Abstract
Computational models can be applied to optimize treatment schedules and model treatment responses in cancer therapy. In this Review, we provide an overview of such computational approaches, including deterministic models, such as those based on ordinary and partial differential equations, stochastic models, spatially explicit agent-based approaches as well as control theory and machine learning methods. We discuss their advantages and current limitations in different scenarios. We outline how therapeutic decision-making can be aided by mathematical and computational approaches and how patient-specific responses can be assessed and incorporated into such methods. We also survey models that can incorporate adaptive changes throughout the course of treatment and discuss data and parameter estimation approaches. Finally, we highlight how such methods can lead to the identification of optimum treatment options for individual cancer and treatment types, and examine the challenges that remain to be addressed to enable the clinical translation of computational models in cancer therapy.
Key points
-
Computational approaches can be applied to describe the response of tumour cells to cancer treatment.
-
Such computational methods can be based on ordinary and partial differential equation modelling, stochastic modelling and spatially explicit agent-based models.
-
Adaptive treatment schedules and incorporation of patient-specific responses allow a personalized assessment of treatment options.
-
Control theory and machine learning methods, such as reinforcement learning, can be applied to design cancer treatment schedules.
-
Multimodal and longitudinal data sets could be integrated into patient-specific models to identify the best therapeutic options for individual patients.





Similar content being viewed by others
References
Jiang, P. et al. Big data in basic and translational cancer research. Nat. Rev. Cancer 22, 625–639 (2022).
Basu, A. et al. An interactive resource to identify cancer genetic and lineage dependencies targeted by small molecules. Cell 154, 1151–1161 (2013).
Van Allen, E. M. et al. Whole-exome sequencing and clinical interpretation of formalin-fixed, paraffin-embedded tumor samples to guide precision cancer medicine. Nat. Med. 20, 682–688 (2014).
Xue, J.-M., Liu, Y., Wan, L.-H. & Zhu, Y.-X. Comprehensive analysis of differential gene expression to identify common gene signatures in multiple cancers. Med. Sci. Monit. 26, e919953 (2020).
Song, Q. et al. Proteomic analysis reveals key differences between squamous cell carcinomas and adenocarcinomas across multiple tissues. Nat. Commun. 13, 4167 (2022).
Reznik, E. et al. A landscape of metabolic variation across tumor types. Cell Syst. 6, 301–313.e3 (2018).
Büttner, M., Miao, Z., Wolf, F. A., Teichmann, S. A. & Theis, F. J. A test metric for assessing single-cell RNA-seq batch correction. Nat. Methods 16, 43–49 (2019).
Sammut, S.-J. et al. Multi-omic machine learning predictor of breast cancer therapy response. Nature 601, 623–629 (2022).
Gallasch, R., Efremova, M., Charoentong, P., Hackl, H. & Trajanoski, Z. Mathematical models for translational and clinical oncology. J. Clin. Bioinform. 3, 23 (2013).
Altrock, P. M., Liu, L. L. & Michor, F. The mathematics of cancer: integrating quantitative models. Nat. Rev. Cancer 15, 730–745 (2015).
Foo, J. & Michor, F. Evolution of resistance to targeted anti-cancer therapies during continuous and pulsed administration strategies. PLoS Comput. Biol. 5, e1000557 (2009).
Yang, J., Lindström, H. J. G. & Friedman, R. Combating drug resistance in acute myeloid leukaemia by drug rotations: the effects of quizartinib and pexidartinib. Cancer Cell Int. 21, 198 (2021).
Poels, K. E. et al. Identification of optimal dosing schedules of dacomitinib and osimertinib for a phase I/II trial in advanced EGFR-mutant non-small cell lung cancer. Nat. Commun. 12, 3697 (2021).
Gatenby, R. A., Silva, A. S., Gillies, R. J. & Frieden, B. R. Adaptive therapy. Cancer Res. 69, 4894–4903 (2009).
Zhang, J., Cunningham, J. J., Brown, J. S. & Gatenby, R. A. Integrating evolutionary dynamics into treatment of metastatic castrate-resistant prostate cancer. Nat. Commun. 8, 1816 (2017).
Luria, S. E. & Delbrück, M. Mutations of bacteria from virus sensitivity to virus resistance. Genetics 28, 491–511 (1943).
Gardner, S. N. Modeling multi-drug chemotherapy: tailoring treatment to individuals. J. Theor. Biol. 214, 181–207 (2002).
Michelson, S. & Leith, J. T. Effects of differential cell kill on the dynamic composition of heterogeneous tumors. Comput. Math. Appl. 20, 149–159 (1990).
Leder, K. et al. Mathematical modeling of PDGF-driven glioblastoma reveals optimized radiation dosing schedules. Cell 156, 603–616 (2014).
Paryad-Zanjani, S., Saint-Antoine, M. M. & Singh, A. Optimal scheduling of therapy to delay cancer drug resistance. IFAC-Pap. 54, 239–244 (2021).
Lea, D. E. & Catcheside, D. G. The mechanism of the induction by radiation of chromosome aberrations in Tradescantia. J. Genet. 44, 216–245 (1942).
Pisco, A. O. et al. Non-Darwinian dynamics in therapy-induced cancer drug resistance. Nat. Commun. 4, 2467 (2013).
Greene, J. M., Gevertz, J. L. & Sontag, E. D. Mathematical approach to differentiate spontaneous and induced evolution to drug resistance during cancer treatment. JCO Clin. Cancer Inform. 3, 1–20 (2019).
Greene, J. M., Sanchez-Tapia, C. & Sontag, E. D. Mathematical details on a cancer resistance model. Front. Bioeng. Biotechnol. 8, 501 (2020).
Johnson, K. E. et al. Integrating transcriptomics and bulk time course data into a mathematical framework to describe and predict therapeutic resistance in cancer. Phys. Biol. 18, 016001 (2020).
Owolabi, K. M. & Shikongo, A. Mathematical modelling of multi-mutation and drug resistance model with fractional derivative. Alex. Eng. J. 59, 2291–2304 (2020).
Strobl, M. A. R. et al. Turnover modulates the need for a cost of resistance in adaptive therapy. Cancer Res. 81, 1135–1147 (2021).
Kim, E., Brown, J. S., Eroglu, Z. & Anderson, A. R. A. Adaptive therapy for metastatic melanoma: predictions from patient calibrated mathematical models. Cancers 13, 823 (2021).
Angelini, E., Wang, Y., Zhou, J. X., Qian, H. & Huang, S. A model for the intrinsic limit of cancer therapy: duality of treatment-induced cell death and treatment-induced stemness. PLoS Comput. Biol. 18, e1010319 (2022).
Fröhlich, F. et al. Efficient parameter estimation enables the prediction of drug response using a mechanistic pan-cancer pathway model. Cell Syst. 7, 567–579.e6 (2018).
Aghamiri, S. S., Amin, R. & Helikar, T. Recent applications of quantitative systems pharmacology and machine learning models across diseases. J. Pharmacokinet. Pharmacodyn. 49, 19–37 (2022).
Neftel, C. et al. An integrative model of cellular states, plasticity, and genetics for glioblastoma. Cell 178, 835–849.e21 (2019).
Shaffer, S. M. et al. Memory sequencing reveals heritable single-cell gene expression programs associated with distinct cellular behaviors. Cell 182, 947–959.e17 (2020).
Rambow, F., Marine, J.-C. & Goding, C. R. Melanoma plasticity and phenotypic diversity: therapeutic barriers and opportunities. Genes Dev. 33, 1295–1318 (2019).
Fukui, R. et al. Tumor radioresistance caused by radiation-induced changes of stem-like cell content and sub-lethal damage repair capability. Sci. Rep. 12, 1056 (2022).
Stein, S., Zhao, R., Haeno, H., Vivanco, I. & Michor, F. Mathematical modeling identifies optimum lapatinib dosing schedules for the treatment of glioblastoma patients. PLoS Comput. Biol. 14, e1005924 (2018).
Gillies, R. J., Verduzco, D. & Gatenby, R. A. Evolutionary dynamics of carcinogenesis and why targeted therapy does not work. Nat. Rev. Cancer 12, 487–493 (2012).
Smith, J. M. & Price, G. R. The logic of animal conflict. Nature 246, 15–18 (1973).
Basanta, D., Gatenby, R. A. & Anderson, A. R. A. Exploiting evolution to treat drug resistance: combination therapy and the double bind. Mol. Pharm. 9, 914–921 (2012).
Orlando, P. A., Gatenby, R. A. & Brown, J. S. Cancer treatment as a game: integrating evolutionary game theory into the optimal control of chemotherapy. Phys. Biol. 9, 065007 (2012).
West, J. B. et al. Multidrug cancer therapy in metastatic castrate-resistant prostate cancer: an evolution-based strategy. Clin. Cancer Res. 25, 4413–4421 (2019).
Gluzman, M., Scott, J. G. & Vladimirsky, A. Optimizing adaptive cancer therapy: dynamic programming and evolutionary game theory. Proc. Biol. Sci. 287, 20192454 (2020).
Stanková, K., Brown, J. S., Dalton, W. S. & Gatenby, R. A. Optimizing cancer treatment using game theory: a review. JAMA Oncol. 5, 96–103 (2019).
West, J. et al. Towards multidrug adaptive therapy. Cancer Res. 80, 1578–1589 (2020).
Roy, M. & Finley, S. D. Computational model predicts the effects of targeting cellular metabolism in pancreatic cancer. Front. Physiol. 8, 217 (2017).
Yu, L. et al. Modeling the genetic regulation of cancer metabolism: interplay between glycolysis and oxidative phosphorylation. Cancer Res. 77, 1564–1574 (2017).
Jia, D. et al. Elucidating cancer metabolic plasticity by coupling gene regulation with metabolic pathways. Proc. Natl Acad. Sci. USA 116, 3909–3918 (2019).
Shan, M., Dai, D., Vudem, A., Varner, J. D. & Stroock, A. D. Multi-scale computational study of the Warburg effect, reverse Warburg effect and glutamine addiction in solid tumors. PLoS Comput. Biol. 14, e1006584 (2018).
Li, W. & Wang, J. Uncovering the underlying mechanisms of cancer metabolism through the landscapes and probability flux quantifications. iScience 23, 101002 (2020).
Tripathi, S. et al. A mechanistic modeling framework reveals the key principles underlying tumor metabolism. PLoS Comput. Biol. 18, e1009841 (2022).
Vernieri, C. et al. Targeting cancer metabolism: dietary and pharmacologic interventions. Cancer Discov. 6, 1315–1333 (2016).
Stine, Z. E., Schug, Z. T., Salvino, J. M. & Dang, C. V. Targeting cancer metabolism in the era of precision oncology. Nat. Rev. Drug Discov. 21, 141–162 (2022).
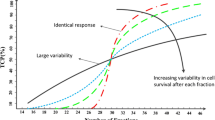
Sun, X., Bao, J. & Shao, Y. Mathematical modeling of therapy-induced cancer drug resistance: connecting cancer mechanisms to population survival rates. Sci. Rep. 6, 22498 (2016).
Jackson, T. L. & Byrne, H. M. A mathematical model to study the effects of drug resistance and vasculature on the response of solid tumors to chemotherapy. Math. Biosci. 164, 17–38 (2000).
Hamis, S., Nithiarasu, P. & Powathil, G. G. What does not kill a tumour may make it stronger: in silico insights into chemotherapeutic drug resistance. J. Theor. Biol. 454, 253–267 (2018).
Jain, R. K., Tong, R. T. & Munn, L. L. Effect of vascular normalization by antiangiogenic therapy on interstitial hypertension, peritumor edema, and lymphatic metastasis: insights from a mathematical model. Cancer Res. 67, 2729–2735 (2007).
Zheng, X. et al. A continuous model of angiogenesis: initiation, extension, and maturation of new blood vessels modulated by vascular endothelial growth factor, angiopoietins, platelet-derived growth factor-B, and pericytes. Discret. Contin. Dyn. Syst. B 18, 1109–1154 (2013).
Voutouri, C. et al. Experimental and computational analyses reveal dynamics of tumor vessel cooption and optimal treatment strategies. Proc. Natl Acad. Sci. USA 116, 2662–2671 (2019).
De Palma, M., Biziato, D. & Petrova, T. V. Microenvironmental regulation of tumour angiogenesis. Nat. Rev. Cancer 17, 457–474 (2017).
Lugano, R., Ramachandran, M. & Dimberg, A. Tumor angiogenesis: causes, consequences, challenges and opportunities. Cell. Mol. Life Sci. 77, 1745–1770 (2020).
Stylianopoulos, T. The solid mechanics of cancer and strategies for improved therapy. J. Biomech. Eng. 139, 4034991 (2017).
Sefidgar, M. et al. Numerical modeling of drug delivery in a dynamic solid tumor microvasculature. Microvasc. Res. 99, 43–56 (2015).
Arvanitis, C. D. et al. Mechanisms of enhanced drug delivery in brain metastases with focused ultrasound-induced blood–tumor barrier disruption. Proc. Natl Acad. Sci. USA 115, E8717–E8726 (2018).
Mainprize, T. et al. Blood–brain barrier opening in primary brain tumors with non-invasive MR-guided focused ultrasound: a clinical safety and feasibility study. Sci. Rep. 9, 321 (2019).
Ischenko, I., Seeliger, H., Schaffer, M., Jauch, K.-W. & Bruns, C. J. Cancer stem cells: how can we target them? Curr. Med. Chem. 15, 3171–3184 (2008).
Anderson, K. C. et al. The role of minimal residual disease testing in myeloma treatment selection and drug development: current value and future applications. Clin. Cancer Res. 23, 3980–3993 (2017).
da Silva-Diz, V., Lorenzo-Sanz, L., Bernat-Peguera, A., Lopez-Cerda, M. & Muñoz, P. Cancer cell plasticity: impact on tumor progression and therapy response. Semin. Cancer Biol. 53, 48–58 (2018).
Hinohara, K. et al. KDM5 histone demethylase activity links cellular transcriptomic heterogeneity to therapeutic resistance. Cancer Cell 34, 939–953.e9 (2018).
Kimmel, M. & Axelrod, D. E. Branching Processes in Biology (Springer, 2015).
Bozic, I. et al. Accumulation of driver and passenger mutations during tumor progression. Proc. Natl Acad. Sci. USA 107, 18545–18550 (2010).
Bauer, B., Siebert, R. & Traulsen, A. Cancer initiation with epistatic interactions between driver and passenger mutations. J. Theor. Biol. 358, 52–60 (2014).
Yakovlev, A. Y. & Yanev, N. M. Relative frequencies in multitype branching processes. Ann. Appl. Probab. 19, 1–14 (2009).
Roney, J. P., Ferlic, J., Michor, F. & McDonald, T. O. ESTIpop: a computational tool to simulate and estimate parameters for continuous-time Markov branching processes. Bioinformatics 36, 4372–4373 (2020).
Komarova, N. L. & Wodarz, D. Stochastic modeling of cellular colonies with quiescence: an application to drug resistance in cancer. Theor. Popul. Biol. 72, 523–538 (2007).
Chmielecki, J. et al. Optimization of dosing for EGFR-mutant non-small cell lung cancer with evolutionary cancer modeling. Sci. Transl Med. 3, 90ra59 (2011).
Yu, H. A. et al. Phase 1 study of twice weekly pulse dose and daily low-dose erlotinib as initial treatment for patients with EGFR-mutant lung cancers. Ann. Oncol. 28, 278–284 (2017).
Haeno, H. et al. Computational modeling of pancreatic cancer reveals kinetics of metastasis suggesting optimum treatment strategies. Cell 148, 362–375 (2012).
Lindström, H. J. G., de Wijn, A. S. & Friedman, R. Stochastic modelling of tyrosine kinase inhibitor rotation therapy in chronic myeloid leukaemia. BMC Cancer 19, 508 (2019).
Danesh, K., Durrett, R., Havrilesky, L. J. & Myers, E. A branching process model of ovarian cancer. J. Theor. Biol. 314, 10–15 (2012).
Dean, J., Goldberg, E. & Michor, F. Designing optimal allocations for cancer screening using queuing network models. PLoS Comput. Biol. 18, e1010179 (2022).
Chakrabarti, S. & Michor, F. Pharmacokinetics and drug interactions determine optimum combination strategies in computational models of cancer evolution. Cancer Res. 77, 3908–3921 (2017).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT03810807 (2023).
Baar, M. et al. A stochastic model for immunotherapy of cancer. Sci. Rep. 6, 24169 (2016).
Yamamoto, K. N. et al. Computational modeling of pancreatic cancer patients receiving FOLFIRINOX and gemcitabine-based therapies identifies optimum intervention strategies. PLoS ONE 14, e0215409 (2019).
Yamamoto, K. N., Liu, L. L., Nakamura, A., Haeno, H. & Michor, F. Stochastic evolution of pancreatic cancer metastases during logistic clonal expansion. JCO Clin. Cancer Inf. 3, 1–11 (2019).
Moran, P. A. P. The Statistical Processes Of Evolutionary Theory (Clarendon Press, 1962).
Michor, F., Iwasa, Y. & Nowak, M. A. Dynamics of cancer progression. Nat. Rev. Cancer 4, 197–205 (2004).
Beerenwinkel, N. et al. Genetic progression and the waiting time to cancer. PLoS Comput. Biol. 3, e225 (2007).
Park, J. & Newton, P. K. Stochastic competitive release and adaptive chemotherapy. Preprint at bioRxiv https://doi.org/10.1101/2022.06.17.496594 (2022).
Fischer, A., Vázquez-García, I. & Mustonen, V. The value of monitoring to control evolving populations. Proc. Natl Acad. Sci. USA 112, 1007–1012 (2015).
Chen, L., Yang, J., Tan, Y., Liu, Z. & Cheke, R. A. Threshold dynamics of a stochastic model of intermittent androgen deprivation therapy for prostate cancer. Commun. Nonlinear Sci. Numer. Simul. 100, 105856 (2021).
Camara, B. I., Mokrani, H., Diouf, A., Sané, I. & Diallo, A. S. Stochastic model analysis of cancer oncolytic virus therapy: estimation of the extinction mean times and their probabilities. Nonlinear Dyn. 107, 2819–2846 (2022).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT03557372 (2021).
Tanaka, G., Hirata, Y., Goldenberg, S. L., Bruchovsky, N. & Aihara, K. Mathematical modelling of prostate cancer growth and its application to hormone therapy. Phil. Trans. R. Soc. A 368, 5029–5044 (2010).
Albano, G., Giorno, V., Román-Román, P., Román-Román, S. & Torres-Ruiz, F. Estimating and determining the effect of a therapy on tumor dynamics by means of a modified Gompertz diffusion process. J. Theor. Biol. 364, 206–219 (2015).
Sfakianakis, N., Madzvamuse, A. & Chaplain, M. A. J. A hybrid multiscale model for cancer invasion of the extracellular matrix. Multiscale Model. Simul. 18, 824–850 (2020).
Mirams, G. R. et al. Chaste: an open source C++ library for computational physiology and biology. PLoS Comput. Biol. 9, e1002970 (2013).
Chamseddine, I. M. & Rejniak, K. A. Hybrid modeling frameworks of tumor development and treatment. Wiley Interdisc. Rev. Syst. Biol. Med. 12, e1461 (2020).
Olsen, M. M. & Siegelmann, H. T. Multiscale agent-based model of tumor angiogenesis. Proc. Comput. Sci. 18, 1016–1025 (2013).
Noble, R. et al. Spatial structure governs the mode of tumour evolution. Nat. Ecol. Evol. 6, 207–217 (2022).
Beerenwinkel, N., Schwarz, R. F., Gerstung, M. & Markowetz, F. Cancer evolution: mathematical models and computational inference. Syst. Biol. 64, e1–e25 (2015).
Swanton, C. Intratumor heterogeneity: evolution through space and time. Cancer Res. 72, 4875–4882 (2012).
Wu, H.-J. et al. Spatial intra-tumor heterogeneity is associated with survival of lung adenocarcinoma patients. Cell Genom. 2, 100165 (2022).
Zhang, L., Wang, Z., Sagotsky, J. A. & Deisboeck, T. S. Multiscale agent-based cancer modeling. J. Math. Biol. 58, 545–559 (2009).
Fusco, D., Gralka, M., Kayser, J., Anderson, A. & Hallatschek, O. Excess of mutational jackpot events in expanding populations revealed by spatial Luria–Delbrück experiments. Nat. Commun. 7, 12760 (2016).
Paterson, C., Nowak, M. A. & Waclaw, B. An exactly solvable, spatial model of mutation accumulation in cancer. Sci. Rep. 6, 39511 (2016).
Randles, A. et al. Computational modelling of perivascular-niche dynamics for the optimization of treatment schedules for glioblastoma. Nat. Biomed. Eng. 5, 346–359 (2021).
Waclaw, B. et al. A spatial model predicts that dispersal and cell turnover limit intratumour heterogeneity. Nature 525, 261–264 (2015).
Chkhaidze, K. et al. Spatially constrained tumour growth affects the patterns of clonal selection and neutral drift in cancer genomic data. PLoS Comput. Biol. 15, e1007243 (2019).
Liggett, T. M. Interacting Particle Systems (Springer, 2005).
Nicol, P. B., Barabási, D. L., Coombes, K. R. & Asiaee, A. SITH: an R package for visualizing and analyzing a spatial model of intratumor heterogeneity. Comput. Syst. Oncol. 2, e1033 (2022).
Angaroni, F. et al. J-SPACE: a Julia package for the simulation of spatial models of cancer evolution and of sequencing experiments. BMC Bioinformatics 23, 269 (2022).
Opasic, L., Scott, J., Traulsen, A. & Fortmann-Grote, C. CancerSim: a cancer simulation package for Python 3. J. Open Source Softw. 5, 2436 (2020).
Van Liedekerke, P., Palm, M. M., Jagiella, N. & Drasdo, D. Simulating tissue mechanics with agent-based models: concepts, perspectives and some novel results. Comp. Part. Mech. 2, 401–444 (2015).
van Leeuwen, I. M. M. et al. An integrative computational model for intestinal tissue renewal. Cell Prolif. 42, 617–636 (2009).
Ghaffarizadeh, A., Heiland, R., Friedman, S. H., Mumenthaler, S. M. & Macklin, P. PhysiCell: an open source physics-based cell simulator for 3-D multicellular systems. PLoS Comput. Biol. 14, e1005991 (2018).
Gallaher, J. A., Enriquez-Navas, P. M., Luddy, K. A., Gatenby, R. A. & Anderson, A. R. A. Spatial heterogeneity and evolutionary dynamics modulate time to recurrence in continuous and adaptive cancer therapies. Cancer Res. 78, 2127–2139 (2018).
Thomas, D. S., Cisneros, L. H., Anderson, A. R. A. & Maley, C. C. In silico investigations of multi-drug adaptive therapy protocols. Cancers 14, 2699 (2022).
Strobl, M. A. R. et al. Spatial structure impacts adaptive therapy by shaping intra-tumoral competition. Commun. Med. 2, 46 (2022).
Rejniak, K. A. & Anderson, A. R. A. Hybrid models of tumor growth. Wiley Interdisc. Rev. Syst. Biol. Med. 3, 115–125 (2011).
Bacevic, K. et al. Spatial competition constrains resistance to targeted cancer therapy. Nat. Commun. 8, 1995 (2017).
Bergman, D. et al. PhysiPKPD: a pharmacokinetics and pharmacodynamics module for PhysiCell. Gigabyte 2022, gigabyte72 (2022).
Almendro, V. et al. Inference of tumor evolution during chemotherapy by computational modeling and in situ analysis of genetic and phenotypic cellular diversity. Cell Rep. 6, 514–527 (2014).
Sutton, R. S. & Barto, A. G. Reinforcement Learning: An Introduction (MIT Press, 2018).
Schättler, H. M. & Ledzewicz, U. Optimal Control for Mathematical Models of Cancer Therapies: An Application of Geometric Methods (Springer, 2015).
Jarrett, A. M. et al. Optimal control theory for personalized therapeutic regimens in oncology: background, history, challenges, and opportunities. J. Clin. Med. 9, 1314 (2020).
Swan, G. W. & Vincent, T. L. Optimal control analysis in the chemotherapy of IgG multiple myeloma. Bull. Math. Biol. 39, 317–337 (1977).
Kuosmanen, T. et al. Drug-induced resistance evolution necessitates less aggressive treatment. PLoS Comput. Biol. 17, e1009418 (2021).
Jerez, S., Pliego, E., Solis, F. J. & Miller, A. K. Antigen receptor therapy in bone metastasis via optimal control for different human life stages. J. Math. Biol. 83, 44 (2021).
Hu, X., Ke, G. & Jang, S. R.-J. Modeling pancreatic cancer dynamics with immunotherapy. Bull. Math. Biol. 81, 1885–1915 (2019).
de Los Reyes, A. A. & Kim, Y. Optimal regulation of tumour-associated neutrophils in cancer progression. R. Soc. Open. Sci. 9, 210705 (2022).
Lee, T., Jenner, A. L., Kim, P. S. & Lee, J. Application of control theory in a delayed-infection and immune-evading oncolytic virotherapy. Math. Biosci. Eng. 17, 2361–2383 (2020).
Aspirin, A. P., de Los Reyes V, A. A. & Kim, Y. Polytherapeutic strategies with oncolytic virus-bortezomib and adjuvant NK cells in cancer treatment. J. R. Soc. Interf. 18, 20200669 (2021).
Anelone, A. J. N., Villa-Tamayo, M. F. & Rivadeneira, P. S. Oncolytic virus therapy benefits from control theory. R. Soc. Open. Sci. 7, 200473 (2020).
Cunningham, J. et al. Optimal control to reach eco-evolutionary stability in metastatic castrate-resistant prostate cancer. PLoS ONE 15, e0243386 (2020).
Wu, C. et al. Towards patient-specific optimization of neoadjuvant treatment protocols for breast cancer based on image-guided fluid dynamics. IEEE Trans. Biomed. Eng. 69, 3334–3344 (2022).
Angaroni, F. et al. An optimal control framework for the automated design of personalized cancer treatments. Front. Bioeng. Biotechnol. 8, 523 (2020).
Lee, J., Lee, D. & Kim, Y. Mathematical model of STAT signalling pathways in cancer development and optimal control approaches. R. Soc. Open Sci. 8, 210594 (2021).
Martin, R. B., Fisher, M. E., Minchin, R. F. & Teo, K. L. Optimal control of tumor size used to maximize survival time when cells are resistant to chemotherapy. Math. Biosci. 110, 201–219 (1992).
François-Lavet, V., Henderson, P., Islam, R., Bellemare, M. G. & Pineau, J. An introduction to deep reinforcement learning. Found. Trends Mach. Learn. 11, 219–354 (2018).
Engelhardt, D. Dynamic control of stochastic evolution: a deep reinforcement learning approach to adaptively targeting emergent drug resistance. J. Mach. Learn. Res. 21, 1–30 (2020).
Eastman, B., Przedborski, M. & Kohandel, M. Reinforcement learning derived chemotherapeutic schedules for robust patient-specific therapy. Sci. Rep. 11, 17882 (2021).
Ebrahimi Zade, A., Shahabi Haghighi, S. & Soltani, M. Deep neural networks for neuro-oncology: towards patient individualized design of chemo-radiation therapy for glioblastoma patients. J. Biomed. Inf. 127, 104006 (2022).
Moreau, G., François-Lavet, V., Desbordes, P. & Macq, B. Reinforcement learning for radiotherapy dose fractioning automation. Biomedicines 9, 214 (2021).
Tortora, M. et al. Deep reinforcement learning for fractionated radiotherapy in non-small cell lung carcinoma. Artif. Intell. Med. 119, 102137 (2021).
Yauney, G. & Shah, P. in Proc. 3rd Machine Learning Healthcare Conf. Vol. 85 161–226 (PMLR, 2018).
Padmanabhan, R., Meskin, N. & Haddad, W. M. Reinforcement learning-based control of drug dosing for cancer chemotherapy treatment. Math. Biosci. 293, 11–20 (2017).
Wang, M., Scott, J. G. & Vladimirsky, A. Stochastic optimal control to guide adaptive cancer therapy. Preprint at bioRxiv https://doi.org/10.1101/2022.06.17.496649 (2022).
Tseng, H.-H. et al. Deep reinforcement learning for automated radiation adaptation in lung cancer. Med. Phys. 44, 6690–6705 (2017).
Tardini, E. et al. Optimal treatment selection in sequential systemic and locoregional therapy of oropharyngeal squamous carcinomas: deep Q-learning with a patient–physician digital twin dyad. J. Med. Internet Res. 24, e29455 (2022).
Niraula, D., Jamaluddin, J., Matuszak, M. M., Haken, R. K. T. & Naqa, I. E. Quantum deep reinforcement learning for clinical decision support in oncology: application to adaptive radiotherapy. Sci. Rep. 11, 23545 (2021).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT02415621 (2023).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT03543969 (2023).
US National Library of Medicine. Pilot study of adaptive BRAF-MEK inhibitor therapy for advanced BRAF mutant melanoma. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT03543969 (2018).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT03630120 (2021).
Smalley, I. et al. Leveraging transcriptional dynamics to improve BRAF inhibitor responses in melanoma. EBioMedicine 48, 178–190 (2019).
Komorowski, M., Celi, L. A., Badawi, O., Gordon, A. C. & Faisal, A. A. The Artificial Intelligence Clinician learns optimal treatment strategies for sepsis in intensive care. Nat. Med. 24, 1716–1720 (2018).
Dean, J. A. et al. Phase I study of a novel glioblastoma radiation therapy schedule exploiting cell-state plasticity. Neuro Oncol. 25, 1100–1112 (2022).
Zhang, J. et al. A phase 1b adaptive androgen deprivation therapy trial in metastatic castration sensitive prostate cancer. J. Clin. Oncol. 40, 5075 (2022).
Acknowledgements
The authors gratefully acknowledge support from the Dana-Farber Cancer Institute’s Center for Cancer Evolution.
Author information
Authors and Affiliations
Contributions
All authors contributed equally to the preparation of this manuscript.
Corresponding author
Ethics declarations
Competing interests
F.M. is a co-founder of and has equity in Harbinger Health, has equity in Zephyr AI, serves as a consultant for Harbinger Health and Zephyr AI and is on the board of directors of Exscientia Plc. F.M. declares that none of these relationships are directly or indirectly related to the content of this manuscript. All other authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Bioengineering thanks Robert Noble, Blair Colyer and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
McDonald, T.O., Cheng, YC., Graser, C. et al. Computational approaches to modelling and optimizing cancer treatment. Nat Rev Bioeng 1, 695–711 (2023). https://doi.org/10.1038/s44222-023-00089-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s44222-023-00089-7
- Springer Nature Limited