Abstract
Accurate assessment of vital parameters is essential for diagnosis and triage of critically ill patients, but not always feasible in out-of-hospital settings due to the lack of suitable devices. We performed an extensive validation of a novel prototype in-ear device, which was proposed for the non-invasive, combined measurement of core body temperature (Tc), oxygen saturation (SpO2), and heart rate (HR) in harsh environments. A pilot study with randomized controlled design was conducted in the terraXcube environmental chamber. Participants were subsequently exposed to three 15 min test sessions at the controlled ambient temperatures of 20 °C, 5 °C, and − 10 °C, in randomized order. Vital parameters measured by the prototype were compared with Tc measurements from commercial esophageal (reference) and tympanic (comparator) probes and SpO2 and HR measurements from a finger pulse-oximeter (reference). Performance was assessed in terms of bias and Lin’s correlation coefficient (CCC) with respect to the reference measurements and analyzed with linear mixed models. Twenty-three participants (12 men, mean (SD) age, 35 (9) years) completed the experimental protocol. The mean Tc bias of the prototype ranged between − 0.39 and − 0.80 °C at ambient temperatures of 20 °C and 5 °C, and it reached − 1.38 °C only after 15 min of exposure to − 10 °C. CCC values ranged between 0.07 and 0.25. SpO2 and HR monitoring was feasible, although malfunctioning was observed in one third of the tests. SpO2 and HR bias did not show any significant dependence on environmental conditions, with values ranging from − 1.71 to − 0.52% for SpO2 and 1.12 bpm to 5.30 bpm for HR. High CCC values between 0.81 and 0.97 were observed for HR in all environmental conditions. This novel prototype device for measuring vital parameters in cold environments demonstrated reliability of Tc measurements and feasibility of SpO2 and HR monitoring. Through non-invasive and accurate monitoring of vital parameters from the ear canal our prototype may offer support in triage and treatment of critically ill patients in harsh out-of-hospital conditions.
Similar content being viewed by others
Introduction
Accurate on-site assessment of vital parameters, such as core body temperature (Tc), oxygen saturation (SpO2), and heart rate (HR), is essential for triage and care of critically ill patients. Tc is a key parameter driving in-field triage decisions for accidentally hypothermic patients1,2,3,4. SpO2 is a relevant parameter in patients at risk of hypoxaemia5 and it is also used to determine an optimal oxygen target6. HR is the first hemodynamic variable that is extensively monitored in pre-hospital care and to ensure optimal treatment7,8.
Monitoring patient vital signs in emergency conditions in pre-hospital settings requires instruments that are accurate, portable, easy-to-use, and minimally invasive1,9. In addition, measuring vital parameters in harsh environments requires that accuracy is robust at very low ambient temperatures, and in the presence of wind and/or moisture, all conditions that may influence the measurements10,11. Hearables are emerging technologies that allow monitoring of vital parameters from the ear canal9, a location that has practical and physiological advantages in harsh environmental conditions. Probes can be easily inserted and stably positioned in the ear canal, granting stability of measurements12,13,14,15. The vasculature supplying the ear and the tympanic membrane, which includes the basilar artery and internal carotid artery, is shared with the brain, which guarantees the presence of thermal equilibrium between the two sites and supports the reliability of Tc measurements9,16. Moreover, the area is scarcely influenced by the sympathetic nerve activity, which guarantees adequate blood flow even at low temperatures and adequate photoplethysmography signals for HR and SpO2 assessment9.
Nowadays, no portable medical device is available on the market that performs multiparametric physiological monitoring and ensures accurate measurements in harsh environments. Recent studies have suggested the potential of physiological monitoring by in-ear devices9,17,18,19,20,21,22, but no study has been performed up to now to evaluate the reliability of in-ear devices under challenging environmental conditions and in comparison with technology used in routine clinical practice. We developed an in-ear device, called MedSENS, for monitoring Tc, SpO2, and HR from the ear canal. The device was designed with an insulating cover to work also out-of-hospital in harsh environments. In this study we aimed to provide an in-depth, multidimensional assessment of the performance of the MedSENS prototype under different ambient temperatures (Ta). Our primary objective was to assess the accuracy of Tc measurements by the prototype device in comparison to gold standard oesophageal measurements, and to compare its performance with that of commercial ear-probes designed without insulation. Secondary objectives were the assessment of the device accuracy in measuring SpO2 and HR, and the evaluation of its comfort and safety.
Materials and methods
This randomized, controlled, crossover pilot study is reported following the Consolidated Standards of Reporting Trials (CONSORT) reporting guidelines23.
Study population
The recruited participants were healthy male and female volunteers, aged between 18 and 65 years, with no fever, and classified as class I according to the American Society of Anesthesiologists (ASA)24. Exclusion criteria were age under 18 or over 65 years, ASA class greater than I, fever (temperature > 37.5 °C), and any acute disease. Specific exclusion criteria related to audiologic aspects were a history of hearing deficits, acute or chronic otitis media or externa, lesions of the tympanic membrane, major interventions in internal/medial ear or external ear canal, anatomic anomalies of the external ear canal, administration of medications that might influence neuro-otological functions, abnormal curve types during audiometric impedance test (B or C curve types), audiometric conductive deficit or absence of cochlear-stapedial reflex at 500, 1000, 2000, and 4000 Hz frequencies.
Sample size and randomization
The sample size was chosen to meet the criteria of a pilot study, which requires a minimum number of 12 participants to ensure reliable estimates of mean and variance25. Due to the experimental conditions, the randomization plan described below, and the risk of drop-out, the sample size was increased to 24 participants, balanced for gender, i.e., 12 male and 12 female participants.
A randomization list was created with the use of computer-generated sequences. The randomization variable was the sequence of the three test sessions, where the combination of the three different Ta exposures resulted in six different sequences (see Fig. 1 panel A). Each sequence was assigned to four participants, balanced in terms of gender and ear of insertion of the prototype device [i.e., two participants (one male and one female) with prototype device in the right ear and two participants (one male and one female) in the left ear].
Study design and equipment. (A) CONSORT scheme of the study, reporting experimental phases and randomization procedure (left). Following a medical and ENT assessment, the participants underwent a sequence of three test sessions at three different ambient temperatures (baseline temperature, 20 °C; low temperature, 5 °C; very low temperature, − 10 °C), interspersed by recovery sessions at standard room temperature (20 °C). Different conditions were realized in different rooms of an environmental chamber, where the participants were subsequently moved (right). (B) Study equipment. Each participant was equipped with the in-ear prototype device under test (first and second panel), an esophageal temperature probe as temperature reference and a tympanic temperature probe as temperature comparator (third panel). A finger pulse-oxymeter was used as oxygen saturation and heart rate reference (fourth panel).
Study protocol
The study flow chart is provided in Fig. 1 panel A. Each participant was exposed to three experimental sessions in different environmental conditions (i.e., three different Ta). Each session lasted 15 min and was followed by a wash-out period of 15 min. The three Ta were: 20 °C (baseline temperature), 5 °C (low temperature), and − 10 °C (very low temperature).
Prior to the experimental trial, each participant received a medical examination, followed by an ear-nose-throat (ENT) specialist examination to assess health status and eligibility for enrolment.
The participants sat for a stabilization period of 15 min in a room at a temperature of 20 °C, before starting the experimental session. During the sessions, the participant sat on a chair in a resting state. At the end of each test session, the participants evaluated the state of comfort/discomfort associated with the prototype device and the comparator device.
After the trial, the otoneurologist evaluated the potential presence of inflammation/injury induced by the prototype probes.
Experimental setting
All trials were performed in the terraXcube research facility (terraXcube, Eurac Research, Bolzano, Italy, https://terraxcube.eurac.edu) in the summer of 2021. The experimental sessions were performed at 262 m above sea level, where the participants were subsequently exposed to the three different Ta of 20 °C, 5 °C, and − 10 °C in three different chambers (Fig. 1 panel A). terraXcube Ta was kept constant at the scheduled values in each chamber and continuously monitored.
Pre-test examination
Each participant received a general medical examination, followed by an ENT examination, which included otoscopy, rhinoscopy, laryngoscopy, inspection of the external ear canal, and eventual removal of cerumen. The participant was given a pure tone audiometric exam to assess hearing acuity and an impedance test to verify the integrity of the tympanic membrane and ossicular chain, respectively26. A mold of the external ear canal was obtained according to the current clinical practice27 by injection of vulcanizing silicon (Otoform A flex, Dreve Otoplastik GmbH; Egger Otoplastik, Labortechnik GmbH, Kempten, Germany). The earmold was used to measure the length of the ear canal and to retrospectively assess the position of the prototype device in terms of distance from the tympanic membrane.
Measuring devices and equipment
The participant, in a sitting position, was instrumented with the prototype device, reference, and comparison devices for the measurement of the three vital parameters (Tc, SpO2, and HR), as shown in Fig. 1 panel B and described in the following paragraphs.
The MedSENS prototype
MedSENS is a patented prototype device (EP 3020327, EP 4265177 and WO 2023202894), able to simultaneously measure Tc, SpO2, and HR from the external ear canal. It consists of two components: an in-ear probe and an insulating headset cover. The in-ear probe (see Fig. 1B), which is positioned in the ear canal, is composed of two parts. The proximal part is made up of soft expanding polyurethane material for optimal fixing and insulation of the ear canal. The distal part (i.e., closer to the tympanum) is composed of a transparent 3D-printed silicone capsule, which harbors a negative-temperature-coefficient sensor (NTC, resistance of 100 kΩ) to measure Tc, and an ultra-low-power, completely integrated, optical data-acquisition system (Maxim MAXM86161, Maxim Integrated Products Inc, San Jose, CA, USA) to detect photo-plethysmograms for SpO2 and HR measurement28. The optical sensor embeds three programmable high-efficency LED drivers for light transmission, and a high efficiency PIN photo-diode for light detection. The optical readout includes a low-noise signal conditioning analog front-end, a 19-bit charge integrating analog-to-digital converter, and an ambient light cancellation circuit. Five probes were realized and used during the study. The headset, aimed to cover the ear and the mastoid area, is composed of a 3D-printed selective-laser-sintering (SLS) polyamide shell (1zu1 Prototypen GmbH & Co KG, Dornbirn, Austria). It contains a system-in-package microprocessor with built-in antenna [Blue Gecko Bluetooth®SiP Module (BGM 121, 2.4 GHz), Silicon Labs, San Jose, CA, USA], a biometric sensor hub (Maxim MAXM86161 sensor hub, Maxim Integrated Products Inc, San Jose, CA, USA) and a 18,650 Li-ion rechargeable battery (3.7 V, 3000 mA/h; estimated working life of 100 h), embedded in polyester insulating material. The microprocessor coordinates measurements, data display, and data transmission. It directly calculates Tc values, expressed in °C, and it reads SpO2 and HR values from the sensor hub via I2C connection. The sensor hub embeds a firmware and interfaces via I2C with the optical sensor to access raw and processed sensor data. These are elaborated by embedded algorithms to determine SpO2 values as a percentage of oxygenated hemoglobin (%) and HR in beats per minute (bpm). Tc, SpO2, and HR values are acquired by the microprocessor at 200 ms intervals. The bottom part of the headset shell is covered by an additional layer of polyethylene insulating material, embedded in silicon for safe contact with the skin. A small OLED display (Winstar Display Co., Ltd, Taichung City, Taiwan) is encapsulated in the upper part of the shell to display Tc, SpO2, and HR values. The prototype ear probe was inserted into the right/left ear of the participant, according to randomization, and the insulating headset was fixed to the participant’s head with a customized bandage system. The ENT specialist measured the length of the probe part exceeding the edge of the outer ear canal. This length was subtracted from the length of the mold of each participant to calculate the distance of the probe from the tympanic membrane. Tc, SpO2, and HR values measured by MedSENS (indicated by TcMed, SpO2Med, HRMed) constituted the test set of measurements under evaluation.
Reference and comparator devices
Reference invasive measurements of Tc (TcRef) were obtained by inserting an esophageal probe (ER400-12 Level 1® Esophageal Temperature Probe, Smiths Medical ASD, Inc., Minneapolis, MN, USA ) in the third lower part of the esophagus, according to the current guidelines29.
Comparator non-invasive measurements of Tc (TcCom) were obtained by inserting a commercial probe (TTS-400 Level 1® Tympanic Temperature Sensor, Smiths Medical ASD, Inc., St Paul, MN, USA) in the contralateral ear. The probe was positioned according to the producer’s instructions and fixed to the lobe using standard surgical tape to prevent displacement. No insulation of the ear canal was applied to provide comparative Tc measurements according to a standard approach.
Reference measurements of SpO2 (SpO2Ref) and HR (HRRef) were obtained by positioning a finger pulse-oxymeter (Masimo Corporation, Irvine, CA, USA) on the participant’s index finger of the non-dominant hand.
After successful insertion and positioning, the probes were connected to an emergency medicine monitor (Corpuls 3, Corpuls GS Elektromedizinische Geräte G. Stemple GmbH, Kaufering, Germany) for continuous display of reference and comparative measurements.
Other measurements
The otoneurologist scored the difficulty of the probe insertion process according to a visuo-analogue scale (VAS), ranging from 0 (no resistance) to 10 (high-resistance). The participants scored the comfort/discomfort of the MedSENS probe according to a VAS, ranging from 0 (no discomfort) to 10 (high-discomfort) after each test session and at the end of the study. The otoneurologist and the participants placed a mark on a 100-mm VAS, horizontally positioned with the extremes from 0 to 10.
The presence of inflammation/injury induced by the prototype device was evaluated by the ENT specialist by scoring the ear status according to a custom-made ordinal scale, ranging from 0 to 3, with scores defined as: 0 = no soreness; 1 = light superficial decubitus soreness, insertion without bleeding; 2 = decubitus soreness, insertion with auto-limiting bleeding; 3 = cutaneous decubitus soreness with hematic dripping necessitating hemostasis.
Data collection and analysis
T, SpO2, and HR data for the prototype (TcMed, SpO2Med, HRMed), reference (TcRef, SpO2Ref, HRRef) and comparative (TcCom) devices were manually collected from the OLED display and the emergency medicine monitor at 1-min interval during the three test sessions following a chronometer. Manually collected data represented the input data for the assessment of the device performance. Data were reported as mean (standard deviation, SD), or median (interquartile range, IQR), depending on data normality, which was assessed by Shapiro–Wilk test and normal Q-Q plots.
The capability of the prototype device to track vital parameters was assessed by comparing prototype measurements (TcMed, SpO2Med, HRMed) with the corresponding reference measurements (TcRef, SpO2Ref, HRRef). The bias between prototype and reference measurements was evaluated by constructing Bland–Altman plots and calculating the bias or mean difference (MD) and the limits of agreement (LoA, 1.96*SD) between the prototype and reference device. Lin’s concordance correlation coefficient (CCC) with confidence interval (CI) was also estimated as a cumulative measure of agreement. CCC combines both precision and accuracy metrics, being proportional to the Pearson’s correlation coefficient R but adjusted by a measure of bias. To assess the performance of the comparator device to measure Tc, bias and CCC values were computed also for commercial probe, comparing TcCom values with respect to the reference ones (TcRef). Bias and CCC values were computed at time intervals of 5 min during each test session (i.e., at 0, 5, 10, and 15 min).
The main environmental and technical factors influencing the performance of the prototype device to measure Tc, SpO2, and HR were investigated by linear mixed models (LMMs) for repeated measures, inserting the participants as a random effect. Specifically, three separate LMMs were built using the time series of Tc, SpO2, and HR bias at 1 min interval as dependent variables. As experimental factors we considered the time of measurement within each session (from 0 to 15 min), the condition (Ta of 20 °C, 5 °C, and − 10 °C), the interaction between time and condition, and the randomization sequence. As technical variables, we considered: the probe identifier as factor and the distance of the probe from the ear canal as covariate. P-values were corrected by utilizing the Bonferroni method.
Statistical differences among overall discomfort VAS scores of the prototype and commercial probes were assessed by Wilcoxon signed ranks test, while differences in prototype discomfort over time among the three test sessions were assessed by Friedman’s test.
Statistical analyses were performed using SPSS version 25 (IBM Corp., Armonk, NY, USA) and Matlab (Version R2019b, MathWorks, Inc., Natick, MA, United States). A p < 0.05 (two-sided) was considered statistically significant.
Ethical approval and consent to participate
The study was approved by the Ethics Committee review board of Bolzano and the Ministry of Health of Italy (n 42-2021). We conducted the study according to the Declaration of Helsinki. All participants were informed about the possible risks of being exposed to cold Ta and of testing a prototype device, and gave written informed consent prior to enrollment to participate and to use material (including eventual pictures) related to the study.
Results
Study population
Twenty-four participants were enrolled in the study. One participant was unable to participate due to esophageal probe intolerance (see Fig. 1 panel A). Therefore, a total of 23 participants [12 men; mean (SD) age, 35 (9) years] completed the study and were included in the data analysis. The participants had normal ENT parameters and type A tympanograms in both ears. The mean (SD) length of the external ear canal was 26 (3) mm (range 19–31 mm). Probes were inserted at a mean (SD) distance of 8 (2) mm (range 2–13 mm) from the tympanic membrane.
Prototype performance in Tc measurement
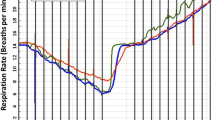
The time course of Tc, measured by the prototype device (in red), the comparator (in green), and the reference (in blue) devices at the three different ambient temperatures are shown in Fig. 2 (panels A). For each device and session, panels B report also the Tc change observed with respect to the start (time = 0 min) of the corresponding test session. At 20 °C (left panels), all three (prototype, comparator, and reference) devices showed no drop in Tc measurements. The prototype and comparator devices showed a mean (SD) Tc of 36.3 (0.7) °C and 34.3 (0.8) °C at 15 min, and the reference one of 36.7 (0.4) °C. At 5 °C (central panels), the prototype measurements showed a SD 0.8 °C and a mean (SD) drop of − 0.27 (0.22) °C after 15 min. The comparator showed a SD of 1.2 °C with a mean (SD) drop of − 1.06 (0.40) °C after 15 min. At − 10 °C (right panels), the prototype measurements showed a SD of 0.9 °C and a mean (SD) drop of − 1.04 (0.30) °C after 15 min, the comparator a SD of 1.8 °C with a mean (SD) drop of − 2.79 (1.03) °C after 15 min.
Time course of core body temperature measurements. Core body temperature (Tc) (A) and temperature changes (B; the reference is the temperature at entrance, time = 0) recorded with the prototype in-ear device (red, Med), commercial in-ear device (green, Com), and reference esophageal probe (blue, Ref) at baseline ambient temperature (20 °C, left), low ambient temperature (5 °C, center), and very low ambient temperature (− 10 °C, right). In all panels, data are mean ± standard deviation over N = 23 participants.
The accuracy and precision metrics for the test device and the comparator are summarized in Table 1, for different time points and ambient temperatures. Bland–Altman plots after 15 min of exposure to the three Ta are shown in Fig. 3. At 20 °C, the prototype measurements showed a mean bias, which improved over time from − 0.77 to − 0.39 °C, and CCC values ranging from 0.08 to 0.10. The comparator probe showed a larger mean bias (− 2.36 °C at 15 min) and a lower CCC (0.04 at 15 min). At 5 °C, the prototype showed a mean bias of − 0.80 °C at 15 min, with a CCC of 0.19. The comparator probe showed a larger mean bias of − 3.75 °C at 15 min, with a CCC of 0.01. At − 10 °C, the prototype measurements showed a mean negative bias not larger than − 1 °C within the first 10 min of exposure, although the bias reached − 1.38 °C at 15 min, with CCC of 0.07. The comparator probe showed a mean negative bias larger than − 4 °C already after 5 min of exposure and a bias of − 5.72 °C after 15 min, with CCC of 0.003.The bias of the prototype device was never statistically significant at any time point or considered condition (i.e., the 95% confidence intervals always contained 0), while the comparator showed always a statistically significant bias (p < 0.05) with the reference device.
Bland-Altmann plots of the core body temperature (Tc) bias of the prototype and of the comparator device. Bias values were calculated as difference between Tc values measured by the prototype in-ear device (TcMed, A) or the comparator in-ear device (TcCom, B) with respect to the esophageal reference (TcRef). The displayed values were measured after 15 min at baseline ambient temperature (20 °C, left), low ambient temperature (5 °C, center), and very low ambient temperature (− 10 °C, right). In the plots, the solid line indicates the mean difference and the dashed lines the limits of agreement (LoA, mean ± 1.96 standard deviation) for the overall population (N = 23 participants). At the top of each panel, we indicated the mean bias and LoA and Lin’s concordance correlation coefficient (CCC) with confidence intervals.
The results of the multivariate analysis on Tc bias of the prototype device are shown in Supplemental Table S1. The bias showed a significant dependence on the time and on the interaction of time and ambient temperature (experimental factors). The bias also showed a significant dependence on the used probe, but not on the distance of the probe from the tympanic membrane (technical factors).
Prototype performance in SpO2 and HR measurement
In eight of 23 cases, the optical sensor displayed malfunctioning, including intermittent behavior and/or unreliable values (see Supplemental Materials—Technical considerations). Data on bias and correlation for SpO2 and HR measurements for the participants with reliable measurements are presented in Table 2 and Fig. 4.
Bland-Altmann plots of the oxygen saturation and heart rate bias of the prototype device. Bias values were calculated as difference between oxygen saturation (A) and heart rate (B) values measured by the prototype in-ear device (SpO2Med and HRMed) with respect to the reference device (SpORef and HRRef). The displayed values were measured after 15 min at baseline ambient temperature (20 °C, left), low ambient temperature (5 °C, center), and very low ambient temperature (− 10 °C, right). In the plots, the solid line indicates the mean difference and the dashed lines the limits of agreement (LoA, mean ± 1.96 standard deviation) for the overall population (N = 23 and 18 participants, for SpO2 and HR, respectively). At the top of each panel, we indicated the mean bias and LoA and Lin’s concordance correlation coefficient (CCC) with confidence intervals.
SpO2 mean bias for the prototype was lower than 1% in most of the conditions. The bias increased in trials at − 10 °C to − 1.71%. CCC values ranged from − 0.06 to 0.24.
HR mean bias was lower than 2 bpm in most of the conditions. The bias was higher at the beginning of the session at − 10 °C (i.e., up to 5.30 bpm). CCC was high in all the analyzed conditions, with values ranging from 0.81 to 0.97.
The results of the multivariate analysis on SpO2 and HR measurements bias of the prototype device are shown in Supplemental Table S1. SpO2 bias was not dependent on any of the considered experimental nor technical factors. HR showed a significant dependence on time.
Prototype safety and comfortability
The mean (SD) VAS score related to the procedure of probe insertion (rated by the otoneurologist) was 6.0 (1.4) on a scale 0–10. The ENT specialist overall rated a moderate soreness in the ear, with 19 (83%) participants displaying no or only light superficial soreness (class 0–1) and four participants (17%) displaying decubitus soreness (class 2).
The VAS discomfort rated by the participants showed a median score (IQR) of 2.6 (0.48; 6.38) on a scale 0–10 for the prototype device and 0.40 (0.30; 0.22) for the comparator one (p = 0.02). Considering the sequence of conditions, the discomfort of the prototype was rated similar after the first two conditions [median (IQR) 1.50 (0.45; 5.78) and 1.40 (0.48; 6.13)], while it increased after the third test session [median (IQR) 2.9 (0.78; 5.68)], albeit no statistically significant difference was observed among the three sessions (p = 0.16).
Discussion
This randomized, controlled, crossover pilot study demonstrated for the first time the feasibility of a multiparameter physiological monitoring from the ear canal under harsh environmental conditions. We demonstrated that the novel multisensor MedSENS prototype was able to provide reliable Tc measurements in normal and cold environments, with a mean bias less than 1 °C, except after 15 min of exposure at − 10 °C. The measurement of SpO2 and HR from the ear canal was feasible, although, in one third of the participants, the prototype displayed intermittent functioning or provided unreliable HR measurements. The prototype probes were safe and produced only light discomfort, although slightly higher than the comparator one.
Performance of the prototype device
Our results showed the possibility of ensuring the accuracy of Tc measurements over a wide range of thermal conditions with a device that is less invasive than the esophageal probe. Under room temperature conditions (Ta of 20 °C), the device slightly underestimated TcRef with an average bias much lower than that obtained for the uncovered comparator probe. We previously reported a mean bias of − 2.9 °C at an average Ta of 23.2 °C between a commercial thermistor-based tympanic thermometer compared to an esophageal one in normothermic participants10. Using insulation, such bias could be reduced by 52% at normal Ta (the absolute difference of 2.9 °C decreased to 1.5 °C). Nagano et al. measured tympanic temperature using a custom-made probe (i.e., thermocouple sensor embedded in an earplug) and insulating the ear canal with a cotton ball in participants at rest at Ta of 25 °C. They reported an average bias of around − 0.3 °C compared to the esophageal reference30. Teunissen et al. built in-ear probes embedding a thermistor sensor in a participant-specific earmold, and tested the probes in participants at a Ta of 30 °C. They reported a mean bias of 1.49 °C with respect to esophageal Tc, bias which was reduced by 40% when the ear was extra-protected from the environment with a cotton patch covering the whole auricle31.
The ear is less conditioned by vasoconstriction and shows more appropriate perfusion compared to other anatomical sites, such as the finger, where poor peripheral perfusion in the presence of cold environments can compromise Tc measurements32. Our prototype device maintained a reliable performance when participants were exposed to lower Ta, thus supporting the hypothesis that the ear canal is a promising site for Tc measurement, if proper insulation is achieved. The prototype device showed low dispersion and bias, which were maintained after 15 min at 5 °C and were still acceptable at − 10 °C. In contrast, the performance of the uncovered commercial probe was significantly compromised in all tested conditions. Such impairment of the comparator confirm the results of previous studies investigating the effects of cold environments on tympanic Tc measurements10,31. In both studies, the tympanic site displayed lower accuracy than the gold-standard esophageal reference in cold and windy ambient conditions and insulation improved the performance. Insulation reduced Tc bias from − 7.2 °C to only − 1.3 °C (82% reduction) in cold conditions10 and from − 2.49 to − 1.73 °C (31% reduction) in the presence of wind31.
Our study investigated the potential factors affecting Tc bias for the prototype device. It pointed out a significant dependence on the time of exposure and on the interaction between time and Ta. Tc bias exhibited also a strong dependence on the probe, highlighting a variability in the production of the probes, production which was manually accomplished at this prototypal stage. Together with the observation of points with positive bias suggesting a wrong calibration (Fig. 3, panels A), the dependence of bias on the probe suggests the need to standardize and automatize the procedures for sensor assessment, calibration, and integration to achieve serial production of the device. The accuracy of Tc measurements did not show a significant dependence on the distance from the tympanic membrane, at least in the measured distance range (within 13 mm). The presence of Tc gradients within the ear canal was previously demonstrated using a customized curved ear probe that synchronously measured Tc at increasing distance from the tympanic membrane. The magnitude of the gradient decreased as Ta increased and in the presence of direct radiation on the probe33. This effect was probably reduced in our measurements thanks to the effect of insulation, that helped to create more homogeneous and stable thermal conditions within the ear canal, as suggested by previous studies in the case of a cool “buffer zone”32.
In view of a multiparametric physiological monitoring with a single device, our study demonstrated also the feasibility of measuring HR and SpO2 by integration of an optical sensor within the probe. The ear canal has been suggested as a suitable site for HR and SpO2 measurement by means of a photo-plethysmographic approach, due to the mild sympathetic nerve activity and the maintenance of perfusion and blood flow even in the cold, which should be associated with a higher quality of photo-plethysmographic signals and reliability of HR and SpO2 parameters13. Consistently, we did not find any significant performance dependence on Ta for HR nor SpO2. The mean HR bias in our study ranged from + 1.1 to + 5.3 bpm, with high CCC values (0.81–0.97) maintained even in the harsh environment conditions. The SpO2 bias ranged from − 0.32 to − 1.42% even in harsh conditions. Only a few recent studies showed the possibility of a multisensor physiological monitoring from the ear canal, but they were all conducted under normal environmental conditions19,21. Combined Tc and HR were monitored in patients during non-cardiac surgery19, while Tc, HR, SpO2, and respiratory rate were remotely monitored in high-risk Covid-positive patients in domestic isolation21. The capability of in-ear devices based on photoplethysmography to measure HR was previously demonstrated at normal Ta under rest and exercise conditions12,14,15,19,34. Bias values in previous studies were slightly lower than the ones observed in our study, ranging between − 0.40 and 0.80 bpm during rest or low intensity exercise12,14,15,34. The performance of in-ear SpO2 measurements under challenging conditions inducing vasoconstriction, such as cold exposure, was previously analyzed by Budidha and Kyriacou13,35, who demonstrated that PPG signal quality and amplitude were minimally affected by vasoconstriction, while reference measurements performed on the fingertip were significantly impaired by the reduced blood flow. Venema et al. performed in-ear SpO2 measurements during induced hypoxic conditions and compared them to gold standard data from blood gas analysis. Good agreement (r2 = 0.96; mean squared error = 3.15) was observed, provided that a single-point subject-specific calibration was applied36. One third of our tests showed malfunctioning of the optical sensor, leading to intermittent functioning or unreliable HR values (see Supplementary Material).
These limitations suggest the necessity of corrective measures both at the hardware and software levels to improve photo-plethysmographic signal quality and physiological parameter assessment. Hardware improvements may rely on the optimization of sensor placement on the in-ear probe and better sizing, fixing, and orientation of the probe within the ear-canal, to maximize signal-to-noise ratio. In terms of software improvements, direct analysis of raw photo-plethysmographic signals (instead of using SpO2 and HR values calculated by the sensor hub) may be performed, taking advantage of accelerometer-based motion artifact removal and noise cancellation techniques, as well as optimized peak detectors9,37,38,39. On the other hand, the presence of a time-dependence for HR measurements (p < 0.001 for time in LMM model, not observed for SpO2 values), with larger HR bias at the beginning of the sessions, may be related to the higher variability and non-stationarity of HR values (caused by the posture change and transfer of the participant between successive test sessions), which was poorly represented by our single-value one-minute sampling. A beat-to-beat assessment of HR monitoring by our device would be advisable in future studies to fully test HR measurement accuracy under different rest and moving conditions.
Analysis of the ENT data and VAS scores showed that the prototype probes caused no harm and were generally well-tolerated by the participants, although they were less comfortable than the commercial probes. The evaluation of the probe insertion by the otoneurologist revealed some limitations in the handiness of the probe, which may complicate procedures when probes are inserted during rescue operations at low temperatures. Improvements of probe materials and further miniaturization should be addressed to improve the probe usability, handiness, and comfortability.
Clinical implications
Although the pulmonary artery or the lower third of the oesophagus remain the gold standard sites for Tc assessment, these sites are impractical in out-of-hospital settings in harsh environments, as well as in conscious patients when they are not sedated1. Our results support previous findings suggesting the ear canal as a promising alternative site to measure Tc in harsh environmental conditions. Tc monitoring has been extensively reported as a pivotal diagnostic parameter for the triage and management of critically ill patients40. Most clinical systems utilize measured or estimated Tc to stage accidental hypothermia and enable appropriate transport and treatment decisions4,41. Tc values are used to identify patients at high risk of cardiac arrest and should be used to estimate the survival probability in patients rewarmed by extracorporeal life support systems4,41. However, field measurements of Tc are imprecise and indirect evaluation based on score systems are not always reflective of the actual Tc41. Although further insulation improvements may be necessary to grant accuracy at very low Ta and over long periods, our device demonstrated higher accuracy than the available commercial probes and potential to help filling this technological gap. The use of our device may lead to an improved diagnosis and staging of primary or secondary hypothermia3,42, such as patients found outdoor or the elderly with preexisting pathologies, who may develop hypothermia even indoors. As well, the device may be applied for Tc management in trauma patients40, such as polytrauma and bleeding ones, at risk for developing hypovolemic shock43,44. Although the device was designed with selective advantage for the out-of-hospital setting, it may find use also for in-hospital Tc monitoring, such as in the clinical management of patients after cardiac arrest45, perioperative Tc monitoring46, and therapeutic hypothermia management47.
The possibility of a combined measure of Tc, SpO2 and HR in a single portable, non-invasive device, may also help improving risk estimation related to hypoxemia and cardiovascular instability, as well as to determine an optimal oxygen therapy target in agreement with International Liaison Committee on Resuscitation (ILCOR) priorities6.
Study limitations
This pilot feasibility study was performed on a small number of healthy and normothermic participants during acute exposure to cold environment. Thus, it may be underpowered to detect subtle variations in device performance and its results cannot be directly extended to a hypothermic state that may affect blood flow and peripheral circulation2,48, to a hyperthermic state, nor to patients with anatomo-vascular alterations following major ear surgery and to patients with tympanic membrane perforation49. Such conditions should be further addressed by testing the device in controlled clinical settings. The study focused primarily on a thorough assessment of Tc measure, whereas we only provided a proof-of-concept of the feasibility of SpO2 and HR monitoring, without using specific maneuvers to alter SpO2 and HR values or adopting gold standard reference (i.e., blood gas analysis and electrocardiogram). Our study also revealed problems related with the stability and accuracy of measurements, especially for SpO2 and HR, with unstable measurements in 17% of the participants and inaccurate HR measurements in an additional 17%. After optimization of the probe based on the current data, the device should thus be tested under simulated hypoxic conditions at rest and under exercise providing a beat-to-beat assessment of the performance. For safety reasons, the probe was inserted by an experienced ENT physician at normal Ta at the beginning of the study, and it was kept in place until the completion of the experimental sessions. Future studies should investigate the potential bias introduced by variability factors related to probe insertion, considering health care provider skills, the participant’s position50, and the effects of different environmental conditions (e.g. wind and snow) at the time of insertion.
Conclusions
This randomized, controlled, crossover pilot study demonstrated that a novel prototype device for measuring vital parameters in a cold environment yielded reliable Tc measurements with an average bias of less than 1 °C, except after 15 min of exposure at − 10 °C ambient temperature. The measurement of SpO2 and HR in the ear canal was feasible, although measurement stability needs further optimization. Through non-invasive and accurate monitoring of vital parameters from the ear canal our prototype may offer support in triage and treatment of critically ill patients in harsh out-of-hospital conditions.
Data availability
Data is available upon reasonable request to the corresponding author.
Abbreviations
- ASA:
-
American society of anesthesiology
- CI:
-
Confidence interval
- CONSORT:
-
Consolidated standards of reporting trials
- ENT:
-
Ear–nose–throat
- HR:
-
Heart rate
- ILCOR:
-
International liaison committee on resuscitation
- LMM:
-
Linear mixed models
- NTC:
-
Negative-temperature-coefficient
- SpO2 :
-
Oxygen saturation
- Ta:
-
Ambient temperature
- Tc:
-
Core body temperature
- VAS:
-
Visuo-analog scale
References
Strapazzon, G., Procter, E., Paal, P. & Brugger, H. Pre-hospital core temperature measurement in accidental and therapeutic hypothermia. High Alt. Med. Biol. 15, 104–111 (2014).
Paal, P. et al. Accidental hypothermia-an update: The content of this review is endorsed by the International Commission for Mountain Emergency Medicine (ICAR MEDCOM). Scand J. Trauma Resusc. Emerg. Med. 24, 111 (2016).
Pasquier, M. et al. On-site treatment of avalanche victims: Scoping review and 2023 recommendations of the international commission for mountain emergency medicine (ICAR MedCom). Resuscitation. 184, 109708 (2023).
Lott, C. et al. European Resuscitation Council Guidelines 2021: Cardiac arrest in special circumstances. Resuscitation. 161, 152–219 (2021).
Hanning, C. D. & Alexander-Williams, J. M. Pulse oximetry: A practical review. BMJ. 311, 367–370 (1995).
Kleinman, M. E. et al. ILCOR scientific knowledge gaps and clinical research priorities for cardiopulmonary resuscitation and emergency cardiovascular care: A consensus statement. Resuscitation. 127, 132–146 (2018).
Hollenberg, S. M. Hemodynamic monitoring. Chest. 143, 1480–1488 (2013).
Sumann, G. et al. Multiple trauma management in mountain environments - a scoping review: Evidence based guidelines of the International Commission for Mountain Emergency Medicine (ICAR MedCom). Intended for physicians and other advanced life support personnel. Scand. J. Trauma Resusc. Emerg. Med. 28, 117 (2020).
Masè, M., Micarelli, A. & Strapazzon, G. Hearables: New perspectives and pitfalls of in-ear devices for physiological monitoring. A scoping review. Front. Physiol. 11, 568886 (2020).
Strapazzon, G. et al. Influence of low ambient temperature on epitympanic temperature measurement: A prospective randomized clinical study. Scand. J. Trauma Resusc. Emerg. Med. 23, 90 (2015).
Webb, R. K., Ralston, A. C. & Runciman, W. B. Potential errors in pulse oximetry. II. Effects of changes in saturation and signal quality. Anaesthesia. 46, 207–212 (1991).
Poh, N. & Kittler, J. A unified framework for biometric expert fusion incorporating quality measures. IEEE Trans. Pattern Anal. Mach. Intell. 34, 3–18 (2012).
Budidha, K. & Kyriacou, P. A. The human ear canal: Investigation of its suitability for monitoring photoplethysmographs and arterial oxygen saturation. Physiol. Meas. 35, 111–128 (2014).
Leboeuf, S. F., Aumer, M. E., Kraus, W. E., Johnson, J. L. & Duscha, B. Earbud-based sensor for the assessment of energy expenditure, HR, and V̇O2max. Med. Sci. Sports Exerc. 46, 1046–1052 (2014).
Bunn, J., Wells, E., Manor, J. & Webster, M. Evaluation of earbud and wristwatch heart rate monitors during aerobic and resistance training. Int. J. Exerc. Sci. 12, 374–384 (2019).
Benzinger TH, Taylor GW. CRANIAL MEASUREMENTS OF INTERNAL TEMPERATURE IN MAN [Internet]. 1963 [cited 2023 Oct 10]. Available from: https://ntrs.nasa.gov/citations/19630009226
Azudin, K., Gan, K. B., Jaafar, R. & Ja’afar, M. H. The principles of hearable photoplethysmography analysis and applications in physiological monitoring—A review. Sensors (Basel). 23, 6484 (2023).
Ne, C. K. H., Muzaffar, J., Amlani, A. & Bance, M. Hearables, in-ear sensing devices for bio-signal acquisition: A narrative review. Expert. Rev. Med. Devices. 18, 95–128 (2021).
Ellebrecht, D. B., Gola, D. & Kaschwich, M. Evaluation of a wearable in-ear sensor for temperature and heart rate monitoring: A pilot study. J. Med. Syst. 46, 91 (2022).
Davies, H. J., Williams, I., Peters, N. S. & Mandic, D. P. In-ear SpO2: A tool for wearable, unobtrusive monitoring of core blood oxygen saturation. Sensors (Basel). 20, 4879 (2020).
Wurzer, D. et al. Remote monitoring of COVID-19 positive high-risk patients in domestic isolation: A feasibility study. PLoS One. 16, e0257095 (2021).
Schilk, P., Dheman, K., & Magno, M. VitalPod: A low power in-ear vital parameter monitoring system. In 2022 18th International Conference on Wireless and Mobile Computing, Networking and Communications (WiMob) [Internet]. 94–99 (2022). cited 3 Jun 2024. https://ieeexplore.ieee.org/document/9941646
Schulz, K. F., Altman, D. G., Moher, D., CONSORT Group. CONSORT 2010 statement: Updated guidelines for reporting parallel group randomised trials. BMJ. 340, c332 (2010).
Doyle, D.J., Hendrix, J.M., & Garmon, E.H. American Society of Anesthesiologists Classification. StatPearls [Internet]. Treasure Island (FL). (StatPearls Publishing, 2023) [cited 28 Jun 2023]. Available from: http://www.ncbi.nlm.nih.gov/books/NBK441940/
Julious, S. A. Sample size of 12 per group rule of thumb for a pilot study. Pharm. Stat. 4, 287–291 (2005).
Alessandrini, M., Viziano, A., Roselli, L. & Micarelli, A. Surgical treatment of otosclerosis leading to changes in postural control and quality of life. Laryngoscope. 130, 2448–2454 (2020).
Madell, J. R. & Gendel, J. M. Earmolds for patients with severe and profound hearing loss. Ear Hear. 5, 349–351 (1984).
Foo, J. Y. A., Chua, K. P. & Tan, X. J. A. Clinical applications and issues of oxygen saturation level measurements obtained from peripheral sites. J. Med. Eng. Technol. 37, 388–395 (2013).
Pasquier, M. et al. Esophageal temperature measurement. N. Engl. J. Med. 383, e93 (2020).
Nagano, C. et al. Technique for continuously monitoring core body temperatures to prevent heat stress disorders in workers engaged in physical labor. J. Occup. Health. 52, 167–175 (2010).
Teunissen, L. P. J., De Haan, A., De Koning, J. J., Clairbois, H. E. & Daanen, H. A. M. Limitations of temperature measurement in the aural canal with an ear mould integrated sensor. Physiol. Meas. 32, 1403–1416 (2011).
Muth, C.-M. et al. Infrared ear thermometry in water-related accidents-not a good choice. J. Emerg. Med. 38, 417–421 (2010).
Yeoh, W. K. et al. Re-visiting the tympanic membrane vicinity as core body temperature measurement site. PLoS ONE. 12, e0174120 (2017).
Passler, S., Müller, N., & Senner, V. In-ear pulse rate measurement: A valid alternative to heart rate derived from electrocardiography? Sensors (Switzerland) [Internet]. (2019);19. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-85071441740&doi=10.3390%2fs19173641&partnerID=40&md5=270b59e497dc957d7e2136badac0a70b
Budidha, K. & Kyriacou, P. A. In vivo investigation of ear canal pulse oximetry during hypothermia. J. Clin. Monit. Comput. 32, 97–107 (2018).
Venema, B. et al. Advances in reflective oxygen saturation monitoring with a novel in-ear sensor system: Results of a human hypoxia study. IEEE Trans. Biomed. Eng. 59, 2003–2010 (2012).
Poh, M.-Z., Swenson, N. C. & Picard, R. W. Motion-tolerant magnetic earring sensor and wireless earpiece for wearable photoplethysmography. IEEE Trans. Inf. Technol. Biomed. 14, 786–794 (2010).
Marsili, I. A. et al. Implementation and validation of real-time algorithms for atrial fibrillation detection on a wearable ECG device. Comput. Biol. Med. 116, 103540 (2020).
Gutiérrez-Rivas, R., García, J. J., Marnane, W. P. & Hernández, Á. Novel real-time low-complexity QRS complex detector based on adaptive thresholding. IEEE Sens. J. 15, 6036–6043 (2015).
Rauch, S. et al. Pre-hospital times and clinical characteristics of severe trauma patients: A comparison between mountain and urban/suburban areas. Am. J. Emerg. Med. 36, 1749–1753 (2018).
Musi, M. E. et al. Clinical staging of accidental hypothermia: The Revised Swiss System: Recommendation of the International Commission for Mountain Emergency Medicine (ICAR MedCom). Resuscitation. 162, 182–187 (2021).
Strapazzon, G., Forti, A., Rauch, S. & Brugger, H. The integration of prehospital standard operating procedures and in-hospital HOPE score for management of hypothermic patients in cardiac arrest. Resuscitation. 141, 212–213 (2019).
van Veelen, M. J. & Brodmann, M. M. Hypothermia in Trauma. Int. J. Environ. Res. Public Health. 18, 8719 (2021).
Blasco Mariño, R., González Posada, M. Á., Soteras Martínez, I. & Strapazzon, G. Considerations in hypothermia and polytrauma patients. Injury. 52, 3543–3544 (2021).
Elmer, J. & Callaway, C. W. Temperature control after cardiac arrest. Resuscitation. 189, 109882 (2023).
Sessler, D. I. Perioperative thermoregulation and heat balance. Lancet. 387, 2655–2664 (2016).
Masè, M., Micarelli, A., Falla, M., Regli, I. B. & Strapazzon, G. Insight into the use of tympanic temperature during target temperature management in emergency and critical care: A scoping review. J. Intensive Care. 9, 43 (2021).
Paal, P., Brugger, H. & Strapazzon, G. Accidental hypothermia. Handb. Clin. Neurol. 157, 547–563 (2018).
Tasli, H. & Gökgöz, M. C. Does central tympanic membrane perforation affect infrared tympanic thermometer measurements in adults?. J. Otol. 13, 128–130 (2018).
Lorr, D., Lund, A., Fredrikson, M. & Secher, N. H. Tympanic membrane temperature decreases during head up tilt: Relation to frontal lobe oxygenation and middle cerebral artery mean blood flow velocity. Scand. J. Clin. Lab. Investig. 77, 587–591 (2017).
Acknowledgements
We would like to thank the other co-inventors of MedSENS from KERR S.r.l. (Andrea Stona, Mattia Vinante and Lijun Chen) and Minnova Med (Michaela Egebrecht) for having provided MedSENS prototypes and for technical support during the study, and Diane Martinelli and Miriam Gottardi for organizational support. We would like to thank Oberalp S.p.A—Bolzano for having provided the thermal clothing used in the study and the Department of Innovation, Research, University and Museums of the Autonomous Province of Bolzano for having covered the open access publication costs.
Funding
The research leading to these results has received funding from the FESR Program 2014–2020 of the Autonomous Province of Bolzano – Alto Adige, under Grant Agreement [513/2019]/Project number [FESR 1114], [Development of innovative sensors for monitoring vital parameters in emergency medicine, MedSENS].
Author information
Authors and Affiliations
Contributions
HB and GS conceived the idea. MM, AM, and GS designed the study. MM, AM, GR, MF, MJvV, ET, and GS collected the research data. MM and TDC conducted the statistical analysis. MM, AM, GR, MF, MJvV, ET, HB, and GS interpreted the results. MM, AM, and GS wrote the first draft of the manuscript. All authors critically revised the manuscript and gave final approval.
Corresponding author
Ethics declarations
Competing interests
MM, AM, HB and GS are inventors of the patents EP 4265177 and WO 2023202894. All the other authors have no conflict of interest to declare.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Masè, M., Micarelli, A., Roveri, G. et al. Vital parameter monitoring in harsh environment by the MedSENS in-ear multisensor device. Sci Rep 14, 19117 (2024). https://doi.org/10.1038/s41598-024-68936-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-68936-0
- Springer Nature Limited