Abstract
Data sources
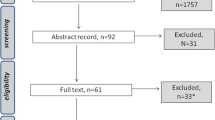
Several electronic databases were searched such as Cochrane Oral Health's Trials, Cochrane Library, Medline Ovid, CINAHL EBSCO and AMED Ovid and ongoing registered clinical trials in clinicaltrials.gov and in the World Health Organization International Clinical Trials Registry Platform. No restriction was placed on language and date of publication.
Study selection
The authors included randomised clinical trials (RCTs) and cross-over trials comparing any pharmacological intervention or any non-pharmacological agent with a control intervention.
Data extraction and synthesis
Two pairs of review authors independently and in duplicate assessed the quality of trials and extracted data.
Results
The review included ten trials (581 participants). Nine were included in the quantitative analysis. Three trials were assessed as having a low risk of bias, four at high risk of boas and three were assessed as unclear risk of bias. The studies included in the review were studies evaluating patients with taste disorders either idiopathic or resulting from zinc deficiency or chronic renal failure.
Nine trials compared zinc supplements to placebo for patients with taste disorders. The participants in two trials were children and adolescents with respective mean ages of ten and 11.2 years and the other seven trials had adult participants. Out of these nine, two trials of very low quality assessed the patient-reported outcome for improvement in taste acuity using zinc supplements (risk ratio (RR) 1.40, 95% confidence interval (CI) 0.94 to 2.09.
The meta-analyses of three trials classified as very low-quality evidence for taste acuity improvement in idiopathic and zinc-deficient taste disorder patients resulted in a standardised mean difference (SMD) = 0.44, (95% CI 0.23 to 0.65); 366 participants.
One cross-over trial using the first half of the results for taste detection (mean difference (MD) 2.50, 95% CI 0.93 to 4.07; 14 participants, very low-quality evidence), and taste recognition (MD 3.00, 95% CI 0.66 to 5.34; 14 participants, very low-quality evidence). The authors performed a meta-analysis for taste acuity improvement using objective outcome (dichotomous data) in idiopathic and zinc-deficient taste disorder patients (RR 1.42, 95% CI 1.09 to 1.84; 292 participants, two trials, very low-quality evidence). Out of the nine trials using zinc supplementation, four reported adverse events like eczema, nausea, abdominal pain, diarrhoea, constipation, decrease in blood iron, increase in blood alkaline phosphatase and minor increase in blood triglycerides.
One trial tested taste discrimination using acupuncture (MD 2.80, 95% CI −1.18 to 6.78; 37 participants, very low-quality evidence).
No adverse events were reported in the acupuncture trial.
Conclusions
The authors found very low-quality evidence that was insufficient to conclude on the role of zinc supplements to improve taste acuity reported by patients and very low-quality evidence that zinc supplements improve taste acuity in patients with zinc deficiency/idiopathic taste disorders. They could not find any evidence to conclude the role of zinc supplements for improving taste discrimination, or any evidence addressing health-related quality of life due to taste disorders.
Very low-quality evidence was found that is not sufficient to conclude on the role of acupuncture for improving taste discrimination in cases of idiopathic dysgeusia (distortion of taste) and hypogeusia (reduced ability to taste).
The authors were unable to draw any conclusions regarding the superiority of zinc supplements or acupuncture as none of the trials compared these interventions.
Similar content being viewed by others
Commentary
The objective of this systematic review published in The Cochrane Library was to assess zinc supplementation or acupuncture therapy in the treatment of zinc-deficient/idiopathic taste disorders and taste disorders secondary to chronic renal failure in children and adults.
Our sense of smell and taste function to protect us from harmful substances but also substantially contribute to our quality of life.1 Therefore, it is paramount that clinicians understand the implications when these senses are compromised. Zinc deficiency has been associated with disturbances in the gustatory and olfactory systems.2 As such, clinical studies have attempted to determine the therapeutic effects of zinc supplementation in patients who suffer from taste impairment. While there is clearly an interest in the treatment of taste disturbances, there is a gap in the current evidence to guide clinicians in their decision-making.
Improvement in taste acuity and taste discrimination were the primary outcomes assessed in this review which included parallel and cross-over randomised controlled trials (RCTs) with either a pharmacological or non-pharmacological intervention. Following systematic searches in electronic databases, data were extracted from ten RCTs of which nine were included in the review, with a combined total of 566 participants. Methodological parameters including risk of bias, units of analysis, missing data, blinding and allocation were addressed as they related to each of the included studies. Importantly, individual study results were clearly displayed and meta-analysis was sub-divided by a common primary reported outcome, shared by two or three of the included trials. Taste acuity improvement was quantified as a patient-reported outcome (two trials), an objective outcome recorded as a continuous variable (three trials) and as a dichotomous variable (three trials), with corresponding meta-analysis demonstrated in figures 3, 4 and 5 respectively. While there appears to be statistical significance in improvement of taste acuity when measured as an objective outcome, there appears to be no improvement when the analysis was based on the patients' reported outcome. While the current evidence is weak, the methodology of the review was appropriate in that it extracted data from RCTs. The authors' conclusions are founded in the data analysis and do not overestimate the effect of zinc supplementation.
Four trials had high risk of bias which impacted on the value of their reported evidence. Furthermore, the evidence in the studies was determined to be of low quality by the GRADE approach.3 As aforementioned, the trials analysed here reported low quality evidence rendering this review inherently weak, despite its thorough methodology. The authors illuminate that there remains a lack of high quality evidence that corroborates improvement in taste perception with zinc supplementation or acupuncture. Further clinical trials with low risk of bias, superior quality evidence and comparable variables are necessary to define the role of these therapeutic interventions in the treatment of taste disturbance. Until then, clinicians should consider that zinc supplementation may marginally improve taste acuity and it may be considered as a treatment option, however side effects such as nausea and abdominal pain should be considered.
References
Heckmann JG, Höcherl C, Dütsch M, Lang C, Schwab S, Hummel T . Smell and taste disorders in polyneuropathy: a prospective study of chemosensory disorders. Acta Neurol Scand 2009; 120: 258–263.
Takaoka T, Sarukura N, Ueda C, et al. Effects of zinc supplementation on serum zinc concentration and ratio of apo/holo-activities of angiotensin converting enzyme in patients with taste impairment. Auris Nasus Larynx 2010; 37: 190–194.
GRADEpro, G. D. T. GRADE Working Group, McMaster University. GRADEpro GDT. Version accessed 10 (2015).
Author information
Authors and Affiliations
Additional information
Address for correspondence: Luisa Fernandez Mauleffinch, Managing Editor, Cochrane Oral Health Group, School of Dentistry, The University of Manchester, JR Moore Building, Oxford Road, Manchester, M13 9PL, UK. E-mail: luisa.fernandez@manchester.ac.uk
Kumbargere Nagraj S, George RP, Shetty N, Levenson D, Ferraiolo DM, Shrestha A. Interventions for managing taste disturbances. Cochrane Database Syst Rev 2017; 12: Art. No.: CD010470. DOI: 10.1002/14651858.CD010470.pub3.
This paper is based on a Cochrane Review published in the Cochrane Library 2017, issue 12 (see www.thecochranelibrary.com for information). Cochrane Reviews are regularly updated as new evidence emerges and in response to feedback, and the Cochrane Library should be consulted for the most recent version of the review.
Rights and permissions
About this article
Cite this article
Michelson, M., Veitz-Keenan, A. Taste disturbances – are there any effective treatments?. Evid Based Dent 19, 60–61 (2018). https://doi.org/10.1038/sj.ebd.6401312
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ebd.6401312
- Springer Nature Limited