Abstract
Handgrip strength (HGS) is a non-invasive and reliable biomarker of overall health, physical function, mobility, and mortality. This study aimed to investigate the possible relationship between HGS and mortality in older adult patients hospitalized with COVID-19 in the intensive care unit (ICU) by Alpha (B.1.1.7) and Delta (B.1.617.2) variants. This retrospective cohort study was conducted on 472 COVID-19 patients (222 female and 250 male) aged 60–85 years admitted to the ICU. Demographic data, underlying comorbidities, COVID-19-related symptoms, as well as laboratory and computed tomography (CT) findings were obtained from the patient’s medical records. Using a JAMAR® hydraulic dynamometer, the average grip strength value (kg) after three measurements on the dominant side was recorded for subsequent analysis. Low grip strength (LGS) was defined as an arbitrary cut-off of two standard deviations below the gender-specific peak mean value of normative HGS in Iranian healthy population, i.e. < 26 kg in males and < 14 kg in females. The findings showed lower mean grip strength and high frequency of LGS in the non-survivors patients versus survivors group and in the Delta (B.1.617.2) variant vs. Alpha (B.1.1.7) variant, respectively (both p < 0.01). The binary logistic regression analysis showed that chronic obstructive pulmonary disease (COPD) (adjusted odds ratio [OR] 5.125, 95% CI 1.425–25.330), LGS (OR 4.805, 95% CI 1.624–10.776), SaO2 (OR − 3.501, 95% CI 2.452–1.268), C-reactive protein (CRP) level (OR 2.625, 95% CI 1.256–7.356), and age (OR 1.118, 95% CI 1.045–1.092) were found to be independent predictors for mortality of patients with Alpha (B.1.1.7) variant (all p < 0.05). However, only four independent predictors including COPD (OR 6.728, 95% CI 1.683–28.635), LGS (OR 5.405, 95% CI 1.461–11.768), SaO2 (OR − 4.120, 95% CI 2.924–1.428), and CRP level (OR 1.893, 95% CI 1.127–8.692) can be predicted the mortality of patients with Delta (B.1.617.2) variant (p < 0.05). Along with the well-known and common risk factors (i.e. COPD, CRP, and SaO2), handgrip strength can be a quick and low-cost prognostic tool in predicting chances of mortality in older adults who are afflicted with COVID-19 variants.
Similar content being viewed by others
Introduction
The pandemic coronavirus infectious disease (COVID-19), caused by the SARS-CoV-2 virus, has had a catastrophic effect on the global economy and health, resulting in approximately 7 million deaths worldwide1. Recent studies have shown that age, gender, smoking, underlying comorbidities, and COVID-19 variant types were considered possible predictors of disease severity and mortality in COVID-19 patients admitted to the hospital2,3. There is growing evidence that COVID-19 patients with underlying cardiovascular disease (CVD), chronic obstructive pulmonary disease (COPD), and escalation of T-troponin levels are more susceptible to a fatal outcome4. Several studies have concluded that the two primary variants, namely Alpha (B.1.1.7) and Delta (B.1.617.2), have an increased risk of hospitalization, ICU admission, and mortality in comparison to the initial virus5,6. The study conducted by Zali et al.7 and Safari et al.8 documented that the Alpha and Delta variants caused the highest number of hospitalizations and high mortality.
Although all ages can be affected, adults aged 60 years and older could be more susceptible to developing severe infection, with a higher risk of morbidity and mortality9,10. A meta-analysis of 59 studies with 36,470 patients showed that patients aged 70 years and older have an approximately 65% higher risk of severe COVID-19 disease (95% CI 1.50–1.81)11. Similarly, the study by Guan et al.12 on hospitalized patients in 30 provinces in China diagnosed with COVID-19 showed that the proportion of mortality in COVID-19 patients over 60 years old accounts for 81% of the total mortality. Based on current evidence in older adults, an imbalance between catabolic and anabolic processes leads to the activation of the ubiquitin–proteasome system, myocyte apoptosis, and the autophagy-lysosome pathway, and thus creates higher levels of inflammatory mediators such as tumor necrosis factor (TNF)-α, interleukin (IL)-1β, IL-6, and C-reactive protein13,14,15. These cytokines can reduce muscle protein synthesis and increase muscle degradation and muscle wasting in older adults16,17. The frailty and reduced muscle force-exertion in older adults with acute and inflammatory lung disease are considered strong reasons for causing malfunction of respiratory muscles, long-term stay in ICU, and eventually deteriorating quality of life and possible mortality18,19.
Handgrip strength (HGS) is considered to be a non-invasive, simple, and reliable indicator of muscle strength, physical function, and overall body health20,21,22,23,24,25. HGS is an even stronger prognostic marker of functional recovery, muscular impairment, whole-body resilience to the aging process26,27. The use of HGS has been recommended as an appropriate supportive measure for the assessment of the overall health of individuals by the Global Leadership Initiative on Malnutrition (GLIM) and the second European Working Group on Sarcopenia in Older People (EWGSOP2)28,29. It is well documented that low grip strength (LGS) is associated with age-related loss of muscle mass, disease severity, longer hospital stays, the development of frailty, sarcopenia, and muscle dystrophy18,30. Kara et al.31 indicated that hospitalized COVID-19 patients with low HGS had three times higher risk for developing pneumonia than patients with high HGS.
However, the hypothesis that low HGS could predict mortality in older adults with COVID-19 admitted to ICU has not been examined to date. On the other hand, the investigation into muscle strength in COVID 19 patients with either of variant types may add a significant insight into how such biomechanical biomarkers provide further evidence in prognostic of the older patients when infected with COVID-19 variants. To our knowledge, along with the other clinical risk factors, the current research work can be considered one of the few studies in the field of clinical medicine and physical ergonomics to objectively assess handgrip strength among older adult patients who are hospitalized with COVID-19 in the ICU in terms of Alpha (B.1.1.7) and Delta (B.1.617.2) variants.
Material and methods
Study design and ethics
The present study and its findings are part of a retrospective multicentric cohort study conducted to investigate the long-term consequences of COVID-19 and its impact on overall health, physical performance, and quality of life (all the measurement data along with CT imaging information was obtained retrospectively). The study protocol was reviewed and approved by the Research and Ethics Committee of Shahid Beheshti University of Medical Sciences (Ethics ID: IR.SBMU.PHNS.REC.1402.087). All methods in this study were carried out in accordance with the relevant guidelines and regulations, and all data in this study were obtained with informed consent from all participating patients and/or their legal guardian(s).
Patient selection
As a multidisciplinary approach to evaluate the long-term consequences of COVID-19 infection32,33,34, electronic medical records were reviewed to identify and pick all appropriate elderly participants patients for the study.
The inclusion criteria were as follows: (1) aged 60 or older, (2) having a laboratory-confirmed SARS-CoV-2 infection (as determined by real-time reverse transcriptase-PCR assays of nasal and pharyngeal swabs), (3) no fracture/deformity/surgery in upper extremities during the past year, (4) no neuromuscular or rheumatic diseases affecting the handgrip strength measurements, and (5) admitted to intensive care unit (ICU) between April and September 2021 based on clinical symptoms stated in World Health Organization (WHO) guidelines issued for COVID-19 patients, including clinical signs of pneumonia (fever, cough, dyspnea, and tachypnea) together with a respiratory rate > 30/min, oxygen saturation (SpO2) ≤ 80%, and extensive lung involvement in CT (CT score > 11) on room air35. In the present study, the average nurse-to-patient ratio for ICU was 1:2–1:3, which is almost consistent with the ratio of 1:2 recommended for a medical ICU36,37.
Based on lineage information38, the infection was deemed to be Alpha if it had the N501Y mutation and lacked the E484K mutation; Delta if it had the critical D614G, L452R, P681R, T478K, and K417N genetic mutations in the S-protein39,40,41,42,43,44.
Exclusion criteria were (1) unconscious patients during ICU admission, (2) patients who required “mechanical ventilation and tracheostomy” at any stage of the study (3) patients without a CT scan during hospitalization, and (4) patients with appendicular skeletal muscle mass index score < 7.0 kg/m2 and < 5.4 kg/m2 for men and women, respectively, or whom were already diagnosed with sarcopenia, based on the Asian working group for sarcopenia45.
Demographic and clinical characteristics
Demographic data, smoking status, comorbidities (e.g. hypertension, obesity, diabetes mellitus (DM), hypothyroidism, cardiovascular disease (CVD), bronchial asthma, chronic obstructive pulmonary disease (COPD), and cancer), COVID-19-related symptoms (cough, fever (> 37.8 °C), myalgia, dyspnea, anosmia/ageusia, and diarrhea), and clinical markers values (C-reactive protein, ferritin, D-dimer, SaO2, white blood cell (WBC), thrombocyte, lymphocyte, neutrophil, and hemoglobin) were obtained from the medical records of the patients. At ICU admission, if the doctor suspected that patient participants were suffering from COPD, he may recommend one or more of the tests including chest x-ray, CT scan, and arterial blood gas analysis. Participants’ stature (cm) and body mass (kg) were measured at ICU admission using the Holtain Harpenden stadiometer (Holtain, Crosswell, UK) and a digital balance (Toledo, Model 2096PP/2, Inc., Brazil), respectively, with light clothing but no shoes. Body mass index (BMI) was calculated as kg/m2 and classified into four groups: underweight (BMI < 18.5), healthy weight (18.5–24.9), overweight (25.0–29.9), and obese (> 30)46.
Computed tomography (CT)
The patients’ CT scans were obtained in a supine position at the end of inspiration47, using a GE Brightspeed 16-Slice CT Scanner (GE Healthcare, Chicago, Illinois, United States). The CT findings were evaluated by a radiologist (A. A.) with 15 years of experience in terms of the presence of infiltration patterns as ground-glass opacities (GGO), GGO with consolidation, consolidation, and other (linear opacities, traction bronchiectasis, cysts, and reticular opacities) for each patient’s initial chest CT scan48. The anatomic distribution of the infiltrations was given to the predominant imaging findings in each zone on CT (3 lobes in the right upper, middle, and lower, and 2 lobes in the left upper and lower). Then, a semi-quantitative CT severity scoring system [0 = no anatomic involvement, 1(< 5%), 2(5–25%), 3(26–50%), 4(51–75%), and 5(> 75%)] for quantifying radiological findings in each lobe49,50 was applied. According to the aforementioned scoring system guidelines, all patients admitted to ICU had a higher than 11 CT score.
Handgrip strength
The maximal isometric grip strength was measured in kilograms by the JAMAR® hydraulic dynamometer (Saehan Corporation, Masan-Korea) in the first 24 h of ICU admission and every 7 days, following standard guidelines and procedures presented in previous studies51. Before starting the test, hand dominance was determined by asking participants the following question: "Which hand do you write with?". Measurements were made in a sitting posture, with feet on the floor, arms hanging relaxed at the side and neutrally rotated, elbows flexed 90°, and forearm and wrist in a neutral position (0°–15° of extension and 0°–15° of ulnar deviation)52. The participants performed one repetition in the dominant hand to familiarize themselves with the dynamometer and the test process. The participants were asked to exert their maximal voluntary contraction (MVC) on the dynamometer for 3 s. Three measurements were taken from each patient on each visit (with a 1-min rest time between each exertion) and their average value was considered for subsequent analysis. Verbal encouragement was provided to ensure maximal effort during each test. If one of the measurements had a difference higher than 10% compared to other measurements, it was canceled and replaced by a consecutive measurement22. The JAMAR® hydraulic dynamometer display was reset manualy to zero after each trial.
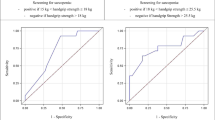
Hand strength is influenced by gender53,54,55, we used sensitivity analysis to determine the optimal handgrip strength cut-off for males and females. Low grip strength (LGS) was determined based on the standard approach provided by Dodds et al.56. LGS was defined as an cut-off of two standard deviations below the gender-specific peak means the value of normative HGS in the Iranian healthy population20, i.e. < 26 kg in males and < 14 kg in females.
Descriptive analysis
Statistical analysis was performed by SPSS 23 (IBM Corporation, New York, NY, United States). The normality test was carried out using the Kolmogorov–Smirnov test for all data sets. Statistical outliers were checked using Grubb’s test which is based on the difference between the mean of the sample and the most extreme data considering the standard deviation57. Relative and absolute reliability were assessed for the grip strength test using the Intra-class Correlation Coefficient (ICC) and standard error of the measurement (SEM), respectively. Basic descriptive statistics such as means ± standard deviation (SD), min–max, and number (percentage) were calculated for clinical and demographic characteristics as well as chest CT scores. An independent sample t-test was carried out to determine the differences in clinical characteristics between males and females. One-way ANOVA test (with Tukey post-hoc test) and Chi-square or Fisher’s exact tests were used to compare the numerical and categorical variables, respectively. Sensitivity analyses were also conducted within subgroups of patients to investigate potential sources of heterogeneity and assess the robustness of the main conclusions. If the results of the sensitivity analyses were consistent with the primary results, we are confident that the assumptions made for the primary analysis had little effect on the results, giving strength to the study findings.
For binary logistic regression analysis (with backward likelihood ratio selection), COVID-19 patients admitted to the ICU were categorized into two groups deceased and non-deceased. For predicting mortality, demographic and significant clinical variables were taken into analysis. The statistical significance was set at p < 0.05.
Results
The sample consisted of 472 COVID-19 patients aged between 60 and 85 years old; 250 (53%) males and 222 (47%) females. The mean age for males and females was 76.1 ± 5.6 and 74.4 ± 6.4 years, respectively. According to variant type, 197 and 275 elderly patients with the Alpha (B.1.1.7) and Delta (B.1.617.2) variants were hospitalized in the ICU, respectively. A flowchart presenting the sampling procedure is presented in Fig. 1. It could be seen, that the handgrip strength of 2907 out of 3379 patients was not recorded due to the respected inclusion and exclusion criteria.
Clinical and demographic characteristics
Table 1 shows the clinical and biomechanical biomarkers and demographic characteristics of COVID-19 patients according to variant type as well as survived/deceased. In total, 244 patients died (157 males and 87 females), resulting in a high mortality rate of 51.7% (62.8% and 39.2% for males and females, respectively). To learn about clinical causes of death, we assessed the legal death certificates of the 244 decedents. The most frequent causes of death, documented in 154 cases (63.1%), were infection-related and included sepsis, septic shock, or sepsis-related multi-organ failure in 97 cases (39.8%), bacterial infections in 32 cases (13.1%), and viral pneumonia in 25 cases (10.2%). The second most common were respiration-related causes of death, documented as respiratory insufficiency, COVID-19 pneumonia, hypoxia, or acute respiratory distress syndrome (ARDS) in 60 cases (24.6%). Further individual immediate causes of death were pulmonary embolism, cardiovascular failure, and cancer in 30 cases (12.3%). In a general view, the most frequent symptoms and comorbidities of the COVID-19 patients as well as the significance of differences can be seen at the 0.05 level (P-values under 0.05 are shown in bold).
Mean handgrip strength values were lower and the frequency of low grip strength was higher in the deceased patients versus the survived group and Delta (B.1.617.2) variant versus Alpha (B.1.1.7) variant (both p < 0.01). Participants showed high to very high test–retest reliability for the Jamar dynamometer (0.87 ≤ ICC ≤ 0.92; P ≤ 0.001; n = 50 subjects out of the total sample).
Considering that 30–50% of COVID-19 patients had myalgia and their HGS was lower, we performed sensitivity analysis as well as robustness analyses based on rare-events logistic regression in this subgroup of patients. Sensitivity analysis showed that the main results did not change despite the presence of COVID-19 patients who had myalgia (OR 0.60, 95% CI 0.40–0.91, p = 0.016).
Mean differences in HGS by variant type, gender, age group, and survived/deceased
Figure 2 shows the trend of mean HGS for older male and female patients admitted to ICU in terms of variant type and survived/deceased. In general, a significant difference was observed between the HGS of deceased and survived male/female patients in both variants. Figure 2a demonstrated that HGS of older male patients who died from the Delta (B.1.617.2) variant was lower than their counterparts who died from Alpha (B.1.1.7) variant (by about 15–25%, where the highest difference was observed in the older male patients aged 80–85 years). At the same time, the HGS of older male patients who survived from Delta (B.1.617.2) variant was lower than their counterparts who survived from Alpha (B.1.1.7) variant (12–22%, where the highest difference was observed in the 75–79 age group).
A similar pattern can be seen for older female patients in Fig. 2b. Similar to older male patients, the HGS of older female patients who died from the Delta (B.1.617.2) variant was lower than their counterparts who died from the Alpha (B.1.1.7) variant (5–18%, where the highest difference was observed in the 60–64 age group). Whereas, the HGS of older female patients who survived from the Delta (B.1.617.2) variant was lower than their counterparts who survived from the Alpha (B.1.1.7) variant (10–20%, where the highest difference was observed in the older female patients aged 70–74 years).
Binary logistic regression analyses for predicting mortality
“Initially, 30 variables listed in Table 1 were mapped into the model. All factors were tested using the Variance Inflation Factor (VIF) test58 and the correlation matrix. As a result, 19 independent variables were included in the model, which includes age, gender, BMI, smoking status, LGS, hypertension, D-dimer, Ferritin, SaO2, C-reactive protein, cardiovascular disease, COPD, bronchial asthma, thrombocyte, lymphocyte, hemoglobin, diabetes mellitus, WBC, neutrophil. However, the step-wise analysis gave the best-fitted model including five and four variables, which are found to have significance for mortality of patients with Alpha (B.1.1.7) and Delta (B.1.617.2) variants, respectively (Table 2). The insignificant value of Hosmer-Lemeshow’s goodness of fit guides us to accept the null hypothesis, i.e., no difference between observed and model-predicted values.”
Table 2 shows the results of binary logistic regression analyses for both Alpha (B.1.1.7) and Delta (B.1.617.2) variants as non-survivors versus survivors. Among the patients with the Alpha (B.1.1.7) variant, low grip strength was found in 40 (50.6%) and 32 (27.1%) patients of the non-survivors and survivors groups, respectively (p < 0.001). For the Delta (B.1.617.2) variant, low grip strength was present in 79 (47.9%) and 33 (30%) patients in the non-survivors and survivors groups, respectively (p < 0.001). When age, gender, BMI, smoking status, presence of comorbidities, low grip strength, and abnormal laboratory findings were taken into analyses (Table 2); COPD, LGS, SaO2, CRP level, and age were found to be independent predictors for mortality of patients with Alpha (B.1.1.7) variant (all p < 0.05). However, the findings of the present study depicted that only four independent predictors including COPD, LGS, SaO2, and CRP level can predict the mortality of patients with Delta (B.1.617.2) variant (p < 0.05). Also, the findings of the present study showed that COVID-19 patients with the Delta variant had far more muscle weakness, severe chronic obstructive pulmonary disease (COPD), and lower CRP level and SaO2 than COVID-19 patients with the Alpha variant (all p < 0.05).
Discussion
In this retrospective cohort study, we aimed to evaluate the HGS among older adult patients with COVID-19 infection admitted to ICU in terms of Alpha (B.1.1.7) and Delta (B.1.617.2) variants and investigate the possible relationship between HGS and mortality among them. To the best of our knowledge, this is the first study to demonstrate the prognostic value of muscle strength in older adult patients who died due to the Alpha (B.1.1.7) and Delta (B.1.617.2) variants of COVID-19 infection.
Age, BMI, gender, and smoking effects
The relationship between age and COVID-19 mortality was linear, following the same pattern reported in the majority of previous studies12,59, meaning that mortality rates increased steeply in patients aged 60 and higher, regardless of variant type. It is documented that aging is associated with decreased levels of dehydroepiandrosterone, testosterone, insulin-like growth factor I (IGF-I), and estrogen hormones that regulate muscle mass60. Indeed, the chronic elevation of inflammatory biomarkers such as IL-6, TNF-α, and CRP in older adults ≥ 65 years leads to anabolic resistance during the infectious pandemic, and as a result muscle protein synthesis (MPS) is reduce61. This is related to the higher rates of ICU stay with a large and diverse group of underlying disorders including CVD, COPD, diabetes mellitus, cancer, sarcopenia, cachexia, lower quality of life, and mortality rate in older adults ≥ 65 years62.
Although it has been reported that obesity is a contributing factor to COVID-19 mortality63,64, in the current study none of the participants were considered obese as they did not have a BMI larger than or equal to 30 and less than 8% of them were in the “overweight” group with 25 ≤ BMI ≤ 29.9. Our findings indicated that older adult patients with 25 ≤ BMI ≤ 29.9 (overweight) had a higher mortality rate than patients with a healthy weight, inconsistent with previous studies65,66. The higher mortality among overweight older adults may be attributed to reduced chest wall compliance, respiratory muscle strength, leading to airway narrowing and peripheral airway blockage65.
Our results supported the previous COVID-19 studies conducted globally, indicating a male bias in COVID-19 mortality with a higher mortality rate for males than females67,68. More precisely, the present study found that the mortality rate was 1.6 times higher for older males than older females hospitalized with COVID-19 in the ICU. Additionally, a higher rate of risky behaviors (i.e., smoking, alcohol consumption, etc.) and higher existence of comorbidities (i.e., CVD, diabetes, hypertension, and cancer, etc.) in males than females have been considered other reasons for higher COVID-19 severity and mortality69,70.
In line with the previous studies71,72, the present study showed that the mortality rate was 1.5 times higher for older smokers than older non-smokers hospitalized with COVID-19 in the ICU, regardless of the variant type. A recent meta-analysis confirmed that smokers have 1.9 times the odds of progression in COVID-19 severity than patients who have never smoked73. Robust evidence shows that smoking can reduce the ability of macrophage cytokines to defend the host against virulent infections and almost double the risk of developing tuberculosis infection due to impaired immune function74.
Underlying comorbidities and clinical symptoms effects
The results of the present study reflected that COVID-19 disproportionately endangers older adult patients, especially those with at least one underlying comorbidity75. The most common COVID-19-related symptoms in the present study were fever (64.0%), cough (49.8%), myalgia (47.0%), and dyspnea (43.6%), consistent with the pertinent studies76,77. As seen in our patients, regardless of the variant type, studies indicate that older patients aged ≥ 60 years with underlying comorbidities such as hypertension, DM, obesity, bronchial asthma, COPD, and CVD mainly experience more serious consequences and even higher mortality in the ICUs78,79. The present study findings showed that hypertension (40.5%), diabetes mellitus (21.6%), cardiovascular disease (19.7%), and hypothyroidism (13.1%) were the most common comorbidities among the deceased older adult patients, respectively. In particular, the SARS-CoV-2 antigens can directly lead to adverse kidney and heart function in patients by infecting tubular epithelial cells of the kidney and pluripotent stem cell-derived cardiomyocytes, respectively80. A step further, binary logistic regression analysis showed that only COPD was the most important underlying disease predicting mortality in older adult patients with both Alpha (B.1.1.7) and Delta (B.1.617.2) variants. Emerging evidence has shown that the level of ACE2 expression is associated with the severity of COPD caused by the SARS-CoV infection and mediates the production of IL-6, IL-8, and IL-10 cytokines associated with acute respiratory distress syndrome81.
Our study revealed that high levels of CRP, ferritin, D-dimer, WBC, and neutrophils were associated with high mortality rates due to COVID-19 in older adults. Likewise, the deceased patients had lower SaO2, thrombocyte, and hemoglobin levels than the surviving patients, regardless of variant type. These results corroborated the earlier findings of Yang et al.14 and She et al.19, in which abnormal clinical and lab findings were commonly stated concerning higher severity of the COVID-19 infection and mortality, especially in the older ages. However, our binary logistic regression model showed that among biological parameters, only elevated CRP and decreased SaO2 levels were independently associated with COVID-19 mortality in hospitalized patients in the ICU. Vetrugno et al.82 stated that despite the effect of invasive or non-invasive ventilation in improving SaO2 levels, it can increase the risk of barotrauma, as an independent factor in increasing mortality in mainly patients with more severe COVID-19 disease.
Low grip strength effect
Our findings have shown that other than well-known and common clinical risk factors, LGS should be considered as an independent/complimentary predictor of mortality in older adult patients with COVID-19. The present study revealed that deceased patients (in both genders) had lower grip strength and higher frequency of LGS as compared to survived ones. Our findings showed that low grip strength independently increased COVID-19 mortality by up to five times. In line with the present study, Kara et al. (2021) study on COVID-19 patients aged 21–74 years showed that the LGS increases the risk of severe disease about three times31. Sevilla et al.83 concluded that low grip strength independently increased the length of ICU stay and 30-day mortality at older ages. Msigwa et al.84 proposed that increased protein turnover in patients with COVID-19, as a response to massive proteolytic stimuli, can cause direct muscle inflammation by equine coronavirus (ECoV) particles and immune-mediated muscle injury. Several recent studies have shown that declining muscle mass such as observed in severe COVID-19 infection is associated with lower levels of testosterone and IGF-I, which are introduced as contributors to muscle loss85,86. In addition, it has been shown that isolation/quarantine or hospitalization due to the COVID-19 pandemic accelerates the decline in isometric and concentric strength, the number and size of muscle fibers, physical abilities, and severity of disease symptoms in older adult patients aged ≥ 65 years62,87. Poor muscle strength in older patients is primarily due to the selective atrophy of type II fibers and can adversely affect motor control and respiratory functions and lead to poor immune response and metabolic stress when facing chronic infectious diseases88,89. As HGS is a biomarker of muscle strength and sarcopenia90, it can be used as a prognostic factor for mortality among older adult patients with COVID-1991. Therefore, patients with low HGS on ICU admission should be closely monitored to plan interventions and treatments in time and avoid or reduce the health deterioration trends in older adults.
A comparison of Alpha (B.1.1.7) and Delta (B.1.617.2) variants
In the present study, the mortality rate of older adult patients admitted to ICU was increased in the Delta (B.1.617.2) variant than in the Alpha (B.1.1.7) variant. When all variables were evaluated together on binary logistic regression, COPD, LGS, SaO2, CRP, and age were found to be independent predictors for mortality in older adult patients with the Alpha (B.1.1.7) variant. Likewise, COPD, LGS, SaO2, and CRP were obtained as independent predictors for mortality in older patients with the Delta (B.1.617.2) variant. However, the present study showed a higher adjusted odds ratio (OR) between these independent predictors and mortality of older adult patients admitted to the ICU in the Delta variant than the Alpha strain. In terms of LGS, in particular, Salleh et al.92 concluded that viral fitness through effective mutation on spike proteins of the Delta variant and improved binding affinity to ACE2 have been linked to poor motor and respiratory function and high mortality in patients infected with Delta variant.
This study had several strengths. This is the first study to examine the COVID-19 variant differences in handgrip strength of older adults hospitalized with COVID-19 in the ICU and the possible relationship between HGS and mortality, underlying risk factors, and health conditions. Also, the collection of various data, such as body composition variables (weight, height, BMI, HGS) and clinical markers values (C-reactive protein, ferritin, D-dimer, SaO2, WBC, thrombocyte, lymphocyte, neutrophil, and hemoglobin), as well as daily monitoring of patients by clinicians, were performed based on evidence-based clinical practice guidelines.
The current investigation has a few limitations to note. First, the current study does not include any information on the quality of life (QOL) of COVID-19 patients, despite the significant association of HGS and QOL in critically ill COVID-19 patients at long-term follow-up. Second, several variables such as dietary habits, lifestyle, physical activity, anthropometric data, maturity stages, the effects of other COVID-19 variants, and SARS-CoV-2 vaccination were not considered, which can be regarded as a reasonable limitation due to the potential for misinterpretation. Third, the absence of obese elderly patients and the lack of adequate effort by patients while gripping the dynamometer, which can reduce the generalizability of the present study, however, the number of elderly obese patients in Iran is standing between 9 and 10% and therefore, this study still is valid and may consider generalized as the number of Iranian elderly who fall in this category is still over 85%. Fourth, we do not have detailed information about the oxygen intake process of each patient, as well as its effect on the improvement of neuromotor control and muscle strength. Therefore, it is recommended that in future studies an oxygen mask is utilized whenever HGS is measured and use caution to normalize SaO2 (Oxygen saturation) through O2 cannula. Also, we excluded many patients based on inclusion criteria, so this may be biased against real-world performance and more comprehensive data may be needed to better verify the role of HGS biomarker in predicting mortality in COVID-19 patients. Nevertheless, our results were significant enough to demonstrate the importance of the handgrip strength test.
Conclusions
The present study advances our knowledge about the prevalence and prognostic implications of low grip strength (LGS) in older adult patients hospitalized with COVID-19 in the ICU. Along with the well-known clinical and laboratory risk factors including age, COPD, CRP, and SaO2, handgrip strength—the vital sign of the neuromuscular status—can be used as a quick and low-cost prognostic tool in the COVID-19 mortality of older adults. Our study suggests that low grip strength may serve as a potential risk factor helping clinicians in early diagnosis, stratification, and initial follow-up of older patients with COVID-19 infection. Such a process will enhance the effectiveness of clinical practice and interventions during the pandemic and will reduce the wastage of financial and human resources.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
Sharma, A., Tiwari, S., Deb, M. K. & Marty, J. L. Severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2): A global pandemic and treatment strategies. Int. J. Antimicrob. Agents. 56(2), 106054 (2020).
Nassar, Y. et al. Outcomes and risk factors for death in patients with coronavirus disease-2019 (COVID-19) pneumonia admitted to the intensive care units of an Egyptian University Hospital. A retrospective cohort study. J. Infect. Public Health 14(10), 1381–1388 (2021).
Abate, S. M., Assen, S., Yinges, M. & Basu, B. Survival and predictors of mortality among patients admitted to the intensive care units in southern Ethiopia: a multi-center cohort study. Ann. Med. Surg. 65(5), 102318 (2021).
Pranata, R. et al. Effect of chronic obstructive pulmonary disease and smoking on the outcome of COVID-19. Int. J. Tuberc. Lung. Dis. 24(8), 838–843 (2020).
Dhar, M. S. et al. Genomic characterization and epidemiology of an emerging SARS-CoV-2 variant in Delhi, India. Science 374(6570), 995–999 (2021).
Bast, E., Tang, F., Dahn, J. & Palacio, A. Increased risk of hospitalisation and death with the delta variant in the USA. Lancet Infect Dis. 21(12), 1629–1630 (2021).
Zali, A. et al. Mortality among hospitalized COVID-19 patients during surges of SARS-CoV-2 alpha (B. 1.1. 7) and delta (B. 1.617. 2) variants. Sci. Rep. 12(1), 18918 (2022).
Safari, I. & Elahi, E. Evolution of the SARS-CoV-2 genome and emergence of variants of concern. Arch. Virol. 167(2), 293–305 (2022).
Zhang, J., Dong, X., Liu, G. & Gao, Y. Risk and protective factors for COVID-19 morbidity, severity, and mortality. Clin. Rev. Allergy Immunol. 64(1), 90–107 (2023).
Mattiuzzi, C. & Lippi, G. Efficacy of COVID-19 vaccine booster doses in older people. Eur. Geriatr. Med. 13(1), 275–278 (2022).
Pijls, B. G. et al. Demographic risk factors for COVID-19 infection, severity, ICU admission and death: a meta-analysis of 59 studies. BMJ Open. 11(1), e044640 (2021).
Guan, W. et al. Clinical characteristics of coronavirus disease 2019 in China. N. Engl. J. Med. 382(18), 1708–1720 (2020).
Puthucheary, Z. A. et al. Acute skeletal muscle wasting in critical illness. Jama 310(15), 1591–1600 (2013).
Yang, X. et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: A single-centered, retrospective, observational study. Lancet Respir. Med. 8(5), 475–481 (2020).
Tang, Y. et al. Cytokine storm in COVID-19: The current evidence and treatment strategies. Front. Immunol. 11(4), 1708 (2020).
Files, D. C. et al. Lung injury-induced skeletal muscle wasting in aged mice is linked to alterations in long chain fatty acid metabolism. Metabolomic 12(134), 1–16 (2016).
Zhou, J., Liu, B., Liang, C., Li, Y. & Song, Y.-H. Cytokine signaling in skeletal muscle wasting. Trends Endocrinol. Metab. 27(5), 335–347 (2016).
Ali, A. M. & Kunugi, H. Physical frailty/sarcopenia as a key predisposing factor to coronavirus disease 2019 (COVID-19) and its complications in older adults. BioMed 1(1), 11–40 (2021).
She, Q. et al. Frailty pathogenesis, assessment, and management in older adults with COVID-19. Front. Med. 8(7), 694367 (2021).
Rostamzadeh, S., Saremi, M. & Bradtmiller, B. Age, gender and side-stratified grip strength norms and related socio-demographic factors for 20–80 years Iranian healthy population: Comparison with consolidated and international norms. Int. J. Ind. Ergon. 80(6), 103003 (2020).
Rostamzadeh, S., Saremi, M. & Tabatabaei, S. Normative hand grip strength and prediction models for Iranian office employees. Work 62(2), 233–241 (2019).
Saremi, M., Rostamzadeh, S. & Nasr, E. M. Hand functionality in dentists: The effect of anthropometric dimensions and specialty. Int. J. Occup. Saf. Ergon. 28(3), 1473–1481 (2021).
Rostamzadeh, S. et al. Analysis of hand-forearm anthropometric components in assessing handgrip and pinch strengths of school-aged children and adolescents: A partial least squares (PLS) approach. BMC Pediatr. 21(1), 1–12 (2021).
Ekiz, T., Kara, M. & Özçakar, L. Measuring grip strength in COVID-19: A simple way to predict overall frailty/impairment. Hear Lung. 49(6), 853–854 (2020).
Saremi, M. & Rostamzadeh, S. Hand dimensions and grip strength: A comparison of manual and non-manual workers. In Congress of the International Ergonomics Association (eds Bagnara, S. et al.) 520–529 (Springer, 2019).
Rantanen, T. et al. Midlife muscle strength and human longevity up to age 100 years: A 44-year prospective study among a decedent cohort. Age (Omaha) 34(3), 563–570 (2012).
Leong, D. P. et al. Prognostic value of grip strength: Findings from the prospective urban rural epidemiology (PURE) study. Lancet 386(9990), 266–273 (2015).
Cederholm, T. et al. GLIM criteria for the diagnosis of malnutrition–a consensus report from the global clinical nutrition community. J. Cachexia Sarcopenia Muscle 10(1), 207–217 (2019).
Cruz-Jentoft, A. J. et al. Sarcopenia: Revised European consensus on definition and diagnosis. Age Ageing 48(1), 16–31 (2019).
Grigioni, S. et al. Low thoracic skeletal muscle index is associated with negative outcomes in 244 patients with respiratory COVID-19. Clin. Nutr. 42(2), 102–107 (2023).
Kara, Ö., Kara, M., Akın, M. E. & Özçakar, L. Grip strength as a predictor of disease severity in hospitalized COVID-19 patients. Hear Lung. 50(6), 743–747 (2021).
Aghagoli, G. et al. Neurological involvement in COVID-19 and potential mechanisms: A review. Neurocrit. Care 34(7), 1062–1071 (2021).
Tajbakhsh, A. et al. COVID-19 and cardiac injury: Clinical manifestations, biomarkers, mechanisms, diagnosis, treatment, and follow up. Expert. Rev. Anti. Infect. Ther. 19(3), 345–357 (2021).
Wang, F., Kream, R. M. & Stefano, G. B. Long-term respiratory and neurological sequelae of COVID-19. Med. Sci. Monit. Int. Med. J. Exp. Clin. Res. 26(6), 1–10 (2020).
World Health Organization. Clinical Management of COVID-19: Interim Guidance (World Health Organization, 2020).
Amaravadi, R. K., Dimick, J. B., Pronovost, P. J. & Lipsett, P. A. ICU nurse-to-patient ratio is associated with complications and resource use after esophagectomy. Intensive Care Med. 26(6), 1857–1862 (2000).
Blot, S. I. et al. Patient to nurse ratio and risk of ventilator-associated pneumonia in critically ill patients. Am. J. Crit. Care. 20(1), e1-9 (2011).
Mertens, J. et al. Monitoring the SARS-CoV-2 pandemic: Screening algorithm with single nucleotide polymorphism detection for the rapid identification of established and emerging variants. Clin. Microbiol. Infect. 28(1), 124–129 (2022).
Wibmer, C. K. et al. SARS-CoV-2501Y.V2 escapes neutralization by South African COVID-19 donor plasma. Nat. Med. 27(4), 622–625 (2021).
Bian, L. et al. Impact of the Delta variant on vaccine efficacy and response strategies. Expert. Rev. Vaccines 20(10), 1201–1209 (2021).
Johnson, B. A. et al. Furin cleavage site is key to SARS-CoV-2 pathogenesis. BioRxiv 591(7849), 293–299 (2020).
Motozono, C. et al. An emerging SARS-CoV-2 mutant evading cellular immunity and increasing viral infectivity. BioRxiv 5(2), 2004–2021 (2021).
McCallum, M. et al. SARS-CoV-2 immune evasion by the B. 1.427/B. 1.429 variant of concern. Science 373(6555), 648–654 (2021).
Deng, X. et al. Transmission, infectivity, and neutralization of a spike L452R SARS-CoV-2 variant. Cell 184(13), 3426–3437 (2021).
Vellas, B. et al. Implications of ICD-10 for sarcopenia clinical practice and clinical trials: report by the international conference on frailty and sarcopenia research task force. J. Frailty aging. 7(1), 2–9 (2018).
World Health Organization. The Asia-Pacific Perspective: Redefining Obesity and its Treatment 24–51 (World Health Organization, 2000).
Valenza, F. et al. Prone position delays the progression of ventilator-induced lung injury in rats: Does lung strain distribution play a role?. Crit. Care Med. 33(2), 361–367 (2005).
Hansell, D. M. et al. Fleischner society: Glossary of terms for thoracic imaging. Radiology 246(3), 697–722 (2008).
Kazerooni, E. A. et al. Thin-section CT obtained at 10-mm increments versus limited three-level thin-section CT for idiopathic pulmonary fibrosis: Correlation with pathologic scoring. AJR Am. J. Roentgenol. 169(4), 977–983 (1997).
Pan, F. et al. Time course of lung changes at chest CT during recovery from coronavirus disease 2019 (COVID-19). Radiology 295(3), 715–721 (2020).
Deana, C. et al. Bioimpedance-assessed muscle wasting and its relation to nutritional intake during the first week of ICU: A pre-planned secondary analysis of Nutriti Study. Ann. Intensive Care. 14(1), 29–38 (2024).
Richards, L. & Palmiter-Thomas, P. Grip strength measurement: A critical review of tools, methods, and clinical utility. Crit. Rev. Phys. Rehabil. Med. 8(1), 315–340 (1996).
Rostamzadeh, S., Abouhossein, A., Alam, K., Vosoughi, S. & Sattari, S. S. Exploratory analysis using machine learning algorithms to predict pinch strength by anthropometric and socio-demographic features. Int. J. Occup. Saf. Ergon. 30(2), 518–531 (2024).
Rostamzadeh, S., Saremi, M. & Taheri, F. Maximum handgrip strength as a function of type of work and hand-forearm dimensions. Work 65(3), 679–687 (2020).
Luna-Heredia, E., Martín-Peña, G. & Ruiz-Galiana, J. Handgrip dynamometry in healthy adults. Clin. Nutr. 24(2), 250–258 (2005).
Dodds, R. M. et al. Grip strength across the life course: Normative data from twelve British studies. PLoS One 9(12), e113637 (2014).
Grubbs, F. E. Procedures for detecting outlying observations in samples. Technometrics 11(1), 1–21 (1969).
Singh, S. G. & Kumar, S. V. Dealing with multicollinearity problem in analysis of side friction characteristics under urban heterogeneous traffic conditions. Arab. J. Sci. Eng. 46(6), 10739–10755 (2021).
Huang, C. et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 395(10223), 497–506 (2020).
Vitale, G., Cesari, M. & Mari, D. Aging of the endocrine system and its potential impact on sarcopenia. Eur. J. Intern. Med. 35(9), 10–15 (2016).
Singh, T. & Newman, A. B. Inflammatory markers in population studies of aging. Ageing Res. Rev. 10(3), 319–329 (2011).
Garg, S. et al. Hospitalization rates and characteristics of patients hospitalized with laboratory-confirmed coronavirus disease 2019—COVID-NET, 14 States, March 1–30, 2020. Morb. Mortal. Wkly Rep. 69(15), 458–464 (2020).
Tamara, A. & Tahapary, D. L. Obesity as a predictor for a poor prognosis of COVID-19: A systematic review. Diabetes Metab. Syndr. Clin. Res. Rev. 14(4), 655–659 (2020).
Aghili, S. M. M. et al. Obesity in COVID-19 era, implications for mechanisms, comorbidities, and prognosis: A review and meta-analysis. Int. J. Obes. 45(5), 998–1016 (2021).
Soeroto, A. Y. et al. Effect of increased BMI and obesity on the outcome of COVID-19 adult patients: A systematic review and meta-analysis. Diabetes Metab. Syndr. Clin. Res. Rev. 14(6), 1897–1904 (2020).
Al-Salameh, A. et al. The association between body mass index class and coronavirus disease 2019 outcomes. Int. J. Obes. 45(3), 700–705 (2021).
Gebhard, C., Regitz-Zagrosek, V., Neuhauser, H. K., Morgan, R. & Klein, S. L. Impact of sex and gender on COVID-19 outcomes in Europe. Biol. Sex Differ. 11, 1–13 (2020).
Brady, E., Nielsen, M. W., Andersen, J. P. & Oertelt-Prigione, S. Lack of consideration of sex and gender in COVID-19 clinical studies. Nat. Commun. 12(1), 4015 (2021).
Abate, B. B., Kassie, A. M., Kassaw, M. W., Aragie, T. G. & Masresha, S. A. Sex difference in coronavirus disease (COVID-19): A systematic review and meta-analysis. BMJ Open. 10(10), e040129 (2020).
Singh, S., Chowdhry, M., Chatterjee, A. & Khan, A. Gender-based disparities in COVID-19 patient outcomes: A propensity-matched analysis. MedRxiv 24(4), 2004–2020 (2020).
Karanasos, A. et al. Impact of smoking status on disease severity and mortality of hospitalized patients with COVID-19 infection: A systematic review and meta-analysis. Nicotine Tob. Res. 22(9), 1657–1659 (2020).
Alqahtani, J. S. et al. Prevalence, severity and mortality associated with COPD and smoking in patients with COVID-19: A rapid systematic review and meta-analysis. PLoS One 15(5), 1–13 (2020).
Patanavanich, R. & Glantz, S. A. Smoking is associated with COVID-19 progression: A meta-analysis. Nicotine Tob. Res. 22(9), 1653–1656 (2020).
López-Hernández, Y., Rivas-Santiago, C. E., López, J. A., Mendoza-Almanza, G. & Hernandez-Pando, R. Tuberculosis and cigarette smoke exposure: An update of in vitro and in vivo studies. Exp. Lung. Res. 44(2), 113–126 (2018).
Flaherty, G. T. et al. COVID-19 in adult patients with pre-existing chronic cardiac, respiratory and metabolic disease: A critical literature review with clinical recommendations. Trop. Dis. Travel Med. vaccines. 6(5), 1–13 (2020).
Kabeerdoss, J. et al. Severe COVID-19, multisystem inflammatory syndrome in children, and Kawasaki disease: immunological mechanisms, clinical manifestations and management. Rheumatol. Int. 41(1), 19–32 (2021).
Gallo Marin, B. et al. Predictors of COVID-19 severity: A literature review. Rev. Med. Virol. 31(1), 1–10 (2021).
Onder, G., Rezza, G. & Brusaferro, S. Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. Jama 323(18), 1775–1776 (2020).
Woolf, S. H., Chapman, D. A. & Lee, J. H. COVID-19 as the leading cause of death in the United States. Jama 325(2), 123–124 (2021).
Martinez-Rojas, M. A., Vega-Vega, O. & Bobadilla, N. A. Is the kidney a target of SARS-CoV-2?. Am. J. Physiol. Physiol. 318(6), 1454–1462 (2020).
He, L. et al. Expression of elevated levels of pro-inflammatory cytokines in SARS-CoV-infected ACE2+ cells in SARS patients: Relation to the acute lung injury and pathogenesis of SARS. J. Pathol. A J. Pathol. Soc. Gt Britain. Irel. 210(3), 288–297 (2006).
Vetrugno, L. et al. Ventilatory associated barotrauma in COVID-19 patients: A multicenter observational case control study (COVI-MIX-study). Pulmonology 29(6), 457–468 (2023).
de Sevilla, G. G. P. & Sánchez-Pinto, B. Associations between muscle strength, dyspnea and quality of life in post-COVID-19 patients. Rev. Assoc. Med. Bras. 68(12), 1753–1758 (2022).
Msigwa, S. S., Wang, Y., Li, Y. & Cheng, X. The neurological insights of the emerging coronaviruses. J. Clin. Neurosci. 78(8), 1–7 (2020).
Maggio, M. et al. The relationship between testosterone and molecular markers of inflammation in older men. J. Endocrinol. Invest. 28(1), 116–119 (2005).
Wang, X. et al. Insulin-like growth factor 1 related to chronic low-grade inflammation in patients with obesity and early change of its levels after laparoscopic sleeve gastrectomy. Obes. Surg. 30(9), 3326–3332 (2020).
Filgueira, T. O. et al. The relevance of a physical active lifestyle and physical fitness on immune defense: mitigating disease burden, with focus on COVID-19 consequences. Front. Immunol. 12(4), 1–23 (2021).
Okazaki, T. et al. Respiratory muscle weakness as a risk factor for pneumonia in older people. Gerontology 67(5), 581–590 (2021).
Nelke, C., Dziewas, R., Minnerup, J., Meuth, S. G. & Ruck, T. Skeletal muscle as potential central link between sarcopenia and immune senescence. EBioMedicine. 49(7), 381–388 (2019).
Moonen, H. P. F. X. et al. Association of bioelectric impedance analysis body composition and disease severity in COVID-19 hospital ward and ICU patients: The BIAC-19 study. Clin. Nutr. 40(4), 2328–2336 (2021).
Piotrowicz, K. et al. Factors associated with mortality in hospitalised, non-severe, older COVID-19 patients–the role of sarcopenia and frailty assessment. BMC Geriatr. 22(1), 1–12 (2022).
Salleh, M. Z., Derrick, J. P. & Deris, Z. Z. Structural evaluation of the spike glycoprotein variants on SARS-CoV-2 transmission and immune evasion. Int. J. Mol. Sci. 22(14), 7425–7446 (2021).
Acknowledgements
This work was supported by the Shahid Beheshti University of Medical Sciences, Tehran, Iran (under Grant No. 43005817). The authors would like to express special thanks to all the physician as well as patients and their families for giving up their time for this research.
Author information
Authors and Affiliations
Contributions
S.R.: Conceptualization, Investigation, Validation, Methodology, Data curation, Formal analysis, Writing-original draft, Writing-review and editing. A.A.: Conceptualization, Investigation, Methodology, Data curation. A.A.: Conceptualization, Validation, Investigation, Methodology, Data curation. A.A.: Conceptualization, Investigation, Project administration, Funding acquisition.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Rostamzadeh, S., Allafasghari, A., Allafasghari, A. et al. Handgrip strength as a prognostic factor for COVID-19 mortality among older adult patients admitted to the intensive care unit (ICU): a comparison Alpha (B.1.1.7) and Delta (B.1.617.2) variants. Sci Rep 14, 19927 (2024). https://doi.org/10.1038/s41598-024-71034-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-71034-w
- Springer Nature Limited