Abstract
Rhegmatogenous retinal detachment (RRD) is a sight-threatening condition with rising global incidence. Identifying factors contributing to seasonal variations in RRD would allow a better understanding of RRD pathophysiology. We therefore performed a retrospective case series study investigating the relationship between RRD occurrence and meteorological factors throughout metropolitan France (the METEO-POC study), particularly the mean temperature over the preceding 10-day period (T-1). Adult patients having undergone RRD surgery and residing in one of the three most populated urban areas of each French region were included (January 2011–December 2018). The study involved 21,166 patients with idiopathic RRD (61.1% males, mean age 59.8–65.1 years). RRD incidence per 100,000 inhabitants increased from 7.79 to 11.81. RRD occurrence was not significantly associated with mean temperature over T-1 in the majority of urban areas (31/36). In a minority of areas (5/36) we observed correlations between RRD incidence and mean temperature over T-1, however these were extremely weak (r = 0.1–0.2; p < 0.05). No associations were found between RRD incidence and secondary outcomes: mean daily temperature over the 10 days prior T-1, minimum/maximum temperatures, rainfall, duration of sunshine, atmospheric pressure, overall radiation, relative humidity, wind speed. Overall, we found no relationships between meteorological parameters and RRD occurrence.
Similar content being viewed by others
Introduction
The three different types of retinal detachment, rhegmatogenous, tractional, or exudative, can be distinguished by their underlying etiology of sub-retinal fluid accumulation and resulting retinal uplift. We focus here on rhegmatogenous retinal detachment (RRD), which generally follows the onset of a retinal break or tear. This leads to infiltration of vitreous fluid into the subretinal space when left untreated. Tractional retinal detachment is due to retinal pulling caused by trauma-related or diabetes-related fibrotic phenomena, and exudative retinal detachment is characterized by blood-retinal barrier disruption without retinal breaks or traction1,2.
RRD is a potentially blinding condition that affects around 1 in every 10,000 people per year worldwide2. RRD treatment is almost always surgical and must be carried out within a reasonable delay in order to preserve the patient's visual prognosis3,4. Developing strategies to prevent this condition is an important public health challenge given the global incidence of RRD continues to rise. Improved understanding of the factors affecting RRD pathophysiology may help clinicians to better anticipate RRD patient influx and plan surgery times accordingly.
Clinicians frequently report fluctuations in RRD patient intake, suggesting that environmental factors may play a role in triggering the onset of RRD. Elevated temperatures are known to increase the risk of dehydration and contraction of the vitreous, and this may promote retinal detachment5. Several studies worldwide have found that the rate of RRD incidence is 1.3 to 1.7 times higher in summer than in winter5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20. Conversely, others found no significant difference between these two seasons21,22,23,24,25, or the presence of a peak in winter26. Some studies have focused on the meteorological parameters potentially involved. However, they often included small numbers of patients and did not reach a consensus5,8,11,14,15,16,19. The only study to have analyzed a large number of patients was conducted in Taiwan on 23,718 cases over 11 years. It found a positive correlation between the incidence of retinal detachment and ambient temperature20.
In France, so far only one national study has investigated seasonal variation of RRD27. The authors analyzed 101,085 patients with RRD between 2010 and 2016. They found a peak in incidence in June and July, but a minimum incidence in August. The authors proposed that the lower RRD incidence in August may relate to school holidays, as the majority of the French population were on vacation, especially abroad, at this time27,28. The study did not, however, study any meteorological parameters.
Here we set out to investigate the meteorological parameters associated with RRD incidence throughout metropolitan France over a period of 8 years. The main objective of this study was to evaluate the association between the occurrence of RRD and the mean temperature over the preceding 10-day period. The secondary objectives were to describe the national incidence of RRD, but also to study the association between RRD occurrence and other meteorological parameters.
Results
The French National Health Insurance Fund (Caisse Nationale d’Assurance Maladie—CNAM) selected 48,590 patients with a hospital diagnosis of idiopathic RRD (of unknown etiology, not secondary to systemic diseases or trauma) that underwent surgical treatment during the study period. We excluded 8,543 patients because they did not reside in one of the 36 urban areas of interest. A further 18,881 patients were excluded because they did not reside in the urban area where they had undergone surgery. Our final study population included 21,166 patients with idiopathic RRD (Fig. 1).
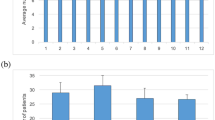
The number of patients admitted to hospital with idiopathic RRD in the same region as their region of residence in metropolitan France increased every year throughout the study. The incidence rate per 100,000 inhabitants was 7.79 in 2011; it increased on a yearly basis, reaching 11.81 in 2018 (eTable 1 and eFig. 1 in the Supplement).
Among our case series, we found a predominance of males (61.1%), and a mean age ranging from 59.8 to 65.1 years (SD 9.5–14.5), depending on the urban area. Paris was the urban area with the most patients studied, followed by Lyon, Toulouse, Marseille-Aix-en-Provence and Nantes (Fig. 2). In each urban area, the proportion of RRD patients who lived in the same residential area as their treatment hospital varied, with a minimum of 23.5% in Besançon and a maximum of 91.2% in Paris (Table 1).
Map showing the number of patients who were hospitalized and treated for rhegmatogenous retinal detachment (RRD) in the same urban area as their residence, between 2011 and 2018, in each of the 36 selected urban areas of metropolitan France (n = 21,166; total included patients). Note that data on meteorological parameters were collected from a weather station located within each corresponding urban area.
We studied the correlation coefficient between the occurrence of RRD and the mean daily temperature over the preceding 10-day period (T-1) in each urban area. We found a statistically significant relationship for 5 out of 36 urban areas. However, for each of these areas, the correlation coefficient was low: Béthune (rs = 0.1, p = 0.032), Montpellier (rs = 0.1, p = 0.038), Rouen (rs = 0.2, p = 0.005), Saint-Etienne (rs = 0.2, p = 0.006) and Toulouse (rs = 0.1, p = 0.022) (Table 2).
We analyzed the correlation coefficient between the occurrence of RRD and the mean daily temperature over the 10-day period prior to T-1 (T-2) in each urban area. We found a statistically significant relationship for the same urban areas, with the same low correlation coefficients (Table 2).
We further studied the correlation coefficient between the occurrence of RRD and the difference between mean daily temperatures during T-1 and T-2. The association was statistically significant for only 2 urban areas: Le Havre, with a low negative correlation (rs = − 0.1, p = 0.022), and Lille, with a low positive correlation (rs = 0.2, p = 0.013) (Table 3).
Lastly, we looked at the correlation coefficient between the occurrence of RRD and other meteorological parameters during T-1: 10-day mean daily minimum and maximum temperatures, the difference between the 10-day means of daily maximum and minimum temperatures, average total daily rainfall (or snowmelt), the number of days with daily rainfall ≥ 1 mm; the total duration of insolation, total overall radiation; mean wind speed averaged over a 10-min timespan and number of days, with maximum daily instantaneous wind speed ≥ 8 m/second; mean relative humidity; mean reduced pressure at sea level and minimum sea pressure. Again, very few urban areas were found to have a statistically significant relationship with these parameters, and when they did, it was with a low correlation coefficient (eTables 2–8 in the Supplement).
Discussion
In this study we investigated, for the first time, the influence of meteorological factors on the occurrence of idiopathic RRD throughout metropolitan France. We did not establish a statistically significant relationship between RRD incidence and the mean temperature over the preceding 10-day period (T-1) in most urban areas. Nor did we find any association between RRD incidence and other meteorological parameters, including mean daily temperature over the 10 days prior to T-1, rainfall, atmospheric pressure, overall radiation, duration of sunshine, relative humidity and wind speed. Nevertheless, in accordance with previous studies throughout Europe, the United States and Asia, we found a significant rise in the incidence of RRD; the number of cases increased each year between January 2011 and December 2018, particularly among men, with a mean age of RDD occurrence between 59.8 and 65.1 years24,27,29,30.
Our findings led us to question the strength and design of our study. Many patients were excluded because they did not reside in the same urban area as their treatment hospital. This was likely due to the fact that only a few centers perform RRD surgery in certain small urban areas, obliging patients to travel sometimes far from their homes. However, we felt it was essential to exclude these patients in order to ensure that the meteorological parameters analyzed were consistent with the patients' place of residence. Limiting the geographical areas of interest to 36 urban areas may have been too restrictive. Nevertheless, if we had chosen a larger area, we would have generalized the meteorological data. Conversely, if we had chosen a more limited area, we would have reduced the number of patients included.
We chose to study meteorological factors over the preceding 10-day period because data from the French weather service, Météo France, are available on a daily, 10-day, and monthly basis. We also analyzed the second and third 10-day periods prior to the event. In our study, the event was defined as the first day of hospitalization for RRD surgery. Surgery is generally performed within 1 to 2 days of diagnosis. However, in most cases, the day of diagnosis does not correspond to the day of RRD onset, let alone the onset of a retinal break. A retinal break generally arises following posterior vitreous detachment (PVD), which appears to progress gradually and insidiously over several weeks or months. It usually only becomes symptomatic when the posterior hyaloid detaches from the papilla31,32. In this light, we additionally cannot eliminate the attribution of RDD incidence to the wrong urban area for some patients; i.e. the treatment hospital was in the same area as where the patient resides, but not in the same area as RDD onset.
Immediately after the onset of PVD symptoms, the risk of retinal break is high: a meta-analysis of 10 studies with a total of 1,568 patients found a retinal break rate of 8.2 to 47.6% in acute symptomatic PVD33. Finally, the risk of break does not stop once PVD has become symptomatic: a retinal break can occur up to 6 weeks after the onset of symptoms34,35,36. Therefore, determining the exact onset date of retinal break and then RRD is challenging. This is why we chose to analyze data over a relatively broad time-frame. Furthermore, it should be noted that with our inclusion and exclusion criteria we sought to select only idiopathic RRD, and to exclude secondary RRD, which do not share the same pathophysiology, and often do not share the same timeframe between the onset of the disease and its diagnosis.
We chose the mean temperature as our primary evaluation criterion. A small number of other studies have reported a significant correlation between RRD incidence and other meteorological parameters. Rossazza et al. found an association between increased RRD and excessive insolation and reduced precipitations over the previous 3 days in Tours, France (n = 773)8. Ghisolfi et al. found a relationship between RRD occurrence and mean light flux and quarterly radiation in Pavia, Italy (n = 363)11. The group of Sevillano Torrado et al.16 reported a positive correlation between RRD and monthly and fortnightly solar radiation in Pontevedra, Spain (n = 256), with increase in solar radiation intensity found significantly associated with increase in incidence of RRD between 2008 and 2014. The authors explain their findings by the fact that the eye can better adapt to meteorological factors not related to solar radiation intensity, such as temperature and humidity. In this light, it would be interesting to design a future study, not taking into account overall solar radiation over T-1 as we did here, but investigating how changes in solar radiation and other meteorological factors could affect RRD incidence according to season and over the long term. This is not only in our entire national case series, but also in different regions of France (e.g. RRD incidence in the North versus South). Finally, Kim et al. found a relationship between RRD and mean monthly daily temperature range in Chungbuk, South Korea (n = 974)5. However, these four studies differ from ours due to their monocentric nature and the comparatively small number of patients analyzed.
Several pathophysiological and behavioral factors may contribute to the seasonal variation in RRD incidence5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20. Greater light exposure and higher temperatures during summer may promote both vitreous and retinal damage. Ultraviolet light, which is abundant in summer, heats the vitreous and the retina, and heat-induced posterior vitreous detachment is thought to promote RRD pathogenesis20. Accordingly, in vitro models using animal tissues have shown that exposure to strong light can alter vitreous collagen37 and destabilize the retinal rod matrix38, whilst low temperatures may delay retinal deterioration39. In addition, Hida et al.40 and Mansour et al.14 proposed a link between RRD and the ocular surface: eye dryness increases in summer and thereby increases ocular friction, inducing vitreoretinal movements. Notably, the frequency of eye rubbing secondary to allergies also increases in the spring/summer and this may further contribute to an increased risk of retinal detachment14,40. Lastly, as outdoor physical activity is greater in the spring/summer, increased physical activity could potentially play a role in the summer peak in RRD. In line with this, outdoor activities and thus sport were limited to a strict minimum in France during the COVID-19 pandemic, between the 17th of March and the 11th of May 2020. One study found a 41.6% decrease in the number of RRD surgeries at this time compared to the same period in 2019. In the 4 months following lockdown, no increase in surgeries related to deferred procedures was observed, but a return to normal RRD patient levels was noted41. Cases of RRD were therefore less frequent when the population was less physically active. Studies in other countries also noted a reduction in the number of retinal detachment surgeries during global lockdown42,43,44. One hypothesis that could explain this phenomenon is that physical activity increases vitreous movements and therefore vitreoretinal traction, a known risk factor for RRD.
In conclusion, although our study confirms the rising incidence of RRD in France, it provides no evidence for an association between meteorological factors and idiopathic RRD occurrence. Further studies are required to better understand if changes in meteorological factors, according to season and over the long term, cause changes in RRD incidence throughout France or in specific regions of France.
Methods
Study design and population
We conducted a national, retrospective, case-series study entitled METEO-POC (Influence des paramètres METEOrologiques et survenue de Pathologies de l’Œil au Cerveau); that is the influence of meteorological parameters on the occurrence of pathologies affecting the eye-brain region. Patient data were extracted from the French National Health Data System (Système National des Données de Santé—SNDS)45 between January 2011 and December 2018. Permission to access patient data from the SNDS, without informed patient consent given the retrospective and non-interventional nature of the study, was granted by: (1) the IRB “Comité d’Expertise pour les Recherches, les Etudes et les Evaluations dans le domaine de la Santé” (CEREES, Expert Committee for Research, Studies and Evaluations in the Healthcare Field, project number 1595168) on June 9th 2020, and (2) the Commission nationale de l’informatique et des libertés (CNIL, National Commission on Informatics and Liberty, authorization request number 920251, approval number DR-2020-286) on August 6th 202046. All research was performed in accordance with the principles and regulations of the Helsinki Declaration of 1964 and its later amendments. All data have been anonymized for publication.
The French National Health Insurance Fund (Caisse Nationale d’Assurance Maladie—CNAM) carried out an initial selection of the study population according to the following inclusion and exclusion criteria. The event of interest was defined as the first day of hospitalization for the treatment of RRD. The inclusion criteria were as follows:
-
all patients were adults;
-
patients with a hospital admission diagnosis (main, related or associated) of RRD between January 2011 and December 2018;
-
patients having surgery for RRD in a French public or private health center between January 2011 and December 2018.
Exclusion criteria:
-
patients whose residential postcode belonged to a different region from that of their treatment center;
-
patients with a history of vitreoretinal surgery within the previous 2 years;
-
patients with a hospital admission diagnosis (main, related or associated) within the previous 2 years for: retinal detachment with retinal tear, exudative or tractional retinal detachment, aphakia, Marfan syndrome, abnormalities in the metabolism of sulfur-containing amino acids, a history of eye or orbit trauma, intraocular foreign body, traumatic cataract, lens dislocation, hyphema, a history of endophthalmitis, a history of inflammatory damage to the orbit, a history of chorioretinitis or proliferative retinopathy;
-
patients with a history of eye trauma within the past 2 years;
-
patients with a history of cataract surgery or laser capsulotomy within the past 6 months.
In order to verify the quality of data collected by the SNDS, we first studied the SNDS selection of patients who underwent RRD surgery at Toulouse University Hospital between January 2017 and December 2017 and compared it with those selected by our reference Softalmo computer software (Corilus Ophtalmo, Paris, France)46. We found that the eligibility criteria performed well47,48 with a positive predictive value of 82.0%, a sensitivity of 83.8%, a specificity of 69.9%, and a negative predictive value of 72.5%46.
Linking patients and health centers to urban areas of interest
We linked patients and health centers to their urban areas of residence (according to the National Institute of Statistics and Economic Studies’ (INSEE) list of communes for 2020) using their geographical post codes. We limited our study to patients residing in one of the three most populated urban areas of each region of metropolitan France according to the INSEE 2010 zoning and INSEE 2016 classification49, with the exception of the Ile de France area (where Paris represents the only urban area), and Corsica (where only the 2 largest urban areas were studied due to the lack of population density in the other urban areas); that is 36 urban areas in total. The geographical scale of the urban area was chosen because it includes the outer suburbs. We also chose to restrict our study to patients residing in the same urban area as their treatment center.
Retrieving the meteorological data
Data on meteorological parameters were collected using the French meteorological service Météo France database50. Urban areas were linked to their corresponding geographical weather stations (refer to Table 1 and Fig. 2 for the station locations). Where there was only one weather station in the urban area, it was taken into account; where there were several, the station with the most available meteorological data was chosen. The meteorological parameters were selected per 10-day period, which in this study corresponds to one third of a month: the first two 10-day periods systematically consisting of 10 days, the third consisting of 8 to 11 days. We did not calculate a correlation coefficient when no meteorological data were available for a ten-day period.
Statistical analyses
Statistical analyzes were carried out by a biostatistical engineer from the Clinical Investigation Centre (CIC), authorized to consult SNDS data extractions on the portal, using SAS Enterprise Guide® software, version 7.1 (Copyright © 2006–2010, SAS Institute Inc, Cary, NC, USA). Spearman Rank Correlation Coefficients (rs) were calculated for the analysis of the evaluation criteria. A significance level of 5% (p-value < 0.05) was implemented. Categorical variables were analyzed and presented as frequencies and percentages. Continuous variables were presented in the form of mean, standard deviation, median, and minimum and maximum values. Patients’ characteristics were taken into account at the date of the first event.
For calculation of correlation coefficients between RRD occurrence and T-1, each month was divided into 10-day periods.
-
If an RRD patient received surgery during the first 10 days of the month (1st to 10th), the correlation was calculated based on the mean* temperature over the last 10 days of the preceding month (21st to 28th, 29th, 30th or 31st depending on the month and year).
-
If the patient received surgery during the second 10 days of the month (11th to 20th), the correlation was calculated based on the mean* temperature over the first 10 days of the same month (1st to 10th).
-
If the patient received surgery during the last 10 days of the month (21st to 28th, 29th, 30th or 31st depending on the month and year), the correlation was calculated based on the mean* temperature over the second 10 days of the same month (11th to 20th). *Note that mean temperature was calculated as the 10-day average of daily mean temperatures.
Data availability
The datasets generated and analyzed in this study are available from the corresponding author on reasonable request.
References
Kirchhof, B., Oh, K. T., Hartnett, M. E. & Landers, M. B. Pathogenetic mechanisms of retinal detachment. In Retina Enhanced Online Features and Print 2564 (Saunders, 2013).
Kuhn, F. & Aylward, B. Rhegmatogenous retinal detachment: A reappraisal of its pathophysiology and treatment. Ophthalmic Res. 51(1), 15–31 (2014).
Warren, A., Wang, D. W. & Lim, J. I. Rhegmatogenous retinal detachment surgery: A review. Clin. Exp. Ophthalmol. 51(3), 271–279 (2023).
Sothivannan, A. et al. Impact of the time to surgery on visual outcomes for rhegmatogenous retinal detachment repair: A meta-analysis. Am. J. Ophthalmol. 244, 19–29 (2022).
Kim, D. Y. et al. The association between the frequency of rhegmatogenous retinal detachment and atmospheric temperature. J. Ophthalmol. 2020, 2103743 (2020).
Weekers, R. Seasonal variations in the frequency of essential retinal detachment. Ophthalmologica 110, 218–2. https://doi.org/10.1159/000300276 (1945).
Weekers, R. Seasonal variations in retinal detachment frequency. Arch. Ophtalmol. Rev. Gen. Ophtalmol. 9(1), 64 (1949).
Rossazza, C., Banchereau, A. & Jezegabel, C. The effect of atmospheric disturbances in the precipitation of idiopathic retinal detachment. Bull. Soc. Ophtalmol. Fr. 81(6–7), 705–8 (1981).
Paavola, M., Chehova, S. & Forsius, H. seasonal variations in retinal detachment in northern Finland and Novosibirsk. Acta Ophthalmol. 61(5), 806–12. https://doi.org/10.1111/j.1755-3768.1983.tb01461.x (2009).
Laatikainen, L., Tolppanen, E. M. & Harju, H. Epidemiology of rhegmatogenous retinal detachment in a Finnish population. Acta Ophthalmol. 63(1), 59–64. https://doi.org/10.1111/j.1755-3768.1985.tb05216.x (1985).
Ghisolfi, A., Vandelli, G. & Marcoli, F. Seasonal variations in rhegmatogenous retinal detachment as related to meteorological factors. Ophthalmologica 192(2), 97–102 (1986).
Qassim, A., Viki, M., Ng, S. K., Jersmann, H. & Casson, R. J. Climate and season: The effects on ophthalmic diseases: Effects of climate and season on ophthalmic diseases. Clin. Exp. Ophthalmol. 45(4), 385–92. https://doi.org/10.1111/ceo.12883 (2017).
Jonkers, G. H. Seasonal variations in the occurrence of retinal detachments. Ophthalmologica 115(5), 308–318 (1948).
Mansour, A. M. et al. Seasonal variation of retinal detachment in Lebanon. Ophthalmic Res. 41(3), 170–4 (2009).
Bertelmann, T., Cronauer, M., Stoffelns, B. & Sekundo, W. Seasonal variation in the occurrence of rhegmatogenous retinal detachment at the beginning of the 21st century Study results and literature review. Ophthalmologe 108(12), 1155–63 (2011).
Sevillano Torrado, C., Viso, E., Moreira, S., Blanco, M. J. & Gude, F. Rhegmatogenous retinal detachment and solar radiation in Northwestern Spain. Ophthalmologica 243(1), 51–57 (2020).
Prabhu, P. B. & Raju, K. V. Seasonal variation in the occurrence of rhegmatogenous retinal detachment. Asia Pac. J. Ophthalmol. (Phila). 5(2), 122–126 (2016).
Jonkers, G. H. Seasonal variation in retinal detachment. Ned Tijdschr Geneeskd. 96(20), 1241–3 (1952).
Thelen, U., Gerding, H. & Clemens, S. Rhegmatogenous retinal detachments Seasonal variation and incidence. Ophthalmologe. 94(9), 638–41 (1997).
Lin, H. C. et al. Seasonality of retinal detachment incidence and its associations with climate: An 11-year nationwide population-based study. Chronobiol. Int. 28(10), 942–948 (2011).
Ivanisević, M., Erceg, M. & Eterović, D. Rhegmatogenous retinal detachment and seasonal variations. Acta Med. Croatica 56(2), 49–51 (2002).
Li, X., Beijing Rhegmatogenous Retinal Detachment Study Group. Incidence and epidemiological characteristics of rhegmatogenous retinal detachment in Beijing. China. Ophthalmology. 110(12), 2413–7 (2003).
Erdöl, H., Uzlu, D. & Kola, M. Characteristics and Seasonal Variations of Rhegmatogenous Retinal Detachment in the Eastern Black Sea Region of Turkey: 8-Year Results. Turk. J. Ophthalmol. 50(2), 94–8 (2020).
Iida, M. et al. Association of meteorological factors with the frequency of primary rhegmatogenous retinal detachment in Japan. Sci. Rep. 11, 8879 (2021).
Shaheen, A. R. et al. Nationwide demographic disparities in united states emergency department visits in patients with rhegmatogenous retinal detachment. Retina 43(11), 1936–44 (2023).
Al Samarrai, A. R. Seasonal variations of retinal detachment among Arabs in Kuwait. Ophthalmic Res. 22(4), 220–223 (1990).
Ben Ghezala, I. et al. Incidence of rhegmatogenous retinal detachment in France from 2010 to 2016: Seasonal and geographical variations. Br. J. Ophthalmol. 106(8), 1093–1097 (2022).
Biausque, V., Thévenot, C. & Wolff, L. En 2010, les salariés ont pris en moyenne six semaines de congé - Insee Première - 1422. https://www.insee.fr/fr/statistiques/1281344.
van Leeuwen, R. et al. Association of rhegmatogenous retinal detachment incidence with myopia prevalence in the Netherlands. JAMA Ophthalmol. 139(1), 85–92 (2021).
Saraf, S. S. et al. Demographics and seasonality of retinal detachment, retinal breaks, and posterior vitreous detachment from the intelligent research in sight registry. Ophthalmol. Sci. 2(2), 100145 (2022).
Johnson, M. W. Posterior vitreous detachment: Evolution and complications of its early stages. Am. J. Ophthalmol. 149(3), 371-382.e1 (2010).
Ramovecchi, P., Salati, C. & Zeppieri, M. Spontaneous posterior vitreous detachment: A glance at the current literature. World J. Exp. Med. 11(3), 30–6 (2021).
Coffee, R. E., Westfall, A. C., Davis, G. H., Mieler, W. F. & Holz, E. R. Symptomatic posterior vitreous detachment and the incidence of delayed retinal breaks: Case series and meta-analysis. Am. J. Ophthalmol. 144(3), 409–413 (2007).
van Overdam, K. A., Bettink-Remeijer, M. W., Mulder, P. G. & van Meurs, J. C. Symptoms predictive for the later development of retinal breaks. Arch. Ophthalmol. 119(10), 1483–1486 (2001).
van Overdam, K. A. et al. Symptoms and findings predictive for the development of new retinal breaks. Arch Ophthalmol. 123(4), 479–484 (2005).
Richardson, P. S., Benson, M. T. & Kirkby, G. R. The posterior vitreous detachment clinic: Do new retinal breaks develop in the six weeks following an isolated symptomatic posterior vitreous detachment?. Eye 13, 237–40 (1999).
Akiba, J., Ueno, N. & Chakrabarti, B. Mechanisms of photo-induced vitreous liquefaction. Curr. Eye Res. 13(7), 505–512 (1994).
Uehara, F., Yasumura, D. & LaVail, M. M. Rod- and cone-associated interphotoreceptor matrix in the rat retina. Differences in light-evoked distributional changes. Invest. Ophthalmol. Vis Sci. 32(2), 285–92 (1991).
Endo, E. G., Yao, X. Y. & Marmor, M. F. Pigment adherence as a measure of retinal adhesion: Dependence on temperature. Invest. Ophthalmol. Vis. Sci. 29(9), 1390–1396 (1988).
Hida, T., Tano, Y., Okinami, S., Ogino, N. & Inoue, M. Multicenter retrospective study of retinal detachment associated with atopic dermatitis. Jpn. J. Ophthalmol. 44(4), 407–418 (2000).
Baudin, F. et al. Impact of COVID-19 lockdown on surgical procedures for retinal detachment in France: A national database study. Br. J. Ophthalmol. 107(4), 565–569 (2023).
Rohl, A., Kalhorn, A., Singh, J. & Mandava, N. Decreased retinal detachments during a COVID-19 lockdown period in Colorado. Acta Ophthalmol. 99(4), e618–e619 (2021).
Poyser, A. et al. Impact of COVID-19 pandemic and lockdown on retinal detachments. Eye (Lond) 35(8), 2322–3 (2021).
Pellegrini, M. et al. The impact of COVID-19 pandemic on ophthalmological emergency department visits. Acta Ophthalmol. 98(8), e1058–e1059 (2020).
SNDS. http://snds.gouv.fr.
Barioulet, L. et al. Validation des critères d’identification des patients opérés d’un décollement de rétine rhegmatogène au CHU de Toulouse. J. Français Ophtalmol. 46(5), 518–26 (2023).
Barrett, B. J. & Fardy, J. M. Evaluation of diagnostic tests. Methods Mol. Biol. 2249, 319–333 (2021).
Eusebi, P. Diagnostic accuracy measures. Cerebrovasc. Dis. 36(4), 267–272 (2013).
INSEE. https://www.insee.fr.
Publithèque Météo France. https://publitheque.meteo.fr.
Acknowledgements
We are grateful to Dr Lena Brydon and Dr Jacqueline Butterworth for manuscript writing support.
Funding
This study received funding from the Club Francophone des Spécialistes de la Rétine (2018) and from the Toulouse University Hospital Appel à projets Recherche et Innovation scheme (2018).
Author information
Authors and Affiliations
Contributions
Vanessa Sentis, Ségolène Mrozek, Déborah Méligne, Guillaume Moulis, Agnès Sommet, and Vincent Soler contributed to study conception and design. Data collection was performed by Lisa Barioulet, Manuela Rueter, Vanessa Sentis, Pierre Fournié, Ségolène Mrozek, and Déborah Méligne. Data analysis and interpretation was performed by Lisa Barioulet, Agnès Sommet, Manuela Rueter, and Vincent Soler. Lisa Barioulet wrote the first draft of the manuscript and all authors contributed to later drafts. All authors have approved the final manuscript version and agree to be accountable for all aspects of this work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Barioulet, L., Rueter, M., Sentis, V. et al. Meteorological factors and rhegmatogenous retinal detachment in metropolitan France. Sci Rep 14, 18857 (2024). https://doi.org/10.1038/s41598-024-69591-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-69591-1
- Springer Nature Limited