Abstract
Stereotactic radiation therapy (SBRT) has emerged as a promising treatment modality for locally advanced pancreatic cancer. The aim of this study is to assess the dosimetric efficacy of online adaptive radiotherapy (ART) in comparison to image-guided radiation therapy (IGRT) for pancreatic cancer. We conducted a retrospective analysis involving 8 patients diagnosed with locally advanced pancreatic cancer. The gross tumor volume (GTV) delineates the visible extent of the tumor on imaging, while the planning tumor volume (PTV) was generated by expanding 5 mm from the GTV and ensuring a 3 mm distance from the small intestine, duodenum, and stomach simultaneously. Treatment planning was executed using the United Imaging Healthcare Treatment Planning System workstation. The control group underwent evaluation based on daily validated fan-beam CT (FBCT) scans, assessing both the dose delivered to actual organs at risk (OARs) and the target volume. Radiotherapy plans were developed utilizing simulation CT, and conventional radiotherapy with daily image-guided radiation therapy (IGRT) was administered using FBCT-Linac. Conversely, patients in the study group received daily validated FBCT-guided adaptive radiotherapy plans, with a focus on mean dose assessment of both the target volume and OARs. Subsequently, we compared the average outcomes of each treatment fraction between IGRT and online adaptive radiotherapy (ART). Comparison between ART and IGRT treatment plans revealed significant differences in various dosimetric parameters: For PTV: V98%: ART (96.28%) vs IGRT (89.73%), p = 0.000, V95%: ART (96.28%) vs IGRT (89.73%), p = 0.031, V90%: ART (98.58%) vs IGRT (93.65%), p = 0.000, Dmean: ART (4912.91) vs IGRT (4804.11), p = 0.000. For GTV: V100%: ART (97.96%) vs IGRT (94.85%), p = 0.314, V98%: ART (100.00%) vs IGRT (96.83%), p = 0.000, V90%: ART (100.00%) vs IGRT (97.75%), p = 0.000, Dmean: ART (4972.17) vs IGRT (4907.23), p = 0.000. For the duodenum: D0.5cc: ART (2883.92) vs IGRT (3359.35), p = 0.000, D1cc: ART (2726.32) vs IGRT (3128.66), p = 0.001, D5cc: ART (2051.96) vs IGRT (2273.93), p = 0.015, D10cc: ART (1650.73) vs IGRT (1731.74), p = 0.211. For the small bowel: D0.5cc: ART (3022.3) vs IGRT (3142.64), p = 0.037. D5cc: ART (2151.09) vs IGRT (2389.15), p = 0.043, D10cc: ART (1775.20) vs IGRT (1942.00), p = 0.079. For the stomach: D0.5cc: ART (3353.92) vs IGRT (4117.85), p = 0.000, D5cc: ART (2860.20) vs IGRT (3235.41), p = 0.000, D10cc: ART (2553.72) vs IGRT (2836.73), p = 0.000. For the Dmean of the left kidney and right kidney: Left kidney: ART (248.28) vs IGRT (239.65), p = 0.100. Right kidney: ART (314.55) vs IGRT (307.17), p = 0.345. These results suggest significant improvements in PTV coverage and sparing of OARs with ART compared to IGRT, indicating the potential of ART in optimizing treatment outcomes for pancreatic cancer patients. Compared to conventional IGRT-guided SBRT programs, ART-based SBRT for pancreatic cancer not only enhances the dose distribution to the target volume but also mitigates the radiation exposure to critical organs-at-risk (OARs) such as the duodenum, small intestine, and stomach. This approach may offer a more favorable safety profile while concurrently enhancing treatment efficacy.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Addressing local disease in inoperable pancreatic cancer presents a significant clinical challenge, with up to one-third of patients experiencing progression of the tumor within the local region1. Presently, the standard approach to managing patients with unresectable locally advanced disease involves a combination of chemotherapy and radiotherapy2. However, the adjacent gastrointestinal tract, being sensitive to radiation, restricts the radiation dosage, leading to a high rate of local recurrence post-treatment.
Stereotactic body radiation therapy (SBRT) is an emerging RT technique because of its ability to deliver highly ablative radiation dose in several fractions3,4. Park et al. have demonstrated improved quality of life scores and manageable acute toxicity with a five-fraction SBRT regimen compared to intensity-modulated radiation therapy5. Despite its precision and accuracy, SBRT presents challenges in escalating prescribed doses without compromising safety. A significant factor is the variation in position and shape of the stomach and duodenum between fractions of radiotherapy, caused by changes in organ peristalsis and filling6.
Recent studies have shown promise for SBRT in local advanced pancreatic cancer, exhibiting higher local control rates compared to conventional segmental radiation therapy regimens3,7. However, the duodenum often serves as the dose-limiting organ in pancreatic SBRT, with potential severe toxicity if dose limits are exceeded9. Strategies to enhance radiation conformability and delivery accuracy include utilizing baseline markers in the tumor, minimizing margins on the target volume, employing intensity-modulated radiation therapy, and managing respiratory motion10,11,12. While these techniques optimize dose distribution, they do not fully account for the dynamic nature of the duodenum, which undergoes natural movement, expansion, contraction, and deformation daily due to peristalsis and changes in gastrointestinal contents13,14,15. Addressing these anatomical variations is crucial to minimizing toxicity in pancreatic cancer and abdominal SBRT.
At present, adaptive radiotherapy offers a promising approach to mitigate over-irradiation of organs at risks (OARs) and under-irradiation of the planning tumor volume (PTV) caused by daily anatomical changes. Adaptive radiotherapy encompasses both offline and online adaptive approaches, wherein the initial radiotherapy plan is adjusted based on changes in tumor size, morphology, and location to achieve adaptive irradiation for each fraction. There are multiple studies showing the efficacy of online adaptive RT with real-time online tracking using MR-LINAC administering ablative doses to pancreatic cancer. It needs to be emphasized that while there can be dosimetric superiority with advanced technology like MR-LINAC, it is not widely available and CT-based SBRT is more commonly used across the world16,17,18. Online adaptive radiotherapy involves scanning the patient’s radiotherapy area before each session to capture real-time changes in tumor and surrounding organs, allowing for adjustments to the treatment plan to maximize tumor destruction while protecting normal organs. In this study, SBRT was administered to pancreatic cancer patients using an online adaptive radiotherapy technique.
This study entails a retrospective analysis comparing the dose distribution in patients treated with online adaptive radiotherapy based on the United Imaging 506 C CT-Linac and United Imaging TPS, aiming to investigate the dosimetric advantages of adaptive radiotherapy in practice.
Materials and methods
Patients
After obtaining institutional review board approval, we conducted a retrospective review of medical records of all patients treated for upper abdominal malignancies at Zhongnan Hospital of Wuhan University between September 2021 and April 2022. The studies involving human participants were reviewed and approved by the Institutional Review Board of Zhongnan Hospital of Wuhan University. All patients/participants provided their written informed consent to participate in this study. All methods were performed in accordance with the relevant guidelines and regulations. Among them, 8 patients received pancreatic radiotherapy, and the radiation planning scans of these selected patients were conducted using 4D CT scans. Daily fan-beam CT (FBCT) scans of the pancreas were performed at the time of treatment, with patients positioned supine with SBRT body frame immobilization and arms raised above the head. The online ART flow chart was shown in Fig. 1.
IMRT planning
Using the initial radiotherapy CT scans, all patients underwent radiation treatment planning at the United Imaging KVCT-Linac workstation, prescribed as a 5-day SBRT session. A 9-field coplanar static intensity-modulated radiation treatment plan was employed, with a prescribed dose of 45 Gy. Standardized tumor and normal organ volumes were utilized for each patient, with the gross tumor volume (GTV) encompassing the pancreatic tumor. Among the 8 patients, 6 had pancreatic cancer, with 2 of them having tumors located in the head of the pancreas. The GTV, representing the visible extent of the tumor on imaging, was used to generate the planning tumor volume (PTV) by expanding 3 mm from the GTV. The prescribed dose for PTV-GTV was 45 Gy over 5 fractions19,20. The median PTV volume was 33 cm3 (range 14 to 67 cm3). Normal organs at risk included the duodenum, stomach, adjacent small intestine, kidney, liver, and spinal cord.
Online ART planning
Following patient setup, fan-beam CT (FBCT) was acquired as part of the online adaptive process. Deformable alignment was utilized to register the simulation CT to the FBCT. Normal organs were delineated using the co-image automatic contour system by the treatment planning system (TPS), with modifications to the gross tumor volume (GTV) performed by experienced clinicians post-deformable registration. The planning tumor volume (PTV) was generated by expanding 3 mm from the GTV. Online adaptive radiotherapy (ART) plans were automatically generated on FBCT using TPS algorithms, which underwent evaluation by physicists and clinicians before being transmitted to the treatment terminal for FBCT guidance and treatment.
Evaluation indicators
The plans were evaluated for actual target coverage rate and sparing of organs at risk (OARs) for patients on both IGRT and ART plans. To obtain parameter values of IGRT plans, the treatment plan on the simulation FBCT was rigidly copied to the FBCT on each treatment day for dose calculation, representing the IGRT dose received by the patient in each treatment fraction. Dose parameters of each IGRT plan were statistically analyzed, and the average values of the final IGRT plans were obtained. Similarly, the average values of the final ART plans were obtained.
In this study, the dose and coverage of PTV and OARs were compared. Vx% was defined as the volume of the prescription dose line for x% including the volume of PTV or OAR, while Dx% represented the maximum dose of volume accepted by x% of PTV or OAR. The prescription dose covered more than 95% of PTV volume (D95 should be more than 45 Gy in this study). Additionally, the 35 Gy dose was required to be less than 0.5 cc for the duodenum, stomach, and adjacent small intestine, and less than 10 Gy on average for the kidneys.
Statistical analysis
Data were analyzed using the Statistical Package for Social Sciences version 22.0 (IBM Corporation, Armonk, NY, USA). The significance of differences between mean values was determined by paired bilateral T-test, with p values ≤ 0.05 considered statistically significant.
Results
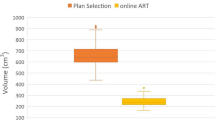
The average values of 8 patients were summarized in Tables 1 and 2. PTV parameters were shown in Table 3, and OAR parameters were shown in Table 4.
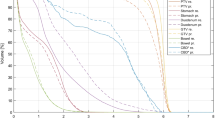
In this study, compared with the IGRT plan, the ART plan parameters showed significant improvements. Specifically, there were significant differences in V98, V95, V90, and Dmean (p < 0.05) for PTV parameters between the two groups. Additionally, significant differences were observed for all GTV parameters between the two groups (p < 0.05). The results were shown in Figs. 2 and 3.
In the duodenum, stomach, and small intestine, the IGRT-based SBRT plan exhibited higher values for D0.5 cc, D5cc, and D10cc compared to the ART plan parameters. Significant differences were observed in D0.5 cc, D1cc, and D5cc for the duodenum between the two groups (p < 0.05). Additionally, significant differences were found in D0.5 cc and D5cc for the small bowel between the two groups (p < 0.05). Moreover, significant differences were noted for all stomach parameters between the two groups (p < 0.05). The results were shown in Figs. 4, 5, 6 and 7.
In this study, we observed that the presence of air in the dilatable stomach significantly influenced the actual delivered radiation dose, as illustrated in Figs. 8, 9 and 10. During the positioning CT, gas was detected in the patient’s stomach; however, there was an absence of gas during the actual treatment sessions. This discrepancy resulted in a notable deviation when comparing the dose delivered by the Origin plan to that of the IGRT plan.
Discussion
This study highlights the dosimetric advantages of daily adaptive radiotherapy (ART) for pancreatic stereotactic body radiotherapy (SBRT) compared to image-guided radiation therapy (IGRT). The results indicate that online ART technology not only significantly improves target coverage but also reduces the dose to organs at risk (OARs), except for certain parameters related to the right kidney.
Our findings are consistent with studies from other institutions examining the impact of ART on pancreatic cancer. Researchers at the Medical College of Wisconsin conducted a similar study on patients receiving conventional fractionated radiation therapy for pancreatic cancer and observed a reduction in duodenal volume and dose with ART10,21. Similarly, our study found significant reductions in duodenal, small intestine, stomach, and liver doses with ART, corroborating previous findings. However, while our study achieved better protection in high-dose areas, certain parameters such as V20 were not significantly improved. This may be attributed to our focus on high-dose volume during daily radiotherapy planning, similar to studies on MR-guided daily adaptive radiotherapy for prostate cancer SBRT22. However, the relatively longer treatment time remains an issue, and a potential weakness of the MR‑guided daily‑adaptive, also when compared to conventional Cone Beam CT-based linear accelerators, where the usual delivery time is below 10 min21.
The discrepancy between ART and IGRT plans in the parameters related to the right kidney may be attributed to the optimization process during radiation therapy planning. Specifically, limitations in controlling the kidney’s V10 parameter during planning optimization may have contributed to differences in Dmean values between IGRT and ART plans.
Our study also found significant differences in PTV-GTV D95 and prescription dose coverage between IGRT and ART plans, suggesting that target volume displacement during IGRT treatment may have led to variability in dose coverage compared to simulation CT.
Offset of the target volume during IGRT treatment, particularly due to patient rotation, may have contributed to differences in target volume irradiation between IGRT and ART plans. This offset, while random, may have affected OARs differently depending on their proximity to the target volume.
An important finding of our study pertains to the dose effect of air within the gastrointestinal system, as illustrated in our figures. Air in the stomach could substantially alter the actual radiation dose delivered, posing challenges in radiation modalities with tighter depth dose distribution, particularly in the context of pancreatic cancer-associated gastritis and enteritis12,23.
Despite the promising results of pancreatic SBRT ART, several technical considerations must be addressed before clinical implementation. These include optimizing the time patients spend on the treatment table during ART, ensuring efficient image processing, and integrating respiratory gating into ART for accurate dose delivery. The small sample size is recognised as a limitation of this study. We are therefore we plan to increase the sample size and follow-up data in the upcoming research.
In conclusion, while our study demonstrates the potential of pancreatic SBRT ART, further research is needed to refine technical aspects and address challenges associated with image quality and respiratory motion integration.
Conclusion
In conclusion, our study underscores the potential benefits of daily adaptive radiotherapy (ART) in pancreatic stereotactic body radiotherapy (SBRT). ART shows promise in reducing radiation doses to organs at risk (OARs) such as the duodenum, small intestine, and stomach, while enhancing radiation doses to pancreatic tumors. This approach has the potential to minimize treatment-related toxicity and enhance tumor control in abdominal SBRT. Further research and clinical implementation of ART could lead to improved outcomes for patients with pancreatic cancer undergoing SBRT.
Data availability
The raw data supporting the conclusions of this article will be made available by the corresponding authors, without undue reservation.
References
Zarepisheh, M., Long, T., Li, N., Romeijn, E. & Jiang, S. A novel prior-knowledge-based optimization algorithm for automatic treatment planning and adaptive radiotherapy re-planning. Med. Phys.40(6), 530–530 (2013).
Men, C. et al. GPU-based ultrafast IMRT plan optimization. Phys. Med. Biol.54, 6565–73 (2009).
Koong, A. C., Le, Q. T., Ho, A., Fong, B. & Bastidas, J. A. Phase I study of stereotactic radiosurgery in patients with locally advanced pancreatic cancer. Int. J. Radiat. Oncol. Biol. Phys.58, 1017–21 (2004).
Yechieli, R. L., Robbins, J. R., Mahan, M., Siddiqui, F. & Ajlouni, M. Stereotactic body radiotherapy for elderly patients with medically inoperable pancreatic cancer. Am. J. Clin. Oncol.40, 22–26 (2017).
Park, J. J. et al. Stereotactic body radiation vs. intensity-modulated radiation for unresectable pancreatic cancer. Acta Oncol.56, 1746–1753 (2017).
Ermongkonchai, T. et al. Stereotactic radiotherapy and the potential role of magnetic resonance-guided adaptive techniques for pancreatic cancer. World J. Gastroenterol.28(7), 745–754 (2022).
Schellenberg, D., Goodman, K. A., Lee, F., Chang, S. & Kuo, T. Gemcitabine chemotherapy and single-fraction stereotactic body radiotherapy for locally advanced pancreatic cancer. Int. J. Radiat. Oncol. Biol. Phys.72, 678–86 (2008).
Chang, D. T. et al. Stereotactic radiotherapy for unresectable adenocarcinoma of the pancreas. Cancer115, 665–72 (2009).
Murphy, J. D. et al. A dosimetric model of duodenal toxicity after stereotactic body radiotherapy for pancreatic cancer. Int. J. Radiat. Oncol. Biol. Phys.78, 1420–6 (2010).
Minn, A. Y., Koong, A. C. & Chang, D. T. Stereotactic body radiation therapy for gastrointestinal malignancies. Front. Radiat. Ther. Oncol.43, 412–27 (2011).
Goldstein, S. D. et al. Use of respiratory-correlated fourdimensional computed tomography to determine acceptable treatment margins for locally advanced pancreatic adenocarcinoma. Int. J. Radiat. Oncol. Biol. Phys.76, 597–602 (2010).
Langendijk, J. A., Doornaert, P., Leeuw, V. D., Leemans, C. R. & Slotman, B. J. Impact of late treatment-related toxicity on quality of life among patients with head and neck cancer treated with radiotherapy. J. Clin. Oncol.26(22), 3770–3776 (2008).
Li, Y. et al. Dosimetric benefit of adaptive re-planning in pancreatic cancer stereotactic body radiotherapy. Med. Dosim.40(4), 318–24 (2015).
Boldrini, L. et al. Online adaptive magnetic resonance guided radiotherapy for pancreatic cancer: state of the art, pearls and pitfalls. Radiat. Oncol.14(1), 1–6 (2019).
Nishi, T. et al. Volume and dosimetric changes and initial clinical experience of a two-step adaptive intensity modulated radiation therapy (IMRT) scheme for head and neck cancer. Radiother. Oncol.106, 85–89 (2013).
Hanna, G. G. et al. Uk consensus on normal tissue dose constraints for stereotactic radiotherapy. Clin. Oncol.30, 5–14 (2018).
Brunner, T. B. et al. ESTRO ACROP guidelines for target volume definition in pancreatic cancer. Radiother. Oncol.154, 60–69 (2021).
Li, X. A. et al. Development of an online adaptive solution to account for inter- and intra-fractional variations. Radiother. Oncol.100, 370–4 (2011).
Nicosia, L. et al. Daily dosimetric variation between image-guided volumetric modulated arc radiotherapy and mr-guided daily adaptive radiotherapy for prostate cancer stereotactic body radiotherapy. Acta Oncol. (Stockholm, Sweden)60(1084), 1–7 (2020).
Kumagai, M. et al. Impact of intrafractional bowel gas movement on carbon ion beam dose distribution in pancreatic radiotherapy. Int. J. Radiat. Oncol. Biol. Phys.73, 1276–81 (2009).
Francesco, C. et al. Mitigation on bowel loops daily variations by 1.5-T MR-guided daily-adaptive SBRT for abdomino-pelvic lymph-nodal oligometastases. J Cancer Res Clin Oncol147(11), 1 (2021).
Lois, A. D. et al. Online adaptive MR-guided stereotactic radiotherapy for unresectable malignancies in the upper abdomen using a 1.5T MR-linac. Acta Oncol.61(1), 1 (2021).
Brigid, A. M. et al. Dose accumulation for MR-guided adaptive radiotherapy: From practical considerations to state-of-the-art clinical implementation. Front Oncol.12, 1 (2023).
Acknowledgements
The authors express their gratitude to the Department of Radiation and Medical Oncology at Zhongnan Hospital of Wuhan University. They also extend their appreciation to all colleagues for their assistance and guidance throughout the study.
Funding
This work is supported by National Key R&D Program of China, Ministry of Science and Technology of the People’s Republic of China. (Grant No. 2022YFC2407100, 2022YFC2407104) and the Science, Technology and Innovation Seed Fund of Zhongnan Hospital, Wuhan University (project number znpy2019022), Technology and Innovation Seed Fund of Zhongnan Hospital, Wuhan University (project number.
CXPY2023102).
Author information
Authors and Affiliations
Contributions
D.J.: Conception and design of the study; generation of treatment plans; drafting of the article; data analysis; final approval of the version to be published. J.P.: Conception and design of the study; drafting of the article; data analysis; final approval of the version to be published. H.X.: Drafting of the article; final approval of the version to be published. D.W.: Data analysis; drafting of the article. X.W.: Drafting of the article. C.X.: Drafting of the article. B.L.: Data analysis; drafting of the article. S.G.: Conception and design of the study; drafting of the figures; data analysis. C.W.: Conception and design of the study; drafting of the figures; data analysis. H.L.: Project design; drafting and final approval of the version to be published. All authors contributed to the article and approved the submitted version.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics statement
The studies involving human participants were reviewed and approved by the Institutional Review Board of Zhongnan Hospital of Wuhan University. All patients/participants provided their written informed consent to participate in this study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Jiang, D., Jin, P., Xu, H. et al. Online adaptive radiotherapy in stereotactic body radiotherapy for pancreatic cancer patients. Sci Rep 14, 22101 (2024). https://doi.org/10.1038/s41598-024-72831-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-72831-z
- Springer Nature Limited