Abstract
Despite the clear association between remnant cholesterol (RC)and diabetes risk, no study to date has examined the relationship between RC and reversal of prediabetes to normoglycemia. This retrospective cohort study included a total of 15,023 patients with prediabetes who underwent a physical examination between 2010 and 2016. The link between initial RC levels and the reversion from prediabetes to normoglycemia was analyzed using the Cox proportional-hazards regression model. Additionally, the study explored the possible relationship between RC and the probability of returning normoglycemia by applying Cox proportional hazards regression models with cubic spline functions. To address competing risks, a multivariate Cox regression analysis was undertaken, treating the onset of diabetes as a competing risk event for reversing prediabetes to normoglycemia. Additionally, the study incorporated extensive subgroup analyses alongside multiple sensitivity analyses, enhancing the reliability and robustness of the results. After adjusting for covariates, the findings indicated that RC was inversely associated with the likelihood of reverting to normoglycemia (per 5 mg/dL increase, HR = 0.918, 95% CI 0.909–0.927). The analysis also revealed a nonlinear relationship between RC and normoglycemia reversion, with an inflection point at 51.08 mg/dL. For RC values below this inflection point (RC < 50.08 mg/dL), the HR for the probability of returning to normoglycemia was 0.907 (95% CI 0.897–0.917 per 5 mg/dL). Additionally, the competing risks model demonstrated a negative relationship between RC and the reversal of prediabetes to normoglycemia (SHR = 0.92, 95% CI 0.91–0.93). Sensitivity analyses confirmed the robustness and stability of these results. This study demonstrated a negative and non-linear association between RC and the probability of reversion to normoglycemia in Chinese adults with prediabetes. By actively intervening to reduce RC levels, at least to below 51.08 mg/dL, further reduction of RC may significantly increase the probability of returning to normoglycemia from prediabetes.
Similar content being viewed by others
Introduction
Prediabetes (Pre-DM) represents the transitional phase preceding the onset of diabetes. This stage includes impaired fasting glucose (IFG), impaired glucose tolerance (IGT), and a combination of both (IFG + IGT), situating it as an intermediate hyperglycemic condition between normoglycemia and diabetes mellitus (DM)1,2,3. The International Diabetes Federation (IDF) reports that the global prevalence of Pre-DM has been escalating swiftly, with approximately 536.6 million adults diagnosed in 2021. Furthermore, projections suggest that the number of adults with Pre-DM will soar to 783.2 million by 2045, constituting roughly 12.2% of the adult population4. Pre-DM increases an individual's absolute risk of diabetes by 3 to 10 times5. Epidemiologic studies have shown that the risk of complications such as microvascular disease (microalbuminuria, neuropathy, and retinopathy) and cardiovascular disease (peripheral vascular disease, stroke, and heart disease) begins in the early stages of the transition from normal glucose tolerance to Pre-DM6,7,8,9. Therefore, early diagnosis and treatment of Pre-DM will reduce or slow the progression of diabetes and its complications. Some individuals with Pre-DM may persist in the prediabetic phase without progressing to full-blown diabetes, and a substantial number (ranging from 20 to 50%) can even revert to normoglycemia10,11,12. Previous research has compellingly shown that achieving even a temporary return to normal blood glucose levels significantly diminishes the risk of developing diabetes and related complications in those with Pre-DM13,14,15. Therefore, the primary goal of screening and treatment of Pre-DM is to prevent or delay progression to DM by reversing blood glucose to normal with appropriate interventions.
It is crucial to study the rate at which individuals with Pre-DM return to normoglycemia and to identify the factors that facilitate this reversal. Such research is essential for informing public health strategies aimed at preventing the transition from Pre-DM to DM and improving the long-term health prospects of those at high risk. Unfortunately, the primary focus in clinical settings has been on the progression of the disease, with few studies investigating the rate of normoglycemic reversion and its contributing factors in patients with Pre-DM13,14. Early findings from epidemiological research indicate that several factors, including age, initial fasting glucose levels, body mass index (BMI), insulin secretion, β-cell function, and fasting triglyceride (TG) levels, might be associated with the reversion to normoglycemia in these patients16,17,18.
Previous research has established a significant connection between dyslipidemia and dysglycemia19,20,21. Recently, a growing interest has emerged in a lipid marker known as remnant cholesterol (RC), which is believed to be linked to an elevated risk of cardiovascular disease and overall mortality22,23. RC is the cholesterol found in triglyceride-rich lipoproteins (TRLs), which mainly include chylomicron remnants (CR), intermediate-density lipoprotein (IDL), and very low-density lipoprotein (VLDL)24. Earlier research has established a notable link between remnant cholesterol (RC) and the development of diabetes mellitus (DM). Elevated RC levels have been shown to not only increase the risk of microvascular complications but also potentially play a role in the occurrence of macrovascular complications in those with DM25,26,27,28. Nevertheless, the association between RC and the reversion of Pre-DM to normoglycemia has not been previously investigated. Consequently, this cohort study aims to examine the link between RC and the likelihood of reverting from Pre-DM to normoglycemia, utilizing existing data.
Methods
Study design and data sources
This post hoc analysis stems from a cohort study performed by the Rich Healthcare Group in China29. The raw data utilized in this analysis were generously provided by Chen et al. and are accessible on DATADRYAD (http://www.datadryad.org). For comprehensive details, readers should refer to the published study titled "Association of body mass index and age with the onset of diabetes in Chinese adults: a population-based cohort study" (https://doi.org/10.5061/dryad.ft8750v)29. This article is freely available under the Creative Commons Attribution Non-Commercial (CC BY-NC 4.0) license, which allows for sharing, reprinting, adaptation, and the creation of derivative works for non-commercial purposes29.
Study population
As reported by the primary investigator, the data utilized in this study were sourced from an extensive digital database established by the Rich Healthcare Group in China. This extensive dataset comprises medical records of individuals who participated in health screenings from 2010 to 2016, encompassing 32 regions and 11 cities throughout China29. The original study received approval from the Rich Healthcare Group Review Board. Given the retrospective design of the research, the necessity for informed consent was waived by the institutional ethics committee29. Therefore, no further ethical approval was necessary for this secondary analysis.In addition, the original study adhered to the Declaration of Helsinki, ensuring all procedures met relevant guidelines and regulations, as noted in the declarations section29,30. The same standards were observed in this secondary analysis.
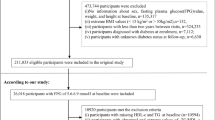
In the original study, a total of 685,277 individuals aged 20 years and older, who had undergone at least two health screenings, were initially included. However, 473,444 of these individuals were excluded based on specific criteria. The exclusion criteria applied in the study were as follows: (I) individuals without follow-up information 2 years after the initial examination, due to the chronic nature of changes in glucose metabolism; (II) participants lacking baseline information crucial for assessing glucose metabolism, such as height, gender, age, fasting plasma glucose (FPG) levels, and weight; (III) individuals diagnosed with diabetes at the baseline; (IV) participants with abnormal body mass index (BMI) values, either exceptionally low (under 15 kg/m2) or excessively high (over 55 kg/m2) and (V) individuals for whom diabetes status remained undetermined during the follow-up period. After applying these criteria, the final analysis conducted by the Rich Healthcare Group included 211,833 individuals29.
In the present investigation, participants with baseline FPG levels below 5.6 mmol/L or above 6.9 mmol/L were initially excluded, based on the American Diabetes Association’s 2021 guideline criteria for Pre-DM, resulting in the inclusion of 26,018 individuals with Pre-DM. Then, those with missing baseline data for total cholesterol (TC), high-density lipoprotein cholesterol (HDL-c), and low-density lipoprotein cholesterol (LDL-c) were also excluded (n = 10,620). Additionally, participants with extreme RC values, defined as three standard deviations above or below the mean, were removed from the dataset (n = 375). Ultimately, the study comprised a total of 15,023 participants. The screening procedure used to select study participants is illustrated in Fig. 1.
Variables
Independent variable
RC is a continuous variable in milligrams per deciliter. RC = TC − HDL-c–LDL-c (mg/dL) is the detailed formula for calculating RC31,32.
Outcome variable
The primary outcome of interest in this study is the reversion to normoglycemia. Reversion from Pre-DM to normoglycemia is defined as participants not being diagnosed with diabetes at the follow-up assessment and having an FPG level of less than 5.6 mmol/L during the follow-up period3,13.
Covariates included in this secondary analysis
The choice of covariates for this study was guided by the original study, along with prior studies on Pre-DM or DM, and clinical insights21,29,33,34,35. The categorical variables considered included smoking status, sex, family history of diabetes, and alcohol consumption status. Conversely, the continuous variables encompassed age, TG, BMI, serum creatinine (Scr), alanine aminotransferase (ALT), diastolic blood pressure (DBP), height, HDL-c, weight, aspartate aminotransferase (AST), blood urea nitrogen (BUN), TC, systolic blood pressure (SBP), and LDL-c.
Data collection
Data collection procedures were grounded in the original research conducted by the Rich Healthcare Group. Trained healthcare practitioners utilized a standardized questionnaire to gather baseline data from participants, encompassing metrics such as weight, sex, smoking and drinking habits, height, family medical history, age., alongside other physical examination indicators. Blood pressure readings were obtained with a mercury sphygmomanometer. Fasting venous blood samples were collected following a minimum of 10 h of fasting during each visit. TC, HDL-c, TG, and LDL-c were measured with an autoanalyzer (Beckman 5800). FPG was assessed using the glucose oxidase method, also on an autoanalyzer (Beckman 5800)29.
Treatment of missing data
In this secondary analysis, there were missing data on several variables: 5 (0.03%) for SBP, 34 (0.23%) for ALT, 5 (0.03%) for DBP, 113 (0.75%) for Scr, 354 (2.36%) for BUN, 10,406 (69.27%) for drinking status, 8064 (53.68%) for AST, and 10,406 (69.27%) for smoking status. To reduce discrepancies caused by missing data and to streamline the analysis, single imputation was applied36. The imputation model included TC, drinking status, sex, HDL-c, DBP, age, BUN, Scr, SBP, ALT, smoking status, LDL-c, AST, and family history of diabetes, utilizing linear regression with 10 iterations. The analysis assumed the data were missing at random (MAR)36,37. It should be noted that version 3.4.3 of the R language software (mice package) was used to conduct a single imputation, and subsequent statistical analyses were based on this single imputed dataset.
Statistical analysis
Participants were grouped into quartiles based on their RC levels. Variables were compared across different RC quartile groups. For continuous variables following a normal distribution, means and standard deviations were reported. For skewed continuous variables, medians and interquartile ranges were used. Categorical variables were expressed as frequencies and percentages. The Kruskal–Wallis H test was employed to evaluate statistical significance for skewed distributions, one-way ANOVA was used for normally distributed variables, and the χ2 test was applied for categorical data.
The Cox proportional hazards regression model was employed to investigate the relationship between RC and reversion to normoglycemia in patients with Pre-DM. The models with three different adjustment strategies are as follows: (i) Model I: No adjustments were made for covariates. (ii) Model II: Adjustments were made for three covariates: BMI, sex, and age. (iii) Model III: Comprehensive adjustments were made for the following covariates: BMI, sex, drinking status, age, ALT, TG, AST, DBP, smoking status, Scr, family history of DM, AST, and SBP. TC was omitted from the multivariate Cox proportional hazards regression models due to its collinearity with other covariates (Supplementary Table S1). Additionally, the emergence of DM during the follow-up period could obscure the reversal from Pre-DM to normoglycemia or affect the likelihood of this occurrence38. Thus, to validate the association between RC and the reversion of Pre-DM to normoglycemia, a competing risks multivariate Cox proportional hazards regression was performed, following the methodology of Fine and Gray38,39. This method considers the progression from Pre-DM to DM as a competing event against reversion to normoglycemia.
To further examine potential non-linear associations between RC and the likelihood of returning to normoglycemia among pre-diabetic participants, a Cox proportional hazards regression model integrated with a cubic spline function was utilized. Upon detecting non-linearity, a recursive algorithm identified the inflection point. Subsequent multivariate Cox proportional hazards regression analyses were then executed for populations on either side of the inflection point—specifically, those with values < inflection point and those with values ≥ inflection point. This analysis yielded distinct hazard ratio values for each subgroup. Ultimately, the most effective model elucidating the connection between RC and the reversion from pre-diabetes to normoglycemia was chosen using the log-likelihood ratio test.
Previous studies have demonstrated a strong link between glucose metabolism and factors such as obesity, a family history of DM, and hypertriglyceridemia40,41,42,43. To corroborate these findings, multiple sensitivity analyses were conducted. Initially, the analysis focused on participants with a BMI below 24 kg/m2 (n = 6115). Additionally, individuals with a family history of DM were excluded from the sensitivity analyses (n = 14,630). The association between RC and the restoration of normoglycemia from Pre-DM was also examined in those with TG levels less than 1.7 mmol/L (n = 9148). Furthermore, continuous covariates were incorporated into the equations using generalized additive modeling (GAM). Finally, to evaluate the potential influence of unmeasured confounders on the relationship between RC and the reversion of Pre-DM to normoglycemia, the E-value was computed44.
Subgroup analyses were conducted utilizing stratified Cox proportional hazards regression models based on drinking status, sex, smoking status, and age. To achieve this, continuous variables such as SBP and DBP were categorized according to clinical thresholds (age: < 30, 30–40, 40–50, 50–60, 60–70, ≥ 70 years; DBP: < 90, ≥ 90 mmHg; SBP: < 140, ≥ 140 mmHg). Along with the stratification factors, adjustments were made for sex, drinking status,BMI, AST, DBP, ALT, Scr, age, TG, AST, family history of DM, smoking status, and SBP. To determine the presence of interaction terms, likelihood ratio tests were employed in models both with and without these interaction terms.
All findings were documented in accordance with the STROBE statement45. Statistical analyses were carried out using R software version 3.4.3 and Empower(R) software version 4.0. A two-sided P value of less than 0.05 was considered to indicate statistical significance.
Ethics approval and consent to participate
This study was approved by the Rich Healthcare Group Review Board and conducted in strict compliance with the ethical principles set forth in the Declaration of Helsinki. Given the retrospective nature of the research, the institutional ethics committee (The Rich Healthcare Group Review Board) waived the requirement for informed consent and approval.
Results
Characteristics of patients with prediabetes
A total of 15,023 participants were included in the analysis, comprising 9718 men and 5305 women, with an average age of 50.96 (± 13.48) years. The RC exhibited a normal distribution, with values ranging from 0.39 to 89.40 mg/dL and a mean of 29.25 mg/dL (Fig. 2). Table 1 displayed the anthropometric and biochemical characteristics of the participants, categorized by RC quartiles. The findings indicated a significant progressive increase in various parameters—including LDL-c, AST, age, height, BUN, TG, DBP, ALT, TC, BMI, weight, SBP, and Scr—across higher RC quartiles. Conversely, HDL-c demonstrated a decreasing trend. Additionally, the proportion of males and alcohol drinkers increased steadily with higher RC values, while the proportion of females showed a gradual decline.
Participants were divided into two groups according to their reversion to normoglycemia during the follow-up period. As depicted in Fig. 3, individuals with Pre-DM who reverted to normoglycemia exhibited lower RC levels compared to those who did not achieve normoglycemia.
Reversal rate from Pre-DM to normoglycemia, progression rate from Pre-DM to DM, and the Pre-DM stay rate
Over an average follow-up period of 2.95 (± 0.92) years, 6235 individuals with Pre-DM reverted to normoglycemia. The overall rate of reversion was 140.63 per 1000 person-years. Within the RC quartiles, reversion rates were as follows: Q1: 180.62 per 1000 person-years; Q2: 159.10 per 1000 person-years; Q3: 130.05 per 1000 person-years; and Q4: 107.03 per 1000 person-years. The overall cumulative reversal rate from Pre-DM to normoglycemia stood at 41.50%. For the specific RC quartiles, the cumulative reversal rates were Q1: 49.58%, Q2: 42.71%, Q3: 39.21%, and Q4: 34.58%. Higher RC values were associated with significantly lower reversal rates compared to lower RC values (Table 2).
Additionally, as indicated in Supplementary Table S2, we have documented the persistence rate of prediabetic status among participants, as well as the rate at which Pre-DM advanced to DM. The overall progression rate from Pre-DM to DM was found to be 11.72%. The progression rates for each RC quartile were Q1: 8.28%; Q2: 9.99%; Q3: 12.75%; and Q4: 15.81%. It was observed that participants with higher RC values experienced significantly higher progression rates compared to those with lower RC values. Furthermore, the overall rate of maintaining prediabetic status was 46.78%, with the maintenance rates within each RC quartile delineated as 42.13% for Q1, 47.30% for Q2, 48.03% for Q3, and 49.60% for Q4. It was noted that participants with higher RC values had significantly greater rates of maintaining their prediabetic state than those with lower RC values.
RC, remnant cholesterol; CI: confidence interval.
Univariate Cox proportional hazards regression was conducted to analyze the factors influencing the reversion from prediabetes to normoglycemia
Univariate analysis indicated that reversion to normoglycemia was significantly and negatively associated with DBP, LDL-c, AST, BUN, age, ALT, TG, SBP, BMI,TC, and family history of DM. In contrast, it was positively associated with HDL-c (Supplemental Table S3).
Figure 4 displayed Kaplan–Meier curves depicting the probability of transitioning from Pre-DM to normoglycemia stratified by RC quartiles. The log-rank test (P < 0.001) indicated a significant difference in reversion probabilities across varying RC groups. The probability of returning to normoglycemia decreases as the RC increases, so patients with Pre-DM at the highest RC have the lowest probability of returning to normoglycemia.
The relationship between RC and reversion to normoglycemia in patients with Pre-DM
To investigate the relationship between RC and the likelihood of reverting from Pre-DM to normoglycemia, three Cox proportional-hazards regression models were constructed. Model I indicated that a 5 mg/dL increase in RC was significantly associated with a 9.5% reduction in the chance of reversion to normoglycemia (HR = 0.905, 95% CI 0.897–0.912). Model II, which adjusted for demographic factors and BMI, indicated that each 5 mg/dL rise in RC still significantly decreased the likelihood of returning to normoglycemia by 7.3% (HR = 0.927, 95% CI 0.919–0.935). Model III, which included adjustments for a range of potential confounders, further reinforced the association between RC (per 5 mg/dL increment) and the likelihood of reversing from Pre-DM to normoglycemia, with an HR of 0.918 (95% CI 0.909–0.927; p < 0.001) (Table 3).
Furthermore, RC was converted from a continuous variable into a categorical one and then incorporated back into the Cox proportional-hazards regression model. In the multivariable-adjusted model, taking the first quartile (Q1) of RC as the reference point, the HRs for reversion to normoglycemia were 0.804 (95% CI 0.751–0.860) for the second quartile (Q2), 0.654 (95% CI 0.609–0.703) for the third quartile (Q3), and 0.498 (95% CI 0.459–0.540) for the fourth quartile (Q4). This demonstrated that the probability of a participant reverting to normoglycemia from Pre-DM was 19.6% lower in Q2, 35.6% lower in Q3, and 50.2% lower in Q4 compared to Q1 (Table 3—Model III).
Sensitivity analysis
A series of sensitivity analyses were conducted to verify the robustness of our findings. To begin with, the Generalized Additive Model (GAM) was employed to include continuous covariates as curves in the equation. As indicated in Table 3 (Model IV), the findings were generally consistent with those of the fully adjusted model. The HR for the relationship between RC (per 5 mg/dL) and the likelihood of reverting to normoglycemia was estimated to be 0.915 (95% CI 0.906–0.924).
A sensitivity analysis was performed on a subset of participants with a BMI under 24 kg/m2, involving 6115 individuals. After adjusting for confounding factors, the results revealed a negative correlation between RC (per 5 mg/dL) and the probability of transitioning from prediabetes to normoglycemia (HR = 0.900, 95% CI 0.886–0.913). Additionally, when excluding participants with a family history of DM and adjusting for other variables, the negative association between RC and normoglycemia reversion remained significant (HR = 0.919, 95% CI 0.910–0.928). Moreover, focusing the analysis on individuals with TG levels below 1.7 mmol/L, the Cox proportional hazards regression indicated an HR of 0.895 (95% CI 0.883–0.907) for the relationship between RC and the likelihood of returning to normoglycemia (Table 4).
Additionally, we discovered that the E-value (1.4) exceeded the relative risk associated with RC and potential unmeasured confounders (1.1). This implies that unknown or unmeasured confounders are unlikely to significantly impact the relationship between RC and the reversion of Pre-DM to normoglycemia. Considering all sensitivity analyses, our results appear to be robust and reliable.
Results of multivariate Cox proportional-hazards reversion for competing risks
The results of the competing risk analysis, which considered the progression from Pre-DM to DM as a competing event for the reversal to normoglycemia, are presented in Table 5. In Model I, RC was found to be negatively correlated with the probability of returning to normoglycemia (SHR = 0.90, 95% CI 0.90–0.91). In Model II, after adjusting for sex, age, and BMI, the SHR was 0.93 (95% CI 0.92–0.93). In the fully adjusted Model III, which accounted for confounders such as sex, TG, age, drinking status, AST, BMI, smoking status, ALT, DBP, family history of diabetes, Scr, and SBP, RC remained negatively associated with reversion to normoglycemia (SHR = 0.92, 95% CI 0.91–0.93). This negative association was also evident when RC was treated as a categorical variable. The fully adjusted models indicated that the likelihood of returning to normoglycemia was 20% lower (SHR = 0.80, 95% CI 0.75–0.86) in the second quartile (Q2) compared to the first quartile (Q1), 35% lower (SHR = 0.65, 95% CI 0.61–0.70) in the third quartile (Q3), and 50% lower in the fourth quartile (Q4) (SHR = 0.50, 95% CI 0.46–0.54).
Results of subgroup analysis
The association between RC and the reversion to normoglycemia from Pre-DM remained consistent across all the examined prespecified and exploratory subgroups, including sex, SBP,smoking, age, DBP, and drinking status (Supplementary Table S4). In other words, there was no statistically significant interaction between RC and these variables (P > 0.05 for interaction).
Non-linear relationship between RC and the reversion to normoglycemia from Pre-DM
Utilizing the Cox proportional hazards regression model with cubic spline functions, we identified a nonlinear association between RC and the HR value (Fig. 5). By employing recursive techniques, the inflection point for RC was pinpointed at 51.08 mg/dL. The relationship between RC and the reversion to normoglycemia was subsequently analyzed on either side of this inflection point using the Cox proportional hazards regression model, resulting in HR and confidence interval (CI) values for both segments (Table 6). Prior to the inflection point, the HR was 0.907 (95% CI 0.897–0.917, P < 0.001, per 5 mg/dL). Beyond this point, the HR was observed to be 0.985 (95% CI 0.953–1.019, P = 0.386, per 5 mg/dL), which did not show statistical significance. The significant disparity in the relationship between RC and normoglycemia reversion on either side of the inflection point (P < 0.05 for the likelihood ratio test) indicates a potential nonlinear relationship.
Discussion
This retrospective cohort study identified a negative relationship between RC levels and the likelihood of reversion to normoglycemia in patients with Pre-DM. Moreover, a threshold effect was noted, with an inflection point occurring at an RC level of 50.24 mg/dL. The relationship between RC and reversion to normoglycemia from Pre-DM exhibited different characteristics on either side of this inflection point.
A cohort study conducted in the United Kingdom revealed that 54% of individuals with Pre-DM reverted to normoglycemia within a year of follow-up, while 6% progressed to DM46. Another investigation involving 491 participants found that 22.6% of prediabetics returned to normoglycemia9. Additionally, a Chinese cohort study including 14,231 adults with Pre-DM reported that 44.9% reversed to normoglycemia within a two-year period15. In our study, the median follow-up duration was 2.95 years, with 45.54% of prediabetic patients reverting to normoglycemia. The varying reversion rates observed in different studies may be attributed to differences in age, ethnicity, and follow-up duration among the participants. Notably, a substantial proportion of prediabetic individuals can return to normoglycemia. Therefore, understanding the factors that facilitate this reversion is essential for preventing the progression to DM and its associated complications.
Atherogenic dyslipidemia, characterized by TG levels and diminished levels of TG-rich lipoproteins and HDL-c, has been extensively investigated in the context of cardiovascular disease over an extended period27,47,48,49. This lipid pattern is now acknowledged as a significant contributor to the residual risk of major cardiovascular events22,27,32. Atherogenic dyslipidemia, characterized by excessive production of TG-rich lipoproteins and inadequate lipolytic processing, is known to promote the formation of RC24. A mounting body of evidence suggests that RC is closely linked to DM and overall glucose metabolism25,33,50,51. A cohort study from China with 6 years of follow-up showed that the adjusted HR (95% confidence interval) for DM risk in the highest versus the lowest quartile of RC was 1.45 (1.19–1.75), with a 9% increase in diabetes risk for every one standard deviation (19.52 mg/dl) increase in RC (HR = 1.09; 1.03–1.15)33. A study from Korea showed that participants in the upper quartile of RC had a higher risk of developing T2D compared to the lowest quartile of RC, with HR of 1.25 (95% CI 1.24–1.27) in the second quartile, 1.51 (95% CI 1.50–1.53) in the third quartile, and 1.95 (95% CI 1.93- 1.97) in the fourth quartile50. A similar finding was reported in another Chinese study, where increased RC (mmol/L) levels were linked to a higher risk of developing DM (HR = 2.44, 95% CI 1.50–3.89)25. In addition, Additionally, Ohnishi et al. analyzed data from 472 residents in a rural Japanese community and found a strong association between RC and the homeostasis model assessment index (HOMA-R)52. Likewise, Funada et al. identified RC as an independent predictor of HOMA-R53. Given that RC is a common dyslipidemia pattern in insulin-resistant individuals, we hypothesized that elevated RC might negatively impact the reversion to normoglycemia from prediabetes. However, most current research has centered on the link between RC and disease progression, neglecting its potential impact on regression to normoglycemia from prediabetes. Our study supports the hypothesis that higher RC is associated with a lower likelihood of reverting to normoglycemia from Pre-DM. Recognizing RC as a risk factor for the return to normoglycemia and understanding its association provides a crucial reference for facilitating this reversion and preventing DM in patients with Pre-DM. Moreover, our study examined RC both as a categorical and continuous variable in relation to reverting to normoglycemia from Pre-DM, reducing information loss and quantifying the relationship more accurately. Sensitivity analyses focused on participants with a BMI < 24 kg/m2, no family history of DM, or TG < 1.7 mmol/L. These analyses confirmed the previously mentioned relationships within this subset of participants. Additionally, the results from the multivariate Cox proportional hazards regression analysis for competing risks matched those from the standard multivariate Cox model, underscoring the robustness of our findings. In conclusion, our study offers valuable insights into potential interventions for individuals with prediabetes, aiming to enhance their likelihood of returning to normoglycemia and lowering their risk of developing DM and its complications. These findings contribute to better public health outcomes and improved management of Pre-DM.
The mechanisms underlying the association between RC and the reversal of Pre-DM to normoglycemia remain unclear. IR might be a key factor in this relationship. Research in a rural community demonstrated a strong association between fasting RC and IR52. Another study found that postprandial RC independently predicted IR, regardless of BMI, age, and other lipid profiles53. Furthermore, RC can directly induce β-cell dysfunction, subsequently suppressing insulin secretion54. Thus, reducing RC may decrease IR, enhance insulin sensitivity, and promote the reversal of Pre-DM to normoglycemia, potentially explaining the observed association.
In addition, for the first time in our study, a non-linear relationship was observed between RC and reversal of Pre-DM to normoglycemia. The inflection point of RC was determined to be 51.08 mg/dL. When RC was less than 51.08 mg/dL, the probability of return to normoglycemia declined by 9.3% for every 5 mg/d increase in RC. On the other hand, when the RC was greater than 51.08 mg/dL, there was no significant association. In other words, the probability of returning to normoglycemia did not increase significantly as the patient's RC decreased. However, when the RC decreased to approximately 51.08 mg/dL, further decreases in RC significantly increased the probability of reversion to normoglycemia. This finding of a curvilinear relationship between RC and regression to normoglycemia from Pre-DM has significant clinical value. It facilitates clinical counseling and provides a basis for decision-making to optimize diabetes prevention. In other words, by controlling RC levels at least below 51.08 mg/d through dietary interventions and lifestyle changes, further control of RC levels may significantly increase the probability of returning to normal blood glucose in prediabetic patients.
This study possesses several notable strengths: (i) It marks the first exploration of the relationship between RC and the reversion of Pre-DM to normoglycemia using a cohort of Chinese adults with Pre-DM. (ii) The study's sample size exceeded 15,000 participants, spanning multiple regions in China, thereby enhancing the generalizability and relevance of the findings to the Chinese population. (iii) It identified a potential nonlinear relationship between RC and the reversion of prediabetes to normoglycemia, representing a significant advancement. (iv) Single imputation was employed for missing data, which maximized statistical power and minimized bias arising from incomplete covariate data. (v) To ensure the robustness of the findings, a series of sensitivity analyses were conducted: these included treating RC as a categorical variable, incorporating continuous covariates as curves in the equation through a generalized additive model, utilizing a competing risks model, and reanalyzing the relationship between RC and the reversion to normoglycemia after excluding participants with a BMI ≥ 24 kg/m2, TG ≥ 1.7 mmol/L, and a family history of DM.
However, some limitations should be acknowledged: First, the relationship between RC and reversion to normoglycemia from Pre-DM might differ among racial groups. Therefore, our findings need validation across diverse racial populations. Future collaborations with international researchers are planned to verify these associations in populations with varying genetic backgrounds. Second, the Pre-DM definition was solely based on FPG levels ranging from 5.6 to 6.9 mmol/L, excluding glycated hemoglobin (HbA1c) and 2-h oral glucose tolerance test (2 h-OGTT) metrics. Consequently, the identified prediabetic population may be underestimated. Despite the difficulty in obtaining HbA1c measurements or conducting 2 h-OGTT for such a large cohort, future efforts will aim to collect as much 2-h plasma glucose and HbA1c data as possible to create more accurate cohorts to validate our conclusions. Besides, even though all participants adhered to a stringent protocol for fasting venous blood sample collection after a minimum 10-h fast, and FPG was measured with an autoanalyzer (Beckman 5800), FPG levels might still fluctuate based on prior dietary intake, potentially compromising the accuracy of defining prediabetes and its reversion to normoglycemia. The definition of Pre-DM and the reversion to normoglycemia may be inaccurate. But for a cohort study with such a large sample, multiple measurements of fasting glucose at baseline and follow-up are challenging. In the future, we will measure FPG levels as many times as possible to define Pre-DM and the reversion to normoglycemia. Third, this study being a secondary analysis of existing data, adjustments for physical activity, diet, waist circumference, hypersensitive C-reactive protein (hs-CRP), and insulin concentration were limited. However, E-values were calculated, suggesting that unmeasured confounders were unlikely to have significantly influenced the results. Future research designs and collaborations will aim to incorporate comprehensive data, including inflammatory markers, lifestyle factors, and lipid-lowering medications, to thoroughly analyze the RC-normoglycemia relationship and validate our findings. Fourth, although a single imputation is simple and straightforward, it ignores the inherent uncertainty and variability in the process of handling missing data, which may lead to reduced robustness and accuracy of statistical analysis. In the future, we will collect more variable information to reduce missing data and strive to use multiple imputation methods to address missing values, thereby providing more accurate and robust imputation results. Fifth, this investigation assessed RC and other parameters solely at baseline, lacking analysis of longitudinal RC changes. Future studies, including those involving collaborations, will gather data on RC changes over time.Lastly, it is crucial to note that this retrospective observational study can only propose an independent association between RC and the reversion to normoglycemia in prediabetic patients, without establishing a causal relationship.
Conclusion
This study revealed a non-linear negative association between RC levels and the reversion to normoglycemia among Chinese adults with prediabetes. Specifically, when RC measured below 51.08 mg/dL, lower RC levels were significantly linked to a higher likelihood of reverting to normoglycemia in prediabetic individuals. Clinicians and patients should collaborate to reduce RC levels through dietary interventions and lifestyle modifications, aiming to bring RC levels to at least below 51.08 mg/dL. Further reductions beyond this threshold may substantially enhance the chances of successful reversion to normoglycemia.
Data availability
Access to data is available through the 'DATADRYAD' database (http://www.Datadryad.org). Specifically at https://datadryad.org/stash/dataset/doi:10.5061/dryad.ft8750v.
Abbreviations
- ALT:
-
Alanine aminotransferase
- BMI:
-
Body mass index
- Pre-DM:
-
Prediabetes
- Scr:
-
Serum creatinine
- HDL-c:
-
High-density lipoprotein cholesterol
- HBA1c:
-
Glycated hemoglobin
- DBP:
-
Diastolic blood pressure
- LDL-c:
-
Low-density lipoproteins cholesterol
- AST:
-
Aspartate aminotransferase
- FPG:
-
Fasting plasma glucose
- SBP:
-
Systolic blood pressure
- GAM:
-
Generalized additive model
- TG:
-
Triglyceride
- UA:
-
Uric acid
- DM:
-
Diabetes mellitus
- TC:
-
Total cholesterol
- IDF:
-
International Diabetes Federation
- CI:
-
Confidence interval
- BUN:
-
Blood urea nitrogen
- Ref:
-
Reference
- HR:
-
Hazard ratio
References
Echouffo-Tcheugui, J. B., Perreault, L., Ji, L. & Dagogo-Jack, S. Diagnosis and management of prediabetes: A review. JAMA J. Am. Med. Assoc. 329, 1206–1216 (2023).
Herman, W. H. Prediabetes diagnosis and management. JAMA J. Am. Med. Assoc. 329, 1157–1159 (2023).
Classification and Diagnosis of Diabetes. Standards of medical care in diabetes-2022. Diabetes Care 45, S17–S38 (2022).
Sun, H. et al. Idf Diabetes atlas: Global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res. Clin. Pract. 183, 109119 (2022).
Garber, A. J. et al. Diagnosis and management of prediabetes in the continuum of hyperglycemia: When do the risks of diabetes begin? A consensus statement from the American College of Endocrinology and the American Association of Clinical Endocrinologists. Endocr. Pract. 14, 933–946 (2008).
Brannick, B. & Dagogo-Jack, S. Prediabetes and cardiovascular disease: Pathophysiology and interventions for prevention and risk reduction. Endocrinol. Metabol. Clin. N. Am. 47, 33–50 (2018).
Brannick, B., Wynn, A. & Dagogo-Jack, S. Prediabetes as a toxic environment for the initiation of microvascular and macrovascular complications. Exp. Biol. Med. 241, 1323–1331 (2016).
Abdul-Ghani, M., DeFronzo, R. A. & Jayyousi, A. Prediabetes and risk of diabetes and associated complications: impaired fasting glucose versus impaired glucose tolerance: Does it matter?. Curr. Opin. Clin. Nutr. Metab. Care. 19, 394–399 (2016).
Sevilla-González, M. et al. Clinical and metabolomic predictors of regression to normoglycemia in a population at intermediate cardiometabolic risk. Cardiovasc. Diabetol. 20, 56 (2021).
Knowler, W. C. et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N. Engl. J. Med. 346, 393–403 (2002).
Gerstein, H. C. et al. Effect of rosiglitazone on the frequency of diabetes in patients with impaired glucose tolerance or impaired fasting glucose: A randomised controlled trial. Lancet. 368, 1096–1105 (2006).
Busquets-Cortés, C. et al. Utility of fatty liver index to predict reversion to normoglycemia in people with prediabetes. PLoS ONE. 16, e249221 (2021).
Lazo-Porras, M. et al. Regression from prediabetes to normal glucose levels is more frequent than progression towards diabetes: The Cronicas Cohort Study. Diabetes Res. Clin. Pract. 163, 107829 (2020).
Perreault, L. et al. Regression from prediabetes to normal glucose regulation and prevalence of microvascular disease in the Diabetes Prevention Program Outcomes Study (DPPOS). Diabetes Care. 42, 1809–1815 (2019).
Liu, X., Wu, S., Song, Q. & Wang, X. Reversion from pre-diabetes mellitus to normoglycemia and risk of cardiovascular disease and all-cause mortality in a Chinese population: A prospective cohort study. J. Am. Heart Assoc. 10, e19045 (2021).
Herman, W. H. et al. Impact of lifestyle and metformin interventions on the risk of progression to diabetes and regression to normal glucose regulation in overweight or obese people with impaired glucose regulation. Diabetes Care. 40, 1668–1677 (2017).
Hwang, Y. C., Cho, I. J., Jeong, I. K., Ahn, K. J. & Chung, H. Y. Factors associated with regression from prediabetes to normal glucose tolerance in a Korean general population: A community-based 10-year prospective cohort study. Diabet. Med. 35, 1544–1551 (2018).
Han, Y., Hu, H., Huang, Z. & Liu, D. Association between body mass index and reversion to normoglycemia from impaired fasting glucose among chinese adults: A 5-year cohort study. Front. Endocrinol. 14, 1111791 (2023).
Athyros, V. G. et al. Diabetes and lipid metabolism. Horm.-Int. J. Endocrinol. Metab. 17, 61–67 (2018).
Al, A. T. et al. The association between prediabetes and dyslipidemia among attendants of primary care health centers in Jeddah, Saudi Arabia. Diabetes Metab. Syndr. Obes. 12, 2735–2743 (2019).
Huang, Z. et al. Triglyceride to high-density lipoprotein cholesterol ratio is associated with regression to normoglycemia from prediabetes in adults: A 5-year cohort study in China. J. Transl. Med. 21, 868 (2023).
Castañer, O. et al. Remnant cholesterol, not LDL cholesterol, is associated with incident cardiovascular disease. J. Am. Coll. Cardiol. 76, 2712–2724 (2020).
Jepsen, A. M. et al. Increased remnant cholesterol explains part of residual risk of all-cause mortality in 5414 patients with ischemic heart disease. Clin. Chem. 62, 593–604 (2016).
Ginsberg, H. N. et al. Triglyceride-rich lipoproteins and their remnants: Metabolic insights, role in atherosclerotic cardiovascular disease, and emerging therapeutic strategies—a consensus statement from the European Atherosclerosis Society. Eur. Heart J. 42, 4791–4806 (2021).
Xie, G., Zhong, Y., Yang, S. & Zou, Y. Remnant cholesterol is an independent predictor of new-onset diabetes: A single-center cohort study. Diabetes Metab. Syndr. Obes. 14, 4735–4745 (2021).
Cao, Y. X. et al. The longitudinal association of remnant cholesterol with cardiovascular outcomes in patients with diabetes and pre-diabetes. Cardiovasc. Diabetol. 19, 104 (2020).
Yu, D. et al. Remnant cholesterol and cardiovascular mortality in patients with type 2 diabetes and incident diabetic nephropathy. J. Clin. Endocrinol. Metab. 106, 3546–3554 (2021).
Schaefer, E. J. et al. Elevated remnant-like particle cholesterol and triglyceride levels in diabetic men and women in the framingham offspring study. Diabetes Care. 25, 989–994 (2002).
Chen, Y. et al. Association of body mass index and age with incident diabetes in Chinese adults: A population-based cohort study. BMJ Open. 8, e21768 (2018).
Goodyear, M. D., Krleza-Jeric, K. & Lemmens, T. The Declaration of Helsinki. BMJ Br. Med. J. 335, 624–625 (2007).
Pan, W., Han, Y., Hu, H. & He, Y. The non-linear link between remnant cholesterol and diabetic retinopathy: A cross-sectional study in patients with type 2 diabetic mellitus. BMC Endocr. Disord. 22, 326 (2022).
Mach, F. et al. 2019 ESC/EAS guidelines for the management of dyslipidaemias: Lipid modification to reduce cardiovascular risk. Eur. Heart J. 41, 111–188 (2020).
Zheng, X., Jiang, M., Ren, X. & Han, L. The longitudinal association of remnant cholesterol with diabetes in middle-aged and elderly Chinese: A nationwide population-based cohort study. J. Diabetes Complications. 37, 108360 (2023).
Mo, Z. et al. Association between non-high-density lipoprotein to high-density lipoprotein ratio and reversion to normoglycemia in people with impaired fasting glucose: A 5-year retrospective cohort study. Diabetol. Metab. Syndr. 15, 259 (2023).
Sun, Y., Wang, Z., Huang, Z., Hu, H. & Han, Y. The association between the triglyceride-to-high-density lipoprotein cholesterol ratio and the risk of progression to diabetes from prediabetes: A 5-year cohort study in Chinese adults. Front. Endocrinol. 13, 947157 (2022).
White, I. R., Royston, P. & Wood, A. M. Multiple imputation using chained equations: Issues and guidance for practice. Stat. Med. 30, 377–399 (2011).
Groenwold, R. H. et al. Missing covariate data in clinical research: When and when not to use the missing-indicator method for analysis. Can. Med. Assoc. J. 184, 1265–1269 (2012).
Basak, R., Mistry, H. & Chen, R. C. Understanding competing risks. Int. J. Radiat. Oncol. Biol. Phys. 110, 636–640 (2021).
Berger, M., Schmid, M., Welchowski, T., Schmitz-Valckenberg, S. & Beyersmann, J. Subdistribution hazard models for competing risks in discrete time. Biostatistics. 21, 449–466 (2020).
Wagner, R. et al. Family history of diabetes is associated with higher risk for prediabetes: A multicentre analysis from the German Center for Diabetes Research. Diabetologia. 56, 2176–2180 (2013).
Klein, S., Gastaldelli, A., Yki-Järvinen, H. & Scherer, P. E. Why does obesity cause diabetes?. Cell Metab. 34, 11–20 (2022).
Karin, A. et al. Body mass index in adolescence, risk of type 2 diabetes and associated complications: A nationwide cohort study of men. Eclinicalmedicine. 46, 101356 (2022).
Zhao, J. et al. Triglyceride is an independent predictor of type 2 diabetes among middle-aged and older adults: A prospective study with 8-year follow-ups in two cohorts. J. Transl. Med. 17, 403 (2019).
Haneuse, S., VanderWeele, T. J. & Arterburn, D. Using the E-value to assess the potential effect of unmeasured confounding in observational studies. JAMA-J. Am. Med. Assoc. 321, 602–603 (2019).
von Elm, E. et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: Guidelines for reporting observational studies. Lancet. 370, 1453–1457 (2007).
Bodicoat, D. H. et al. Incident type 2 diabetes and the effect of early regression to normoglycaemia in a population with impaired glucose regulation. Diabet. Med. 34, 396–404 (2017).
Sandesara, P. B., Virani, S. S., Fazio, S. & Shapiro, M. D. The forgotten lipids: Triglycerides, remnant cholesterol, and atherosclerotic cardiovascular disease risk. Endocr. Rev. 40, 537–557 (2019).
Duran, E. K. et al. Triglyceride-rich lipoprotein cholesterol, small dense LDL cholesterol, and incident cardiovascular disease. J. Am. Coll. Cardiol. 75, 2122–2135 (2020).
Varbo, A., Freiberg, J. J. & Nordestgaard, B. G. Extreme nonfasting remnant cholesterol vs extreme LDL cholesterol as contributors to cardiovascular disease and all-cause mortality in 90000 individuals from the general population. Clin. Chem. 61, 533–543 (2015).
Huh, J. H. et al. Remnant cholesterol is an independent predictor of type 2 diabetes: A nationwide population-based cohort study. Diabetes Care. 46, 305–312 (2023).
Mensenkamp, A. R., Havekes, L. M., Romijn, J. A. & Kuipers, F. Hepatic steatosis and very low density lipoprotein secretion: The involvement of apolipoprotein E. J. Hepatol. 35, 816–822 (2001).
Ohnishi, H. et al. Relationship between insulin-resistance and remnant-like particle cholesterol. Atherosclerosis. 164, 167–170 (2002).
Funada, J. et al. The close relationship between postprandial remnant metabolism and insulin resistance. Atherosclerosis. 172, 151–154 (2004).
Hao, M., Head, W. S., Gunawardana, S. C., Hasty, A. H. & Piston, D. W. Direct effect of cholesterol on insulin secretion: A novel mechanism for pancreatic beta-cell dysfunction. Diabetes. 56, 2328–2338 (2007).
Acknowledgements
The primary data and methodology for this secondary analysis were derived from the research conducted by Chen, Ying et al. (2018) titled "Association of body mass index and age with incident diabetes in Chinese adults: a population-based cohort study". We extend our sincere gratitude to the authors of this study for providing the foundation of our study.
Funding
The present study was funded by the Key Clinical Research Project of Shenzhen Second People's Hospital (20243357011).
Author information
Authors and Affiliations
Contributions
The study design and initial manuscript draft were developed by Weifeng Chen, Haofei Hu, and Changchun Cao. Statistical analysis and data interpretation, aimed at ensuring data integrity and accuracy, were undertaken by Haofei Hu and Yong Han. Moreover, Yong Han and Dehong Liu provided significant input to the discussion sections and critically reviewed the manuscript. All authors have thoroughly examined and approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Chen, W., Hu, H., Cao, C. et al. Link between remnant cholesterol and the reversion to normoglycemia in Chinese adults with prediabetes: a 5-year cohort study. Sci Rep 14, 18098 (2024). https://doi.org/10.1038/s41598-024-69169-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-69169-x
- Springer Nature Limited