Abstract
The role of nutritional status as a prognostic factor in patients with Sjögren’s syndrome-associated interstitial lung disease (SjS-ILD) is currently unclear. This study aimed to predict the prognosis of patients with SjS-ILD through their nutritional status assessment. In this retrospective observational study, nutritional status was evaluated at the time of diagnosis using body mass index (BMI) and nutritional markers such as controlling nutritional status (CONUT), the Glasgow prognostic score (GPS), and prognostic nutrition index (PNI) for all participants. Receiver operating characteristic (ROC) analyses were performed using BMI and each nutritional marker data to compare the area under the ROC curve (AUC) and find the cutoff value using the maximum Youden index. Kaplan–Meier analysis and Cox proportional hazards regression analysis were performed to predict the prognosis of SjS-ILD patients. A total of 112 SjS-ILD patients were enrolled in the study, and 8.9% died during the follow-up period. The median time from diagnosis to follow-up period was 4.2 years. The AUC for PNI was the highest among nutritional markers and BMI, and PNI cutoff value was used to distinguish between the PNI < 47.7 and PNI ≥ 47.7 groups. A statistical difference was observed in the Kaplan–Meier analysis and log-rank test (p = 0.005). In multivariable analyses, PNI < 47.7 (hazard ratio 9.40, 95% confidence interval 1.54–57.21) is associated with increased mortality, suggesting the importance of early nutritional intervention for malnutrition in SjS-ILD patients.
Similar content being viewed by others
Introduction
Sjögren’s syndrome (SjS) is an autoimmune disease characterized by dryness of the eyes and mouth. It is the second highest prevalent systemic autoimmune disease, following rheumatoid arthritis. SjS affects the exocrine glands and has the potential to invade the entire body, leading to various systemic symptoms1,2,3,4. The lungs are also commonly affected in SjS, with its involvement ranging 12–65%5,6,7,8. The most prevalent form of pulmonary involvement is SjS-associated interstitial lung disease (SjS-ILD)9. Interstitial lung disease (ILD) coexistence with SjS is associated with increased mortality rate and elevated prevalence of lung cancer10,11. Therefore, in addition to implementing pharmacological treatment in cases of deterioration in SjS-ILD, clinical demand exists for the exploration and prevention of modifiable exacerbating factors to improve prognosis.
Recent studies have emphasized the importance of nutritional status as a modifiable prognostic factor in patients with idiopathic pulmonary fibrosis (IPF)12,13, a subtype of ILD, showing its association with both hospitalization and mortality in IPF patients14. Regarding patients with SjS-ILD, previous studies have indicated an association between hypoproteinemia, which could potentially be related to the nutritional status of the patients, and mortality11. However, direct investigations exploring the nutritional status as a prognostic factor in SjS-ILD remain scarce.
Several nutritional markers are used in respiratory diseases. Body mass index (BMI) and the prognostic nutrition index (PNI) are used in chronic respiratory diseases14,15,16,17 whereas controlling nutritional status (CONUT) and Glasgow prognostic score (GPS) are frequently used in lung cancer. These markers can be easily applied in clinical settings, as they only require a single blood test or knowledge of height and weight18,19.
Therefore, this study aimed to assess the nutritional status of patients with SjS-ILD through nutritional markers at the time of diagnosis and identify assistance in predicting mortality, serving as a reference for future treatment strategies.
Methods
Study design and population
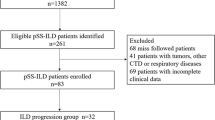
This retrospective single-center observational study was conducted at the Severance hospital in the Republic of Korea. We identified SjS and ILD based on international classification of disease, tenth revision (ICD-10) codes recorded in the electronic medical records (EMR). The study included adult individuals (aged ≥ 19 years) with ICD-10 codes corresponding to SjS (M 35.0), who visited the outpatient clinic or were hospitalized at Severance hospital from January 2005 to December 2020. Figure 1 depicts the process of selecting study participants after the initial enrollment of 8615 patients. We excluded patients with unavailable chest computed tomography (CT) data [n = 8213], those without ILD ICD-10 codes (B22.1, J84.1, J84.18, J84.8, J84.9, J84.10, J98.4, J70.2, J70.9, R91) [n = 247], those who were misdiagnosed as having SjS by the ICD-10 code but did not meet any of the following criteria for SjS diagnosis [n = 40]: American-European Consensus Group 2002 criteria, American College of Rheumatology 2012 criteria, or American College of Rheumatology/European League Against Rheumatism 2016 criteria20,21,22, and those who did not undergo laboratory tests [n = 3] (Fig. 1). As a result, 112 participants were included in the final analysis.
Data collection
Clinico-demographic factors, such as age, sex, BMI, smoking status, comorbidity, treatment types and times, laboratory data, CT images, and pulmonary function test (PFT) data were collected at the time of SjS-ILD diagnosis. If the diagnosis of SjS and ILD was made at different times, the diagnosis of ILD was used as a reference point. The CT interpretations for ILD diagnosis were independently performed by two radiologists blinded to the patient’s clinical status. Furthermore, at least one of the radiologists was a thoracic imaging specialist with experience of over 10 years. We included FVC < 80% as a covariate to represent the patient group with impaired pulmonary function23,24. To assess changes in pulmonary function, we compared follow-up pulmonary function tests conducted 1 year after the initial diagnosis with those conducted within 1 year before and after the diagnosis. The > 10% decrease in PFT was confirmed through the absolute value change of the predicted percentage. Additionally, PFT changes were expressed as slopes obtained by dividing the absolute value change of the predicted percentage by the measured time interval (years). The survival status and cause of death of participants during the follow-up period were confirmed using EMR.
Nutritional markers were obtained through the laboratory data at the time of diagnosis. PNI was calculated following the method elucidated by Onodera et al., using albumin and lymphocyte levels measured from peripheral blood, as shown in the following formula: PNI = 10 × serum albumin level (g/dL) + 0.005 × total lymphocyte count (×103/μL)25. GPS was graded 0–2 based on the range of albumin and C-reactive protein (CRP) levels, whereas CONUT was scored 0–12, considering albumin, total cholesterol, and lymphocyte count18. Both GPS and CONUT scores were closer to normal as they decreased.
Statistical analysis
Categorical variables were compared using the Chi-square and Fisher’s exact tests, whereas continuous variables were evaluated using Student’s t-test and Mann–Whitney U-test. The area under the receiver operating characteristic (ROC) curve (AUC) and the cutoff value by the maximum Youden index were calculated using the ROC curve for each nutritional marker and BMI. The Kaplan–Meier method and log-rank test were used to determine the survival probability and curve. Univariable and multivariable analyses using Cox proportional hazards regression model were performed to compare the prognostic value for each variable. For nutritional markers, we selected the one with the highest AUC and compared it to other variables. In the multivariable analysis, the confounding factors used were identified through clinical evidence and confirmed through a directed acyclic graph (DAG) (Supplementary Fig. 1). Two models were employed in the multivariable analysis. Model 1 were adjusted for age and sex. In model 2, adjustments were made for potentially confounding variables using a DAG, including age, sex, history of smoking, tuberculosis (TB), cancer, BMI, FVC < 80%, and CRP. We depicted the change in hazard ratio according to PNI variation using a restricted cubic spline curve (3 knots) on a graph. Statistical significance was defined as a p-value ≤ 0.05. All statistical analyses were performed using SPSS (IBM corp. Armonk, NY, USA, Ver. 26.0) and R software (R Foundation for Statistical Computing, Vienna, Austria, Ver. 4.2.1). The DAG was constructed using Dagitty (v.3.0; http://www.dagitty.net/).
Ethics statements
The study protocol was reviewed and approved by the Institutional Review Board of the Severance Hospital Ethics Committee (IRB approval number: 4-2022-0775). Informed consent was waived by the Institutional Review Board of the Severance Hospital Ethics Committee. All methods were performed in accordance with the Declaration of Helsinki.
Results
Baseline characteristics
A total of 112 patients with SjS-ILD were enrolled in the final analysis. The baseline characteristics and descriptive comparison between survivors and non-survivors are shown in Table 1. The median age of the total participants was 63.8 (57.0–76.0) years, and 83.9% were female. Among the total participants, 8.9% (n = 10) died during the follow-up period. Pneumonia (n = 8) was the main cause of death, with myocarditis (n = 2) as another contributing factor. In the non-survivor group, there was a higher proportion of males and a history of smoking, along with lower albumin levels and higher CRP and erythrocyte sedimentation rate (ESR). The median and quartile values of the nutritional markers such as CONUT, GPS, and PNI were within or adjacent to the normal range in the entire patient population and among the survivors. Whereas, in the non-survivor group, they exhibited values outside the normal range, indicating a relatively poorer nutritional status compared to that of the survivors18,26. There were no statistically significant differences between the two groups regarding the proportion of abnormal lung function, annual pulmonary function change, and CT patterns. However, when considering the change in pulmonary function over the entire follow-up period, there was a statistically significant higher rate of more than 10% FVC decline in the non-survivor group. The median follow-up duration for SjS-ILD was 4.2 years in total participants. SjS diagnosed before ILD accounted for 59.8% of total participants, exceeding the 33.9% diagnosed after ILD, with concurrent diagnoses at 6.3%. We additionally investigated the differences between primary and secondary SjS-ILD patients; however, we did not find any significant statistical differences in the other variables, except for BMI and treatment times ≥ 1 (Supplementary Table S1).
Cutoff value for PNI and comparison between patients with PNI < 47.7 and PNI ≥ 47.7
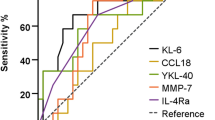
The AUC and a cutoff value for BMI and nutritional markers were analyzed using the ROC curve. Among BMI and nutritional markers, PNI had the highest AUC of 0.753 (Supplementary Table S2). The optimal cutoff value of PNI was 47.7, with 80.0% sensitivity and 62.7% specificity, as illustrated in Fig. 2. Based on this, the PNI cutoff value was used to distinguish between the PNI < 47.7 and PNI ≥ 47.7 groups.
Table 2 presents a comparison between the PNI < 47.7 and PNI ≥ 47.7 groups, revealing that 41.1% of the total participants were classified into the PNI < 47.7 group. BMI, lymphocyte count, hemoglobin, and albumin levels were lower in the PNI < 47.7 group compared with in the PNI ≥ 47.7 group, whereas CRP and ESR level, CONUT, and GPS were higher. For baseline lung function, the PNI < 47.7 group showed a higher proportion of abnormal FVC and forced expiratory volume in 1 s compared to the PNI ≥ 47.7 group. However, there were no differences between the two groups in terms of changes in PFT. Figure 3 presents the results of the Kaplan–Meier analysis and log-rank test conducted for the two groups, demonstrating a significant association between PNI < 47.7 and poor prognosis (p = 0.005). Additionally, we investigated Kaplan–Meier curves for the PNI divided into 3 groups (based on PNI values at 25% and 75%) and 4 groups (based on PNI values at 10%, 50%, and 90%). The results are depicted in Supplementary Fig. 2. Both the 3-group and 4-group exhibited trends similar to those seen in Fig. 3.
Univariable and multivariable analyses of PNI
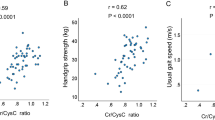
Table 3 presents the association between PNI < 47.7 and mortality in SjS-ILD patients, as determined using the Cox proportional hazards regression model. In the univariable analysis, female sex (hazard ratio [HR] 0.17, 95% confidence interval [CI] 0.05–0.58) was associated with decreased mortality, while smoking (HR 5.75, 95% CI 1.60–20.67) and PNI < 47.7 (HR 6.83, 95% CI 1.45–32.3) were associated with increased mortality. In both multivariable analysis model 1 and 2, PNI < 47.7 was associated with mortality in SjS-ILD patients (HR 9.40, 95% CI 1.54–57.21, model 2). To explore the hazard ratio not only for PNI < 47.7 but also for PNI ≥ 47.7, we investigated the variation of hazard ratio across the entire PNI range and depicted this in Fig. 4. In the covariate-adjusted Fig. 4B, within the PNI < 47.7 range, the hazard ratio increases as PNI decreases, but there was no statistically significant relationship between PNI variation and hazard ratio within the PNI ≥ 47.7 range.
Discussion
This study investigates the potential of utilizing the PNI as an indicator reflecting nutritional status to assess the prognostic value of nutritional status in SjS-ILD patients at the time of diagnosis. We found that PNI < 47.7 at the time of diagnosis was significantly associated with all-cause mortality in patients with SjS-ILD. In contrast, the correlation between changes in PNI and mortality was not clear when PNI was ≥ 47.7.
The prevalence of SjS-ILD varies in the literature, ranging 12–65%5,6,7,8, and this variability may be attributed to the possible existence of asymptomatic patients. In a study by Uffmann et al., the results of CT scans conducted on asymptomatic SjS patients revealed ILD in 65% of the cases8. Similarly, Li et al. found that among patients with ILD detected using imaging study, only 62.1% exhibited respiratory symptoms27. These findings indicate a substantial proportion of asymptomatic SjS-ILD cases. In our study, the prevalence of SjS-ILD among SjS patients who underwent CT scans was 31.8%. However, since CT scans were predominantly conducted on SjS patients with respiratory symptoms, the actual prevalence was possibly higher than these results. The cumulative incidence of ILD in patients with SjS is reported to be 3% and 4% at 10 and 20 years, respectively, after SjS diagnosis28. Nonetheless, for the same reasons, the actual incidence rate might have been underestimated.
The presence of ILD in SjS patients is crucial because coexisting ILD significantly influences the prognosis. In contrast to the 5-year survival rate of 96% in SjS patients10, SjS-ILD exhibits a lower 5-year survival rate, ranging 81.1–88.5%29,30. Moreover, the duration from SjS-ILD diagnosis to death is approximately 9 years31. In our study, the 5-year survival rate was 97.8% in the PNI ≥ 47.7 group and 80.0% in the PNI < 47.7 group. These findings indicate that the PNI ≥ 47.7 group exhibited a survival rate similar to SjS patients without ILD, suggesting that PNI ≥ 47.7 is associated with a reduced adverse prognostic impact of ILD. Therefore, while treatment during exacerbation is essential, there is also a need to proactively manage nutritional status before exacerbation to reduce risk factors.
In chronic respiratory diseases, the frequency of malnutrition is high. Approximately 19–38% of patients with IPF experience malnutrition32,33,34, whereas the prevalence of malnutrition ranges from 30 to 60% among hospitalized chronic obstructive pulmonary disease (COPD) patients35. In our study, the prevalence of malnutrition according to PNI < 47.7 in SjS-ILD patients was 41.1%. The PNI cutoff value of 47.7 is comparable to the 2.5th percentile in the PNI distribution among healthy individuals. In Yang et al.’s study, the median PNI at the 2.5th percentile for individuals aged 40–65 was 49.4, and for those aged 65–79, it was 48.126. In another study that determined the cutoff value for PNI as a predictive factor for exacerbation in COPD, the PNI value was also found to be 48.8517. These results aided in determining the value of our study’s cutoff. Considering the studies that have shown an association between malnutrition and mortality in chronic respiratory diseases36,37, we suggest the need to consider malnutrition as a prognostic factor in patients with SjS-ILD.
Low FVC has been considered an indicator of poor prognosis in SjS-ILD29, and in the findings of this study, the relatively decreased lung function at the diagnosis in the PNI < 47.7 group corresponds to the higher mortality observed in this group. Moreover, the lack of statistical difference in lung function changes between the two groups aligns with other research findings38. Malnutrition can be associated with the destruction of lung parenchyma39, a decrease in surfactant and elastic fiber content40, and respiratory muscle weakness41, leading to impaired lung function due to reduced ventilatory drive42. These previous results support the finding of relatively decreased lung function at the diagnosis in the PNI < 47.7 group compared with the PNI ≥ 47.7 group.
The interaction between inflammation, lung function, and malnutrition is intricately linked to the progression of chronic pulmonary diseases and exerts a significant impact on mortality. Among these factors, malnutrition is anticipated as a pivotal prognostic determinant, a notion supported by the study conducted by Chen YH et al.43 In the research, patients with progressive fibrosing interstitial lung disease (PF-ILD) exhibited lower 3-year overall survival compared to non-PF-ILD patients, and it was confirmed that albumin levels, one of the indicators reflecting nutritional status, were consistently lower. Additionally, low albumin levels were found to be associated with PF-ILD in multivariate logistic regression analysis, and a decrease in DLco was observed in the PF-ILD group at 12 months compared to baseline. Other previous studies have revealed that in mouse experiments, gene expression promoting lung cell regeneration increases after caloric restriction followed by refeeding44. Moreover, in other respiratory conditions such as COPD, nutritional intervention has been observed to improve physical function, decrease lung function deterioration, and reduce inflammation, suggesting the potential benefits of nutritional intervention in SjS-ILD as well45.
To the best of our knowledge, this is the first study to evaluate the nutritional status of SjS-ILD patients. Furthermore, in the context of insufficient evidence-based treatment strategies for selecting treatment or determining the appropriate treatment initiation for SjS-ILD1, we have provided the evidence supporting nutritional intervention as a non-pharmacological treatment to enhance the prognosis of SjS-ILD patients.
However, this study had some limitations. First, this study was conducted at a single center, which might have introduced a geographical bias in the recruitment of patients. Therefore, further research with a large-scale sample size involving multiple institutions or at a national level is needed to address this limitation. Second, because this study was retrospective, it was challenging to completely exclude the influence of uninvestigated comorbidities. Given that the presence of chronic comorbid conditions may impact the nutritional status and mortality rate of SjS-ILD patients, it is believed that future research, such as randomized controlled trials, will be necessary to minimize the influence of comorbidities. Third, there was a shortage of samples from the deceased group, which was unavoidable owing to the relatively low mortality of SjS compared with that of other diseases. There was no statistical difference in pulmonary function between the deceased and surviving groups during diagnosis, although there was a difference in absolute values.
Conclusions
Malnutrition, as indicated by low PNI, at the time of diagnosis is associated with higher mortality rate of SjS-ILD patients. Further research is needed to determine if long-term nutritional interventions from the early stages, aiming to reduce modifiable risk factors, can prevent disease progression.
Data availability
The datasets used or analyzed during the current study are available from the corresponding author on reasonable request.
References
Luppi, F. et al. Lung complications of Sjogren syndrome. Eur. Respir. Rev. https://doi.org/10.1183/16000617.0021-2020 (2020).
Flament, T. et al. Pulmonary manifestations of Sjogren’s syndrome. Eur. Respir. Rev. 25, 110–123. https://doi.org/10.1183/16000617.0011-2016 (2016).
Bowman, S. J., Ibrahim, G. H., Holmes, G., Hamburger, J. & Ainsworth, J. R. Estimating the prevalence among Caucasian women of primary Sjogren’s syndrome in two general practices in Birmingham, UK. Scand. J. Rheumatol. 33, 39–43. https://doi.org/10.1080/03009740310004676 (2004).
Rehman, H. U. Sjogren’s syndrome. Yonsei. Med. J. 44, 947–954. https://doi.org/10.3349/ymj.2003.44.6.947 (2003).
Fauchais, A. L. et al. Immunological profile in primary Sjogren syndrome: Clinical significance, prognosis and long-term evolution to other auto-immune disease. Autoimmun. Rev. 9, 595–599. https://doi.org/10.1016/j.autrev.2010.05.004 (2010).
Kelly, C., Gardiner, P., Pal, B. & Griffiths, I. Lung function in primary Sjogren’s syndrome: A cross sectional and longitudinal study. Thorax 46, 180–183. https://doi.org/10.1136/thx.46.3.180 (1991).
Matsuyama, N. et al. Pulmonary lesions associated with Sjogren’s syndrome: Radiographic and CT findings. Br. J. Radiol. 76, 880–884. https://doi.org/10.1259/bjr/18937619 (2003).
Uffmann, M. et al. Lung manifestation in asymptomatic patients with primary Sjogren syndrome: Assessment with high resolution CT and pulmonary function tests. J. Thorac. Imaging 16, 282–289. https://doi.org/10.1097/00005382-200110000-00009 (2001).
Kreider, M. & Highland, K. Pulmonary involvement in Sjogren syndrome. Semin. Respir. Crit. Care Med. 35, 255–264. https://doi.org/10.1055/s-0034-1371529 (2014).
Brito-Zeron, P. et al. Systemic activity and mortality in primary Sjogren syndrome: Predicting survival using the EULAR-SS disease activity index (ESSDAI) in 1045 patients. Ann. Rheum. Dis. 75, 348–355. https://doi.org/10.1136/annrheumdis-2014-206418 (2016).
Xu, Y. et al. Risk factors for progression and prognosis of primary Sjogren’s syndrome-associated interstitial lung disease in a Chinese population. Int. J. Rheum. Dis. 23, 1734–1740. https://doi.org/10.1111/1756-185X.14023 (2020).
Jouneau, S., Lederlin, M., Vernhet, L. & Thibault, R. Malnutrition in idiopathic pulmonary fibrosis: the great forgotten comorbidity. Eur. Respir. J. 53, https://doi.org/10.1183/13993003.00418-2019 (2019).
Nishiyama, O. et al. Fat-free mass index predicts survival in patients with idiopathic pulmonary fibrosis. Respirology 22, 480–485. https://doi.org/10.1111/resp.12941 (2017).
Jouneau, S. et al. Malnutrition and decreased food intake at diagnosis are associated with hospitalization and mortality of idiopathic pulmonary fibrosis patients. Clin. Nutr. 41, 1335–1342. https://doi.org/10.1016/j.clnu.2022.05.001 (2022).
Rolo Silvestre, C. et al. The nutritional status of chronic obstructive pulmonary disease exacerbators. Can. Respir. J. 2022, 3101486. https://doi.org/10.1155/2022/3101486 (2022).
Kim, C. Y. et al. Usefulness of the preoperative prognostic nutritional index score as a predictor of the outcomes of lung transplantation: A single-institution experience. Clin. Nutr. 38, 2423–2429. https://doi.org/10.1016/j.clnu.2018.10.027 (2019).
Suzuki, E. et al. Prognostic nutritional index (PNI) as a potential prognostic tool for exacerbation of COPD in elderly patients. Int. J. Chron. Obstruct. Pulmon. Dis. 18, 1077–1090. https://doi.org/10.2147/COPD.S385374 (2023).
Lee, S. C. et al. Prediction of postoperative pulmonary complications using preoperative controlling nutritional status (CONUT) score in patients with resectable non-small cell lung cancer. Sci. Rep. 10, 12385. https://doi.org/10.1038/s41598-020-68929-9 (2020).
Zhang, C. L., Fan, K., Gao, M. Q. & Pang, B. Prognostic value of Glasgow prognostic score in non-small cell lung cancer: A systematic review and meta-analysis. Pathol. Oncol. Res. 28, 1610109. https://doi.org/10.3389/pore.2022.1610109 (2022).
Vitali, C. et al. Classification criteria for Sjogren’s syndrome: A revised version of the European criteria proposed by the American-European consensus group. Ann. Rheum. Dis. 61, 554–558. https://doi.org/10.1136/ard.61.6.554 (2002).
Shiboski, S. C. et al. American college of rheumatology classification criteria for Sjogren’s syndrome: A data-driven, expert consensus approach in the Sjogren’s international collaborative clinical alliance cohort. Arthritis Care Res. 64, 475–487. https://doi.org/10.1002/acr.21591 (2012).
Shiboski, C. H. et al. 2016 American College of rheumatology/European league against rheumatism classification criteria for primary Sjogren’s syndrome: A consensus and data-driven methodology involving three international patient cohorts. Ann. Rheum. Dis. 76, 9–16. https://doi.org/10.1136/annrheumdis-2016-210571 (2017).
Barreiro, T. J. & Perillo, I. An approach to interpreting spirometry. Am. Fam. Phys. 69, 1107–1114 (2004).
Richeldi, L. et al. Relative versus absolute change in forced vital capacity in idiopathic pulmonary fibrosis. Thorax 67, 407–411. https://doi.org/10.1136/thoraxjnl-2011-201184 (2012).
Onodera, T., Goseki, N. & Kosaki, G. Prognostic nutritional index in gastrointestinal surgery of malnourished cancer patients. Nihon Geka Gakkai Zasshi 85, 1001–1005 (1984).
Yang, G. et al. Normal reference intervals of prognostic nutritional index in healthy adults: A large multi-center observational study from Western China. J. Clin. Lab. Anal. 35, e23830. https://doi.org/10.1002/jcla.23830 (2021).
Li, X. et al. Clinical and laboratory profiles of primary Sjogren’s syndrome in a Chinese population: A retrospective analysis of 315 patients. Int. J. Rheum. Dis. 18, 439–446. https://doi.org/10.1111/1756-185X.12583 (2015).
Nannini, C., Jebakumar, A. J., Crowson, C. S., Ryu, J. H. & Matteson, E. L. Primary Sjogren’s syndrome 1976–2005 and associated interstitial lung disease: A population-based study of incidence and mortality. BMJ Open 3, e003569. https://doi.org/10.1136/bmjopen-2013-003569 (2013).
Kim, Y. J., Choe, J., Kim, H. J. & Song, J. W. Long-term clinical course and outcome in patients with primary Sjogren syndrome-associated interstitial lung disease. Sci. Rep. 11, 12827. https://doi.org/10.1038/s41598-021-92024-2 (2021).
Gao, H. et al. Prevalence, risk factors, and prognosis of interstitial lung disease in a large cohort of Chinese primary Sjogren syndrome patients: A case-control study. Medicine 97, e11003, https://doi.org/10.1097/MD.0000000000011003 (2018).
Gao, H. et al. Characteristics and mortality in primary Sjogren syndrome-related interstitial lung disease. Medicine 100, e26777, https://doi.org/10.1097/MD.0000000000026777 (2021).
Jouneau, S. et al. What are the best indicators to assess malnutrition in idiopathic pulmonary fibrosis patients? A cross-sectional study in a referral center. Nutrition 62, 115–121. https://doi.org/10.1016/j.nut.2018.12.008 (2019).
Nakatsuka, Y. et al. The clinical significance of body weight loss in idiopathic pulmonary fibrosis patients. Respiration 96, 338–347. https://doi.org/10.1159/000490355 (2018).
Mochizuka, Y. et al. Geriatric nutritional risk index is a predictor of tolerability of antifibrotic therapy and mortality risk in patients with idiopathic pulmonary fibrosis. Respirology 28, 775–783. https://doi.org/10.1111/resp.14523 (2023).
Collins, P. F., Elia, M. & Stratton, R. J. Nutritional support and functional capacity in chronic obstructive pulmonary disease: a systematic review and meta-analysis. Respirology 18, 616–629. https://doi.org/10.1111/resp.12070 (2013).
Comes, A. et al. Association of BMI and change in weight with mortality in patients with fibrotic interstitial lung disease. Chest 161, 1320–1329. https://doi.org/10.1016/j.chest.2021.11.008 (2022).
Aniwidyaningsih, W., Varraso, R., Cano, N. & Pison, C. Impact of nutritional status on body functioning in chronic obstructive pulmonary disease and how to intervene. Curr. Opin. Clin. Nutr. Metab. Care 11, 435–442. https://doi.org/10.1097/MCO.0b013e3283023d37 (2008).
Davidson, B. K., Kelly, C. A. & Ten Griffiths, I. D. year follow up of pulmonary function in patients with primary Sjogren’s syndrome. Ann. Rheum. Dis. 59, 709–712. https://doi.org/10.1136/ard.59.9.709 (2000).
Massaro, D., Massaro, G. D., Baras, A., Hoffman, E. P. & Clerch, L. B. Calorie-related rapid onset of alveolar loss, regeneration, and changes in mouse lung gene expression. Am. J. Physiol. Lung Cell Mol. Physiol. 286, L896-906. https://doi.org/10.1152/ajplung.00333.2003 (2004).
Dias, C. M. et al. Effects of undernutrition on respiratory mechanics and lung parenchyma remodeling. J. Appl. Physiol. 1985(97), 1888–1896. https://doi.org/10.1152/japplphysiol.00091.2004 (2004).
Fiaccadori, E., Zambrelli, P. & Tortorella, G. Physiopathology of respiratory muscles in malnutrition. Minerva Anestesiol. 61, 93–99 (1995).
Ferrari-Baliviera, E., Pierdominici, S. & Sarcinelli, L. Effects of the nutritional status on the respiratory system. Minerva Anestesiol. 55, 443–450 (1989).
Chen, Y. H. et al. Clinical outcomes and risk factors of progressive pulmonary fibrosis in primary Sjogren’s syndrome-associated interstitial lung disease. BMC Pulm. Med. 23, 268. https://doi.org/10.1186/s12890-023-02562-w (2023).
Massaro, D. et al. Rapid onset of gene expression in lung, supportive of formation of alveolar septa, induced by refeeding mice after calorie restriction. Am. J. Physiol. Lung Cell Mol. Physiol. 292, L1313-1326. https://doi.org/10.1152/ajplung.00146.2006 (2007).
Furulund, E. et al. Effects of nutritional interventions in individuals with chronic obstructive lung disease: A systematic review of randomized controlled trials. Int. J. Chron. Obstruct. Pulmon. Dis. 16, 3145–3156. https://doi.org/10.2147/COPD.S323736 (2021).
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Y.A.K., Y.S.K. and M.S.P. designed the study. S.H.L., S.Y.K., E.Y.K. and J.Y.J. acquired data. E.C., A.W., S.H.Y. and Y.P interpreted data. E.C. and M.S.P. conducted analysis and wrote the main manuscript text. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Chung, E., Woo, A., Yong, S.H. et al. Malnutrition is associated with mortality in Sjögren’s syndrome-associated interstitial lung disease. Sci Rep 14, 17842 (2024). https://doi.org/10.1038/s41598-024-68754-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-68754-4
- Springer Nature Limited