Abstract
The effect of systemic inflammation, represented by high-sensitivity C-reactive protein (hsCRP), on triglyceride glucose (TyG) index-associated cardiovascular risk in patients with acute coronary syndrome (ACS) undergoing percutaneous coronary intervention (PCI) has not yet been determined. This study was a retrospective analysis of a single-center prospective registry and finally included 1701 patients (age, 60 ± 10 years; male, 76.7%). The primary endpoint was defined as major adverse cardiovascular events (MACE), including cardiovascular mortality, non-fatal stroke, and non-fatal myocardial infarction. In the multivariate COX regression model that included the GRACE risk score, higher TyG index was significantly associated with a greater incidence of MACE in patients with hsCRP levels less than 2 mg/L but not 2 mg/L or more (P for interaction = 0.039). Each unit increase in the TyG index was independently associated with a 52% increased risk of MACE only in patients with hsCRP levels less than 2 mg/L (P = 0.021). After adjustment for other confounding factors, including the GRACE risk score, compared with those in the group of TyG index < 8.62 and hsCRP < 2 mg/L, patients in the group of TyG index ≥ 8.62 and hsCRP ≥ 2 mg/L had a 3.9 times higher hazard ratio for developing MACE. The addition of both TyG index and hsCRP had an incremental effect on the predictive ability of the GRACE risk score-based prognostic model for MACE (C-statistic: increased from 0.631 to 0.661; cNRI: 0.146, P = 0.012; IDI: 0.009, P < 0.001). In conclusion, there was a significant interaction between the TyG index and hsCRP for the risk of MACE, and the TyG index was reliably and independently associated with MACE only when hsCRP levels were less than 2 mg/L. Furthermore, high TyG index and high hsCRP levels synergistically increased the risk of MACE, suggesting that the prognostic value of TyG index combined with hsCRP might be promising in patients with ACS undergoing PCI.
Similar content being viewed by others
Introduction
Acute coronary syndrome (ACS) is a group of clinical syndromes characterized by complete or incomplete occlusive thrombosis secondary to the rupture or erosion of coronary atherosclerotic plaques, and is composed of ST-segment elevation myocardial infarction (STEMI), non-STEMI (NSTEMI), and unstable angina (UA). Despite significant advances in the treatment of ACS over the past decades, such as superior percutaneous coronary intervention (PCI) techniques and instruments, more potent P2Y12 inhibitors (ticagrelor or prasugrel), intensive lipid-lowering therapy (low-density lipoprotein cholesterol < 1.4 mmol/L), neurohormonal agents, and lifestyle modification, an unacceptable proportion of patients continue to experience future adverse cardiovascular events1. Age-related physiological changes and the accumulation of known and unexplored cardiovascular risk factors increase the lifetime susceptibility of patients with ACS undergoing PCI to adverse cardiovascular events. Early identification of patients with ACS undergoing PCI at a high risk of short- and long-term adverse cardiovascular outcomes is helpful for the timely implementation of effective treatment to reduce such risk.
Insulin resistance is an important cardiovascular risk factor that can easily be overlooked. A series of studies have provided compelling evidence that insulin resistance is strongly associated with cardiovascular diseases and events, both in the general population and in patients with diabetes2. The triglyceride glucose (TyG) index is considered a reliable surrogate marker of insulin resistance3 and has been shown to be a sound predictor of adverse cardiovascular outcomes in a variety of patient populations, including ACS patients, regardless of diabetes status4,5,6. In fact, inflammation is an important cause of insulin resistance and the latter has adverse cardiovascular effects mainly through the former7,8. However, whether and how systemic inflammation affects the predictive value of insulin resistance in adverse cardiovascular outcomes has not been adequately studied. A large body of evidence supports the use of high-sensitivity C-reactive protein (hsCRP) as a clinical marker of systemic inflammation9. Therefore, the present study was designed to investigate the effect of hsCRP as a substitute indicator of systemic inflammation on the TyG index in predicting major adverse cardiovascular events (MACE) in ACS patients who underwent PCI.
Methods
Study population
This study was a retrospective analysis of a single-center prospective registry involving 1770 consecutive patients who had received primary or elective percutaneous coronary intervention (PCI) for ACS at our cardiovascular center between June 2016 and November 2017. For the purpose of the present study, patients with prior coronary artery bypass grafting (CABG), left ventricular ejection fraction (LVEF) < 30%, Killip class > II, renal dysfunction with creatinine clearance (CrCl) < 30 ml/min, acute and/or chronic infection, connective tissue disease, or known malignancy were excluded. Four patients were also excluded because of missing follow-up data despite at least four separate attempts to contact them. Finally, 1701 patients were included in the analysis. Because the data analyzed were obtained from a prospective registry database, no missing laboratory data existed. This study was conducted in accordance with the Helsinki Declaration of Human Rights and approved by the Medical Ethics Committee of Beijing Anzhen Hospital, Capital Medical University. The requirement for informed consent was waived by the Medical Ethics Committee of Beijing Anzhen Hospital, Capital Medical University due to the retrospective nature of this study.
Measurements
Data on demographics, lifestyle, medical history, and medication history were prospectively collected using standardized questionnaires. The concentrations of hsCRP, fasting plasma glucose (FPG), triglycerides, total cholesterol (TC), high-density lipoprotein cholesterol (HDL-C) and serum creatinine (SCr) in the first fasting blood samples after admission, which were obtained after 12 h of fasting, were measured at the central laboratory of Beijing Anzhen Hospital. Low-density lipoprotein cholesterol (LDL-C) levels were calculated using the Friedewald equation. The TyG index was calculated as ln (fasting triglyceride [mg/dL] × fasting glucose [mg/dL]/2). CrCl was calculated using the method described by Cockcroft and Gault10. Hypertension was defined as a blood pressure ≥ 140/90 mmHg, chronic use of antihypertensive drugs, or self-reported previous diagnosis of hypertension. Diabetes was defined as symptoms of diabetes with casual plasma glucose ≥ 200 mg/dL, FPG ≥ 126 mg/dL, or 2-h plasma glucose ≥ 200 mg/dL from a 75 g oral glucose tolerance test, chronic use of antidiabetic drugs, or self-reported previous diabetes diagnosis. Dyslipidemia was defined as fasting TC > 200 mg/dL, LDL-C > 130 mg/dL, HDL-C < 40 mg/dL, triglyceride > 150 mg/dL, chronic use of lipid-lowering drugs, or self-reported previous diagnosis of dyslipidemia. Peripheral arterial disease (PAD) was defined as vascular diseases related to the aorta and arteries, except the coronary arteries, which were accompanied by exercise-related intermittent claudication, revascularization surgery, reduced or absent pulsation, angiographic stenosis > 50%, or a combination of these characteristics. Heart failure was defined as signs or symptoms of heart failure, treatment for heart failure, or LVEF of less than 40%. The GRACE risk score was calculated based on age, heart rate at admission, systolic blood pressure at admission, Killip class, serum creatinine and cardiac biomarker levels, ST-segment deviation at admission and the presence of cardiac arrest at presentation for each patient.
Follow-up and endpoints
Follow-up visits were conducted one month and every six months after discharge. Information on adverse cardiovascular outcomes was obtained by trained personnel with no knowledge of baseline characteristics through telephone contact with the patients or their family members and was determined by careful review of the corresponding medical records. The primary endpoint was defined as MACE, including cardiovascular mortality, non-fatal stroke, and non-fatal myocardial infarction (MI). Cardiovascular death was defined as death due to acute myocardial infarction, sudden cardiac death, heart failure, stroke, cardiovascular surgery, cardiovascular bleeding, or other cardiovascular causes. Non-fatal stroke was defined as acute local dysfunction of the brain, spinal cord, or retina caused by a central nervous system tissue infarct that did not result in death. Non-fatal MI was defined as elevated levels of cardiac biomarkers (cardiac troponin or creatine kinase-MB) with at least one value above the 99% upper reference value accompanied by ischemic symptoms or electrocardiogram changes that did not result in death. The most severe endpoint event was selected for the primary endpoint analysis if the patients had multiple endpoint events during follow-up (death > stroke > MI). If more than one stroke or MI event occurred, then the first stroke or MI event was considered. The final follow-up was conducted in November 2019.
Statistical analysis
Patients were divided into two groups based on whether a primary endpoint event occurred, which served as the primary analysis set. Receiver operating characteristic (ROC) curve analysis and Youden’s index (sensitivity + specificity—1) was used to determine the optimal cutoff value of TyG index as a continuous variable (= 8.62) for predicting the occurrence of MACE. All patients were grouped according to the TyG index dichotomy (cutoff value = 8.62) and/or hsCRP dichotomy (cutoff value = 2 mg/L) for the additional analysis. Continuous variables were reported as mean ± standard deviation for normal distribution where t-test was used for comparisons between two groups or ANOVA was used for comparisons between multiple groups, and were reported as median and interquartile range (IQR) for non-normal distribution where Mann–Whitney U test was used for comparisons between two groups or the Kruskal–Wallis H test was used for comparisons between multiple groups. Categorical variables were reported as frequency and percentage where the Chi-square test (χ2 test) or Fisher’s exact test was used for comparisons between groups. Kaplan–Meier curves were used to describe the cumulative incidence of MACE over time, and the log-rank test was used to compare differences between the groups. After confirming that the proportional hazards assumption was satisfied, multivariable Cox proportional hazards regression modeling was used to compare the hazard ratios (HRs) with 95% confidence intervals (CIs) for MACE across groups, while adjusting for covariates of statistical significance and clinical importance, including or excluding the GRACE risk score. The interaction between the TyG index and hsCRP for the risk of MACE was tested using the likelihood test with the multivariate Cox proportional hazard regression model including GRACE risk score. Stratified analysis was performed when a significant interaction was observed. At last, the C-statistics, continuous net reclassification improvement (cNRI) and integrated discrimination improvement (IDI) were calculated to show the incremental predictive effect of adding both TyG index and hsCRP to the GRACE risk score-based prognostic model. All P values were derived from 2-tailed tests and the results were considered statistically significant at P < 0.05. Statistical analyses were performed using SPSS (version 24.0; IBM Corp., Armonk, New York, US) and R software (version 4.1.0; R Foundation for Statistical Computing, Beijing, China). Figures were created using GraphPad Prism (version 7.0; GraphPad Software Inc., San Diego, California, US).
Ethical approval
This study was approved by the Institutional Review Board of the Beijing Anzhen Hospital, Capital Medical University. The requirement for informed consent was waived by the Medical Ethics Committee of Beijing Anzhen Hospital, Capital Medical University due to the retrospective nature of this study.
Results
Of the 1,701 included patients (mean age, 60 ± 10 years), 396 (23.3%) were female and 1305 (76.7%) were male. The median follow-up duration was 30 months (IQR, 30–36 months). During the follow-up period, 100 (5.9%) patients developed at least one primary endpoint event, including 36 cardiovascular deaths, 24 non-fatal strokes, and 49 non-fatal MIs. Of the 100 patients who had MACE, 10 (10.0%) suffered two MACE events.
Table 1 describes the baseline characteristics of patients stratified according to MACE. Compared with those without, patients with MACE had a higher proportion of previous MI (28.0 vs. 18.6%; P = 0.020), previous PCI (33.0 vs. 19.1%; P = 0.001), PAD (35.0 vs. 8.5%; P < 0.001), heart failure (26.0 vs. 5.6%; P < 0.001), and ST-segment deviation (28.0 vs. 16.9%; P = 0.004). Patients with MACE tended to be older and have higher heart rate, systolic blood pressure, GRACE risk score, FPG levels, TyG index, hsCRP levels, and SYNTAX score and lower HDL-C levels and LVEF. In patients with MACE, there were fewer patients with low TyG index and low hsCRP levels, and more patients with high TyG index and high hsCRP levels. In terms of medication use, among patients with MACE, more were prescribed angiotensin-converting enzyme inhibitors (ACEIs)/angiotensin receptor blockers (ARBs) and insulin at discharge. The baseline characteristics of patients stratified by the TyG index, the hsCRP, and the combination of TyG index and hsCRP are shown in Tables S1, S2, and S3, respectively. Of note, compared with those with TyG index < 8.62, patients with TyG index ≥ 8.62 had higher heart rate at admission (70 ± 9 vs. 66 ± 9 bpm; P < 0.001) (Table S1). Spearman’s rank correlation analysis showed a relatively weak positive correlation between heart rate at admission and TyG index (Rs = 0.173; P < 0.001). Patients with TyG index ≥ 8.62 had higher rates of STEMI and left-main/multi-vessel disease, and higher levels of SCr (Table S1)). Also, patients with TyG index ≥ 8.62 had higher SYNTAX score (a valuable tool which can estimate the severity and complexity of coronary artery disease) and a higher rate of prior ischemic cerebrovascular disease (ischemic stroke or transient ischemic attack) (Table S1). Compared with patients with TyG index < 8.62, patients with TyG index ≥ 8.62 had significantly higher odds ratios (ORs) of having left-main/multi-vessel disease (OR 1.413; 95% CI 1.077–1.853; P = 0.012), intermediate-to-high SYNTAX score (SYNTAX score > 22) (OR 1.326; 95% CI 1.079–1.630; P < 0.001), and ischemic cerebrovascular disease (OR 1.779; 95% CI 1.094–2.893; P = 0.020).
Univariate and multivariate Cox proportional hazards regression analyses for the primary endpoint in the overall population are shown in Table 2, where both the TyG index and hsCRP levels were considered categorical variables. In order to avoid repeatedly adding the same or highly correlated variables to affect Cox model fitting, components of the GRACE risk score were not included in the multivariate Cox regression model which had included the GRACE risk score. In the univariate analyses, compared with those with the TyG index < 8.62, patients with the TyG index ≥ 8.62 were at higher risk of the primary endpoint (HR, 1.819; 95% CI 1.133–2.920; P = 0.013). Similarly, compared with those with hsCRP levels < 2 mg/L, patients with hsCRP levels ≥ 2 mg/L were at a higher risk of the primary endpoint (HR 2.149; 95% CI 1.446–3.192; P < 0.001). After adjusting for other confounding factors, including the GRACE risk score, both higher TyG index and higher hsCRP levels were significantly associated with the primary endpoint (adjusted HR 1.728 [95% CI 1.041–2.871] for TyG index dichotomy, and 1.742 [95% CI 1.149–2.642] for hsCRP dichotomy). When considered as a continuous variable in the overall population, the TyG index was associated with an HR of 1.460 (95% CI 1.075–1.982, P = 0.015) in the univariate analysis and 1.518 (95% CI 1.066–2.162, P = 0.021) in the multivariate analysis (Table 3). After adjusting for other confounding factors, including heart rate at admission, age, and body mass index but excluding the GRACE risk score, both higher TyG index and higher hsCRP levels remained significantly associated with the primary endpoint (adjusted HR: 1.692 [95% CI 1.004–2.852] for TyG index dichotomy, and 1.819 [95% CI 1.200–2.758] for hsCRP dichotomy) (Table S4). Of note, heart rate at admission was associated with an HR of 1.047 (95% CI 1.027–1.067; P < 0.001) in the univariate analysis and 1.033 (95% CI 1.013–1.054; P = 0.001) in the multivariate analysis (Table S4), which suggested that a higher heart rate at admission was an independent predictor for MACE after ACS undergoing PCI.
When stratifying the overall population according to hsCRP levels less than 2 mg/L vs. 2 mg/L or more, higher TyG index was significantly associated with MACE only when hsCRP levels were less than 2 mg/L (adjusted HR 2.221, 95% CI 1.358–3.632; P = 0.001) (Table 3). In the setting of hsCRP levels of 2 mg/L or more, higher TyG index was not associated with a greater risk of MACE (adjusted HR 1.029; 95% CI 0.588–1.801; P = 0.919) (Table 3).
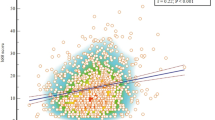
A significant interaction between the continuous TyG index and hsCRP dichotomy was observed for the risk of MACE [P for interaction in the univariate analysis: continuous TyG index × hsCRP dichotomy = 0.015; P for interaction in the multivariate analysis: continuous TyG index × hsCRP dichotomy = 0.039]. Figure 1 shows the cumulative incidence of MACE over time stratified by the TyG index in the setting of hsCRP levels less than 2 mg/L (Fig. 1A) or 2 mg/L or more (Fig. 1B). In those with hsCRP levels of 2 mg/L or more, higher TyG index was not associated with a higher cumulative incidence of MACE over time (log-rank test, P = 0.576). However, in those with hsCRP levels less than 2 mg/L, higher TyG index was significantly associated with a higher cumulative incidence of MACE over time (log-rank test, P = 0.016).
The study patients were further divided into four groups based on the TyG index less than 8.62 vs. greater than or equal to 8.62 and hsCRP less than 2 mg/L vs. 2 mg/L or more. After adjusting for potential confounding factors, including GRACE risk score, compared with those in the low TyG index and low hsCRP group, patients in the high TyG index and low hsCRP, low TyG index and high hsCRP, and high TyG index and high hsCRP groups had a 2.67-fold (HR, 2.670; 95% CI 1.253–5.692), a 3.29-fold (HR 3.290; 95% CI 1.390–7.789), and a 3.87-fold (HR 3.874; 95% CI 1.824–8.229) elevated risk of MACE, respectively (P for trend = 0.005) (Table 4). Figure 2 shows the cumulative incidence of MACE over time stratified by the TyG index less than 8.62 vs. greater than or equal to 8.62 and hsCRP less than 2 mg/L versus 2 mg/L or more. The results showed that the cumulative incidence of MACE over time was highest in patients with TyG index ≥ 8.62 and hsCRP levels ≥ 2 mg/L, and the cumulative incidence of MACE over time was significantly lower in patients with TyG index < 8.62 and hsCRP levels < 2 mg/L (log-rank test, P < 0.001). The addition of both TyG index and hsCRP had an incremental effect on the predictive ability of the GRACE risk score-based prognostic model for MACE (C-statistic: increased from 0.631 [95% CI 0.572–0.691] to 0.661 [95% CI 0.604–0.717]; NRI 0.146 [95% CI 0.036–0.254], P = 0.012; IDI 0.009 [95% CI 0.003–0.022], P < 0.001).
Discussion
In the present study, we found that both higher TyG index and higher hsCRP levels were significantly associated with MACE in the multivariate Cox regression model. In the overall study population, compared with those with TyG index < 8.62, patients with TyG index ≥ 8.62 had a 1.73-fold increased risk of MACE; while compared with those with hsCRP levels < 2 mg/L, patients with hsCRP levels ≥ 2 mg/L had a 1.74-fold increased risk of MACE. There was a significant interaction between the TyG index and hsCRP for the risk of MACE, and the TyG index was reliably and independently associated with MACE in patients with hsCRP levels less than 2 mg/L but not 2 mg/L or more. After the study patients were further divided into four groups based on the TyG index less than 8.62 vs. greater than or equal to 8.62 and hsCRP less than 2 mg/L versus 2 mg/L or more, we found that compared with those in the low TyG index and low hsCRP group, patients in the high TyG index and low hsCRP, low TyG index and high hsCRP, and high TyG index and high hsCRP groups had a 2.67-fold, a 3.29-fold, and a 3.87-fold increased risk of MACE, respectively (P for trend = 0.005). Therefore, the present study supports the idea that the influence of systemic inflammation needs to be considered when using the TyG index to predict adverse cardiovascular outcomes among patients with ACS undergoing PCI, and that the prognostic value of the TyG index combined with hsCRP is more clinically significant.
C-reactive protein (CRP) is a protein associated with systemic inflammation and is therefore a well-recognized indicator of inflammation. As inflammation has been shown to be involved in the development of atherosclerosis, CRP can be used to predict cardiovascular risk when analyzed with a more sensitive assay capable of measuring extremely low levels of CRP, called hsCRP11. The prognostic significance of CRP and hsCRP levels in ACS patients has been demonstrated in several studies. A meta-analysis of 20 longitudinal studies of 17,422 patients with ACS showed a moderately dose-dependent positive association between early blood CRP levels and long-term risk of recurrent cardiovascular events or death after ACS12. A study by Schiele et al., including 1,501 patients with ACS, showed that elevated CRP levels were modestly but independently associated with mortality, and the combination of CRP with the GRACE risk score would allow for improved risk classification13. Recently, a retrospective cohort study based on the National Institute for Health Research Health Informatics Collaborative data, including 102,337 patients with suspected ACS, suggested that elevated hsCRP levels (≥ 2 vs. < 2 mg/L) were clinically meaningful prognostic indicator14. Our study similarly found that hsCRP was a valuable predictor of adverse cardiovascular outcomes in patients with ACS undergoing PCI.
The TyG index is a novel and reliable surrogate marker of insulin resistance independent of glycemic status. The TyG index, an independent predictor of adverse cardiovascular events in patients with ACS, has been confirmed in multiple studies. A study by Xiong et al. including 986 ACS patients undergoing PCI showed that the TyG index was an independent predictor of long-term all-cause death and non-fatal MI after PCI in ACS patients, regardless of diabetes mellitus, and improved the predictive ability of the GRACE risk score-based prognostic model15. The study of Karadeniz FÖ et al. including 646 patients with STEMI and 1,048 patients with NSTEMI showed a significant association between higher TyG index and increased risk of the composite of all-cause mortality, non-fatal MI, and repeat target vessel revascularization in ACS patients16. A recent meta-analysis of 15 observational studies, including 27,880 patients with ACS, revealed that the TyG index was significantly associated with adverse cardiovascular outcomes, both as a categorical and continuous variable17. Of note, Shao QY and colleagues found that the TyG index showed a better ability to predict the risk of the composite of all-cause mortality, non-fatal stroke, non-fatal MI, and unplanned repeat revascularization than the three other triglyceride-derived metabolic indices (Atherogenic Index of Plasma, triglyceride to HDL-C ratio, and Lipoprotein Combine Index)6. Our findings are consistent with those of the aforementioned studies; however, none of these studies considered the effect of systemic inflammation on the prognostic value of the TyG index. In our study, we found that there was a significant interaction between the TyG index and hsCRP for the risk of MACE, and only in patients whose hsCRP levels were less than 2 mg/L, the TyG index was reliably and independently associated with MACE.
The significant interaction between the TyG index and hsCRP for the risk of MACE may be related to the intrinsic bidirectional relationship between insulin resistance and systemic inflammation in a biological context18,19,20,21,22,23,24,25,26,27,28. Insulin resistance is closely associated with chronic inflammation and the production of inflammatory mediators such as interleukin (IL)-6, IL-1β, tumor necrosis factor-α (TNF-α), monocyte chemoattractant protein-1 (MCP-1), and plasminogen activator inhibitor-1 (PAI-1), which lay the foundation for the increased production of CRP29.
Insulin resistance is an important feature of cardiometabolic diseases and has been established as a major risk factor for atherosclerotic cardiovascular disease30. Importantly, substantial evidence suggests that insulin resistance and its underlying molecular etiology of insulin resistance can explain a major component of the unexplained cardiovascular risk in patients with insulin resistance syndrome, obese non-diabetes, prediabetes, and type 2 diabetes31. The etiology of insulin resistance has been thoroughly studied, and chronic inflammation is now recognized as an important cause of insulin resistance7,28. Reciprocally, compensatory hyperinsulinemia caused by insulin resistance leads to overstimulation of the MAP kinase pathway, which is involved in the inflammatory response that leads to cell damage and vascular endothelial dysfunction31. These conditions suggest that inflammation induces insulin resistance, which in turn exacerbates the inflammatory response, forming a vicious cycle that ultimately leads to rapid development of atherosclerosis. Intriguingly, insulin resistance has also been shown to directly reduce vascular smooth muscle cell survival and to promote atherosclerotic plaque vulnerability32. Our study showed that the predictive value of the TyG index for MACE was significantly diminished in patients with an enhanced inflammatory response. This may be related to the hypothesis that insulin resistance plays a role in the initial stages of atherosclerosis; however, in the later stages of atherosclerosis, the role of inflammation far outweighs insulin resistance itself.
Notably, we found that higher heart rate at admission was independently and significantly associated with MACE, and there was a correlation between heart rate at admission and the TyG index, a reliable surrogate marker of insulin resistance. As we know, heart rate can reflect autonomic activity. Studies have shown that increased sympathetic activity might contribute to insulin resistance, and insulin resistance is associated with increased sympathetic and reduced parasympathetic activity33, both of which can lead to an increase in heart rate.
Colchicine, which inhibits systemic inflammation and reduces levels of hsCRP, has been shown to reduce cardiovascular events in patients with coronary artery disease34,35, which suggests that there is a definite causal relationship between inflammation and coronary atherosclerosis. Thiazolidinediones are the only true insulin-sensitizing hypoglycemic drugs, and at least one drug, pioglitazone, has been shown to promote the regression of atherosclerotic lesions36,37 and reduce cardiovascular events38,39 in high-risk patients with type 2 diabetes31. The randomized IRIS trial including 3876 patients without diabetes who had insulin resistance (homeostasis model assessment of insulin resistance [HOMA-IR] index > 3.0) and a recent (≤ 6 months) history of ischemic stroke or transient ischemic attack showed that patients who received pioglitazone had a lower risk of stroke or myocardial infarction than those who received a placebo40. Unfortunately, an association between improved insulin sensitivity and decreased cardiovascular events has not been reported. Pioglitazone can reduce cardiovascular events through multiple mechanisms, the most important of which is the reduction in the inflammatory response31. The TyG index includes triglyceride and glucose in its formula. Elevated triglyceride and glucose levels have been associated with adverse cardiovascular outcomes. Unfortunately, randomized trials of therapies that primarily lowered triglycerides have not consistently shown a reduction in adverse cardiovascular events41,42. Moreover, considerable evidence suggests that intensive (compared with moderate) glycemic control has no significant benefit on microvascular or macrovascular outcomes, except for reducing the incidence of non-fatal MI43.
Notably, we found that the combination of high TyG index and high hsCRP levels led to better identification of patients with ACS undergoing PCI at a higher risk for recurrence of cardiovascular events. The synergistic role of insulin resistance and inflammation in the development of atherosclerosis, as noted above, supports this finding. The value of TyG index combined with hsCRP in predicting cardiovascular disease and events has been validated in several studies. Zhang N and colleagues in their study based on the Kongcun Town asymptomatic intracranial artery stenosis study including 1,398 participants aged ≥ 40 years who were free of stroke or transient ischemic attack, found that participants with high TyG index and high hsCRP levels had higher odds ratio of single or multiple moderate-to-severe asymptomatic intracranial arterial stenosis than those with low TyG index and low hsCRP levels44. A study by Feng et al. including 9,626 middle-aged and elderly adults from the China Health and Retirement Longitudinal Study (CHARLS) showed that participants with high TyG index and high hsCRP levels had a higher risk of new-onset cardiac events or stroke than those with low TyG index and low hsCRP levels45. A study by Li et al. including 4,419 patients with diabetes and chronic coronary syndrome from the PRospective Observational Multi-center cohort for ISchemic and hEmorrhage risk in coronary artery disease patients (PROMISE) showed that the combination of high TyG index and high hsCRP levels significantly increased the 2-year risk of the composite of cardiac death, non-fatal MI, and any revascularization, and hsCRP partially mediated the impact of the TyG index on adverse cardiovascular outcomes46.
To our knowledge, this is the first study to investigate the effect of hsCRP on TyG index-associated cardiovascular risk and the combined effects of the TyG index and hsCRP on cardiovascular risk in patients with ACS undergoing PCI. However, this study had several limitations. First, this was a retrospective observational study, in which a causal relationship could not be definitively established. Second, while identifying and adjusting for potential confounding factors, the influence of unknown or unmeasured confounding factors cannot be excluded because of the observational nature of this study. Third, we did not use the hyperinsulinemic-euglycemic clamp test (the gold standard) or HOMA-IR (the most commonly used method) to assess insulin resistance and thus could not accurately estimate the true insulin resistance status. In addition, we used only hsCRP levels to represent the degree of the systemic inflammatory response, which may lead to an inaccurate assessment of inflammation. Fourth, our study was conducted exclusively in the Chinese population; therefore, our findings may not be generalizable to other ethnic populations. Fifth, because heart rate was measured once at admission and there was a lack of continuous monitoring of heart rate, we were unable to assess sequential heart rate variability after admission in patients. Therefore, the association of TyG index with sequential heart rate variability after admission and its predictive value for adverse cardiovascular outcomes could not be investigated. Sixth, when the original database was established, the time from the onset of ACS to admission to hospital (this time might be related to fasting time) was not collected. Lastly, our study only evaluated the association of the baseline TyG index and hsCRP with MACE (fasting blood samples were obtained on the first morning after admission for testing triglyceride, glucose and hsCRP); therefore, the impact of the change trajectory of these biomarkers on MACE needs to be further verified.
Conclusions
In the overall patient population, both higher TyG index and higher hsCRP levels were significantly associated with MACE. However, there was a significant interaction between the TyG index and hsCRP for the risk of MACE, and the TyG index was reliably and independently associated with MACE in patients only when hsCRP levels were less than 2 mg/L. Furthermore, high TyG index and high hsCRP levels synergistically increased the risk of MACE, suggesting that the prognostic value of TyG index combined with hsCRP might be promising in patients with ACS undergoing PCI. Large, well-designed, prospective studies are needed to validate these findings.
Data availability
The datasets used in this study are available from the corresponding author upon reasonable request.
Abbreviations
- ACEI:
-
Angiotensin-converting enzyme inhibitor
- ACS:
-
Acute coronary syndrome
- ARB:
-
Angiotensin receptor blocker
- CABG:
-
Coronary artery bypass grafting
- CI:
-
Confidence interval
- cNRI:
-
Continuous net reclassification improvement
- CrCl:
-
Creatinine clearance
- CRP:
-
C-reactive protein
- FPG:
-
Fasting plasma glucose
- HDL-C:
-
High-density lipoprotein cholesterol
- HOMA-IR:
-
Homeostasis model assessment of insulin resistance
- HR:
-
Hazard ratio
- HsCRP:
-
High-sensitivity C-reactive protein
- IDI:
-
Integrated discrimination improvement
- IQR:
-
Interquartile range
- LDL-C:
-
Low-density lipoprotein cholesterol
- LVEF:
-
Left ventricular ejection fraction
- MACE:
-
Major adverse cardiovascular events
- MI:
-
Myocardial infarction
- OR:
-
Odds ratio
- PAD:
-
Peripheral artery disease
- PCI:
-
Percutaneous coronary intervention
- SCr:
-
Serum creatinine
- STEMI:
-
ST-segment elevation myocardial infarction
- TC:
-
Total cholesterol
- TyG:
-
Triglyceride glucose
- UA:
-
Unstable angina
References
Bhatt, D. L., Lopes, R. D. & Harrington, R. A. Diagnosis and treatment of acute coronary syndromes: A review. Jama 327(7), 662–675 (2022).
Adeva-Andany, M. M., Martínez-Rodríguez, J., González-Lucán, M., Fernández-Fernández, C. & Castro-Quintela, E. Insulin resistance is a cardiovascular risk factor in humans. Diabetes Metab. Syndr. 13(2), 1449–1455 (2019).
Ramdas Nayak, V. K., Satheesh, P., Shenoy, M. T. & Kalra, S. Triglyceride Glucose (TyG) index: A surrogate biomarker of insulin resistance. J. Pak. Med. Assoc. 72(5), 986–988 (2022).
Ma, X. et al. Triglyceride glucose index for predicting cardiovascular outcomes after percutaneous coronary intervention in patients with type 2 diabetes mellitus and acute coronary syndrome. Cardiovasc. Diabetol. 19(1), 31 (2020).
Tao, L. C., Xu, J. N., Wang, T. T., Hua, F. & Li, J. J. Triglyceride-glucose index as a marker in cardiovascular diseases: Landscape and limitations. Cardiovasc. Diabetol. 21(1), 68 (2022).
Shao, Q. Y. et al. Prognostic significance of multiple triglycerides-derived metabolic indices in patients with acute coronary syndrome. J. Geriatr. Cardiol. 19(6), 456–468 (2022).
Glass, C. K. & Olefsky, J. M. Inflammation and lipid signaling in the etiology of insulin resistance. Cell. Metab. 15(5), 635–645 (2012).
Ormazabal, V. et al. Association between insulin resistance and the development of cardiovascular disease. Cardiovasc. Diabetol. 17(1), 122 (2018).
Lawler, P. R. et al. Targeting cardiovascular inflammation: Next steps in clinical translation. Eur. Heart J. 42(1), 113–131 (2021).
Cockcroft, D. W. & Gault, M. H. Prediction of creatinine clearance from serum creatinine. Nephron 16(1), 31–41 (1976).
Moutachakkir, M., Lamrani Hanchi, A., Baraou, A., Boukhira, A. & Chellak, S. Immunoanalytical characteristics of C-reactive protein and high sensitivity C-reactive protein. Ann. Biol. Clin. (Paris) 75(2), 225–229 (2017).
He, L. P., Tang, X. Y., Ling, W. H., Chen, W. Q. & Chen, Y. M. Early C-reactive protein in the prediction of long-term outcomes after acute coronary syndromes: A meta-analysis of longitudinal studies. Heart 96(5), 339–346 (2010).
Schiele, F. et al. C-reactive protein improves risk prediction in patients with acute coronary syndromes. Eur. Heart J. 31(3), 290–297 (2010).
Kaura, A. et al. Mortality risk prediction of high-sensitivity C-reactive protein in suspected acute coronary syndrome: A cohort study. PLoS Med. 19(2), e1003911 (2022).
Xiong, S. et al. Adjustment of the GRACE score by the triglyceride glucose index improves the prediction of clinical outcomes in patients with acute coronary syndrome undergoing percutaneous coronary intervention. Cardiovasc. Diabetol. 21(1), 145 (2022).
Karadeniz, F., Sancaktepe, E. A. & Karadeniz, Y. High triglyceride-glucose index is associated with poor prognosis in patients with acute coronary syndrome in long-term follow-up. Angiology 74(2), 139–148 (2023).
Liang, S. et al. Triglyceride-glucose index and coronary artery disease: A systematic review and meta-analysis of risk, severity, and prognosis. Cardiovasc. Diabetol. 22(1), 170 (2023).
McLaughlin, T. et al. Differentiation between obesity and insulin resistance in the association with C-reactive protein. Circulation 106(23), 2908–2912 (2002).
Rhee, E. J. et al. Comparison of insulin resistance and serum high-sensitivity C-reactive protein levels according to the fasting blood glucose subgroups divided by the newly recommended criteria for fasting hyperglycemia in 10059 healthy Koreans. Metabolism 55(2), 183–187 (2006).
Lu, B. et al. Insulin resistance in Chinese patients with type 2 diabetes is associated with C-reactive protein independent of abdominal obesity. Cardiovasc. Diabetol. 9, 92 (2010).
Chou, H. H. et al. Insulin resistance is associated with C-reactive protein independent of abdominal obesity in nondiabetic Taiwanese. Metabolism 59(6), 824–830 (2010).
Tanigaki, K. et al. C-reactive protein causes insulin resistance in mice through Fcγ receptor IIB-mediated inhibition of skeletal muscle glucose delivery. Diabetes 62(3), 721–731 (2013).
Dali-Youcef, N., Mecili, M., Ricci, R. & Andrès, E. Metabolic inflammation: Connecting obesity and insulin resistance. Ann. Med. 45(3), 242–253 (2013).
Uemura, H. et al. Relationships of serum high-sensitivity C-reactive protein and body size with insulin resistance in a Japanese cohort. PLoS One 12(6), e0178672 (2017).
Yang, M. et al. Genetic ablation of C-reactive protein gene confers resistance to obesity and insulin resistance in rats. Diabetologia 64(5), 1169–1183 (2021).
Shahid, R., Chu, L. M., Arnason, T. & Pahwa, P. Association between insulin resistance and the inflammatory marker C-reactive protein in a representative healthy adult Canadian population: Results from the Canadian Health Measures Survey. Can. J. Diabetes 47(5), 428–434 (2023).
Li, K. et al. Effect of C-reactive protein deficiency on insulin resistance reversal in rats with polycystic ovary syndrome through augmented leptin action. Diabetol. Metab. Syndr. 15(1), 180 (2023).
Zand, H., Morshedzadeh, N. & Naghashian, F. Signaling pathways linking inflammation to insulin resistance. Diabetes Metab. Syndr. 11(Suppl 1), S307-s309 (2017).
Zhu, Y. et al. Research progress on the relationship between atherosclerosis and inflammation. Biomolecules 8(3), 80 (2018).
Semenkovich, C. F. Insulin resistance and atherosclerosis. J. Clin. Invest. 116(7), 1813–1822 (2006).
Di Pino, A. & DeFronzo, R. A. Insulin resistance and atherosclerosis: Implications for insulin-sensitizing agents. Endocr. Rev. 40(6), 1447–1467 (2019).
Martínez-Hervás, S. et al. Insulin resistance aggravates atherosclerosis by reducing vascular smooth muscle cell survival and increasing CX3CL1/CX3CR1 axis. Cardiovasc. Res. 103(2), 324–336 (2014).
Beddhu, S., Nigwekar, S. U., Ma, X. & Greene, T. Associations of resting heart rate with insulin resistance, cardiovascular events and mortality in chronic kidney disease. Nephrol. Dial. Transpl. 24(8), 2482–2488 (2009).
Sun, M. et al. Low-dose colchicine and high-sensitivity C-reactive protein after myocardial infarction: A combined analysis using individual patient data from the COLCOT and LoDoCo-MI studies. Int. J. Cardiol. 363, 20–22 (2022).
Alam, M. et al. Meta-analysis of the effect of colchicine on C-reactive protein in patients with acute and chronic coronary syndromes. Coron. Artery Dis. 34(3), 210–215 (2023).
Mazzone, T. et al. Effect of pioglitazone compared with glimepiride on carotid intima-media thickness in type 2 diabetes: A randomized trial. JAMA 296(21), 2572–2581 (2006).
Nissen, S. E. et al. Comparison of pioglitazone vs glimepiride on progression of coronary atherosclerosis in patients with type 2 diabetes: The PERISCOPE randomized controlled trial. JAMA 299(13), 1561–1573 (2008).
Dormandy, J. A. et al. Secondary prevention of macrovascular events in patients with type 2 diabetes in the PROactive Study (PROspective pioglitAzone Clinical Trial In macroVascular Events): A randomised controlled trial. Lancet 366(9493), 1279–1289 (2005).
Lincoff, A. M., Wolski, K., Nicholls, S. J. & Nissen, S. E. Pioglitazone and risk of cardiovascular events in patients with type 2 diabetes mellitus: A meta-analysis of randomized trials. JAMA 298(10), 1180–1188 (2007).
Kernan, W. N. et al. Pioglitazone after ischemic stroke or transient ischemic attack. N. Engl. J. Med. 374(14), 1321–1331 (2016).
Marston, N. A. et al. Association between triglyceride lowering and reduction of cardiovascular risk across multiple lipid-lowering therapeutic classes: A systematic review and meta-regression analysis of randomized controlled trials. Circulation 140(16), 1308–1317 (2019).
Das Pradhan, A. et al. Triglyceride lowering with pemafibrate to reduce cardiovascular risk. N. Engl. J. Med. 387(21), 1923–1934 (2022).
Rodriguez-Gutierrez, R., Gonzalez-Gonzalez, J. G., Zuñiga-Hernandez, J. A. & McCoy, R. G. Benefits and harms of intensive glycemic control in patients with type 2 diabetes. BMJ 367, l5887 (2019).
Zhang, N. et al. Association of triglyceride-glucose index and high-sensitivity C-reactive protein with asymptomatic intracranial arterial stenosis: A cross-sectional study. Nutr. Metab. Cardiovasc. Dis. 31(11), 3103–3110 (2021).
Feng, G. et al. Combined effects of high sensitivity C-reactive protein and triglyceride-glucose index on risk of cardiovascular disease among middle-aged and older Chinese: Evidence from the China Health and Retirement Longitudinal Study. Nutr. Metab. Cardiovasc. Dis. 33(6), 1245–1253 (2023).
Li, T. et al. Inflammation and insulin resistance in diabetic chronic coronary syndrome patients. Nutrients 15(12), 28085 (2023).
Funding
This work was supported by grants from the National Key Research and Development Program of China (2022YFC3602500), Youth Program of the National Natural Science Foundation of China (82200405), and Capital’s Funds for Health Improvement and Research (2022-2-1052).
Author information
Authors and Affiliations
Contributions
X.M. and H.C. analyzed the data and drafted the manuscript. X.M., Y.S., Y.C., and D.Z. prospectively collected the demographic data, laboratory data, angiographic and interventional data of the enrolled patients. Y.Z. proposed amendments to the first draft. X.M., X.L., and Z.W. designed the study and revised the manuscript. All authors contributed to the acquisition of data and final approval of the version to be published.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Ma, X., Chu, H., Sun, Y. et al. The effect of hsCRP on TyG index-associated cardiovascular risk in patients with acute coronary syndrome undergoing PCI. Sci Rep 14, 18083 (2024). https://doi.org/10.1038/s41598-024-69158-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-69158-0
- Springer Nature Limited