conferences would further enhance the quality of coordination34. Co-location of CM and conventional clinicians is a potential strategy that can facilitate more frequent communications34,35,36. Nevertheless, these benefits cannot be reaped unless sufficient interprofessional education is provided for both types of clinicians37 and the potential legal barriers of patient record sharing across CM and biomedical clinicians are cleared38.
Building capacity in providing wider range of services: Resource implications for managing complex health needs
Our results indicated that scoring on the “service provided” domain is low and similar pattern is found in both public and private conventional care. Low level of advice provided on diet, sleep, exercise, smoking cessation, medication use, home safety and family conflict provided may be attributed to short consultation time available in Hong Kong, which lasts only 5–7 minutes per episode39. Current evidence suggests that primary care based health promotion can provide some benefits to patients40,42. To relieve burden from clinicians, it is recommended that these tasks can be delegated to other primary care team members41. The possibilities of using a coordinated, team based approach for addressing multiple health promotion needs in primary care setting should be explored, in both CM and biomedical care settings43.
Strengths and Weaknesses of This Study
One of the strengths of this study is that we reduced selection bias by using a stratified sampling strategy. This enabled us to recruit a representative sample of CM users from all three types of clinics. This study compared patients’ experience in CCTRCM, NGO and mobile clinics, of which each has different administrative and delivery model and we aimed at investigating the overall impact of such model. Involvement of the tax funded healthcare system and fee waiver mechanism for patients receiving social security are two distinctive features of CCTRCM. Our primary focus was not to investigate how each feature may influence patients’ experience. That said, to clarify that our findings, we performed a sensitivity analysis and showed that payment has no significant impact on patient experience in CCTRCM.
Meanwhile, this study has several limitations. First, attendees were asked to assess service quality within the CM clinic and thus social desirability bias could have led to inflation of score. Second, due to privacy reason, we were unable to obtain the full attendance lists of the clinics as a sampling frame. Therefore, we have chosen a non-probabilistic, consecutive sampling approach. The response rate for CCTRCM, NGO clinics and mobile clinics were 58.8%, 58.1% and 57.6% respectively. Since the response rate for all three types of clinics are similar, we do not expect significant self-selection bias introduced by patients who have positive preference on a particular style of service.
Lastly, in the discussion section, we have attempted to compare our results with findings on conventional care quality. This comparison should be considered preliminary as we did not sample patients who used both CM and conventional healthcare services. Future research should focus on evaluating the quality of information coordination and continuity among patients who consult both types of clinicians, which will provide direct evidence on whether the postulated differences between two types of care exists. Quantitative results from such investigation can be triangulated with qualitative findings, which will provide more policy relevant insights. For example, focus groups or in-depth interviews maybe conducted for exploring patients’ experiences in navigating both types of care, of which results can be translated to practical, patients centered strategies for integrative service re-design.
Conclusion
Quality of primary care provided by charity and semi-public CM clinics, assessed from patients’ perspective using PCAT, is satisfactory overall. However, there are rooms for improvement in the aspects of information coordination, continuity of care and range of health promotion and preventive service provided. Such weaknesses may be attributed to these clinics’ lack of connectivity with the conventional care sector. Exclusion of CM from the tax funded healthcare system also limited its role in delivering comprehensive care for patients who wish to use both types of services. Streamlining CM and conventional care, especially by sharing of electronic health record and establishing referral system, may improve quality of care. Policy makers should also consider the enhancement of CM sectors’ capacity in providing a more comprehensive range of services. Experience from Hong Kong can serve as a pioneering example for health systems which are considering the integration of T&CM and conventional care.
Additional Information
How to cite this article: Chung, V. C.H. et al. Patients’ experience of Chinese Medicine Primary Care Services: Implications on Improving Coordination and Continuity of Care. Sci. Rep. 5, 18853; doi: 10.1038/srep18853 (2015).
References
Chung, V. C. et al. Views on traditional Chinese medicine amongst Chinese population: a systematic review of qualitative and quantitative studies. Health Expectations, 17, 622–636, doi: 10.1111/j.1369-7625.2012.00794.x (2014).
Hempel, S., Taylor, S. L., Solloway, M. R., Miake-Lye, I. M. & Beroes, J. M., Evidence Map of Acupuncture. Washington (DC): Department of Veterans Affairs. (2014) Available at: http://www.ncbi.nlm.nih.gov/books/NBK185072/. (Accessed: 6th August 2015)
Park, C. & Mind-body C. A. M. interventions: current status and considerations for integration into clinical health psychology. J Clin Psychol. 69, 45–63, doi: 10.1002/jclp.21910 (2013).
Ernst, E. The efficacy of herbal medicine – an overview. Fundamental & Clinical Pharmacology. 19, 405–09, doi: 10.1111/j.1472-8206.2005.00335.x (2005).
Geneva: World Health Organization., WHO Traditional Medicine Strategy 2014-2023. Secondary WHO Traditional Medicine Strategy 2014–2023. (2013) Available at: http://apps.who.int/iris/bitstream/10665/92455/1/9789241506090_eng.pdf. (Accessed: 6th August 2015)
Geneva: World Health Organization., WHO Traditional Medicine Strategy: 2002-2005. Secondary WHO Traditional Medicine Strategy: 2002–2005. (2002) Available at: http://apps.who.int/medicinedocs/en/d/Js2297e/. (Accessed: 6th August 2015)
Chung, V. C., Ma, P. H., Hong, L. C. & Griffiths, S. M. Organizational determinants of interprofessional collaboration in integrative health care: systematic review of qualitative studies. PLoS One. 7, e50022, doi: 10.1371/journal.pone.0050022 (2012).
World Health Organization. In The World Health Report 2008: primary Health Care (now more than ever) (WHO, 2008)
Chung, V. C. H., Lau, C. H., Yeoh, E. K. & Griffiths, S. M. Age, chronic non-communicable disease and choice of traditional Chinese and western medicine outpatient services in a Chinese population. BMC Health Serv Res. 9, 207 (2009).
Griffiths, S. & Chung, V. Development and regulation of traditional Chinese medicine practitioners in Hong Kong. Perspect Public Health. 129, 64–7 (2009).
Griffiths, S., Chung, V. & Tang, J. L. Integrating Traditional Chinese Medicine: Experiences from China. Australasian Medical Journal. 3, 385–96, doi: 10.4066/AMJ.2010.411 (2010).
Hong Kong Special Administrative Region Goverment., Hong Kong : The facts (Public Health). Secondary Hong Kong: The facts (Public Health). (2013) Available at: http://www.gov.hk/en/about/abouthk/factsheets/docs/public_health.pdf. (Accessed: 6th August 2015)
Hospital Authority Chinese Medicine Service., Introduction to HA Chinese Medicine Service. Secondary Introduction to HA Chinese Medicine Service. (2012) Available at:http://www.ha.org.hk/chinesemedicine/intro.asp?lan=en. (Accessed: 6th August 2015)
Hong Kong Special Administrative Region Goverment., Press Releases. LCQ18: Public Chinese medicine clinics. (2007) Available at:http://www.info.gov.hk/gia/general/200706/20/P200706200162.htm(Accessed: 6th August 2015)
Jacobs, J. & Fisher, P. Polypharmacy, multimorbidity and the value of integrative medicine in public health. Eur J Integr Med. 5, 4–7, doi: 10.1016/j.eujim.2012.09.001 (2013).
Feinstein, A. In Multivariate analysis: an introduction New Haven, 226 (Yale University Press, 1996).
DeSalvo, K. B., Bloser, N., Reynolds, K., He, J. & Muntner, P. Mortality prediction with a single general self-rated health question. J Gen Intern Med. 21, 267–275 (2006).
Wong, S. Y. et al. Comparison of primary care experiences among adults in general outpatient clinics and private general practice clinics in Hong Kong. BMC Public Health. 10, 397, doi: 10.1186/1471-2458-10-397 (2010).
Shi, L., Starfield, B. & Xu, J. Validating the adult primary care assessment tool. J Fam Pract. 50, 161W–75W (2001).
Acock, A. C. Working With Missing Values. J Marriage Fam. 67, 1012–28, doi: 10.1111/j.1741-3737.2005.00191.x (2005).
The R Project for Statistical Computing. Secondary The R Project for Statistical Computing. (2015) Available at:http://www.r-project.org/. (Accessed: 6th August 2015)
Boker, S. et al. OpenMx: An Open Source Extended Structural Equation Modeling Framework. Psychometrika. 76, 306–17, doi: 10.1007/s11336-010-9200-6 (2011).
Boker, S. et al. OpenMx 1.3 user guide In Charlottesville (The OpenMx Project, 2012).
Chung, V. C. et al. Referral to and attitude towards traditional Chinese medicine amongst western medical doctors in postcolonial Hong Kong. Soc Sci Med. 72, 247–55, doi: 10.1016/j.socscimed.2010.10.021 (2011).
Goverment HKSAR., eHealth Record Office. Secondary eHealth Record Office. (2015) Available at:http://www.ehealth.gov.hk/en/home/index.html. (Accessed: 6th August 2015)
Chung, V. C., Ma, P. H., Lau, C. H. & Griffiths, S. M. Developing policy for integrating biomedicine and traditional chinese medical practice using focus groups and the delphi technique. Evid Based Complement Alternat Med. 2012, 149512, doi: 10.1155/2012/149512 (2012).
Liu, S. & Yeung, P. Measuring fragmentation of ambulatory care in a tripartite healthcare system. BMC Health Serv Res. 13, 176 (2013).
Posadzki, P., Watson, L. & Ernst, E. Herb–drug interactions: an overview of systematic reviews. Br J Clin Pharmacol. 75, 603–18, doi: 10.1111/j.1365-2125.2012.04350.x (2013).
Fugh-Berman, A. Herb-drug interactions. Lancet. 355, 134–8, doi: 10.1016/s0140-6736(99)06457-0 (2000).
Chung, V. C. H. et al. Do patients tell their clinicians they are using both prescribed and over the counter allopathic and traditional medicines? Eur J Integr Med. 3, e289–e98, doi: 10.1016/j.eujim.2011.09.008 (2011).
Grace, S. & Higgs, J. Interprofessional Collaborations in Integrative Medicine. J Altern Complem Med. 16, 1185–90, doi: 10.1089/acm.2009.0402 (2010).
Mior, S., Barnsley, J., Boon, H., Ashbury, F. D. & Haig, R. Designing a framework for the delivery of collaborative musculoskeletal care involving chiropractors and physicians in community-based primary care. J Interprof Care. 24, 678–89, doi: 10.3109/13561821003608757 (2010).
Allareddy, V. et al. Facilitators and barriers to improving interprofessional referral relationships between primary care physicians and chiropractors. J Ambul Care Manage. 30, 347 (2007).
Soklaridis, S., Greene, B. R., Smith, M., Haas, M. & Liao, J. Integrative health care in a hospital setting: Communication patterns between CAM and biomedical practitioners. J Interprof Care. 23, 655–67, doi: 10.3109/13561820902886287 (2009).
Vohra, S., Feldman, K., Johnston, B., Waters, K. & Boon, H. Integrating complementary and alternative medicine into academic medical centers: Experience and perceptions of nine leading centers in North America. BMC Health Serv Res. 5, doi: 10.1186/1472-6963-5-78 (2005).
Boon, H. S. & Kachan, N. Integrative medicine: a tale of two clinics. BMC Complement Altern Med. 8, doi: 10.1186/1472-6882-8-32 (2008).
Quartey, N. K., Ma, P. H., Chung, V. C. & Griffiths, S. M. Complementary and alternative medicine education for medical profession: systematic review. Evid Based Complement Alternat Med. 2012, 656812, doi: 10.1155/2012/656812 (2012).
Cohen, M. H. et al. Emerging credentialing practices, malpractice liability policies and guidelines governing complementary and alternative medical practices and dietary supplement recommendations: a descriptive study of 19 integrative health care centers in the United States. Arch Intern Med. 165, 289–95, doi: 10.1001/archinte.165.3.289 (2005).
Chung, V. C., Lau, C. H., Wong, E. M., Yeoh, E. K. & Griffiths, S. M. Perceived quality of communication amongst outpatients in western and traditional Chinese medicine clinics in a Chinese population. Health Policy. 90, 66–72, doi: 10.1016/j.healthpol.2008.09.005 (2009).
Todahl, J. & Walters, E. Universal Screening for Intimate Partner Violence: A Systematic Review. J Marital Fam Ther. 37, 355–69 (2011).
Noordman, J., van der Weijden, T. & van Dulmen, S. Communication-related behavior change techniques used in face-to-face lifestyle interventions in primary care: A systematic review of the literature. Patient Educ Couns. 89, 227–44 (2012).
Nakasato, Y. R. & Carnes, B. A. Health promotion in older adults. Promoting successful aging in primary care settings. Geriatrics. 61, 27–31 (2006).
Fernald, D. H. et al. Improving multiple health risk behaviors in primary care: lessons from the Prescription for Health Common Measures, Better Outcomes (COMBO) study. J Am Board Fam Med. 25, 701–11 (2012).
Acknowledgements
The authors would like to thank the anonymous NGO that facilitated the implementation of this study. This study is supported by Direct Grant for Research, Faculty of Medicine, Chinese University of Hong Kong (Reference number: 2010.2.057).
Author information
Authors and Affiliations
Contributions
V.C., S.G. and S.W. conceived the study and contributed to the writing of the manuscript. B.Y., E.Y. and X.Y.W. performed data analysis and provided statistical advice. S.Y.L. and R.H. designed and implemented the data collection plan. R.S., A.L. and J.W. provided critical comments to the design and implementation the study, as well as the manuscript.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Chung, V., Yip, B., Griffiths, S. et al. Patients’ experience of Chinese Medicine Primary Care Services: Implications on Improving Coordination and Continuity of Care. Sci Rep 5, 18853 (2015). https://doi.org/10.1038/srep18853
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep18853
- Springer Nature Limited
This article is cited by
-
Patients’ and clinicians’ expectations on integrative medicine Services for Diabetes: a focus group study
BMC Complementary Medicine and Therapies (2020)
-
Professionalism in traditional Chinese medicine (TCM) practitioners: a qualitative study
BMC Complementary Medicine and Therapies (2020)
-
Morbidity pattern of traditional Chinese medicine primary care in the Hong Kong population
Scientific Reports (2017)