Abstract
Social isolation was associated with emotional problems (depression and anxiety) among older adults, however, little is known in China. Thus, we conducted a cross-sectional study including 6,664 ≥ 65 years older adults in Ningbo, China. We collected data on social isolation, depression, and anxiety by specific scales. The relationship between social isolation and emotional problems was estimated by multivariate-adjusted logistic regression models. The population–attributable risk percentage (PAR%) was used to explore the contribution of social isolation to emotional problems. Overall, the percentage of participants who had experienced social isolation, depression, and anxiety was 12.67%, 4.83%, and 2.63%. Compared with the elderly without social isolation, the adjusted odds ratios (95% confidence interval) of depression and anxiety with social isolation were 1.77 (1.25–2.51) and 1.66 (1.05–2.63), respectively. The PAR analysis showed that 10.66% of depression and 9.03% of anxiety could be attributable to social isolation. In the gender subgroup, ORs and PAR% were only significantly observed in female participants. In Chinese older adults, social isolation has been linked to depression and anxiety, suggesting the importance of taking effective and feasible interventions to reduce social isolation and emotional problems, especially among females.
Similar content being viewed by others
Introduction
Depression and anxiety are the most frequent emotional problems experienced by older adults worldwide1. In China, nearly 3.8% and 4.7% of older adults (over 65 years) were reported to suffer from depressive and anxiety disorders, respectively2, resulting in a high burden of disease in this population. Depression and anxiety are generated both by biological factors (e.g., sex, somatic illness, functional disability) and psychosocial factors (e.g., low contact frequency, a childless or unmarried status)3. Changes in some psychosocial factors may reduce emotional problems in older adults3.
Social isolation refers to a poor living condition involving a lack of social contact and participation or inadequate social interactions with friends, relatives, and others4. Social isolation can be measured by the following variables: whether one lives alone, the frequency of conversations with relatives and friends, and the frequency of participation in social activities5. A study conducted in the United States found that approximately 24.0% of community-dwelling adults older than 65 years old were socially isolated6. Two studies conducted in China showed that the prevalence of social isolation was 29.7% among community-dwelling older adults in Qingdao7 and 28.9% among their counterparts in Shanghai8.
Studies generally have recognized the profound negative effect of social isolation on physical and mental health9,10. The longitudinal Aging Social Survey found that social isolation independently determined the probability of depression in both China11 and the Netherlands12. A study in Ireland13 found that objective social isolation independently affected the process of depression or anxiety. However, no study has explored the proportion of cases of depression and anxiety that might be prevented by alleviating social isolation among older adults. Previous research has indicated that various factors are linked to depression and anxiety among older individuals. Age has been consistently identified as a primary contributing factor to the heightened risk of mental health14,15. Additionally, social and demographic variables, including education status15, marital status16, and household income17 have been shown to correlate with increased prevalence of mental health concerns in older adults. Furthermore, substance use18, lifestyle behaviors18,19, and sleep behaviors20 have been found to have significant associations with mental health outcomes in this population. Self-rated health21 and chronic disease16 have also been identified as relevant factors linked to mental health.
Thus, in our study, we aimed to determine the current prevalence of social isolation, depression, and anxiety symptoms among community-dwelling older adults in Ningbo, China, and to investigate the relationships between these variables, including (1) the adjusted associations of social isolation with depression and anxiety, (2) the adjusted population attributable risk percentage (PAR%) for social isolation among cases of depression and anxiety, (3) the adjusted associations and PAR% in the gender subgroup.
Methods
Study design and population
Ningbo, situated in the Yangtze River Delta region of China, is a prominent city with six districts and four counties. As of 2022, its population reached approximately 9.6 million, with 1.4 million individuals aged 65 and older. A cross-sectional study of older adults (aged 65 years and older) in Ningbo, China was conducted from June to August 2022. Two community units in each district and county in Ningbo were randomly selected by computer generation and included all participants in each unit who met the inclusion criteria in our study. The inclusion criteria were (1) residence in the selected communities for more than one year, (2) an age of 65 years or older, and (3) the ability to understand our questionnaires, with no serious mental illness. The exclusion criteria were the absence of key variables in participants. All of the questionnaires were completed by the participants during face-to-face sessions with community workers. For participants who could not complete the paper questionnaire without assistance, the community workers verbally read the questions and completed the questionnaires according to the participants’ answers. Ethical approval for this study was obtained from the Ethics Committee of Ningbo Kangning Hospital, and written informed consent was obtained from all participants.
Defining depression and anxiety
Depression and anxiety were assessed using a validated 9-item Patient Health Questionnaire (PHQ-9) and a 7-item validated Generalized Anxiety Disorder (GAD-7) scale; these measures were based on the participants’ experiences over the previous 2 weeks, and each item was rated on a 4-point scale: “not at all” = 0, “several days” = 1, “more than half of the days” = 2, and “nearly every day” = 3. The total scores of the PHQ-9 and GAD-7 ranged from 0 to 27 and from 0 to 21, respectively. The Chinese versions of the PHQ-9 and GAD-7 have both been shown to have good reliability and validity for screening anxiety22 and depression23. As previously recommended24,25, we used the screening cutoff score of 10 for both scales, and a score ≥ 10 corresponded to at least a moderate level of depression or anxiety. A PHQ-9 score 10 had a sensitivity (the probability of a positive test given that the elderly has the disease) of 88% and a specificity (the probability of a negative test given that the elderly is well) of 88% for major depression26, A GAD-7 score 10 had a sensitivity of 89% and a specificity of 82% for generalized anxiety disorder25.
Defining social isolation
Social isolation was assessed using three questions that addressed whether the participant lived alone (yes = 1, no = 0), had social contact (contacted less than once per month = 1, other = 0), and participated in social activities (participated less than once per week = 1, other = 0); these questions have been described elsewhere5,27. We then summed the scores of the responses to these questions, and a score of 2 or 3 was considered to indicate social isolation27.
Covariates
All of the covariates were based on baseline data. The sociodemographic characteristics included age (continuous), gender (male, female), residence location (urban, rural), education (< 6 or ≥ 6 years), marital status (married or widowed/divorced/never married), and pension income (< 2000, 2000–5000, or > 5000 CNY/month). Additional covariates included the participants’ self-rated health (good, intermediate, or poor) and number of chronic non-communicable diseases (0, 1, 2, ≥ 3).
Substance use included two aspects: alcohol consumption (never, former, or current) and smoking (never, former, or current). Lifestyle behaviors included three aspects: sedentary time per day (< 3, 3–5, or > 5 h/day), physical activity performance per week (< 3 or ≥ 3 times/week), and a self-reported healthy diet (yes or no). Sleep behaviors included two aspects: sleep disturbance (difficulty falling asleep or waking up after falling asleep) over the past week (0, 1–2, 3–4, or 5–7 times/week) and sleep duration over the past week (< 6, 6–8, > 8 h/day).
Statistical analysis
The participants’ baseline characteristics were compared using the t-test for continuous variables and the chi-squared test for categorical variables. We estimated the proportions of participants with social isolation, depression, and anxiety in all population and gender subgroup. The links between social isolation and depression and anxiety were computed using a multivariate-adjusted logistic regression model and are reported as adjusted odds ratios (AORs). Population attributable risk percentages (PAR%)28 were calculated to assess the proportions of cases of depression and anxiety that could potentially be prevented if social isolation were mitigated among older adults. The calculation was based on the formula reported by Bruzzi et al.28: PAR% = 1 − \(\sum_{j}\frac{{P}_{j}}{\begin{array}{c}\sim \\ {R}_{j}\end{array}}\), where j is 1, 2, 3, … level; Pj is the ratio of the number of cases to the total number of cases at the j level; and \({\begin{array}{c}\sim \\ R\end{array}}_{j}\) is the relative risk of the exposure factor level adjusted for other factors at the j level. In the statistical analysis, P values < 0.05 were considered statistically significant. All the statistical analyses were completed by SAS version 9.4 (SAS Institute, Cary, NC, USA) .
Ethics statement
This work was conducted in accordance with the principles of the Declaration of Helsinki and ethics approval (NBKNYY-2023-LC-29) was obtained from the Ethics Committee of Ningbo Kangning Hospital, and written informed consent was obtained from all participants.
Results
In total, 6,664 community-dwelling older adults were recruited for this study (response rate was 84.9%), of whom 45.50% were men. In Table 1, the men were significantly older than the women (72.89 ± 6.25 vs. 72.40 ± 6.05 years, P = 0.001). The percentages of participants who were current alcohol drinkers and smokers were higher among men than among women (Table 1). The percentage of participants who participated in physical activity more than 3 times/week was lower among men than among women (Table 1). Compared with women, men had better sleep disturbance and sleep duration status (P < 0.001 for both) (Table 1).
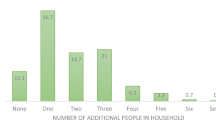
Overall, 12.67% of the participants reported that they had experienced social isolation, and the rate of social isolation was significantly higher among women than among men (15.66% vs. 9.10%, P < 0.05, Fig. 1). The prevalence of depression and anxiety among the participants was 4.83% and 2.63%, respectively. Univariate logistic regression analysis showed that age, sedentary, sleep disturbance, social isolation, and more diseases were significantly positively linked with depression and anxiety. Meanwhile, higher pension income, being in marital status, physical activity, longer sleep duration, healthy diet, and self-rated health were significantly negatively linked with depression and anxiety (Fig. 2).
Multivariate logistic regression analysis showed that older adults who had experienced social isolation were 1.77 times more likely to have depression than those who were not socially isolated (AOR = 1.77, 95% confidence interval [CI]: 1.25–2.51, P < 0.001, Table 2). Social isolation also was significantly associated with an increased likelihood of anxiety in older adults (AOR = 1.66, 95% CI: 1.05–2.63, P = 0.029, Table 2) after controlling for multiple variables. However, no significant associations of social isolation with depression and anxiety were observed in male participants [AOR (95% CI) = 1.42 (0.77–2.58) and 0.98 (0.42–2.26), respectively; P > 0.05 for both]. In contrast, female participants who had experienced social isolation were 1.99 and 1.92 times more likely to have depression and anxiety, respectively, than those who had not experienced social isolation, and these results were significant (P < 0.05 for both, Table 2).
The results regarding the adjusted PAR% for social isolation are shown in Table 3. Among our participants, the PAR% related to social isolation was as high as 10.66% and 9.03% for depression and anxiety, respectively. Besides, the adjusted PAR% related to social isolation were as high as 15.12% and 12.84% for depression and anxiety in women. The adjusted PAR% of social isolation were no statistical significance for depression and anxiety in men (Table 4).
Discussion
This study investigated the prevalence of social isolation, depression, and anxiety in a sample of community-dwelling older adults in Ningbo, China. Overall, 12.67% of the participating older adults reported having experienced social isolation, and the prevalence of depression and anxiety in this population was 4.83% and 2.63%, respectively. The participants who had experienced social isolation were more likely to have depression and anxiety than those who were not socially isolated. Furthermore, our results shed light on some key intermediate factors that affected the relationship between social isolation and increased risks of depression and anxiety.
The participants who had experienced social isolation had 1.77 and 1.66 times greater odds of having depression and anxiety than those who were not socially isolated, which was congruent with the findings of earlier studies. For example, in a study of Irish older adults, the lowest level of social isolation was associated with a 43% and 52% probability of depression or anxiety13. Furthermore, social disconnectedness could predict an increase in subsequent depression and anxiety symptoms due to an increase in perceived isolation among older adults in the United States29. Moreover, social isolation at baseline predicted higher depression and anxiety scores at follow-up (incidence rate ratio = 1.35 and 1.32, respectively) in a study of older adults in Shanghai8. As we have seen, it does seem depressive symptoms are understudied in the elderly in social isolation studies in China, but this does not seem to be true for other East Asia generally. In the results of their studies, social isolation has been actively linked to depressive symptoms in the elderly in Japan30,31 and South Korea32,33,34. Depression and anxiety share a biological mechanism of activation via the hypothalamic–pituitary–adrenal (HPA) axis, which may explain their associations with social isolation35. The HPA axis is a major stress response system in humans. Studies have suggested that social isolation increases the activation of the HPA axis in humans36. Research findings also have confirmed the possibility of excess HPA axis activity in people with both depression and anxiety 37. Thus, social isolation may make older adults more vulnerable to depression and anxiety via activation of the HPA axis35.
In our study, we first found that the PAR% of social isolation was 10.66% and 9.03% for depression and anxiety, respectively, suggesting that eliminating social isolation could reduce depression and anxiety in older adults by almost 10%. In this regard, sufficient attention should be paid to social isolation among older adults, who should be motivated to change their situation and seek relevant help. Moreover, measures to reduce social isolation are needed. Potential interventions for eliminating social isolation among older adults include (1) improving their interpersonal communication skills through lectures and training, (2) increasing regular contact with or the provision of companionship or care for them, (3) offering opportunities for them to engage in social interaction (e.g., community activities), and (4) changing their cognition about social isolation and social support38,39. Social isolation is the objective absence of social relations, meanwhile, loneliness is the subjective experience of the lack of social relations35. Although social isolation and loneliness are not exactly equivalent, potential interventions for eliminating social isolation among older adults might partly mitigate their loneliness, and further alleviate mental unhealth40.
It is evident that elderly women are more likely to experience social isolation. In 2019, the average life expectancy in China was 77.7 years, with a gender disparity of 6.2 years favoring women. This gap is projected to widen to 7.0 years by 203541. Consequently, elderly women are more likely to experience widowhood and live alone, thereby heightening their risk of social isolation. Furthermore, the association and PAR% of social isolation with depression and anxiety were found to be significant exclusively among elderly women. Gender differences in response to social isolation may be partially attributable to sexually dimorphic reactions. In male mice subjected to social isolation, increased dopamine release was observed during subsequent social interactions, leading to enhanced pleasurable sensations. This, in turn, fostered a heightened desire for social engagement42. The phenomenon was not observed in female mice. Consequently, this can explain the reason for the impact of social isolation appeared to be mitigated in males.
Strengths and limitations
The strengths of the current study include a large sample size and the use of validated scales to measure social isolation, depression, and anxiety. In addition, the PAR% of social isolation in depression and anxiety was first explored. However, this study has several limitations. First, all of the participants were recruited from communities in Ningbo, and therefore the conclusions may not be generalizable to other regions in China. Second, this was a cross-sectional study, and therefore causal associations cannot be assumed. Longitudinal studies of the relationships of social isolation with depression and anxiety will be needed to infer causality. In addition. although we adjusted for as many confounders as possible, this was an observational study, and therefore we cannot rule out the possibility of residual confounders. Third, all of the data included in the analyses were based on self-reports, suggesting the possibility of reporting bias. The scales for depression and anxiety were based on self-reports rather than clinical assessments and diagnoses, which may also contribute to different results. Fourth, some of the participants had poor health status (such as having difficulty in reading or writing) and required assistance from the interviewers to complete their questionnaires, which may have increased the risk of social desirability bias.
Conclusions
In conclusion, this study highlights the associations of social isolation with increased risks of depression and anxiety among older adults, especially among females. The findings from this study suggest the importance of identifying older adults who are at risk of social isolation, especially among females. Effective and feasible interventions are needed to eliminate social isolation and pay attention to mental health in this population.
Data availability
The data that support the findings of this study are not openly available due to reasons of sensitivity and are available from the corresponding author upon reasonable request. Data are located in controlled access data storage at Affiliated Kangning Hospital of Ningbo University.
References
Byers, A. L., Yaffe, K., Covinsky, K. E., Friedman, M. B. & Bruce, M. L. High occurrence of mood and anxiety disorders among older adults: The national comorbidity survey replication. Arch. Gen. Psychiatr. 67, 489–496. https://doi.org/10.1001/archgenpsychiatry.2010.35 (2010).
Huang, Y. et al. Prevalence of mental disorders in China: A cross-sectional epidemiological study. Lancet Psychiatr. 6, 211–224. https://doi.org/10.1016/S2215-0366(18)30511-X (2019).
Vink, D., Aartsen, M. J. & Schoevers, R. A. Risk factors for anxiety and depression in the elderly: A review. J. Affect. Disord. 106, 29–44. https://doi.org/10.1016/j.jad.2007.06.005 (2008).
Nicholson, N. R. A review of social isolation: An important but underassessed condition in older adults. J. Prim. Prev. 33, 137–152. https://doi.org/10.1007/s10935-012-0271-2 (2012).
Cudjoe, T. K. M. et al. The epidemiology of social isolation: National health and aging trends study. J. Gerontol. B Psychol. Sci. Soc. Sci. 75, 107–113. https://doi.org/10.1093/geronb/gby037 (2020).
Donovan, N. J. & Blazer, D. Social isolation and loneliness in older adults: Review and commentary of a national academies report. Am. J. Geriatr. Psychiatr. 28, 1233–1244. https://doi.org/10.1016/j.jagp.2020.08.005 (2020).
Zhao, D., Zhao, M., Wang, N., Fu, M. & Wang, A. Relationships among social isolation, depression, loneliness and quality of life in the community-dweling elderly. J. Nurs. Sci. 35, 92–95 (2020).
Zhang, Y. et al. Loneliness, social isolation, depression and anxiety among the elderly in Shanghai: Findings from a longitudinal study. Arch. Gerontol. Geriatr. 110, 104980. https://doi.org/10.1016/j.archger.2023.104980 (2023).
Choi, H., Irwin, M. R. & Cho, H. J. Impact of social isolation on behavioral health in elderly: Systematic review. World J. Psychiatr. 5, 432–438. https://doi.org/10.5498/wjp.v5.i4.432 (2015).
Teo, A. R., Lerrigo, R. & Rogers, M. A. The role of social isolation in social anxiety disorder: A systematic review and meta-analysis. J. Anxiety Disord. 27, 353–364. https://doi.org/10.1016/j.janxdis.2013.03.010 (2013).
Cheng, X., Liu, Y. & Ge, T. The association and mechanism between social isolation, loneliness and mental health of older people. Popul. Dev. 26, 76–84 (2020).
Houtjes, W. et al. The impact of an unfavorable depression course on network size and loneliness in older people: A longitudinal study in the community. Int. J. Geriatr. Psychiatr. 29, 1010–1017. https://doi.org/10.1002/gps.4091 (2014).
Domenech-Abella, J., Mundo, J., Haro, J. M. & Rubio-Valera, M. Anxiety, depression, loneliness and social network in the elderly: Longitudinal associations from The Irish Longitudinal Study on Ageing (TILDA). J. Affect. Disord. 246, 82–88. https://doi.org/10.1016/j.jad.2018.12.043 (2019).
Liu, H. et al. Age-related positivity effect of emotional attention: Time and frequency domain. Psychol. Health Med. 28, 1599–1610. https://doi.org/10.1080/13548506.2022.2050271 (2023).
Tsaras, K. et al. Assessment of depression and anxiety in breast cancer patients: Prevalence and associated factors. Asian Pac. J. Cancer Prev. 19, 1661–1669. https://doi.org/10.22034/APJCP.2018.19.6.1661 (2018).
He, Z. F. et al. Prevalence and factors associated with depression and anxiety among older adults: A large-scale cross-sectional study in China. J. Affect. Disord. 346, 135–143. https://doi.org/10.1016/j.jad.2023.11.022 (2024).
Yang, Z. et al. Prevalence and related factors of depression and anxiety in a cohort of Chinese elderly caregivers in the nursing home. J. Affect. Disord. 295, 1456–1461. https://doi.org/10.1016/j.jad.2021.09.026 (2021).
Yang, G. & D’Arcy, C. The changing relationship between health risk behaviors and depression among birth cohorts of Canadians 65+, 1994–2014. Front. Psychiatr. 13, 1078161. https://doi.org/10.3389/fpsyt.2022.1078161 (2022).
Xu, W. Q. et al. The role of depression and anxiety in the relationship between poor sleep quality and subjective cognitive decline in Chinese elderly: Exploring parallel, serial, and moderated mediation. J. Affect. Disord. 294, 464–471. https://doi.org/10.1016/j.jad.2021.07.063 (2021).
Zhao, Y., Song, J., Brytek-Matera, A., Zhang, H. & He, J. The relationships between sleep and mental and physical Health of Chinese elderly: Exploring the mediating roles of diet and physical activity. Nutrients 13, 1316. https://doi.org/10.3390/nu13041316 (2021).
Shi, C., Yan, J., Wang, L. & Shen, H. Exploring the self-reported physical fitness and self-rated health, mental health disorders, and body satisfaction among Chinese adolescents: A cross-sectional study. Front. Psychol. 13, 1003231. https://doi.org/10.3389/fpsyg.2022.1003231 (2022).
He, X., Li, C., Qian, J., Cui, H. & Wu, W. Reliability and validity of a generalized anxiety disorder scale in general hospital outpatient. Shanghai Arch. Psych. 22, 200–203. https://doi.org/10.3969/j.issn.1002-0829.2010.04.002 (2010).
Sun, X., Li, Y., Yu, C. & Li, L. Reliability and validity of depression scales of chinese version: A systematic review. Zhonghua Liu Xing Bing Xue Za Zhi 38, 110–116. https://doi.org/10.3760/cma.j.issn.0254-6450.2017.01.021 (2017).
Manea, L., Gilbody, S. & McMillan, D. Optimal cut-off score for diagnosing depression with the Patient Health Questionnaire (PHQ-9): A meta-analysis. CMAJ 184, E191-196. https://doi.org/10.1503/cmaj.110829 (2012).
Spitzer, R. L., Kroenke, K., Williams, J. B. & Lowe, B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch. Intern. Med. 166, 1092–1097. https://doi.org/10.1001/archinte.166.10.1092 (2006).
Kroenke, K., Spitzer, R. L. & Williams, J. B. The PHQ-9: Validity of a brief depression severity measure. J. Gen. Intern. Med. 16, 606–613. https://doi.org/10.1046/j.1525-1497.2001.016009606.x (2001).
Shen, C. et al. Associations of social isolation and loneliness with later dementia. Neurology https://doi.org/10.1212/WNL.0000000000200583 (2022).
Bruzzi, P., Green, S. B., Byar, D. P., Brinton, L. A. & Schairer, C. Estimating the population attributable risk for multiple risk factors using case-control data. Am. J. Epidemiol. 122, 904–914. https://doi.org/10.1093/oxfordjournals.aje.a114174 (1985).
Santini, Z. I. et al. Social disconnectedness, perceived isolation, and symptoms of depression and anxiety among older Americans (NSHAP): A longitudinal mediation analysis. Lancet Public Health 5, e62–e70. https://doi.org/10.1016/S2468-2667(19)30230-0 (2020).
Inoue, K. et al. Social isolation and depressive symptoms among older adults: A multiple bias analysis using a longitudinal study in Japan. Ann. Epidemiol. 77, 110–118. https://doi.org/10.1016/j.annepidem.2022.11.001 (2023).
Noguchi, T. et al. Association between social isolation and depression onset among older adults: A cross-national longitudinal study in England and Japan. BMJ Open 11, e045834. https://doi.org/10.1136/bmjopen-2020-045834 (2021).
Lee, G. & Kim, C. Social isolation and mental well-being among Korean older adults: A focus on living arrangements. Front. Public Health 12, 1390459. https://doi.org/10.3389/fpubh.2024.1390459 (2024).
Lim, Y. M., Baek, J., Lee, S. & Kim, J. S. Association between loneliness and depression among community-dwelling older women living alone in South Korea: The mediating effects of subjective physical health, resilience, and social support. Int. J. Environ. Res. Public Health 19, 9246. https://doi.org/10.3390/ijerph19159246 (2022).
Koo, J. H., Son, N. & Yoo, K. B. Relationship between the living-alone period and depressive symptoms among the elderly. Arch. Gerontol. Geriatr. 94, 104341. https://doi.org/10.1016/j.archger.2021.104341 (2021).
Kanbay, M. et al. Social isolation and loneliness: Undervalued risk factors for disease states and mortality. Eur. J. Clin. Invest. 53(10), e14032. https://doi.org/10.1111/eci.14032 (2023).
Cacioppo, J. T., Cacioppo, S., Capitanio, J. P. & Cole, S. W. The neuroendocrinology of social isolation. Annu. Rev. Psychol. 66, 733–767. https://doi.org/10.1146/annurev-psych-010814-015240 (2015).
Juruena, M. F., Eror, F., Cleare, A. J. & Young, A. H. The role of early life stress in HPA axis and anxiety. Adv. Exp. Med. Biol. 1191, 141–153. https://doi.org/10.1007/978-981-32-9705-0_9 (2020).
Masi, C. M., Chen, H. Y., Hawkley, L. C. & Cacioppo, J. T. A meta-analysis of interventions to reduce loneliness. Pers. Soc. Psychol. Rev. 15, 219–266. https://doi.org/10.1177/1088868310377394 (2011).
Fakoya, O. A., McCorry, N. K. & Donnelly, M. Loneliness and social isolation interventions for older adults: A scoping review of reviews. BMC Public Health 20, 129. https://doi.org/10.1186/s12889-020-8251-6 (2020).
Czaja, S. J., Moxley, J. H. & Rogers, W. A. Social support, isolation, loneliness, and health among older adults in the PRISM randomized controlled trial. Front. Psychol. 12, 728658. https://doi.org/10.3389/fpsyg.2021.728658 (2021).
Bai, R. et al. Projections of future life expectancy in China up to 2035: A modelling study. Lancet Public Health 8, e915–e922. https://doi.org/10.1016/S2468-2667(22)00338-3 (2023).
Choi, J. E. et al. Synaptic ensembles between raphe and D(1)R-containing accumbens shell neurons underlie postisolation sociability in males. Sci. Adv. 8, eabo7527. https://doi.org/10.1126/sciadv.abo7527 (2022).
Acknowledgements
The authors express their gratitude to the doctors from the office of Mental health and the community health service center who were involved in the data collection.
Funding
This work was supported by the Ningbo Medical & Health Leading Academic Discipline Project (2022-F28), Ningbo Top Medical and Health Research Program (2022030410) and Ningbo Medical and Health Brand Discipline (PPXK2018-08).
Author information
Authors and Affiliations
Contributions
L.L. conceived and designed the study, performed the statistical analysis, and drafted the article. K.P., J.L., M.J., and Y.G. collected the data. Hongying Yang and Guolin Bian contributed to the study design and the article’s critical revision. All authors revised the article and approved the final version.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Li, L., Pan, K., Li, J. et al. The associations of social isolation with depression and anxiety among adults aged 65 years and older in Ningbo, China. Sci Rep 14, 19072 (2024). https://doi.org/10.1038/s41598-024-69936-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-69936-w
- Springer Nature Limited