Abstract
Background
Monogenic insulin resistance (IR) includes lipodystrophy and disorders of insulin signalling. We sought to assess the effects of interventions in monogenic IR, stratified by genetic aetiology.
Methods
Systematic review using PubMed, MEDLINE and Embase (1 January 1987 to 23 June 2021). Studies reporting individual-level effects of pharmacologic and/or surgical interventions in monogenic IR were eligible. Individual data were extracted and duplicates were removed. Outcomes were analysed for each gene and intervention, and in aggregate for partial, generalised and all lipodystrophy.
Results
10 non-randomised experimental studies, 8 case series, and 23 case reports meet inclusion criteria, all rated as having moderate or serious risk of bias. Metreleptin use is associated with the lowering of triglycerides and haemoglobin A1c (HbA1c) in all lipodystrophy (n = 111), partial (n = 71) and generalised lipodystrophy (n = 41), and in LMNA, PPARG, AGPAT2 or BSCL2 subgroups (n = 72,13,21 and 21 respectively). Body Mass Index (BMI) is lowered in partial and generalised lipodystrophy, and in LMNA or BSCL2, but not PPARG or AGPAT2 subgroups. Thiazolidinediones are associated with improved HbA1c and triglycerides in all lipodystrophy (n = 13), improved HbA1c in PPARG (n = 5), and improved triglycerides in LMNA (n = 7). In INSR-related IR, rhIGF-1, alone or with IGFBP3, is associated with improved HbA1c (n = 17). The small size or absence of other genotype-treatment combinations preclude firm conclusions.
Conclusions
The evidence guiding genotype-specific treatment of monogenic IR is of low to very low quality. Metreleptin and Thiazolidinediones appear to improve metabolic markers in lipodystrophy, and rhIGF-1 appears to lower HbA1c in INSR-related IR. For other interventions, there is insufficient evidence to assess efficacy and risks in aggregated lipodystrophy or genetic subgroups.
Plain language summary
The hormone insulin stimulates nutrient uptake from the bloodstream into tissues. In insulin resistance (IR), this action is blunted. Some rare gene alterations cause severe IR, diabetes that is difficult to control, and early complications. Many treatments have been suggested, but reliable evidence of their risks and benefits is sparse. We analysed all available reports describing treatment outcomes in severe IR. We found that the evidence is of low to very low quality overall. Injections of leptin, a hormone from fat tissue, or thiazolidinedione tablets that increase fat tissue both appear to improve diabetes control in people with reduced ability to make fat tissue. Injections of another treatment, insulin-like growth factor, appear to improve diabetes control in people with direct blockage of insulin action. There is a pressing need to improve evidence for treatment in these rare and severe conditions.
Similar content being viewed by others
Introduction
Diabetes caused by single gene changes is highly heterogeneous in molecular aetiopathogenesis. It may be grouped into disorders featuring primary failure of insulin secretion, and disorders in which insulin resistance (IR), often severe, predates secondary failure of insulin secretion and diabetes. Monogenic IR is itself heterogeneous, encompassing primary lipodystrophy syndromes, primary disorders of insulin signalling, and a group of conditions in which severe IR is part of a more complex developmental syndrome1.
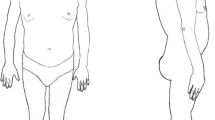
Monogenic IR is rare but underdiagnosed. The commonest subgroup is formed by genetic lipodystrophy syndromes2,3. A recent analysis of a large clinical care cohort unselected for metabolic disease suggested a clinical prevalence of lipodystrophy of around 1 in 20,000, with a prevalence of plausible lipodystrophy-causing genetic variants of around 1 in 70004. Monogenic IR is important to recognise, because affected patients are at risk not only of micro- and macrovascular complications of diabetes, but also of complications such as dyslipidemia, pancreatitis, and steatohepatitis, especially in lipodystrophy syndromes5. Non-metabolic complications specific to individual gene defects may also occur, including hypertrophic cardiomyopathy and other manifestations of soft tissue overgrowth3. Diabetes is also commonly the sentinel presentation of a multisystem disorder, and recognition of complex syndromes in a diabetes clinic may trigger definitive diagnostic testing.
The only therapy licensed specifically for monogenic IR is recombinant human methionyl leptin (metreleptin), with licensed indications encompassing a subset of patients with lipodystrophy and inadequate metabolic control. The current license in the USA is restricted to generalised lipodystrophy, but in Europe, it extends to some patients with partial lipodystrophy. A substantial proportion of the body of evidence considered in licensing addressed patients ascertained by the presence of clinical lipodystrophy, and the role of genetic stratification in the precision treatment of lipodystrophy has not been systematically addressed. Many other medications and other treatment options are also widely used in monogenic IR, although not licensed for that specific subgroup. Such use draws on the evidence base and treatment algorithms developed for type 2 diabetes. Several forms of monogenic IR have molecular and/or clinical attributes that suggest potential precision approaches to treatment.
We sought now to undertake a systematic review of the current evidence guiding the treatment of monogenic IR stratified by genetic aetiology, to assess evidence for differential responses to currently used therapies, to establish gaps in evidence, and to inform future studies. This systematic review is written on behalf of the American Diabetes Association (ADA)/European Association for the Study of Diabetes (EASD) Precision Medicine in Diabetes Initiative (PMDI) as part of a comprehensive evidence evaluation in support of the 2nd International Consensus Report on Precision Diabetes Medicine6. The PMDI was established in 2018 by the ADA in partnership with the EASD to address the burgeoning need for better diabetes prevention and care through precision medicine7.
Our analyses show that metreleptin and thiazolidinediones appear to lower HbA1c, triglycerides, and body weight in patients with lipodystrophy of all genotypes, and rhIGF-1 appears to lower HbA1c in patients with INSR-related IR. For other interventions, there is insufficient evidence to assess efficacy and risks.
Methods
Inclusion criteria and search methodology
To assess the treatment of severe IR of known monogenic aetiology, with or without diabetes mellitus, including generalised and partial lipodystrophy and genetic disorders of the insulin receptor, we developed, registered and followed a protocol for a systematic review (PROSPERO ID CRD42021265365; registered July 21, 2021)8. The study was reported in accordance with Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines. Filtering and selection of studies for data extraction were recorded using the Covidence platform (https://www.covidence.org, Melbourne, Australia).
We searched PubMed, MEDLINE and Embase from 1987 (the year before the identification of the first monogenic aetiology of IR) to June 23, 2021 for potentially relevant human studies in English. We used broad search terms designed to capture the heterogeneity of monogenic IR and its treatments. We searched for studies addressing 1. Severe IR due to variant(s) in a single gene OR 2. Congenital generalised or familial partial lipodystrophy due to variant(s) in a single gene. We selected only studies that reported a treatment term, including but not limited to the mention of 1. Thiazolidinediones (TZD), 2. Metreleptin, 3. SGLT2 inhibitors, 4. GLP-1 analogues, 5. Bariatric surgery (all types), 6. Recombinant human IGF-1 or IGF-1/IGFBP3 composite, 7. U-500 insulin. No interventions were excluded in the primary search. In addition to the automated search, we hand searched reference lists of relevant review articles. Given the rarity of monogenic IR, no study types were excluded in the initial search. We ultimately considered experimental studies, case reports, and case series. The full search strategy is described in Supplementary Table 1.
Study selection for data extraction was performed in two phases, namely primary screening of title and abstract, then full text review of potentially eligible articles. Two authors independently evaluated eligibility, with discrepancies resolved by a third investigator. We excluded publications without original data, such as reviews, editorials, and comments, and those solely addressing severe IR or lipodystrophy of unknown or known non-monogenic aetiology, including HIV-related or other acquired lipodystrophies, or autoimmune insulin receptoropathy (Type B insulin resistance). Studies in which no clear categorical or numerical outcome of an intervention was reported, or in which interventions were administered for less than 28 days were also excluded.
Data extraction and outcome assessments
One author extracted data from each eligible study using data extraction sheets. Data from each study was verified by 3 authors to reach a consensus. Data were extracted from text, tables, or figures. Study investigators were contacted for pertinent unreported data or additional details where possible, most commonly genetic aetiology of insulin resistance in reported patients, and outcome data.
Data extracted for each study included first author, publication year, country, details of intervention, duration of follow-up, study design, and number of participants. Subject-level data were extracted for outcomes of interest, including sex, genetic cause of severe insulin resistance (gene name, mono- vs biallelic INSR pathogenic variant), phenotypic details of severe IR/lipodystrophic subtype (generalised vs partial lipodystrophy; associated syndromic features). Subject level outcome data were extracted prior to and after the longest-reported exposure to the intervention of interest for haemoglobin A1c (A1c), body mass index, serum triglyceride, ALT, or AST concentration, any index of liver size or lipid content, and total daily insulin dose. Potential adverse effects of interventions were recorded, including urinary tract infection, genital candidiasis, hypoglycemia, excessive weight loss, pancreatitis, soft tissue overgrowth, and tumour formation.
Risk of bias and certainty of evidence assessment
The quality of extracted case reports and case series was assessed using NIH Study Quality Assessment Tools9 by a single reviewer and verified by 2 additional reviewers. Grading of the overall evidence for specific research questions was undertaken as detailed in10.
Statistics and reproducibility
Extracted data were managed using Covidence and analysed with SAS version 9.4. Pooled analysis was undertaken for all combinations of genotype and intervention for which sufficient numbers were reported, as well as for aggregated lipodystrophies, and generalized and partial subgroups of lipodystrophy. Generalized Estimating Equation models were used with time as a fixed factor and study as a random factor to examine treatment effects. Serum triglyceride concentrations were analyzed with and without log transformation. Data were summarized using estimated least-squared means with corresponding 95% confidence intervals.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Results
Identification of eligible studies
Initial searching identified 2933 studies, to which 117 were added from the bibliography reviews. 256 articles remained after the screening of titles and abstracts, and 44 after full text screening (Fig. 1).
Included studies addressed limited interventions and most had a high risk of bias
The 44 studies analysed and the assessment of their quality are summarised in Table 1 and detailed in Supplementary Data 1. Study quality was assessed as being fair in 15 cases and poor in 29 cases, including all case reports. This was primarily due to the high risk of bias, particularly related to the lack of a control group for all studies. Three of the 44 studies included in further analysis included only individuals already described in other reports and were discarded, leaving 41 studies for final analysis. These comprised 10 non-controlled experimental studies, 8 case series and 23 individual case reports (Table 1). No controlled trials were found. Individuals reported in the studies included 90 with partial lipodystrophy (72 due to LMNA mutation and 15 due to PPARG mutation), 42 with generalized lipodystrophy (21 AGPAT2, 21 BSCL2, 2 LMNA), and 19 with IR due to INSR mutation(s). Among the interventions described, only the responses to metreleptin (111 recipients), thiazolidinediones (13 recipients) and rhIGF-1 (alone or as a composite with IGFBP3) (17 recipients) were described in more than 5 cases (Table 1). This meant that for the large preponderance of possible genotype-treatment combinations no specific data were recovered (Supplementary Table 2). Full outcome data extracted are summarised in Supplementary Data 2, and subject-level data are shown in Supplementary Figures 1 through 8 with raw data provided in Supplementary Data 2.
Metreleptin treatment was associated with improved metabolic control in lipodystrophy
In our registered systematic review plan we posed several subquestions about treatment of monogenic IR subtypes that we felt were tractable. The first related to the risks and benefits (assessed by side effects, A1c, serum triglyceride concentration, body mass index (BMI), and indices of fatty liver) of metreleptin in patients with different monogenic subtypes of lipodystrophy. The response to metreleptin was described in 111 people (71 with partial lipodystrophy, 40 with generalized lipodystrophy)11,12,13,14,15,16,17,18,19,20,21,22,23. Metreleptin was administered for 19 ± 20 months (median 12, range 1–108) and was associated with lowering of A1c in aggregated lipodystrophy, in generalized and partial subgroups, and in all genetic subgroups for whom sufficient patients were reported, namely those with LMNA, PPARG, AGPAT2 and BSCL2 mutations (0.5 to 1.5% least square mean reduction) (Level 3 evidence, Supplementary Data 3, Fig. 2). Metreleptin treatment was also associated with lowering of serum triglyceride concentration in aggregated lipodystrophy, in generalized and partial subgroups, and in those with LMNA, PPARG, AGPAT2 and BSCL2 mutations (92 to 1760 mg/dL least square mean reduction for analyses of untransformed data) (Level 3 evidence, Supplementary Data 3, Fig. 2). BMI was lower after treatment in aggregated lipodystrophy, in generalized and partial subgroups, and in those with LMNA or BSCL2 mutations, but not PPARG or AGPAT2 mutations (Level 3 evidence, Supplementary Data 3, Fig. 2). Liver outcomes reported were too heterogeneous to analyse in aggregate. Only a single adverse event, namely hypoglycemia, was reported.
Least square mean change in (a) Hemoglobin A1c (A1c), (b) Log10 serum triglyceride concentration and (c) Body Mass Index (BMI) in patients with partial lipodystrophy, generalized lipodystrophy, all forms of lipodystrophy, and subgroups with PPARG, LMNA, BSCL2, and AGPAT2 mutations. Error bars represent 95% confidence intervals. N = 64, 38, 102, 12, 52, 17, and 20 for change in A1c in partial lipodystrophy, generalized lipodystrophy, all lipodystrophy, PPARG, LMNA, BSCL2, and AGPAT2-associated lipodystrophy, respectively. N = 66, 40, 106, 12, 54, 19, and 20 for change in log10 triglycerides in partial lipodystrophy, generalized lipodystrophy, all lipodystrophy, PPARG, LMNA, BSCL2, and AGPAT2-associated lipodystrophy, respectively. N = 47, 14, 61, 10, 35, 8, and 7 for change in BMI in partial lipodystrophy, generalized lipodystrophy, all lipodystrophy, PPARG, LMNA, BSCL2, and AGPAT2-associated lipodystrophy, respectively.
Thiazolidinedione treatment showed variable efficacy in limited studies
We next addressed the evidence of the risks and benefits of thiazolidinediones (TZDs) in patients with lipodystrophy. We were specifically interested in any evidence of a greater or lesser response in partial lipodystrophy caused by PPARG variants than in other lipodystrophy subtypes, as TZDs are potent ligands for the product of the PPARG gene, the master regulator of adipocyte differentiation. The response to TZDs was described in only 13 people, however (12 FPLD, 1 CGL)24,25,26,27,28,29,30,31,32,33,34. TZDs were administered for 29 ± 28 months (median 24, range 2–96). TZD use was associated with improved A1c in aggregated lipodystrophy (least square mean reduction 2.2%) and in PPARG-related but not LMNA-related partial lipodystrophy (Level 4 evidence, Supplementary Data 3, Fig. 3). Serum triglyceride concentration decreased in aggregated lipodystrophy and in those with LMNA-related but not PPARG-related partial lipodystrophy (Level 4 evidence, Supplementary Data 3, Fig. 3). No adverse events were reported.
Least square mean change in (a) Hemoglobin A1c (A1c), (b) Log10 serum triglyceride concentration and (c) Body Mass Index (BMI) in patients with partial lipodystrophy, generalized lipodystrophy, all forms of lipodystrophy, and subgroups with PPARG, and LMNA mutations. Error bars represent 95% confidence intervals. N = 5, 5, and 10 for change in A1c and change in log10 triglycerides in PPARG, LMNA, and all lipodystrophy, respectively. N = 1, 5, and 6 for change in BMI in PPARG, LMNA, and all lipodystrophy, respectively.
rhIGF-1 treatment in INSR-related IR was associated with improvement in A1c
Our last specific question related to the risks (e.g. tumours, hypoglycemia, cardiac hypertrophy, other soft tissue overgrowth) and benefits (assessed by A1c) of recombinant human IGF-1 (rhIGF-1) or IGF-1/IGFBP3 composite in patients with pathogenic INSR variants. The response to rhIGF-1 was described in 17 people with pathogenic INSR variants for a mean of 45 ± 81 months (median 9, range 1–288)35,36,37,38,39,40,41,42,43,44,45,46. In INSR-related IR, we found that use of rhIGF-1, alone or as a composite with IGFBP3, was associated with improvement in A1c, and this was true also in subgroups with monoallelic and biallelic variants (1.5 to 2% least square mean reduction, Level 4 evidence, Supplementary Data 3, Fig. 4). One instance of increased soft tissue overgrowth and two episodes of hypoglycemia was reported.
Many questions about genotype-stratified treatment were not addressed
While many other interesting and clinically relevant questions arise about other potential genotype-specific responses to therapy in monogenic IR, the small size or absence of other genotype by treatment groups precluded the drawing of conclusions about risks and benefits, including for very widely used medications such as metformin26,47,48,49, newer agents commonly used in type 2 diabetes including SGLT2 inhibitors50,51 and GLP-1 agonists, and non pharmacologic interventions such as bariatric surgery52,53,54.
Discussion
Thirty-five years since INSR mutations were identified in extreme IR55,56, and 23 years since the first monogenic cause of lipodystrophy was reported57, many different forms of monogenic IR are known1,2,3,58. These are associated with substantial early morbidity and mortality, ranging from death in infancy to accelerated complications of diabetes and fatty liver disease in adulthood, depending on the genetic subtype. Several opportunities for genotype-guided, targeted treatment are suggested by the causal genes, and so we set out to review the current evidence guiding the treatment of monogenic IR stratified by genetic aetiology. We found a paucity of high-quality evidence (all levels 3 to 4). No controlled trials of any intervention were identified, and there was substantial heterogeneity of study populations and intervention regimens, even for the same interventional agent.
The evidence which we did find, from a small number of uncontrolled experimental studies, augmented by case series and numerous case reports, suggests that metreleptin offers metabolic benefits across different lipodystrophy subtypes, in keeping with its licensing for use in some patients with lipodystrophy in both Europe and the USA. Notably, the evidence base considered by licensing authorities was larger than the one we present, including many studies of phenotypically ascertained lipodystrophy that included acquired or idiopathic disease. In contrast, we have addressed solely individuals with lipodystrophy caused by variation in a single gene. The limited data we identified do not clearly support differential effects among different monogenic lipodystrophy subgroups, but for many subtypes numbers reported are very small. Moreover, although responses appear comparable for partial and generalised lipodystrophy, this is highly likely to reflect selection bias in studies of partial lipodystrophy towards those with more severe metabolic complications and lower baseline serum leptin concentrations.
A clear opportunity for precision diabetes therapy in monogenic IR is offered by the IR and lipodystrophy caused by mutations in PPARG, which encodes the target for thiazolidinediones (TZDs) such as pioglitazone59,60. PPARG is a nuclear receptor that serves as the master transcriptional driver of adipocyte differentiation, and so as soon as PPARG mutations were identified to cause severe IR, there was interest in the potential of TZDs as specific treatments. Although we found small scale evidence supporting greater A1c reduction with TZDs in PPARG vs. LMNA-related lipodystrophy, only 5 patients with PPARG-related lipodystrophy in whom TZD effects were clearly described were reported, and responses were inconsistent. Thus, it remains unclear whether people with IR due to PPARG variants are more or indeed less sensitive to TZDs than people with other forms of lipodystrophy. Loss-of-function PPARG mutations are the second commonest cause of familial partial lipodystrophy2, and the function of coding missense variants in PPARG has been assayed systematically to accelerate genetic diagnosis61, so the opportunity to test genotype-related therapy in PPARG-related IR seems particularly tractable in future.
Other obvious questions about the targeted treatment of monogenic, lipodystrophic IR are not addressed by current evidence. Important examples relate to the risks and benefits of treatments used in type 2 diabetes such as GLP-1 agonists and SGLT2 inhibitors. It is rational to suppose that these medications, which decrease weight as well as improve glycaemia in those with raised BMI and diabetes, may also be efficacious in lipodystrophy even where BMI is normal or only slightly raised. This is because in both situations adipose storage capacity is exceeded, leading to fat failure. It is the offloading of overloaded adipose tissue, rather than the baseline BMI/adipose mass, which underlies the efficacy of therapy. However, GLP-1 agonists are contraindicated in those with prior pancreatitis, while SGLT2 inhibitor use can be complicated by diabetic ketoacidosis. In untreated lipodystrophy pancreatitis is common, yet this is due to hypertriglyceridaemia, which is likely to be improved by GLP-1 agonist use, while excessive supply of free fatty acids to the liver may promote ketogenesis. Thus, assessment of both classes of drugs in lipodystrophy and its genetic subgroups will be important to quantify risks and benefits, which may be distinct from those in obesity-related diabetes.
A further question we prespecified related to the use of rhIGF1 in people with severe IR due to INSR mutations. This use of rhIGF-1 was first described in recessive INSR defects in the early 1990s44, and several studies of rhIGF-1 therapy of duration less than 28 days in people with INSR mutations have provided proof of concept for acute metabolic benefits (summarized in38). This use of rhIGF-1 is based on the rationale that IGF-1 activates a receptor and signalling pathway very closely similar to those activated by insulin. Based on case reports, case series and narrative reviews, rhIGF-1 is now commonly used in neonates with extreme IR due to biallelic INSR mutations, although, unlike metreleptin in lipodystrophy, this use is still unlicensed. Our review of published data, which was limited to durations of intervention greater than 28 days, is consistent with glycaemic benefits of rhIGF-1, alone or in composite form with its binding protein IGFBP3, in people with INSR mutations. Nevertheless, such studies are challenging to interpret and are potentially fraught with bias of different types, particularly publication bias favouring positive outcomes. Responses to rhIGF1 are also challenging to determine in uncontrolled studies as small differences in the residual function of mutated receptors can have substantial effects on the severity and natural history of the resulting IR, yet relatively few INSR mutations have been studied functionally. This underlines the narrow nature of, and substantial residual uncertainty in, the evidence base for the use of rhIGF-1 in monogenic IR.
There are several reasons why important questions about the precision treatment of monogenic IR have not been settled. Although severe autosomal recessive IR is usually detected in infancy, commoner dominant forms of monogenic IR are often diagnosed relatively late, often only after years of management based on presumptive diagnoses of type 2 or sometimes type 1 diabetes. Initial management as type 2 diabetes means that by the time a clinical and then genetic diagnosis is made, most patents have been treated with agents such as metformin, and increasingly SGLT2 inhibitors or GLP-1 agonists, outside trial settings. It is not clear that harm is caused by such use of drugs with well-established safety profiles and efficacy in type 2 diabetes, but the lack of systematic data gathering precludes the identification of specific drug-genotype interactions. Moreover, because attempts to gather evidence for monogenic IR treatment have tended to focus on high-cost adjunctive therapies such as metreleptin, the evidence base for their use is better developed, although controlled trials are lacking. Licensing of high-cost treatments such as metreleptin in lipodystrophy, while effects of many more commonly used, cheaper drugs with well-established safety profiles lack formal testing in monogenic IR is potentially problematic, skewing incentives and guidelines towards expensive therapy before optimal treatment algorithms have been established.
Other challenges in conducting trials in monogenic IR arise from the exquisite sensitivity of IR to exacerbating factors such as puberty, diet, and energy balance. This creates a signal to noise problem particularly problematic in uncontrolled studies, in which non-pharmacological components of interventions such as increased support for behavioural change may confound attribution of beneficial outcomes to pharmacological agents tested.
The key question now is how the evidence base for managing monogenic severe IR can be improved in the face of constraints in studying rare, clinically heterogeneous, and geographically dispersed patients who are often diagnosed late with a condition that is exquisitely environmentally sensitive. Growing interest in and development of methodologies for clinical trials in rare disease62, including Bayesian methodologies63,64, and hybrid single- and multi-site designs65 offer hope for future filling of evidence gaps. One important and pragmatic opportunity arises from the development of large regional, national and international networks and registries for lipodystrophy (e.g. the Europe-based ECLip registry66), allied to emergence of randomised registry-based trial (RRT) methodology67,68. RRTs have attracted increasing interest in several disease areas and are particularly suitable for evaluation of agents with well-established safety profiles. When a simple randomisation tool is deployed in the context of a registry, RRTs can offer rapid, cost-effective recruitment and high external validity (i.e. relevance to real world practice). In monogenic IR this would permit questions to be addressed about optimal usage of different common medications in different genetic subgroups, including the order of introduction of therapies, and their optimal combinations. The quality of such studies will critically rely on good registry design and quality and completeness of data capture67,68.
In summary, severe monogenic IR syndromes are clinically and genetically heterogeneous, with high early morbidity and mortality. However, despite opportunities for targeted therapy of some monogenic subgroups based on the nature of the causal gene alteration, the evidence for genotype-stratified therapy is weak. This is in part because of the rarity and frequent late diagnosis of monogenic IR, but also because therapeutic research to date has focused largely on phenotypically ascertained cross cutting diagnoses such as lipodystrophy. We suggest that approaches such as RRTs hold the best hope to answer some of the persisting major questions about precision treatment in monogenic IR.
Data availability
All data used in this review is available from publicly available and herein referenced sources. A list of included studies is provided in Supplementary Data 1. All data generated or analyzed during this study are included in this published article and its supplementary information files. Source data for the figures are available as Supplementary Data 2.
Change history
26 March 2024
A Correction to this paper has been published: https://doi.org/10.1038/s43856-024-00482-2
References
Bonnefond, A. & Semple, R. K. Achievements, prospects and challenges in precision care for monogenic insulin-deficient and insulin-resistant diabetes. Diabetologia 65, 1782–1795 (2022).
Lim, K., Haider, A., Adams, C., Sleigh, A. & Savage, D. B. Lipodistrophy: a paradigm for understanding the consequences of “overloading” adipose tissue. Physiol. Rev. 101, 907–993 (2021).
Semple, R. K., Savage, D. B., Cochran, E. K., Gorden, P. & O’Rahilly, S. Genetic syndromes of severe insulin resistance. Endocr. Rev. 32, 498–514 (2011).
Gonzaga-Jauregui, C. et al. Clinical and molecular prevalence of lipodystrophy in an unascertained large clinical care cohort. Diabetes 69, 249–258 (2020).
Brown, R. J. et al. The diagnosis and management of lipodystrophy syndromes: a multi-society practice guideline. J. Clin. Endocrinol. Metab. 101, 4500–4511 (2016).
Deirdre, K. et al. Second international consensus report on gaps and opportunities for the clinical translation of precision diabetes medicine. Nat. Med. In press https://doi.org/10.1038/s41591-023-02502-5 (2023).
Nolan, J. J. et al. ADA/EASD precision medicine in diabetes initiative: an international perspective and future vision for precision medicine in diabetes. Diabetes Care 45, 261–266 (2022).
Effects of pharmacologic and non-pharmacologic interventions on metabolic control in severe insulin resistance due to lipodystrophy or genetic insulin receptoropathy, https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=265365 (2021).
Study Quality Assessment Tools, https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools
Sherifali, D. et al. Methods. Can. J. Diabetes 42, S6–S9 (2018).
Musso, C., Major, M. L., Andres, E. & Simha, V. Metreleptin treatment in three patients with generalized lipodystrophy. Clin. Med. Insights Case Rep. 9, 123–127 (2016).
Beltrand, J. et al. Resistance to leptin-replacement therapy in Berardinelli-Seip congenital lipodystrophy: an immunological origin. Eur. J. Endocrinol. 162, 1083–1091 (2010).
Vatier, C. et al. Adherence with metreleptin therapy and health self-perception in patients with lipodystrophic syndromes. Orphanet. J. Rare Dis. 14, 177 (2019).
Beltrand, J. et al. Metabolic correction induced by leptin replacement treatment in young children with Berardinelli-Seip congenital lipoatrophy. Pediatrics 120, e291–e296 (2007).
Chong, A. Y., Lupsa, B. C., Cochran, E. K. & Gorden, P. Efficacy of leptin therapy in the different forms of human lipodystrophy. Diabetologia 53, 27–35 (2010).
Maeda, M., Maeda, T., Ebihara, K. & Ihara, K. The long-term management of congenital generalized lipodystrophy (Berardinelli-Seip syndrome): the clinical manifestations of Japanese siblings for approximately 20 years. Clin. Pediatr. Endocrinol.: Case Rep. Clin. Invest.: Off. J. Jpn Soc. Pediatr. Endocrinol. 28, 139–145 (2019).
Ebihara, K. et al. Efficacy and safety of leptin-replacement therapy and possible mechanisms of leptin actions in patients with generalized lipodystrophy. J. Clin. Endocrinol. Metab. 92, 532–541 (2007).
Ajluni, N., Dar, M., Xu, J., Neidert, A. H. & Oral, E. A. Efficacy and safety of metreleptin in patients with partial lipodystrophy: lessons from an expanded access program. J. Diabetes Metabol. 7 https://doi.org/10.4172/2155-6156.1000659 (2016).
Sekizkardes, H., Cochran, E., Malandrino, N., Garg, A. & Brown, R. J. Efficacy of metreleptin treatment in familial partial lipodystrophy due to PPARG vs LMNA pathogenic variants. J. Clin. Endocrinol. Metab. 104, 3068–3076 (2019).
Simha, V. et al. Comparison of efficacy and safety of leptin replacement therapy in moderately and severely hypoleptinemic patients with familial partial lipodystrophy of the Dunnigan variety. J. Clin. Endocrinol. Metab. 97, 785–792 (2012).
Takeyari, S. et al. Metreleptin treatment for congenital generalized lipodystrophy type 4 (CGL4): a case report. Clin. Pediatr. Endocrinol.: Case Rep. Clin Investigations: Off. J. Jpn Soc. Pediatr. Endocrinol. 28, 1–7 (2019).
Oral, E. A. et al. Leptin-replacement therapy for lipodystrophy. N. Engl. J. Med. 346, 570–578 (2002).
Park, J. Y., Javor, E. D., Cochran, E. K., DePaoli, A. M. & Gorden, P. Long-term efficacy of leptin replacement in patients with Dunnigan-type familial partial lipodystrophy. Metabolism 56, 508–516 (2007).
Chaves, C., Chaves, M., Anselmo, J. & César, R. Successful long-term use of pioglitazone in Berardinelli-Seip lipodystrophy-associated diabetes. Endocrinol. Diabetes Metab. Case Rep. 2021 https://doi.org/10.1530/edm-20-0183 (2021).
Collet-Gaudillat, C., Billon-Bancel, A. & Beressi, J. P. Long-term improvement of metabolic control with pioglitazone in a woman with diabetes mellitus related to Dunnigan syndrome: a case report. Diabetes Metab. 35, 151–154 (2009).
Gambineri, A. et al. Monogenic polycystic ovary syndrome due to a mutation in the lamin A/C gene is sensitive to thiazolidinediones but not to metformin. Eur. J. Endocrinol. 159, 347–353 (2008).
Moreau, F. et al. Efficacy of pioglitazone in familial partial lipodystrophy of the Dunnigan type: a case report. Diabetes Metab. 33, 385–389 (2007).
Owen, K. R., Donohoe, M., Ellard, S. & Hattersley, A. T. Response to treatment with rosiglitazone in familial partial lipodystrophy due to a mutation in the LMNA gene. Diabetes Med. 20, 823–827 (2003).
Simha, V., Rao, S. & Garg, A. Prolonged thiazolidinedione therapy does not reverse fat loss in patients with familial partial lipodystrophy, Dunnigan variety. Diabetes Obes. Metab. 10, 1275–1276 (2008).
Luedtke, A. et al. Thiazolidinedione response in familial lipodystrophy patients with LMNA mutations: a case series. Horm. Metab. Res. 44, 306–311 (2012).
Agostini, M. et al. A pharmacogenetic approach to the treatment of patients with PPARG mutations. Diabetes 67, 1086–1092 (2018).
Francis, G. A. et al. Peroxisomal proliferator activated receptor-gamma deficiency in a Canadian kindred with familial partial lipodystrophy type 3 (FPLD3). BMC Med. Genet. 7, 3 (2006).
Savage, D. B. et al. Human metabolic syndrome resulting from dominant-negative mutations in the nuclear receptor peroxisome proliferator-activated receptor-gamma. Diabetes 52, 910–917 (2003).
Lüdtke, A. et al. Long-term treatment experience in a subject with Dunnigan-type familial partial lipodystrophy: efficacy of rosiglitazone. Diabetes Med. 22, 1611–1613 (2005).
Hashimoto, N. et al. A case of type A insulin resistance associated with heterozygous Asn462Ser mutation of the insulin receptor gene. Diabetol. Int. 3, 239–243 (2012).
Jo, W. et al. Development of endometrial carcinoma in a patient with leprechaunism (donohue syndrome). Clin. Pediatr. Endocrinol.: Case Rep. Clin. Invest.: Off. J. Jpn Soc. Pediatr. Endocrinol. 22, 33–38 (2013).
Perge, K. et al. Intrauterine growth restriction and hypertrophic cardiomyopathy as prenatal ultrasound findings in a case of leprechaunism. Mol. Syndromol. 11, 223–227 (2020).
Plamper, M., Gohlke, B., Schreiner, F. & Woelfle, J. Mecasermin in insulin receptor-related severe insulin resistance syndromes: case report and review of the literature. Int. J. Mol. Sci. 19 https://doi.org/10.3390/ijms19051268 (2018).
Carmody, D., Ladsaria, S. S., Buikema, R. K., Semple, R. K. & Greeley, S. A. Successful rhIGF1 treatment for over 5 years in a patient with severe insulin resistance due to homozygous insulin receptor mutation. Diabetes Med. 33, e8–e12 (2016).
de Kerdanet, M. et al. Ten-year improvement of insulin resistance and growth with recombinant human insulin-like growth factor 1 in a patient with insulin receptor mutations resulting in leprechaunism. Diabetes Metab. 41, 331–337 (2015).
Weber, D. R., Stanescu, D. E., Semple, R., Holland, C. & Magge, S. N. Continuous subcutaneous IGF-1 therapy via insulin pump in a patient with Donohue syndrome. J. Pediatr. Endocrinol. Metab. 27, 1237–1241 (2014).
Regan, F. M. et al. Treatment with recombinant human insulin-like growth factor (rhIGF)-I/rhIGF binding protein-3 complex improves metabolic control in subjects with severe insulin resistance. J. Clin. Endocrinol. Metab. 95, 2113–2122 (2010).
Vestergaard, H., Rossen, M., Urhammer, S. A., Müller, J. & Pedersen, O. Short- and long-term metabolic effects of recombinant human IGF-I treatment in patients with severe insulin resistance and diabetes mellitus. Eur. J. Endocrinol. 136, 475–482 (1997).
Kuzuya, H. et al. Trial of insulinlike growth factor I therapy for patients with extreme insulin resistance syndromes. Diabetes 42, 696–705 (1993).
Takahashi, Y. et al. A homozygous kinase-defective mutation in the insulin receptor gene in a patient with leprechaunism. Diabetologia 40, 412–420 (1997).
Nakashima, N., Umeda, F., Yanase, T. & Nawata, H. Insulin resistance associated with substitution of histidine for arginine 252 in the alpha-subunit of the human insulin receptor: trial of insulin-like growth factor I injection therapy to enhance insulin sensitivity. J. Clin. Endocrinol. Metab. 80, 3662–3667 (1995).
Metwalley, K. A. & Farghaly, H. S. Berardinelli-Seip syndrome type 1 in an Egyptian child. Indian J. Hum. Genet. 20, 75–78 (2014).
Kirel, B. et al. A case of Donohue syndrome “Leprechaunism” with a novel mutation in the insulin receptor gene. Turk. Pediatr. Ars. 52, 226–230 (2017).
Saito-Hakoda, A. et al. A follow-up during puberty in a Japanese girl with type A insulin resistance due to a novel mutation in INSR. Clin. Pediatr. Endocrinol.: Case Rep. Clin. Invest.: Off. J. Jpn Soc. Pediatr. Endocrinol. 27, 53–57 (2018).
Kawana, Y., Imai, J., Sawada, S., Yamada, T. & Katagiri, H. Sodium-glucose cotransporter 2 inhibitor improves complications of lipodystrophy: a case report. Ann. Intern. Med. 166, 450–451 (2017).
Hamaguchi, T. et al. Treatment of a case of severe insulin resistance as a result of a PIK3R1 mutation with a sodium-glucose cotransporter 2 inhibitor. J. Diabetes Invest. 9, 1224–1227 (2018).
Ciudin, A. et al. Successful treatment for the Dunnigan-type familial partial lipodystrophy with Roux-en-Y gastric bypass. Clin. Endocrinol. (Oxf) 75, 403–404 (2011).
Grundfest-Broniatowski, S., Yan, J., Kroh, M., Kilim, H. & Stephenson, A. Successful treatment of an unusual case of FPLD2: the role of Roux-en-Y gastric bypass-case report and literature review. J. Gastrointest Surg. 21, 739–743 (2017).
Kozusko, K. et al. Clinical and molecular characterization of a novel PLIN1 frameshift mutation identified in patients with familial partial lipodystrophy. Diabetes 64, 299–310 (2015).
Kadowaki, T. et al. Two mutant alleles of the insulin receptor gene in a patient with extreme insulin resistance. Science 240, 787–790 (1988).
Yoshimasa, Y. et al. Insulin-resistant diabetes due to a point mutation that prevents insulin proreceptor processing. Science 240, 784–787 (1988).
Shackleton, S. et al. LMNA, encoding lamin A/C, is mutated in partial lipodystrophy. Nat. Genet. 24, 153–156 (2000).
Lightbourne, M. & Brown, R. J. Genetics of Lipodystrophy. Endocrinol. Metab. Clin. North Am. 46, 539–554 (2017).
Barroso, I. et al. Dominant negative mutations in human PPARgamma associated with severe insulin resistance, diabetes mellitus and hypertension. Nature 402, 880–883 (1999).
Hegele, R. A., Cao, H., Frankowski, C., Mathews, S. T. & Leff, T. PPARG F388L, a transactivation-deficient mutant, in familial partial lipodystrophy. Diabetes 51, 3586–3590 (2002).
Majithia, A. R. et al. Prospective functional classification of all possible missense variants in PPARG. Nat. Genet. 48, 1570–1575 (2016).
Mikita, J. S. et al. Determining the suitability of registries for embedding clinical trials in the united states: a project of the clinical trials transformation initiative. Ther. Innov. Regul. Sci. 55, 6–18 (2021).
Kidwell, K. M. et al. Application of Bayesian methods to accelerate rare disease drug development: scopes and hurdles. Orphanet J. Rare Dis. 17, 186 (2022).
Partington, G., Cro, S., Mason, A., Phillips, R. & Cornelius, V. Design and analysis features used in small population and rare disease trials: a targeted review. J. Clin. Epidemiol. 144, 93–101 (2022).
Adams, H. R. et al. A novel, hybrid, single- and multi-site clinical trial design for CLN3 disease, an ultra-rare lysosomal storage disorder. Clin. Trials 16, 555–560 (2019).
von Schnurbein, J. et al. European lipodystrophy registry: background and structure. Orphanet J. Rare Dis. 15, 17 (2020).
Doherty, D. A. et al. Registry randomised trials: a methodological perspective. BMJ open 13, e068057 (2023).
James, S., Rao, S. V. & Granger, C. B. Registry-based randomized clinical trials-a new clinical trial paradigm. Nat. Rev. Cardiol. 12, 312–316 (2015).
Acknowledgements
This research was funded in part, by the Wellcome Trust [Grant WT 210752 to RKS and WT 219606 to KAP]. For the purpose of open access, the author has applied a CC0 Public Domain Dedication to any Author Accepted Manuscript version arising from this submission. RJB and SA are supported by the intramural research program of the National Institute of Diabetes and Digestive and Kidney Diseases. The ADA/EASD Precision Diabetes Medicine Initiative, within which this work was conducted, has received the following support: The Covidence license was funded by Lund University (Sweden) for which technical support was provided by Maria Björklund and Krister Aronsson (Faculty of Medicine Library, Lund University, Sweden). Administrative support was provided by Lund University (Malmö, Sweden), University of Chicago (IL, USA), and the American Diabetes Association (Washington D.C., USA). The Novo Nordisk Foundation (Hellerup, Denmark) provided grant support for in-person writing group meetings (PI: L Phillipson, University of Chicago, IL).
Author information
Authors and Affiliations
Consortia
Contributions
R.K.S., R.J.B., and K.A.P. researched data, wrote the manuscript, and reviewed and approved the final manuscript. S.A. conducted statistical analyses and reviewed and approved the final manuscript. Members of the ADA/EASD PMDI Consortium provided feedback on methodology and reporting guidelines.
Corresponding author
Ethics declarations
Competing interests
The authors declare the following competing interests: R.K.S. has received speaker fees from Eli Lilly, Novo Nordisk, and Amryt. R. J. B. has received research support from Amryt, Third Rock Ventures, Ionis, and Regeneron. K.A.P. and S.A. report no conflicts of interest.
Peer review
Peer review information
Communications Medicine thanks Fabrizio Barbetti and Antonio Atalaia for their contribution to the peer review of this work. A peer review file is available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Semple, R.K., Patel, K.A., Auh, S. et al. Genotype-stratified treatment for monogenic insulin resistance: a systematic review. Commun Med 3, 134 (2023). https://doi.org/10.1038/s43856-023-00368-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s43856-023-00368-9
- Springer Nature Limited