Abstract
Non-small cell lung cancer (NSCLC) remains a significant challenge, as it is one of the leading causes of cancer-related deaths, and the development of resistance to anticancer therapy makes it difficult to treat. In this study, we investigated the anticancer mechanism of deoxybouvardin (DB), a cyclic hexapeptide, in gefitinib (GEF)-sensitive and -resistant NSCLC HCC827 cells. DB inhibited the viability and growth of HCC827 cells in a concentration- and time-dependent manner. In vitro kinase assay showed DB inhibited epidermal growth factor receptor (EGFR), mesenchymal–epithelial transition (MET), and AKT, and their phosphorylation was suppressed in HCC827 cells treated with DB. A molecular docking model suggested that DB interacts with these kinases in the ATP-binding pockets. DB induces ROS generation and cell cycle arrest. DB treatment of HCC827 cells leads to mitochondrial membrane depolarization. The induction of apoptosis through caspase activation was confirmed by Z-VAD-FMK treatment. Taken together, DB inhibited the growth of both GEF-sensitive and GEF-resistant NSCLC cells by targeting EGFR, MET, and AKT and inducing ROS generation and caspase activation. Further studies on DB can improve the treatment of chemotherapy-resistant NSCLC through the development of effective DB-based anticancer agents.
Similar content being viewed by others
Introduction
Lung cancer remains the leading cause of cancer-related death worldwide, accounting for almost two million deaths annually1. Non-small cell lung cancer (NSCLC), a common type of lung cancer, is very fatal due to the high rate of metastasis even though the progress of cancer is somewhat slow2. Several aberrations have been identified as causes of NSCLC. These include mutations in the epidermal growth factor receptor (EGFR) and Kirsten rat sarcoma viral oncogene homologue (KRAS), amplification of mesenchymal–epithelial transition (MET), and translocation of anaplastic lymphoma kinase3. EGFR mutations in NSCLC result in the constant activation of EGFR4. Specific tyrosine kinase inhibitors (TKIs) such as gefitinib (GEF) may suppress EGFR signaling and exert anticancer activity5. These target-specific anticancer drugs are specific and do not harm non-cancer cells, unlike classical chemotherapeutics6. Nonetheless, these targeted anticancer therapies cannot avoid resistance7. Despite successful initial clinical outcomes, many patients develop acquired resistance to TKIs8.
HCC827 cells grown in the presence of GEF acquire resistance through MET amplification9. The study with GEF-resistant HCC827 (HCC827GR) cell line shows promise in overcoming resistance, and a combination of TKIs targeting EGFR and MET has been proposed for this purpose10. The regulation of cellular ROS levels modulates important cellular physiology and pathophysiology11. Additionally, ROS generation and EGFR signaling are interrelated, promoting tumor proliferation and drug resistance12. In most cases, the generation of excessive ROS can be antiproliferative, and the regulation or dysregulation of ROS generation by EGFR targets may lead to the apoptosis of cancer cells13.
Deoxybouvardin (DB, Fig. 1) is a bicyclic hexapeptide that was first isolated from Bouvardia ternifolia (Rubiaceae), a shrub native to Mexico. Later, it was isolated from other Rubia species and is also known as RA-V. DB has a unique 14-membered cyclophane macrocycle unit in which two tyrosines are connected by an ether linkage, and a few structurally related analogs have been discovered in natural products, and chemical synthesis of DB is possible too14. DB is reported to exhibit antitumor activity, possibly acting as an ionophore, similar to valinomycin15. RA-V and other related cyclic hexapeptides, such as RA-I, RA-IV, RA-VII, and RA-700, have been shown to exert antitumor activity in mouse models16. Although DB reportedly inhibits angiogenesis by downregulating ERK1/2 phosphorylation17, the detailed molecular mechanisms have not yet been elucidated.
In this study, we investigated whether DB exhibits selective antitumor activity in NSCLC cells. We examined if DB exerted an antiproliferative effect on the NSCLC cell lines HCC827 and HCC827GR. By analyzing the kinase activities of EGFR, MET, and AKT in the presence of DB, we determined whether DB could function as an inhibitor of multiple kinases. The antiproliferative activity of DB is expected to provide insights for GEF-resistant NSCLC therapy.
Material and methods
Chemicals
DB was obtained from a previous chemical study on Rubia philippinensis18. Briefly, the EtOH extract of R. philippinensis (150 g) was suspended in 1.5 L H2O and partitioned with CH2Cl2 (2 L × 3) to obtain a CH2Cl2-soluble fraction (50 g). Six column fractions, D-1 through D-6, were obtained from the CH2Cl2-soluble fraction via silica gel vacuum liquid chromatography with elution solvents of n-hexane–EtOAc (20:1, 10:1, 5:1, 3:1, 2:1) and CHCl3–MeOH (8:1). Fraction D-6 (10.0 g) was further fractionated into 12 sub-fractions, D-6–1 through D-6–12, via medium-pressure liquid chromatography using the C18 SNAP Cartridge KPC18-HS column with a gradient mobile phase of MeOH/H2O (10:90 → 100:0, 7 L). DB (tR 59 min, 250 mg) was isolated from D-6-5 (400 mg) via preparative high-performance liquid chromatography using the Phenomenex Kinetex 5 μm C18 column (250 × 21.20 mm), with MeOH/H2O (65:35, 4 mL/min, UV 205 nm) as the eluent. The chemical structure of DB was determined by analyzing nuclear magnetic resonance (NMR) spectroscopic data (Table 1) and comparing it with existing data15. DB: white amorphous powder; 1H and 13C NMR data (CDCl3, 300 and 75 MHz); ESIMS, m/z 757.3 [M + H]+, m/z 797.3 [M + Na]+, m/z 755.2 [M − H]−; see Table 1 and Figs. S1–S3.
Reagents
Savolitinib (SAV) and AZD5363 were purchased from Selleck Chemicals (Houston, TX, USA). GEF was obtained from Cayman Chemical Co. (Ann Arbor, MI, USA). NAC, Z-VAD-FMK, dimethyl sulfoxide (DMSO), 3-[4,5-dimethylthiazol2-yl]-2,5-diphenyltetrazolium bromide (MTT), and Basal Medium Eagle (BME) were purchased from Sigma-Aldrich (St. Louis, MO, USA). The Roswell Park Memorial Institute (RPMI) medium, phosphate-buffered saline (PBS), and trypsin–EDTA solution were obtained from HyClone (Logan, UT, USA). Fetal bovine serum (FBS) and penicillin–streptomycin (P/S) were purchased from Gibco (Carlsbad, CA, USA). Primary antibodies detecting phosphorylated (p)-EGFR (Thr1068), p-MET (Tyr1234/1235), MET, p-AKT (Ser473), and poly ADP-ribose polymerase (PARP) were obtained from Cell Signaling Technology (Danvers, MA, USA). Antibodies specific to EGFR, cyclin B1, cdc2, p27, caspase-3, BCl-2, Bad, Bim, cytochrome c (cyto c), cytochrome c oxidase subunit 4 (COX4), β-actin, and β-Tubulin were purchased from Santa Cruz Biotechnology (Santa Cruz, CA, USA). All secondary antibodies were purchased from Thermo Fisher Scientific (Waltham, MA, USA).
Cell culture and treatment
The human NSCLC cell line HCC827 (EGFR del E746-A750; GEF-sensitive cells) and human keratinocyte HaCaT cells were obtained from the ATCC (Manassas, VA, USA). HCC827GR (MET-amplified and GEF-resistant HCC827) cells were provided by Professor Pasi A. Jänne (Department of Medical Oncology, Dana-Farber Cancer Institute, Boston, MA, USA)19. The HCC827 and HCC827GR cells were maintained in RPMI-1640 medium containing 10% FBS and 100 U/mL P/S. The HCC827GR cells were maintained in 0.1 μM GEF for long-term culture. The HaCaT cells were maintained in DMEM supplemented with 10% FBS and 100 U/mL P/S. The cells were cultured at 37 °C in a humidified atmosphere containing 5% CO2. The cells were treated with DB (0, 2, 4, and 8 nM) for 24 or 48 h. The HCC827 and HCC827GR cells were pretreated with NAC (ROS inhibitor, 4 mM) or Z-VAD-FMK (pan-caspase inhibitor, 12 μM) for 3 h and exposed to DB (8 nM) for 48 h.
Cell viability assay
The cells were seeded in a 96-well plate and treated with DB (0, 2, 4, and 8 nM), GEF (1 μM), or SAV (2 nM) for 24 or 48 h. MTT solution was added to the medium and incubated for 2 h at 37 °C. After removal of the medium, formazan was dissolved in 100 μL DMSO. Lastly, absorbance was measured at 570 nm using a Multiscan GO spectrophotometer (Thermo Fisher Scientific).
Colony formation assay
The anchorage-independent growth of the cells was analyzed by colony formation on soft agar. For this assay, the bottom agar (0.6% agar, BME, 10% FBS, 5 μg/mL gentamicin, and 2 mM l-glutamine) was solidified in a 6-well plate. The cells (8 × 103 cells/well) were seeded in 0.3% agar mixed with medium containing DB (0, 2, 4, and 8 nM), GEF (1 μM), or SAV (2 nM). After 14 d of incubation, the size and number of the colonies were measured under a light microscope (Leica Microsystems, Wetzlar, DEU) and an IMT iSolution System (IMT i-Solution Inc., Vancouver, BC, Canada).
In vitro ADP-Glo kinase assay
The in vitro kinase assay was performed in a 384-well plate using the ADP-Glo Kinase Assay Kit (Promega, Madison, Wl, USA). The active recombinant protein kinase (EGFR, MET, AKT1, or AKT2) was added to a kinase buffer containing inhibitors (DB, GEF, SAV, or AZD5363) and ATP/substrate using the I-DOT dispenser (Dispendix GmbH, Stuttgart, Germany). The reaction mixture was incubated for 1 h. ADP-Glo reagent was added to the kinase reactions and incubated for 40 min. To evaluate kinase activity, a kinase detection solution was added to each well, and luminescence was measured using a Centro LB 960 microplate luminometer (Berthold Technologies, Bad Wildbad, Germany).
Molecular modeling
To predict the binding mode of DB to each kinase, a molecular docking simulation was performed using AutoDock Vina20. The PDB files for EGFR, MET, AKT1, and AKT2 were 1M17, 4XYF, 6CCY, and 3D0E, respectively, and the residue numbers were not altered. An unbiased search was performed by keeping the grid sufficiently large to cover most of the protein surface. Among the modes reported by AutoDock Vina, the best mode was chosen for graphical depiction.
Cell cycle analysis
HCC827 (5.5 × 104 cells) and HCC827GR (5 × 104 cells) were seeded in a 6-well plate and treated with DB (0, 2, 4, and 8 nM) for 48 h. The cells were washed with cold 1 × PBS and fixed in 70% ethanol at − 20 °C. Next, the cells were subjected to Muse™ Cell Cycle Reagent (Merck Millipore, MA, USA) for 30 min in the dark and analyzed using the Muse™ Cell Analyzer (Merck Millipore).
ROS measurement
ROS measurement was performed using the Muse™ Oxidative Stress Kit (Merck Millipore). The cells were incubated with different concentrations of DB (0, 2, 4, and 8 nM) for 48 h and harvested using 1 × assay buffer. The prepared samples were added to the Muse™ Oxidative Stress Reagent working solution for 30 min at 37 °C in the dark and further analyzed using the Muse™ Cell Analyzer.
JC-1 staining
Changes in the mitochondrial membrane potential (MMP) in the cells were determined using the JC-1 assay. The cells were seeded in 60 mm culture dishes and treated with DB (0, 2, 4, and 8 nM). After 48 h, the cells were harvested, washed twice with 1 × PBS, and incubated in RPMI medium (10% FBS and 100 U/mL P/S) containing 10 μg/mL JC-1 dye (Thermo Fisher Scientific, MA, USA) at 37 °C for 15 min in the dark. JC-1 monomers and aggregate cells were analyzed using a MACSQuant Analyzer 16 (Miltenyi Biotec, Bergisch Gladbach, Germany).
Annexin V/7-AAD staining
Apoptosis was determined using the Muse™ Annexin V & Dead Cell Kit (Merck Millipore). Untreated or DB-treated cells were stained with Annexin V/7-ADD in 1 × binding buffer for 30 min. All stained cells were analyzed using the Muse™ Cell Analyzer.
Multicapase-7AAD staining
Multicaspase (caspase-1, -3, -4, -5, -6, -7, -8, and -9) activity was measured using the Muse™ MultiCaspase Kit (Merck Millipore), following the manufacturer’s instructions. The cells were washed with caspase buffer, incubated in the Muse™ MultiCaspase Reagent at 37 °C for 15 min, and stained with the 7-AAD working solution for 10 min. Finally, caspase-activated cells were detected using the Muse™ Cell Analyzer.
Western blotting
Protein samples were extracted using the PRO-PREP™ Protein Extraction Solution (iNtRON Biotechnology, Seongnam, Korea) containing protease and phosphatase inhibitors. Protein concentration was quantified using the Bio-Rad DC Protein Assay kit (Bio-Rad, CA, USA). The proteins were separated using sodium dodecyl sulfate–polyacrylamide gel electrophoresis and transferred onto polyvinylidene difluoride membranes. After blocking with skimmed milk for 2 h, primary antibodies in 1 × PBS containing 0.1% Tween 20 (PBST) were added to the membranes and kept aside overnight at 4 °C. Next, the membranes were washed with 1 × PBST for 30 min and incubated with secondary antibodies for 2 h. The protein levels were visualized using the Miracle-Star™ Western Blot Detection System (iNtRON Biotechnology), while the bands were analyzed using ImageJ software (NIH, Bethesda, MD).
Isolation of cytosol and mitochondrial fractionation
Untreated or DB-treated cells were homogenized in plasma membrane extraction buffer (1 mM EDTA, 1 mM EGTA, 10 mM HEPES [pH 8.0], 250 mM sucrose, 10 mM KCl, 1.5 mM MgCl2∙6H2O, 0.1 mM phenylmethylsulfonyl fluoride, 0.01 mg/mL leupeptin, 0.01 mg/mL aprotinin, and 0.1% digitonin). The homogenized cells were centrifuged, and the supernatants were separated to determine the cytosolic fraction. After the remaining pellets were washed in plasma membrane extraction buffer, 0.5% Triton X-100 was added, and the supernatants were collected for analysis of the mitochondrial fractions.
Statistical analysis
All experiments were performed in triplicate, and the data were presented as mean ± standard deviation (SD). Multiple comparisons were conducted using one-way or two-way analysis of variance using GraphPad Prism 5 (San Diego, CA, USA). Asterisk-marked p-values were used to indicate statistically significant differences (*p < 0.05, **p < 0.01, ***p < 0.001).
Results
DB inhibits cell viability and growth of NSCLC cells
We performed an MTT viability assay to determine whether DB inhibited the growth of NSCLC cells. The results indicated that DB inhibited the growth of both GEF-sensitive and GEF-resistant HCC827 (HCC827GR) cells in a concentration- (2, 4, and 8 nM) and time-dependent (24 and 48 h) manner. The cell viability of HCC827 cells treated with DB (2, 4, and 8 nM) was 87.1%, 75.2%, and 59.6% at 24 h and 82.8%, 64.6%, and 42.2% at 48 h, respectively, compared to untreated cells. Similarly, the cell viability of HCC827GR cells treated with DB (2, 4, and 8 nM) was 88.3%, 83.4%, and 69.7% at 24 h and 80.6%, 62.9%, and 40.8% at 48 h, respectively, compared to untreated cells. To determine whether the cytotoxicity of DB was selective for NSCLC cells, we performed an MTT cell viability assay using the HaCaT cell line. We observed negligible cytotoxic effects of DB on HaCaT cells, and the cell viability of HaCaT cells treated with DB (2, 4, and 8 nM) was 99.4%, 98.6%, and 94.5% at 24 h and 97.8%, 97.5%, and 97.4% at 48 h, respectively. We also determined whether GEF and SAV had cytotoxic effects on these cells. The cell viability of HCC827 cells treated with GEF (1 μM) was 48.3% at 24 h and 23.9% at 48 h compared to untreated cells, indicating that HCC827 cells were susceptible to GEF treatment. In contrast, the HCC827GR cells treated with GEF (1 μM) demonstrated resistance to GEF, with cell viabilities of 94.0% at 24 h and 94.2% at 48 h. Meanwhile, the cell viability of HCC827 cells treated with SAV (2 nM) was 98.1% at 24 h and 93.8% at 48 h, indicating that SAV at 2 nM did not affect the viability of HCC827 cells. The viability of HCC827GR cells treated with SAV was 99.5% at 24 h and 99.3% at 48 h, suggesting that SAV was non-cytotoxic for both GEF-sensitive and GEF-resistant HCC827 cells. In addition, the cytotoxic effects of GEF on HCC827 cells were not enhanced by the co-administration of SAV. The viability of HCC827 cells treated with GEF (1 μM) and SAV (2 nM) was 47.7% at 24 h and 22.1% at 48 h, which was comparable to the effect of GEF alone. However, the combination of GEF and SAV was cytotoxic enough to inhibit the growth of HCC827GR cells, exhibiting cell viabilities of 56.2% at 24 h and 34.8% at 48 h. The cytotoxic effects of GEF and SAV on HaCaT cells were similar to those on HCC827 cells (Fig. 2A). We performed a soft agar assay to evaluate colony formation, which showed that DB inhibited colony formation. Both the count and size of the colonies decreased following DB treatment in a concentration-dependent manner (Fig. 2B). Treatment with DB (2, 4, and 8 nM) for 14 d decreased the colony size to 81.9%, 57.6%, and 51.8% in HCC827 cells, respectively, and 78.1%, 55.2%, and 42.0% in HCC827GR cells, respectively; the colony counts decreased to 21.0%, 18.0%, and 11.0% in HCC 827 cells, respectively, and 43.8%, 28.6%, and 11.4% in HCC827GR cells, respectively (Fig. 2C). Parallel experiments involving the treatment of cells with GEF and SAV further demonstrated the different effects of these compounds on HCC827 and HCC827GR cells. Taken together, these results indicated that DB inhibited the viability and growth of HCC827 and HCC827GR NSCLC cells.
Antiproliferative activity of DB in NSCLC cells. (A) NSCLC cells HCC827 and HCC827GR were treated with DB (0, 2, 4, and 8 nM) for 24 (solid) and 48 h (empty). Cell viability was determined using the MTT cell viability assay. The data are shown as mean ± SD (n = 3). *p < 0.05, **p < 0.01 and ***p < 0.001 compared to the control group (0 µM). GEF and SAV treatment were used as positive controls. (B and C) Soft agar assay to determine the anchorage-independent colony growth in NSCLC cells treated with DB after 14 d of incubation. HCC827 and HCC827GR cells were observed using microscopy after indicated treatments with DB, GEF, or SAV for 14 d. (B) Photographs. Scale bar, 400 μm. (C) Histograms for colony numbers. **p < 0.01 and ***p < 0.001 compared to the control group (0 µM).
DB inhibits the kinase activity of EGFR, MET, and AKT
To determine whether DB inhibits the kinase activities of EGFR, MET, and AKT, we performed an in vitro kinase assay for EGFR, MET, ATK1, and AKT2. We observed that the enzyme activities of all three kinases were inhibited by DB in a dose-dependent manner (0, 2, 4, and 8 nM; Fig. 3A,B). The kinase activity measured in the presence of DB (2, 4, and 8 nM) was compared to the kinase activity of untreated kinases and kinases treated with corresponding inhibitors: 1 μM GEF for EGFR, 2 nM SAV for MET, and 30 nM AZD5363 for AKT1 and AKT2. DB inhibited kinase activity in a dose-dependent manner. DB (2, 4, and 8 nM) inhibited the kinase activity of EGFR by 18.8%, 32.9%, and 61.5%, MET by 41.2%, 52.0%, and 67.9%, AKT1 by 18.9%, 37.7%, and 52.7%, and AKT2 by 6.1%, 33.7%, and 52.9%, respectively (Fig. 3A). The IC50 values of kinase inhibition by DB were 6.39, 3.5, 7.27, and 7.4 nM for EGFR, MET, AKT1, and AKT2, respectively. The strong inhibition of protein kinases by DB was supported by molecular modeling using AutoDock Vina20. DB can be docked into ATP-binding pockets, as shown in Fig. 3B. In AutoDock molecular modeling, DB was located near several hydrophobic amino acids, such as Phe residues 699, 1089, 161, and 163 in EGFR, MET, AKT1, and AKT2, respectively.
Inhibition of protein kinases by DB. (A) In vitro ADP-Glo kinase activity assay was performed in the presence of DB, GEF, SAV, or AZD5363 for kinases EGFR, MET, AKT1, and AKT2. Data are shown as the mean ± SD (n = 3). *p < 0.05, **p < 0.01, and ***p < 0.001 compared to the controls. (B) AutoDock molecular modeling of binding of DB to the kinases. For each kinase, an overview of the surface and cartoon depiction are shown; DB is shown in spheres. Zoomed in: DB in pink sticks and surrounding amino acids in purple sticks.
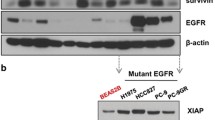
DB suppresses the EGFR/MET and AKT signaling pathways
We used western blotting to determine the level of phosphorylation of the proteins involved in the EGFR/MET/AKT signaling pathways (Fig. 4A). HCC827 and HCC827GR cells treated with DB (2, 4, and 8 nM) were monitored for changes in the phosphorylation of EGFR, MET, and AKT, which decreased significantly after DB treatment (Fig. 4B–D). In contrast, the protein levels remained relatively unchanged. These results indicate that DB suppresses the signaling pathways of EGFR/MET and AKT by decreasing their phosphorylation. To compare the effect of DB on the phosphorylation of these kinases with that of GEF, we treated both HCC827 and HCC827GR cells with GEF only. We observed the ratio of phosphorylated kinases decreased in HCC827 cells treated with GEF (1 μM). On the other hand, the phosphorylation decreased significantly only for EGFR in HCC827GR cells treated with GEF, while the phosphorylation of both MET and AKT remained relatively in high level (Fig. 4E,F).
Suppression of protein phosphorylation by DB. NSCLC cells HCC827 and HCC827GR treated with DB (0, 2, 4, and 8 nM) for 48 h were harvested and subjected to western blot analysis with antibodies against p-EGFR (Tyr1068), EGFR, p-MET (Tyr1234/1235), MET, p-AKT (Ser473), AKT, and β-actin. (A) Western blot analysis. (B) Relative intensity of p-EGFR/EGFR relative to the level of β-actin. (C) Relative intensity of p-MET/MET. (D) Relative intensity of p-AKT/AKT. (E, F) HCC827 and HCC827GR cells were treated with or without GEF (1 μM) and the level of kinases EGFR, MET, and AKT was determined by western blotting to examine the relative intensity of phosphoproteins. Data are shown as the mean ± SD (n = 3). *p < 0.05, **p < 0.01, and ***p < 0.001 compared to the controls.
DB exerts antiproliferative activity by modulating the G2/M phase transition
To analyze the cell cycle distribution in HCC827 cells treated with DB, we performed flow cytometry. In untreated HCC827 cells, the proportion of cells in the G0/G1 phase was 61.0%, which decreased with DB treatment (2, 4, and 8 nM) to 58.7%, 58.6%, and 53.1%, respectively; however, the proportion of cells in the G2/M phase increased from 32.8% among untreated cells to 34.9%, 35.3%, and 40.3% among DB-treated cells, respectively. In addition, there was a slight increase in the proportion of cells in the S phase from 6.2% among untreated cells to 6.4%, 6.0%, and 6.5% among DB-treated cells, respectively (Fig. 5A,B). Similar results were observed in HCC827GR cells. The proportion of cells in the G0/G1 phase decreased with DB treatment (0, 2, 4, and 8 nM) from 60.0 to 59.3%, 55.5%, and 44.1%, whereas the proportion of cells in the G2/M phase increased from 33.3 to 33.9%, 37.4%, and 47.3%, respectively. The proportion of cells in the S phase increased from 6.7 to 6.6%, 7.0%, and 8.2%, respectively (Fig. 5A,C). Western blot analysis showed a decrease in the level of the G2/M phase regulator cyclin B1 and cdc2, whereas the expression of p27 was strongly increased by DB treatment (Fig. 5D). These results imply that DB inhibits cell cycle progression in NSCLC cells by arresting the G2/M phase transition.
Cell cycle arrest by DB. NSCLC cells HCC827 and HCC827GR treated with DB (0, 2, 4, and 8 nM) for 48 h were analyzed using flow cytometry with PI staining. (A) Flow cytometry plots. (B and C) Histograms of cell cycle distribution. *p < 0.05, **p < 0.01, and ***p < 0.001 compared to the controls. (D) Western blot analysis of cell cycle-related proteins cyclin B1, cdc2, and p27. β-actin was used as the loading control.
DB induces an increase in ROS generation in NSCLC cells
To analyze the increase in ROS generation induced by DB treatment in NSCLC cells, we used a cell analyzer after labeling the cells with fluorescent probes. In HCC827 cells, the level of ROS increased from 10.4 to 16.2%, 29.0%, and 31.4% after treatment with DB at 2, 4, and 8 nM, respectively. Similarly, the level of ROS in HCC827GR cells increased from 9.8 to 42.8%, 46.4%, and 48.8% after DB (2, 4, and 8 nM) treatment, respectively (Fig. 6A). To verify whether the increase in ROS levels mediated the antiproliferative effect of DB, NSCLC cells were treated with or without NAC (4 mM), a ROS scavenger, before DB treatment at 8 nM. NAC alone, without DB treatment, did not affect the proliferation of NSCLC cells, whereas NAC pretreatment before DB treatment prevented the antiproliferative effects of DB. The cell viability after DB treatment was 40.8% and 37.4% for HCC827 and HCC827GR cells, respectively, compared to the untreated cells. After pretreatment with NAC, viability increased to 92.8% and 92.7% for HCC827 and HCC827GR cells, respectively (Fig. 6B). Next, we analyzed the levels of phosphorylated proteins involved in the EGFR/MET/AKT signaling pathways. There was a decrease in phosphorylation levels following DB treatment alone or in the presence of NAC. In contrast, the levels of proteins involved in apoptosis (caspase-3 and PARP) were decreased by DB treatment, which was prevented by pretreatment with NAC. The level of cleaved PARP increased after DB treatment, and pretreatment with NAC reversed this increase to the control level (Fig. 6C). These results indicate that DB induces ROS generation and decreases EGFR/MET/AKT phosphorylation, thereby exerting its antiproliferative effects.
Induction of ROS generation by DB. NSCLC cells HCC827 and HCC827GR treated with DB (0, 2, 4, and 8 nM) for 48 h were analyzed using flow cytometry using a MuseTM Oxidative Stress Kit. (A) Flow cytometry plots and histogram of cellular ROS. ***p < 0.001 compared to the controls. (B and C) NSCLC cells were pretreated with NAC (4 mM) or vehicle for 3 h and then incubated with DB for 48 h. (B) Histogram of cell viability measured by the MTT assay. ***p < 0.001 compared to the controls; ###p < 0.001 compared to DB treatment. (C) Immunoblot analysis of phosphorylated forms of EGFR, MET, AKT, whole caspase-3, and PARP. β-actin was used as the control.
DB induces MMP disruption in NSCLC cells
We measured MMP with JC-1 fluorescence probes to assess whether DB induces MMP disruption in HCC827 and HCC827GR cells treated with DB. In HCC827 cells, the proportion of JC-1 green increased from 5.9% in the untreated cells to 15.5%, 21.5%, and 31.3% after DB treatment (2, 4, and 8 nM), respectively. Moreover, the proportion of JC-1 green increased in HCC827GR cells from 6.0% in untreated cells to 7.6%, 15.7%, and 21.9% in DB-treated cells, respectively (Fig. 7A). Western blot analysis showed a decrease in the level of Bcl-2, an anti-apoptotic protein, whereas the levels of the pro-apoptotic proteins Bad and Bim increased after DB treatment (Fig. 7B). In addition, DB treatment decreased the levels of whole caspase-3 and PARP and increased the level of cleaved PARP. These results indicate that DB induces the disruption of MMP to activate apoptosis in NSCLC cells.
Dysregulation of MMP by DB. NSCLC cells HCC827 and HCC827GR treated with DB (0, 2, 4, and 8 nM) for 48 h were analyzed using flow cytometry with JC-1 staining. (A) Flow cytometry plots and histograms. The histogram indicates the proportion of cells with depolarized mitochondrial membranes. ***p < 0.001 compared to the controls. (B) Immunoblot analysis of proteins related to mitochondrial permeability (Bcl-2, Bad, Bim, and cyto c) and apoptosis (caspase-3 and PARP). Cytosol and mitochondrial fractions were separated to determine cyto c levels. The loading controls for cytosolic and mitochondrial fractions included β-Tubulin and COX4, respectively.
DB induces apoptosis in NSCLC cells by activating caspases
To determine the proportion of cells undergoing apoptosis, NSCLC cells treated with DB (2, 4, and 8 nM) were stained with Annexin V/7-AAD and analyzed using flow cytometry (Fig. 8A). The proportion of cells undergoing apoptosis in the early stages (Annexin V+/7-AAD−, located in the lower-right quadrant of the plot) increased from the background level (2.6% and 1.1% for HCC827 and HCC827GR, respectively) to 3.9%, 4.2%, and 27.2% for HCC827, and 2.8%, 4.1%, and 25.2% for HCC827GR cells, respectively. The number of cells in the late stages of apoptosis also increased from the background levels. Next, to determine whether DB-induced apoptosis was caspase dependent, the activities of multiple caspases were determined, which increased from the background (5.7% and 5.6% for HCC827 and HCC827GR, respectively) to 14.3%, 19.4%, and 35.6% for HCC827, and 14.3%, 22.1%, and 34.6% for HCC827GR cells, respectively (Fig. 8B). To further evaluate the effect of DB on the caspase-dependent apoptotic pathway, HCC827 and HCC827GR cells were pretreated with the pan-caspase inhibitor Z-VAD-FMK (12 μM) 3 h prior to incubation with DB for 48 h. As exhibited in Fig. 8E, compared with DB alone-treated cells, HCC827 and HCC827GR cell viability increased to 81.7% and 86.5% in the Z-VAD-FMK combination treatment, respectively. These results illustrate that DB induces apoptosis in HCC827 and HCC827GR cells by activating caspases.
Induction of apoptosis by caspase activation in DB-treated NSCLC cells. NSCLC cells HCC827 and HCC827GR treated with DB (0, 2, 4, and 8 nM) for 48 h were analyzed using flow cytometry with Annexin V/7-AAD double staining and a MuseTM MultiCaspase Kit. (A) Flow cytometry plots of Annexin V/7-AAD double staining. (B) The histogram indicates the proportion of apoptotic cells. **p < 0.01 and ***p < 0.001 compared to the controls. (C) Flow cytometry plots of MultiCaspase analysis. (D) The histogram indicates the proportion of the cells with activated caspases. ***p < 0.001 compared to the controls. (E) NSCLC cells were co-treated with Z-VAD-FMK (12 µM) or a vehicle for 3 h and then incubated with DB for 48 h. The viability of the cells was measured using the MTT assay.
Discussion
DB and related cyclic hexapeptides have been shown to exert antitumor activity in leukemia and melanoma cell culture models15. Although early studies indicated that protein synthesis could be inhibited by these compounds, inhibitory activity was observed at micromolar concentrations21. The 14-membered ring structure of the cyclic peptide was found to exert strain, maintaining the molecule in an active conformation22. However, the antitumor activity of DB and its related compounds has not been thoroughly explored, and the molecular targets of DB remain unknown. This study is the first to report that DB exerts an anticancer effect in both GEF-sensitive and GEF-resistant NSCLC HCC827 cells.
In patients with NSCLC, treatment with an EGFR inhibitor offers initial success but leads to relapse owing to the development of resistance7. Drug resistance is prevalent and may exist even before the commencement of treatment23. The main cause of the resistance to EGFR-specific TKIs is a threonine-to-methionine mutation at residue 790 (T790M) of EGFR, prevalent in 60% of all resistant cases7. The T790M point mutation allows tighter binding between ATP and EGFR, thereby weakening the binding between EGFR and kinase inhibitors24. In addition, MET amplification adds to this burden by activating ERBB3 survival and tumorigenesis signaling25. In the presence of an EGFR-specific TKI, MET is amplified, and survival signaling independent of EGFR is activated26. In a phase Ib clinical trial in which patients with NSCLC with prior EGFR-TKI treatment were treated with a combination of GEF and SAV10, the results underscored the potential of targeting multiple targets simultaneously. In this study, DB effectively inhibited the growth of both GEF-sensitive and GEF-resistant HCC827 cells (Fig. 2A). The antiproliferative activity of DB (8 nM) on HCC827 cells was comparable to that of GEF (1 μM). Interestingly, in HCC827GR cells, DB was as cytotoxic as the combination of GEF and SAV (1 μM and 2 nM, respectively). These results suggest that DB-based anticancer therapy can be applied to treat GEF-resistant NSCLC.
AKT is involved in the downstream signaling pathways of EGFR and MET27. Therefore, the activation of AKT, in addition to EGFR and MET, is a possible target for anticancer therapy. An in vitro kinase assay demonstrated that DB inhibited the kinases EGF, MET, AKT1, and AKT2 (Fig. 3A). In support of the results of the in vitro kinase assay, DB was placed in the ATP-binding pocket of the kinases EGF, MET, AKT1, and AKT2. Moreover, DB treatment decreased phosphorylation levels (Fig. 4). In both HCC827 and HCC827GR cells, the phosphorylation of EGFR, MET, and AKT decreased, whereas the levels of these proteins remained unchanged. Conversely, GEF treatment alone was ineffective in reducing the phosphorylation of MET and AKT in HCC827GR cells, suggesting the potential of DB in treating GEF-resistant lung cancer. While it is unknown whether these protein kinases are direct molecular targets of DB, these results suggest that DB suppresses signaling through the EGFR/MET/AKT pathways. The regulation of AKT signaling pathway by DB is clinically relevant as AKT signaling is involved with GEF sensitivity28. Moreover, DB targets exactly where GEF is not useful: MET and AKT are highly activated in GEF-resistant lung cancer cells19.
Cell cycle regulation contributes to the cytotoxicity of anticancer therapeutics. GEF arrests cells at the G0/G1 phase29, and our results indicate that DB causes the accumulation of cells in the G2/M phase (Fig. 5A–C). To elucidate the molecular mechanisms underlying cell cycle arrest, we examined cyclins and cyclin-dependent kinases (CDKs). The formation of specific cyclins and CDKs is important in cell cycle progression30, and the cyclin B1/cdc2 complex is important in the transition to the G2/M phase31. DB treatment downregulated the expression of both cyclin B1 and cdc2 (Fig. 5D). We suspect that the upregulation of p27, an inhibitory protein of the cyclin/CDK complex, contributes to G2/M arrest32.
ROS generation is involved in various cellular, physiological, and pathophysiological processes33. Although mild ROS generation may contribute to tumorigenesis and cancer cell survival34, excessive ROS generation can be detrimental35. In this study, the level of cellular ROS increased in DB-treated cells (Fig. 6A). Pretreatment of cells with NAC (4 mM) prevented the apoptotic activity of DB, suggesting that an increase in ROS is involved in the regulation of DB-induced apoptosis (Fig. 6B). Indeed, the DB-induced downregulation of protein phosphorylation and PARP cleavage was prevented by NAC pretreatment (Fig. 6C). Notably, the downregulation of EGFR, MET, and AKT signaling induced by DB was not reversed by NAC pretreatment. This implies that EGFR/MET/AKT signaling is an upstream event in ROS generation.
The generation of excessive ROS can result in the dysregulation of MMP36. The loss of MMP may lead to apoptosis37 or necrosis-like cell death in lung cancer cells38. Upon DB treatment, depolarization of the mitochondrial membrane was observed through flow cytometry using a JC-1 probe (Fig. 7A). In line with the decrease in MMP, the balance between pro- and anti-apoptotic Bcl-2 family proteins was disturbed, which was accompanied by the release of cyto c and elevated levels of cleaved PARP and cleaved caspase-3 (Fig. 7B). The Annexin V/7-AAD double staining assay indicated that the number of apoptotic cells increased as the DB concentration increased (Fig. 8A,B). Multiple caspases were activated in both HCC827 and HCC827GR cells after DB treatment (Fig. 8C,D). Pretreatment with Z-VAD-FMK prevented DB-induced apoptosis (Fig. 8E). These results demonstrate that DB induces apoptosis by activating caspases.
In conclusion, our study showcases the efficacy of DB in inhibiting the growth of both GEF-sensitive and GEF-resistant HCC827 cells. Through in vitro experiments, we demonstrated that DB effectively targets the kinases EGFR, MET, and AKT. This inhibition of EGFR/MET/AKT signaling leads to cell cycle arrest, increased ROS production, MMP dysregulation, and the activation of multiple caspases (Fig. 9). The ability of DB to target multiple protein kinases underscores the importance of further investigation, offering potential avenues to overcome chemotherapy-resistant lung cancer.
Data availability
The datasets are available from the corresponding author on reasonable request.
Abbreviations
- 7-AAD:
-
7-Aminoactinomycin D
- MMP:
-
Mitochondrial membrane potential
- MTT:
-
3-(4,5-Dimethylthiazol-2-yl)-2,5 diphenyltetrazolium bromide
- NAC:
-
N-Acetyl-l-cysteine
- ROS:
-
Reactive oxygen species
- Z-VAD-FMK:
-
N-Benzyloxycarbonyl-Val-Ala-Asp(O-Me) fluoromethyl ketone
- DB:
-
Deoxybouvardin
- GEF:
-
Gefitinib
- SAV:
-
Savolitinib
- NSCLC:
-
Non-small cell lung cancer
References
Thandra, K. C., Barsouk, A., Saginala, K., Aluru, J. S. & Barsouk, A. Epidemiology of lung cancer. Contemp. Oncol. (Pozn.) 25, 45–52. https://doi.org/10.5114/wo.2021.103829 (2021).
Alduais, Y., Zhang, H., Fan, F., Chen, J. & Chen, B. Non-small cell lung cancer (NSCLC): A review of risk factors, diagnosis, and treatment. Medicine (Baltimore) 102, e32899. https://doi.org/10.1097/MD.0000000000032899 (2023).
Akhtar, N. & Bansal, J. G. Risk factors of Lung Cancer in nonsmoker. Curr. Probl. Cancer 41, 328–339. https://doi.org/10.1016/j.currproblcancer.2017.07.002 (2017).
Tian, X., Gu, T., Lee, M. H. & Dong, Z. Challenge and countermeasures for EGFR targeted therapy in non-small cell lung cancer. Biochim. Biophys. Acta Rev. Cancer 1877, 188645. https://doi.org/10.1016/j.bbcan.2021.188645 (2022).
Kris, M. G. et al. Efficacy of gefitinib, an inhibitor of the epidermal growth factor receptor tyrosine kinase, in symptomatic patients with non-small cell lung cancer: a randomized trial. JAMA 290, 2149–2158. https://doi.org/10.1001/jama.290.16.2149 (2003).
Griffin, R. & Ramirez, R. A. Molecular targets in non-small cell lung cancer. Ochsner. J. 17, 388–392 (2017).
Kobayashi, S. et al. EGFR mutation and resistance of non-small-cell lung cancer to gefitinib. N. Engl. J. Med. 352, 786–792. https://doi.org/10.1056/NEJMoa044238 (2005).
Ciardiello, F. et al. The role of anti-EGFR therapies in EGFR-TKI-resistant advanced non-small cell lung cancer. Cancer Treat Rev. 122, 102664. https://doi.org/10.1016/j.ctrv.2023.102664 (2024).
Narita, M. et al. Chronic treatment of non-small-cell lung cancer cells with gefitinib leads to an epigenetic loss of epithelial properties associated with reductions in microRNA-155 and -200c. PLoS One 12, e0172115. https://doi.org/10.1371/journal.pone.0172115 (2017).
Yang, J. J. et al. A phase Ib study of the highly selective MET-TKI savolitinib plus gefitinib in patients with EGFR-mutated, MET-amplified advanced non-small-cell lung cancer. Invest. New Drugs 39, 477–487. https://doi.org/10.1007/s10637-020-01010-4 (2021).
Circu, M. L. & Aw, T. Y. Reactive oxygen species, cellular redox systems, and apoptosis. Free Radic. Biol. Med. 48, 749–762. https://doi.org/10.1016/j.freeradbiomed.2009.12.022 (2010).
Weng, M. S., Chang, J. H., Hung, W. Y., Yang, Y. C. & Chien, M. H. The interplay of reactive oxygen species and the epidermal growth factor receptor in tumor progression and drug resistance. J. Exp. Clin. Cancer Res. 37, 61. https://doi.org/10.1186/s13046-018-0728-0 (2018).
Mohammad, R. M. et al. Broad targeting of resistance to apoptosis in cancer. Semin. Cancer Biol. 35(Suppl), S78–S103. https://doi.org/10.1016/j.semcancer.2015.03.001 (2015).
Bigot, A., Beugelmans, R. & Zhu, J. A formal total synthesis of deoxybouvardin. Tetrahedron 53, 10753–10764. https://doi.org/10.1016/S0040-4020(97)00706-0 (1997).
Jolad, S. D. et al. Bouvardin and deoxybouvardin, antitumor cyclic hexapeptides from Bouvardia ternifolia (Rubiaceae). J. Am. Chem. Soc. 99, 8040–8044. https://doi.org/10.1021/ja00466a043 (1977).
Kato, T. et al. Leukocytosis in mice following therapy with a novel antitumor agent, RA-700. Jpn. J. Cancer Res. 80, 290–293. https://doi.org/10.1111/j.1349-7006.1989.tb02307.x (1989).
Yue, G. G. et al. Cyclopeptide RA-V inhibits angiogenesis by down-regulating ERK1/2 phosphorylation in HUVEC and HMEC-1 endothelial cells. Br. J. Pharmacol. 164, 1883–1898. https://doi.org/10.1111/j.1476-5381.2011.01458.x (2011).
Son, Y. et al. Lucidin 3-methyl ether from Rubia philippinensis suppresses the proliferation of multiple myeloma cells through the promotion of beta-catenin degradation. Phytomedicine 99, 153971. https://doi.org/10.1016/j.phymed.2022.153971 (2022).
Engelman, J. A. et al. MET amplification leads to gefitinib resistance in lung cancer by activating ERBB3 signaling. Science 316, 1039–1043 (2007).
Trott, O. & Olson, A. J. AutoDock Vina: Improving the speed and accuracy of docking with a new scoring function, efficient optimization, and multithreading. J. Comput. Chem. 31, 455–461. https://doi.org/10.1002/jcc.21334 (2010).
Zalacain, M., Zaera, E., Vazquez, D. & Jimenez, A. The mode of action of the antitumor drug bouvardin, an inhibitor of protein synthesis in eukaryotic cells. FEBS Lett. 148, 95–97. https://doi.org/10.1016/0014-5793(82)81250-7 (1982).
Bates, R. B. et al. Solution forms of bouvardin and relatives from NMR studies. 6-O-Methylbouvardin. J. Am. Chem. Society. 105, 1343–1347. https://doi.org/10.1021/ja00343a045 (1983).
Wang, X., Zhang, H. & Chen, X. Drug resistance and combating drug resistance in cancer. Cancer Drug Resist. 2, 141–160. https://doi.org/10.20517/cdr.2019.10 (2019).
Saldana-Rivera, L., Bello, M. & Mendez-Luna, D. Structural insight into the binding mechanism of ATP to EGFR and L858R, and T790M and L858R/T790 mutants. J. Biomol. Struct. Dyn. 37, 4671–4684. https://doi.org/10.1080/07391102.2018.1558112 (2019).
Engelman, J. A. & Janne, P. A. Mechanisms of acquired resistance to epidermal growth factor receptor tyrosine kinase inhibitors in non-small cell lung cancer. Clin. Cancer Res. 14, 2895–2899. https://doi.org/10.1158/1078-0432.CCR-07-2248 (2008).
Peng, L. X. et al. MET amplification identified by next-generation sequencing and its clinical relevance for MET inhibitors. Exp. Hematol. Oncol. 10, 52. https://doi.org/10.1186/s40164-021-00245-y (2021).
Kim, J. Y. et al. Phosphoproteomics reveals MAPK inhibitors enhance MET- and EGFR-driven AKT signaling in KRAS-mutant lung cancer. Mol. Cancer Res. 14, 1019–1029. https://doi.org/10.1158/1541-7786.MCR-15-0506 (2016).
Wang, Q., Shen, B., Qin, X., Liu, S. & Feng, J. Akt/mTOR and AMPK signaling pathways are responsible for liver X receptor agonist GW3965-enhanced gefitinib sensitivity in non-small cell lung cancer cell lines. Transl. Cancer Res. 8, 66–76. https://doi.org/10.21037/tcr.2018.12.34 (2019).
Wu, M., Yuan, Y., Pan, Y.-Y. & Zhang, Y. Combined gefitinib and pemetrexed overcome the acquired resistance to epidermal growth factor receptor tyrosine kinase inhibitors in non-small cell lung cancer. Mol. Med. Rep. 10, 931–938. https://doi.org/10.3892/mmr.2014.2243 (2014).
Eymin, B. & Gazzeri, S. Role of cell cycle regulators in lung carcinogenesis. Cell Adh. Migr. 4, 114–123. https://doi.org/10.4161/cam.4.1.10977 (2010).
Shang, Z. F. et al. DNA-PKcs negatively regulates cyclin B1 protein stability through facilitating its ubiquitination mediated by Cdh1-APC/C pathway. Int. J. Biol. Sci. 11, 1026–1035. https://doi.org/10.7150/ijbs.12443 (2015).
Lee, S. O. et al. Licochalcone C inhibits the growth of human colorectal cancer HCT116 cells resistant to oxaliplatin. Biomol. Ther. (Seoul) 32, 104–114. https://doi.org/10.4062/biomolther.2023.167 (2024).
Checa, J. & Aran, J. M. Reactive oxygen species: Drivers of physiological and pathological processes. J. Inflamm. Res. 13, 1057–1073. https://doi.org/10.2147/JIR.S275595 (2020).
Chun, K. S. & Joo, S. H. Modulation of Reactive oxygen species to overcome 5-fluorouracil resistance. Biomol. Ther. (Seoul) 30, 479–489. https://doi.org/10.4062/biomolther.2022.017 (2022).
Li, A. X., Sun, M. & Li, X. Withaferin-A induces apoptosis in osteosarcoma U2OS cell line via generation of ROS and disruption of mitochondrial membrane potential. Eur. Rev. Med. Pharmacol. Sci. 21, 1368–1374 (2017).
Zorov, D. B., Juhaszova, M. & Sollott, S. J. Mitochondrial reactive oxygen species (ROS) and ROS-induced ROS release. Physiol. Rev. 94, 909–950. https://doi.org/10.1152/physrev.00026.2013 (2014).
Yang, S. et al. Sesamin induces A549 cell mitophagy and mitochondrial apoptosis via a reactive oxygen species-mediated reduction in mitochondrial membrane potential. Korean J. Physiol. Pharmacol. 24, 223–232. https://doi.org/10.4196/kjpp.2020.24.3.223 (2020).
Zhang, Y. X., Yu, P. F., Gao, Z. M., Yuan, J. & Zhang, Z. Caffeic acid n-butyl ester-triggered necrosis-like cell death in lung cancer cell line A549 is prompted by ROS mediated alterations in mitochondrial membrane potential. Eur. Rev. Med. Pharmacol. Sci. 21, 1665–1671 (2017).
Acknowledgements
This work was supported by the National Research Foundation of Korea (NRF) Grants funded by the Korea Government (MSIT) (2022R1A5A8033794, RS-2024-00336900, and RS-2023-00246380).
Author information
Authors and Affiliations
Contributions
A-Young Nam: Conceptualization and design of research, Investigation, and Writing of original draft. Sang Hoon Joo: Conceptualization and design of research, visualization, review, and editing. Quan T. Khong: Conceptualization and design of research. Jisu Park: Investigation and curation of data. Na Yeong Lee: Investigation. Seung-On Lee: Investigation and Resources. Goo Yoon: Resources. Jin Woo Park: Conceptualization and design of research, and Investigation. MinKyun Na: Project administration, Funding acquisition, Final review, and confirm of writing. Jung-Hyun Shim: Project administration, Funding acquisition, Supervision, and Final review and confirm of writing.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Nam, AY., Joo, S.H., Khong, Q.T. et al. Deoxybouvardin targets EGFR, MET, and AKT signaling to suppress non-small cell lung cancer cells. Sci Rep 14, 20820 (2024). https://doi.org/10.1038/s41598-024-70823-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-70823-7
- Springer Nature Limited