Abstract
The World Health Organisation advocates Digital Health Technologies (DHTs) for advancing population health, yet concerns about inequitable outcomes persist. Differences in access and use of DHTs across different demographic groups can contribute to inequities. Academics and policy makers have acknowledged this issue and called for inclusive digital health strategies. This systematic review synthesizes literature on these strategies and assesses facilitators and barriers to their implementation. We searched four large databases for qualitative studies using terms relevant to digital technology, health inequities, and socio-demographic factors associated with digital exclusion summarised by the CLEARS framework (Culture, Limiting conditions, Education, Age, Residence, Socioeconomic status). Following the PRISMA guidelines, 10,401 articles were screened independently by two reviewers, with ten articles meeting our inclusion criteria. Strategies were grouped into either outreach programmes or co-design approaches. Narrative synthesis of these strategies highlighted three key themes: firstly, using user-friendly designs, which included software and website interfaces that were easy to navigate and compatible with existing devices, culturally appropriate content, and engaging features. Secondly, providing supportive infrastructure to users, which included devices, free connectivity, and non-digital options to help access healthcare. Thirdly, providing educational support from family, friends, or professionals to help individuals develop their digital literacy skills to support the use of DHTs. Recommendations for advancing digital health equity include adopting a collaborative working approach to meet users’ needs, and using effective advertising to raise awareness of the available support. Further research is needed to assess the feasibility and impact of these recommendations in practice.
Similar content being viewed by others
Introduction
The World Health Organisation (WHO) advocates Digital Health Technologies (DHTs) to advance population health1. Digital health can be defined as the use of information and communication technologies within healthcare to provide healthcare users with services relating to the prevention, detection, diagnosis and management of diseases and other health conditions2,3,4. Examples of DHTs include smartphone applications and wearable monitoring devices that can empower people to better manage their own conditions, such as keeping track of symptoms or remotely monitoring their condition(s) over time2,3,4. DHTs can pick up signs of deterioration in healthcare users’ symptoms longitudinally and provide real-time data to healthcare professionals to help support tailored clinical decision making4. DHTs can also enable individuals with mobility issues and those living in rural areas to access healthcare. Digital health has gained global momentum due to its potential to contribute to personalised health care for patients, improved quality of care, and lower healthcare costs5,6.
However, there are growing concerns that DHTs may not lead to health benefits in all populations, with underserved groups (i.e., those typically left out of research or experience inadequate access to healthcare) at particular risk7. One possible factor contributing to this is digital exclusion, denoting disparities in motivation, access and use of DHTs across different demographic groups8. Digital exclusion can potentially create a barrier for various underserved groups, such as those who are on a low income, are not fluent in English, or homeless, thus exacerbating health inequities for these groups9. Individuals with visual impairment may also find on-screen reading challenging and many older adults with hearing impairments have expressed low motivation to use phone calls as a remote option to access healthcare due to their disability10.
Technology has advanced rapidly over recent years, with some DHTs (e.g., telehealth services, mobile phones, wearable devices, smartphone apps and other software) having greater relevance to the direct inequities underserved groups face compared to other DHTs. For example, DHTs designed to be solely used by healthcare professionals (e.g., electronic patient records) are less likely to directly impact healthcare service users, and so it is prudent to focus on DHTs that underserved groups may be asked to use. Qualitative studies gathering rich in-depth experiences from those whose voices are rarely heard (i.e., underserved groups)11,12 will provide valuable insights into the facilitators and barriers regarding access, motivated and/or use of DHTs.
The WHO Bellagio eHealth Evaluation Group (2019) recognised the need to mitigate digital exclusion13, with organisations such as NICE (National Institute for Health and Care Excellence) requiring evidence that health inequities have been considered in the design of DHTs2. This includes important aspects of design, development or implementation of a DHT that support digital inclusivity, such as strategies to increase an individual’s access to suitable devices or connectivity, and educational support in digital literacy to increase DHT use14. To support the development of such strategies, it is vital to understand the needs of underserved groups as well as their experiences and perspectives of these strategies to identify what does and does not support digital inclusivity. However, there is currently no qualitative systematic review of key strategies conducted in this area; a key knowledge gap in the literature. To advance digital health equity, we aimed to systematically synthesise the literature on what key strategies have been used to promote digital inclusivity, and assess the facilitators and barriers to implementing and adopting these in practice based on underserved groups’ experiences and perspectives.
Results
Study descriptions
Our search yielded 13,216 results. After removing duplicates (n = 2815), titles (n = 10,401) abstracts (n = 1224) and full-texts (n = 143) were screened. Ten papers met our inclusion criteria (Fig. 1). Inter-reviewer reliability was high with 99.33% agreement at title stage, 99.43% at abstract stage, and 97.89% at full-text stage. All included studies were found to have moderate- to high-quality levels (Supplementary Tables 7 and 8). None of the included studies measured or reported any participants’ health literacy.
Included studies incorporated a range of participants at risk of digital exclusion, including those from different cultural backgrounds (ethnic diversity, languages and religion) (n = 8)15,16,17,18,19,20,21,22,23, those with limiting conditions (visual and hearing impairments) (n = 2)21,22, low educational attainment (n = 4)15,19,20,21, aged over 65 (n = 4)16,20,21,22, homeless (n = 2)19,24, and those who had low socioeconomic status (n = 5)15,16,17,18,21 (Supplementary Table 9). All 10 studies used interviews15,16,17,18,19,20,21,22,23,24, with two studies also conducting focus groups with participants18,21. (Supplementary Table 10). Inclusive digital health strategies were grouped into either outreach programmes providing educational support and/or access to devices (n = 2)19,22, or co-designing DHTs with underserved groups (n = 8) to gain feedback on the usability and acceptability of DHT to enhance inclusivity in future versions of the DHT (Table 1)15,16,17,18,20,21,23,24.
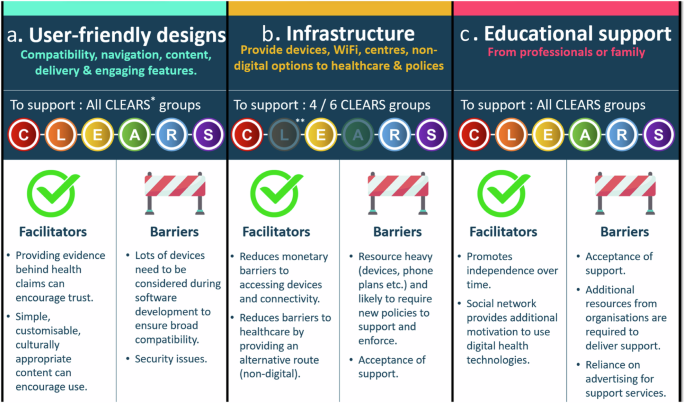
Our narrative thematic synthesis generated three overarching themes; user-friendly designs (e.g., software and website design elements that promoted inclusivity), infrastructure (e.g., access to DHTs) and educational support (e.g., training to develop digital literacy skills required to use DHTs) (Supplementary Table 10). Facilitators and barriers to the adoption of these themes are embedded in the discussion below and summarised in Fig. 2.
User-friendly designs
User-friendly designs were a key theme supporting access and use of DHTs across seven studies15,16,20,21,22,24. Health-related software and websites needed to be compatible across different digital platforms, operating systems and devices including smartphones and desktops, and assistive technologies (e.g., screen reading software) to accommodate the needs of ethnically and linguistically diverse groups17,18,22, individuals with limiting conditions (visual and hearing impairments)20,21, older adults (+65 years)20,22, those with low educational attainment and low socioeconomic status17,18. For example, Yeong et al. noted how older adults with visual impairments and of low socioeconomic status needed websites to be compatible with different magnification levels and assistive technologies (e.g., iOS Voiceover [Apple Inc]; a screen reading software) to aid visibility21. The authors also noted how certain features aided navigation and minimised scrolling to help the user find information, such as tables of contents, drop-down menus, and ‘jump to top’ buttons21. Older adults with limiting conditions (visual or hearing) also suggested that navigation features, such as search bars and hyperlinks, needed to be of high contrast (compared to the rest of the screen) to improve visibility20,21. Yeong et al. emphasised how search features should be designed in a similar way to commonly visited search engines, like Google, to improve usability and reduce confusion21.
Older adults, homeless, ethnically diverse individuals and those with visual impairments all described how digital messages on software, health related websites or text messages should be simple, concise, and presented in a logical manner without time restrictions18,20,21,24. For example, older adults with visual impairments described how they did not have enough time to read the information when presented on a timed loop (i.e., rotating between different screens with information), and suggested that the user be able to manually control the timing of this loop21. Older adults interviewed in another study described how it would be useful if they could change the font size to improve the visibility of the text, and provide alternative languages for those who are not fluent in English22. Personalising information, such as allowing users to choose content that they are interested in, was felt to be one way of increasing the motivation to use health related websites and software amongst those with visual impairments21 and ethnically diverse individuals18. Additionally, providing evidence that supported the key messages in healthcare information, such as the importance of reducing alcohol intake to reduce the risk of developing chronic health conditions, enhanced trust amongst ethnically diverse individuals18. Kramer et al. also emphasised how any communication should be culturally appropriate and avoid reinforcing stereotypes, especially for ethnically and linguistically diverse users18. For example, the language used to categorise different ethnicities on DHTs should avoid generic terms such as ‘men of colour’ as some ethnically diverse men found this offensive; they felt it defined them based on their skin colour and not their ethnic background. Instead, specific terminology should be used that accurately represented their ethnicities (e.g., African American for individuals with an African and American descent)18. Any imagery should also be inclusive to all cultural groups18.
It was felt that the overall user friendliness and engagement of health related software could be improved with the addition of engaging features15,18,20,22,24. This included interactive quiz elements20, notifications encouraging behavioural changes18, reminders about upcoming appointments (particularly for homeless individuals as this they may not have access to other reminders, like letters)24, ability to order a repeat prescription and schedule specific appointments (e.g., physiotherapy)22. Older adults of Jewish faith also suggested simplifying security features, as many found flicking between a text message with the password reset information and the screen (where the information should be entered) challenging22.
Infrastructure
Five studies described the need for supportive infrastructure, such as access to devices and connectivity (i.e., Wi-Fi) to support homeless individuals, ethnically and linguistically diverse groups, and individuals of low socioeconomic status15,17,19,23,24. For example, Howell et al. explained how community nurses in the UK provided homeless individuals with temporary access to smartphones during the pandemic so as to enable them to access vital digital healthcare support19. In the United States (US), homeless individuals were provided with phones (the Obama phone), credit and data plans financed through a government programme24. However, Asgary et al. found that some of these homeless individuals using the Obama phone plan often exceeded their limits when put on hold to schedule medical appointments24. They subsequently turned to friends and family for financial support to purchase credit24. Other homeless individuals were hesitant to accept this government support, with the authors reflecting on how this may have been due to the homeless experiencing a lack of government financial aid in the past24.
Homeless individuals19, ethnically and linguistically diverse groups15,17,23, and those of low educational attainment and low socioeconomic status15,17,19 reported relying heavily on free Wi-Fi to be able to access healthcare. This included accessing free Wi-Fi in public spaces and transport systems, fast-food restaurants, clinics and families’ houses. However, they often experienced barriers to this connectivity with time limits set by the specific organisations (e.g., opening hours)15 or restrictions placed on using shared devices (e.g., computer keyboards due to the risk of coronavirus spreading)19. Many participants suggested creating dedicated centres for digital health services with suitable devices and free Wi-Fi that would also include some private areas15. Access to these private spaces was felt to be important for some ethnic and linguistically diverse groups with low educational attainment and socioeconomic status, as they were concerned about being overheard when discussing/looking at confidential health information17. Many groups suggested that they would like the choice between both digital and non-digital access to healthcare, as this would help mitigate the risk of possibly excluding those with poor digital literacy skills, those who would prefer in-person consultations, or those who lack the resources to access digital healthcare15,18,19,23.
To complement infrastructural changes, ethnically diverse adults based in the US advocated for more resources to be provided by local government15. This included the introduction of new policies, such as reduced payment plans and regulations on the price of DHTs for lower income earners to make them affordable15. Older adults of Jewish faith and ethnically diverse adults with a low educational attainment and socioeconomic status also suggested that financial incentives could help promote greater access to DHTs and encourage motivation to use DHTs15,22. Alkureishi et al. highlighted how different organisations, such as hardware and Wi-Fi companies, might need to collaborate to ensure that these different components (e.g., devices, connectivity, financial aid) are jointly available to support successful implementation15.
Educational support
Provision of educational support was important for ethnically diverse individuals and older adults to enable their use of DHTs in five studies15,16,19,20,22. Ethnically diverse individuals with lower educational attainment and low socioeconomic status, and older adults of Jewish faith commonly reported asking family members to remain close during video healthcare consultations in case of technical issues15, or for their guidance with accessing online health information22. Mizrachi et al. found this support promoted independence over time as older adults’ digital skills developed through learning and they were further motivated to use DHTs on hearing positive experiences from their family and friends22.
Some individuals relied on educational support from professional services to use DHTs19. It was felt that in-person educational support from community workers or health care professionals with supplementary materials (e.g., videos and written information) would be beneficial prior to attending virtual appointments to support ethnically diverse adults (both above and below 65 years) from a low socioeconomic status and low educational attainment15,16 Alternatively, Alkureishi et al. noted some participants expressed preference for accessing training classes at healthcare sites (e.g., hospitals) and community centres, where support was provided by ‘technology champions and coaches’15. However, older adults of Jewish faith highlighted how advertisements to promote awareness of support services would be unlikely to reach individuals in their community and those who were socially isolated and arguably most in need of support22. Some studies also highlighted how certain groups (e.g., ethnically diverse adults with low socioeconomic status and low educational attainment, and older adults of Jewish faith) might also be reluctant to accept this educational support due to concerns around burdening others, feeling helpless, and/or reaffirming how they are unable to do something independently15,22.
Discussion
This systematic review synthesises strategies that promote digital inclusivity and assess the barriers and facilitators to adopting these in practice. Our findings highlighted three key themes relating to user-friendly designs, supportive infrastructure, and provision of educational support. Barriers to adopting these strategies included a lack of acceptance amongst some underserved groups to receive such support, whilst facilitators included promoting trust amongst ethnically diverse groups by providing lay term friendly evidence that supports health claims.
Our findings highlighted how health-related software and websites must be interoperable across different devices to accommodate the needs of underserved groups. This form of user-friendly design is advocated by national healthcare providers and government bodies; for example, the UK and US have legislation in place which mandates that websites and software in the public sector be ‘perceivable, operable, understandable and robust’ to ensure that those with visual and hearing impairments, low reading ability (reading age of 9) and/or those who are not fluent in English can access and understand the information provided25,26. However, a recent study reported that public health authority websites in only three countries (UK, Italy, China) out of a total of 24 actually adhered to these accessibility standards when checked27. Additionally, the wider literature supports our findings on how the use of appropriate language and imagery can improve end-user satisfaction18,28. National bodies, such as the US National Institute of Health (NIH), have developed the ‘National Culturally and Linguistically Appropriate Services (CLAS) Standards’ to assist developers and researchers in developing culturally and linguistically appropriate services29. The wider literature also suggests co-designing DHTs with underserved groups at the earliest stages to help ensure that they meet the needs of all end-users30. This involves co-designing security features that are easy-to-use and align with the UK government ‘secure by design principles’, to help overcome any potential future barriers to usage31,32.
Our results also highlighted the need for supportive infrastructure to facilitate access and use of DHTs. Government schemes in high-income countries are already available; for example, the ‘Obama phone’ in the USA and the Emergency Broadband Benefits and social tariffs (reduced payment phone plans) in the UK, to support those on a low income to access smartphones and phone plans24,33. However, implementing supportive infrastructure might not be viable for low to middle income countries as they may have less suitable centres to provide devices and free public Wi-Fi spots, which high income countries already have access to34. Some charity organisations, such as the Good Things Foundation, have started to repurpose donated corporate IT devices and deliver them to those who are digitally excluded35. However, better promotion of the support available and a collaborative working environment is needed, especially by healthcare professionals, social services, and charities. Free phone numbers would also help to facilitate access to healthcare services. Some underserved groups would like the option of accessing healthcare via non digital means, thus questioning the temptation to always use technology to potentially address healthcare challenges36. Researchers need to consider whether a new DHT will provide an equitable solution to the healthcare problem and whether other means of accessing healthcare should also be provided within healthcare systems37.
This systematic review also underlined the importance of providing educational support, from family or professional services, to encourage motivation and capability to use DHTs. There is a need for effective advertising of this support to groups at particular risk of both digital and social exclusion, such as older adults and homeless individuals, in order to increase their awareness38. A systematic review conducted by Ige et al.39 suggested using a combination of two or more strategies to reach socially isolated individuals, including referrals from relevant agencies (e.g., GPs, pharmacists etc), as this might be a more effective approach than relying solely on public facing methods39.
Previous recommendations to promote digital health equity have centred around guidance for behavioural and social science researchers with limited insight to the facilitators and barriers to implementing strategies into society and appear limited to research settings40. Previous reviews have applied the socioeconomic model to inform recommendations to promote digital health equity, such as providing devices (individual level support), educational support (relationship/interpersonal level support), access to connectivity infrastructure (community level support) and implementing policies (societal level support)41,42. However, there has been little consideration given to those individuals who belong to two or more underserved groups at risk of digital exclusion. Our systematic review considered this intersectionality and provides practical recommendations that focus on two main areas: collaborative working and effective advertising (Fig. 3). Collaborative working between the DHT developer, healthcare professionals, policy-makers, voluntary sectors, patients and public members of underserved groups is vital to help improve the co-design of DHTs and provision of support and should be embedded from the very beginning of the design and development process30. Effective advertising strategies are also vital to raise public awareness and ensure that those who are, or know of an individual, at risk of digital exclusion are made aware of in-person support that is available and how to access it. DHT developers and researchers should also be aware of the accessibility and inclusivity standards (e.g., government legislation and CLAS) and on how to use them to support digital health equity.
This review used a comprehensive and systematic approach to identify relevant literature. Included studies were published within the last decade to remain relevant to the current digital healthcare landscape. We opted to focus on qualitative research to gather rich detailed information on the facilitators and barriers to each strategy. Despite no geographical restrictions being placed on this search, we found that all included studies were conducted in high-income countries, which may limit the applicability of these findings to low- and middle-income countries; this also highlights the importance of further work in this area. Representation of the different religious groups and languages was limited, highlighting a gap in the literature and a need for greater diverse inclusion in research. None of the included studies reported on participants’ health literacy, which has previously been suggested to overlap with low digital literacy43; this information would have aided our understanding of whether the participants included in the qualitative studies were truly representative of the groups that they were intended to represent. Future research should incorporate a standardised health literacy measure, such as the Newest Vital Sign (NVS)44 or the Health Literacy Questionnaire (HLQ)45, into their methodology to provide greater detail on the participants in their study.
The appropriateness of recommendations from this systematic review could be further explored using an established framework, such as the APEASE criteria (Affordability, Practicability, Effectiveness, Acceptability, Size effects/safety, and Equity)46. This would involve seeking the perspectives of CLEARS demographic groups’ and relevant stakeholders’ (e.g., policy makers and community workers) on the practicalities of implementing these different strategies and recommendations to further advance this important area of digital health equity. The facilitators and barriers to implementing government-issued public health website accessibility standards should also be explored to further understand how to encourage use of these standards.
This systematic review identified three key themes relating to digital inclusivity, associated facilitators and barriers, and recommendations for advancing digital health equity. This information will guide individuals when designing, developing and implementing digital health interventions to ensure it is done in a digitally inclusive manner. This review also highlighted the need for further work to explore the feasibility and acceptance of implementing different strategies and recommendations to support digital health equity amongst those at risk of digital exclusion.
Methods
Identification of key groups at risk of digital exclusion
We conducted a scoping review of the literature to identify the sociodemographic factors that could put an individual at risk of digital exclusion. Based on the findings published in peer-reviewed articles24,47,48,49,50,51,52,53,54,55,56,57,58,59,60, systematic reviews61,62,63,64, government reports8,65, and regulatory organisation documents66, we identified a number of sociodemographic factors that we complied into six groups, relating to Culture (ethnicity, language, and religion)8,47,48,49,50,51,52,53,62, Limiting conditions (visual and hearing impairments)6,54,66, Education (at or below United Kingdom (UK) government mandated level or equivalent)52,55,56,66, Age (over 65 years)51,54,55,56,62,66, Residence (rural or deprived areas [based on consensus data within a country], or homeless)8,24,51,60, and Socioeconomic status (low income [earns less than 60% of the median household annual income within a country] and unemployed individuals)8,52,55,56,62,65,66 abbreviated to CLEARS (Fig. 4). These factors often intersect (i.e. intersectionality), placing an individual at even greater risk of digital exclusion8,64,65,66.
Search strategy
This systematic review was registered with PROSPERO (CRD42022378199) and followed PRISMA guidelines67. The search string utilised terms from two relevant scoping reviews8,68, with additional relevant terms included when searching four large online databases (Medline, Embase, PsycINFO and Scopus) (Supplementary Tables 1–4). The search focused on words associated with digital technology, health inequities, and CLEARS (Table 2).
Eligibility criteria
The eligibility criteria followed the Population, Intervention, Comparison, Outcomes and Study design (PICOS) framework, recommended by the Cochrane Handbook for Systematic Reviews69, and provided an organising framework to list the main concepts in the search. The Population criteria included any group represented by our CLEARS framework (see above). The Intervention criteria focused on inclusive digital health strategies, which we defined as an action designed to alleviate the digital exclusion of individuals by promoting access, motivation, and/or use of information and communication technologies2,3,4,5. Articles needed to have discussed the facilitators or barriers associated with the inclusive digital health strategy (outcome criteria) to be included. This allowed the researchers to reflect on what currently worked or did not work to inform key recommendations. Only qualitative studies that provided rich in-depth experiences from CLEARS groups were included to aid our understanding of how a complex phenomenon, i.e., intersectionality, can affect digital exclusion11,12. Quantitative studies were excluded as they are designed to test a hypothesis or enumerate events or phenomena11,12, which was not aligned with the aim of this review. Only peer-reviewed articles published between 2012 and 2022 in the English language were included; this ensured only the latest advancements in digital technologies were considered.
Study selection
Results from each database were exported into EndNote (version 20.5, Clarivate, International) and duplicates removed. Remaining articles were uploaded to Rayyan (Qatar Foundation, State of Qatar)70, where titles, abstracts, and full-texts were screened independently by two reviewers (SW, LL, EB) to minimise bias. The lead author (SW) screened all articles, acting as a constant throughout the process. Disagreements were resolved by a third reviewer (RMA). The reasons for excluding full text articles were recorded (Fig. 1).
Data extraction and synthesis
The lead author (SW) developed a data-extraction sheet with the research team to extract and record specific study details, including participant demographics and a description of the inclusive digital health strategy under investigation (Supplementary Tables 5 and 6). Any measure used to record participants’ health literacy in the included studies, such as the Newest Vital Sign (NVS)44 or the Health Literacy Questionnaire (HLQ)45, was also extracted. A quality assessment was carried out on the included studies using the Critical Appraisal Skills Programme (CASP) Qualitative Review Checklist71. Quality was measured by reporting the frequency of ‘yes’ (denoting the study met the criteria on the checklist) (Supplementary Tables 7 and 8).
The lead author (SW) performed a narrative thematic synthesis of the included studies. Firstly, the authors began by developing a preliminary synthesis of findings from included studies to identify the key strategies and list the facilitators and barriers to implementation. We then considered the factors that might explain any commonalities and differences in the successful implementation of these digital inclusive strategies across included studies. This involved exploring the directly reported verbatim quotations obtained from particular CLEARS groups and seeking to draw descriptive and explanatory conclusions around key themes72,73. All data management and analysis was carried out within N-Vivo (version 1.6.1, QSR International). Discussions with co-authors (SPS, RM, CT) were conducted at several stages throughout the analysis to discuss, refine and define themes to ensure a coherent narrative that reflected the data. Detailed descriptions and contextual material from the included studies was kept throughout the analysis to ensure that the trustworthiness was upheld74,75. Ethics approval was not required for this systematic review.
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Data availability
All relevant data used for the study has been included in the manuscript and supplementary information.
References
World Health Organization. Digital Health. URL: https://www.who.int/health-topics/digital-health#tab=tab_3 (2020).
National Institute for Health and Clinical Excellence. Evidence standards framework for digital health technologies. URL: https://www.nice.org.uk/corporate/ecd7/resources/evidence-standards-framework-for-digital-health-technologies-pdf-1124017447605 (2022).
Arora, S. et al. Detecting and monitoring the symptoms of Parkinson’s disease using smartphones: A pilot study. Parkinsonism Relat. Disord. 21, 650–653 (2015).
Yao, R. et al. Inequities in Health Care Services Caused by the Adoption of Digital Health Technologies: Scoping Review. J. Med. Internet Res. 24, e34144 (2022).
Berwick, D. M., Nolan, T. W. & Whittington, J. The triple aim: care, health, and cost. Health Aff. 27, 759–769 (2008).
Espay, A. J. et al. Technology in Parkinson’s disease: challenges and opportunities. Mov. Disord. 31, 1272–1282 (2016).
National Institute for Health Research. Improving inclusion of under-served groups in clinical research: Guidance from include project. URL: https://www.nihr.ac.uk/documents/improving-inclusion-of-under-served-groups-in-clinical-research-guidance-from-include-project/25435 (2022).
Honeyman, M., Maguire, D., Evans, H. & Davies, A. Digital technology and health inequalities: a scoping review (Public Health Wales NHS Trust, 2020).
Mitchell, C. et al. Underserved ‘Deep End’ populations: a critical analysis addressing the power imbalance in research. Br. J. Gen. Pract. 73, 326–329 (2023).
Kaihlanen, A. M. et al. Towards digital health equity—a qualitative study of the challenges experienced by vulnerable groups in using digital health services in the COVID-19 era. BMC Health Serv. Res. 22, 188 (2022).
Patton, M. Q. Alternative Evaluation Research Paradigm (University of North Dakota, 1975).
Sofaer, S. Qualitative methods: what are they and why use them? Health Serv. Res. 34, 1101 (1999).
World Health Organization. WHO guideline: recommendations on digital interventions for health system strengthening (World Health Organization, 2019).
NHS England. Supporting digital inclusion in general practice: 10 top tips. Available from: https://www.england.nhs.uk/long-read/supporting-digital-inclusion-in-general-practice-10-top-tips/#:~:text=For%20NHS%20patients%2C%20digital%20inclusion,confidently%20to%20access%20NHS%20services (2023). (Accessed 29 October 2023).
Alkureishi, M. A. et al. Digitally disconnected: qualitative study of patient perspectives on the digital divide and potential solutions. JMIR Hum. Factors 8, e33364 (2021).
Choxi, H., VanDerSchaaf, H., Li, Y. & Morgan, E. Telehealth and the digital divide: Identifying potential care gaps in video visit use. J. Med. Syst. 46, 58 (2022).
Kim, H. & Zhang, Y. Health information seeking of low socioeconomic status Hispanic adults using smartphones. Aslib J. Inf. Manag. 67, 542–561 (2015).
Kramer, J. et al. Black men’s experiences with health care: individuals’ accounts of challenges, suggestions for change, and the potential utility of virtual agent technology to assist black men with health management. Qualitative Health Res. 31, 1772–1785 (2021).
Howells, K. et al. Remote primary care during the COVID-19 pandemic for people experiencing homelessness: a qualitative study. Br. J. Gen. Pract. 72, e492–e500 (2022).
Maidment, D. W. et al. Evaluating a theoretically informed and co-created mobile health educational intervention for first-time hearing aid users: qualitative interview study. JMIR mHealth uHealth 8, e17193 (2020).
Yeong, J. L., Thomas, P., Buller, J. & Moosajee, M. A newly developed web-based resource on genetic eye disorders for users with visual impairment (Gene. Vision): usability study. J. Med. Internet Res. 23, e19151 (2021).
Mizrachi, Y., Shahrabani, S., Nachmani, M. & Hornik, A. Obstacles to using online health services among adults age 50 and up and the role of family support in overcoming them. Isr. J. Health Policy Res. 9, 1–10 (2020).
Wikaire, E. et al. Reducing healthcare inequities for Māori using telehealth during COVID-19. NZ Med. J. 135, 112–117 (2022).
Asgary, R. et al. Perceptions, attitudes, and experience regarding mHealth among homeless persons in New York City shelters. J. Health Commun. 20, 1473–1480 (2015).
Public Sector Bodies (Websites and Mobile Applications) (No. 2) Accessibility Regulations https://www.legislation.gov.uk/uksi/2018/952/contents (2018).
Checklist of requirements for federal websites and digital services. Accessibility and Section 508. https://digital.gov/resources/checklist-of-requirements-for-federal-digital-services/ (2018).
Alajarmeh, N. Evaluating the accessibility of public health websites: an exploratory cross-country study. Univers. Access Inf. Soc. 21, 771–789 (2022).
Brach, C. & Fraserirector, I. Can cultural competency reduce racial and ethnic health disparities? A review and conceptual model. Med. Care Res. Rev. 57, 181–217 (2000).
U.S. Department of Health and Human Services, Office of Minority Health. National Standards for Culturally and Linguistically Appropriate Services in Health and Health Care: Compendium of State-Sponsored National CLAS Standards Implementation Activities. Washington, DC: U.S. Department of Health and Human Services (2016).
Slattery, P., Saeri, A. K. & Bragge, P. Research co-design in health: a rapid overview of reviews. Health Res. Policy Syst. 18, 1–3 (2020).
Central Digital and Data Office (CDDO). Secure by design principles. URL: https://www.security.gov.uk/guidance/secure-by-design/principles/#4-design-usable-security-controls (2024).
Central Digital and Data Office (CDDO). Understanding business objectives and user needs. URL: https://www.security.gov.uk/guidance/secure-by-design/activities/understanding-business-objectives-and-user-needs (2024).
UK Government. Low cost broadband and mobile phone tariffs. URL: https://www.gov.uk/government/news/low-cost-broadband-and-mobile-phone-tariffs (2022).
Verhagen, L. M. et al. COVID-19 response in low-and middle-income countries: Don’t overlook the role of mobile phone communication. Int. J. Infect. Dis. 99, 334–337 (2020).
National Device Bank: Donate unused corporate IT equipment. URL: https://www.goodthingsfoundation.org/national-device-bank/ (2023).
IJsselsteijn, W., Tummers-Heemels, A. & Brankaert, R. Warm technology: A novel perspective on design for and with people living with dementia. In HCI and Design in the Context of Dementia, 33–47 (2020).
Shull, J. G. Digital health and the state of interoperable electronic health records. JMIR Med. Inform. 7, e12712 (2019).
Landeiro, F., Barrows, P., Musson, E. N., Gray, A. M. & Leal, J. Reducing social isolation and loneliness in older people: a systematic review protocol. BMJ Open 7, e013778 (2017).
Ige, J., Gibbons, L., Bray, I. & Gray, S. Methods of identifying and recruiting older people at risk of social isolation and loneliness: a mixed methods review. BMC Med. Res. Methodol. 19, 1–10 (2019).
Jaworski, B. K. et al. Advancing digital health equity: Directions for behavioral and social science research. Transl. Behav. Med. 13, 132–139 (2023).
McCall, T. et al. A socio-ecological approach to addressing digital redlining in the United States: a call to action for health equity. Front. Digital Health 4, 897250 (2022).
Richardson, S., Lawrence, K., Schoenthaler, A. M. & Mann, D. A framework for digital health equity. NPJ Digital Med. 5, 119 (2022).
Stone, E., Nuckley, P. & Shapiro, R. Digital inclusion in health and care: lessons learned from the NHS Widening Digital Participation Programme (Good Things Foundation, 2020).
Weiss, B. D. et al. Quick assessment of literacy in primary care: the newest vital sign. Ann. Fam. Med. 3, 514–522 (2005).
Osborne, R. H. et al. The grounded psychometric development and initial validation of the Health Literacy Questionnaire (HLQ). BMC Public Health 13, 7 (2013).
Michie, S., Atkins, L. & West, R. The behaviour change wheel. A guide to designing interventions (Silverback Publishing, 2014).
Boonya-Ananta, T. et al. Monte Carlo analysis of optical heart rate sensors in commercial wearables: the effect of skin tone and obesity on the photoplethysmography (PPG) signal. Biomed. Opt. Express 12, 7444–7457 (2021).
Mitchell, U. A., Chebli, P. G., Ruggiero, L. & Muramatsu, N. The digital divide in health-related technology use: The significance of race/ethnicity. Gerontologist 59, 6–14 (2019).
Diao, J. A. et al. Clinical implications of removing race from estimates of kidney function. JAMA 325, 184–186 (2021).
Levey, A. S. et al. Kidney disease, race, and GFR estimation. Clin. J. Am. Soc. Nephrol. 15, 1203–1212 (2020).
Dilmaghani, M. Religiosity and the digital divide in Canada. Commun. Rev. 21, 181–211 (2018).
Jamil, S. From digital divide to digital inclusion: Challenges for wide-ranging digitalization in Pakistan. Telecommun. Policy 44, 102206 (2021).
Bix, A. S. Remember the Sabbath’: a history of technological decisions and innovation in Orthodox Jewish communities. Hist. Technol. 36, 205–239 (2020).
Harris, J. The use, role and application of advanced technology in the lives of disabled people in the UK. Disability Technol. 80–127 (2017).
Estacio, E. V., Whittle, R. & Protheroe, J. The digital divide: examining socio-demographic factors associated with health literacy, access and use of internet to seek health information. J. Health Psychol. 24, 1668–1675 (2019).
Alvarez-Galvez, J. et al. The persistence of digital divides in the use of health information: A comparative study in 28 European countries. Int. J. Public Health 65, 325–333 (2020).
Elena-Bucea, A. et al. Assessing the role of age, education, gender and income on the digital divide: Evidence for the European Union. Inf. Syst. Front. 23, 1007–1021 (2021).
Yao, Y. et al. Bridging the digital divide between old and young people in China: challenges and opportunities. Lancet Healthy Longev. 2, e125–e126 (2021).
Holgersson, J. & Söderström, E. Bridging the gap: Exploring elderly citizens’ perceptions of digital exclusion. In 27th European Conference on Information Systems (ECIS) (Association for Information Systems, 2019).
Rhoades, H. et al. No digital divide? Technology use among homeless adults. J. Soc. Distress Homeless 26, 73–77 (2017).
Saeed, S. A. & Masters, R. M. Disparities in health care and the digital divide. Curr. Psychiatry Rep. 23, 1–6 (2021).
Reiners, F. et al. Sociodemographic factors influencing the use of eHealth in people with chronic diseases. Int. J. Environ. Res. Public Health 16, 644 (2019).
Almathami, H. K., Win, K. T. & Vlahu-Gjorgievska, E. Barriers and facilitators that influence telemedicine-based, real-time, online consultation at patients’ homes: systematic literature review. J. Med. Internet Res. 22, e16407 (2020).
Husain, L. et al. Desperately seeking intersectionality in digital health disparity research: narrative review to inform a richer theorization of multiple disadvantage. J. Med. Internet Res. 24, e42358 (2022).
Gov.uk. Ethnicity facts and figures: People in low-income households. URL: https://www.ethnicity-facts-figures.service.gov.uk/work-pay-and-benefits/pay-and-income/people-in-low-income-households/latest (2022).
Ofcom. Digital exclusion: A review of Ofcom’s research on digital exclusion among adults in the UK. URL: https://www.ofcom.org.uk/__data/assets/pdf_file/0022/234364/digital-exclusion-review-2022.pdf (2022).
Page, M. J. et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int. J. Surg. 88, 105906 (2021).
Budhwani, S. et al. Challenges and strategies for promoting health equity in virtual care: findings and policy directions from a scoping review of reviews. J. Am. Med. Inform. Assoc. 29, 990–999 (2022).
Tacconelli, E. Systematic reviews: CRD’s guidance for undertaking reviews in health care. Lancet Infect. Dis. 10, 226 (2010).
Rayyan: AI powered tool for Systematic Literature Reviews. Available from: https://www.rayyan.ai/ (2023).
Critical Appraisal Skills Programme. CASP Qualitative Studies Checklist. URL: https://casp-uk.net/images/checklist/documents/CASP-Qualitative-Studies-Checklist/CASP-Qualitative-Checklist-2018_fillable_form.pdf (2023). (Accessed 30 April 2023).
Pope, C. & Mays, N. Reaching the parts other methods cannot reach: an introduction to qualitative methods in health and health services research. BMJ 311, 42–45 (1995).
Popay, J., Rogers, A. & Williams, G. Rationale and standards for the systematic review of qualitative literature in health services research. Qualitative Health Res. 8, 341–351 (1998).
Wertz, F. J. Five ways of doing qualitative analysis: Phenomenological psychology, grounded theory, discourse analysis, narrative research, and intuitive inquiry, 228 (Guilford Press, 2011).
Lucas, P. J., Baird, J., Arai, L., Law, C. & Roberts, H. M. Worked examples of alternative methods for the synthesis of qualitative and quantitative research in systematic reviews. BMC Med. Res. Methodol. 7, 1–7 (2007).
Acknowledgements
We would like to thank the social sciences librarian, Karen Crinnion, at Philip Robinson Library, Newcastle University, for her help and advice regarding the search strategy, choice of databases and search keywords for this systematic review. This work has been supported by the Early Detection of Neurodegenerative diseases (EDoN) research initiative, funded by Alzheimer’s Research UK with support from Gates Ventures and the Alzheimer’s Drug Discovery Foundation through its Diagnostic Accelerator Project. This project is also funded by the NIHR, (NIHR205190). The views expressed are those of the author(s) and not necessarily those of the NIHR or the Department of Health and Social Care. The funder of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report. Ríona Mc Ardle is funded by the National Institute for Health Research (NIHR) (NIHR 301677) and the NIHR Newcastle Biomedical Research Centre (BRC) based at The Newcastle upon Tyne Hospital National Health Service (NHS) Foundation Trust; Newcastle University; and the Cumbria, Northumberland and Tyne and Wear (CNTW) NHS Foundation Trust. The views expressed in this publication are those of the author(s) and not necessarily those of the NIHR, NHS or the UK Department of Health and Social Care.
Author information
Authors and Affiliations
Contributions
S.W. (Lead author): Conception and design of the work. Methodology. Literature search and data acquisition, analysis and interpretation of the data. Drafting (writing original draft) and revising. Visualisations. Completion of version. Accountability for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. S.S. (Corresponding author): Conception of the work. Funding acquisition. Methodology. Revising the work (providing feedback) and supervision of lead author. Final approval of the completed version. Accountability for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. C.T.: Conception of the work. Methodology. Revising the work (providing feedback) and supervision of lead author. Accountability for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. R.M.A.: Conception of the work. Methodology. Revising the work (providing feedback) and supervision of lead author. Accountability for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. R.S.: Conception of the work. Methodology. Revising the work (providing feedback) and supervision of lead author. Accountability for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. N.H.: Revising the work (providing feedback). E.B.: Data acquisition (second check of the articles). Revising the work (providing feedback). L.L.: Data acquisition (second check of the articles). Revising the work (providing feedback).
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wilson, S., Tolley, C., Mc Ardle, R. et al. Recommendations to advance digital health equity: a systematic review of qualitative studies. npj Digit. Med. 7, 173 (2024). https://doi.org/10.1038/s41746-024-01177-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41746-024-01177-7
- Springer Nature Limited