Abstract
Female urethral caruncle is the most common urethral mass in postmenopausal women, yet there is a lack of studies on its imaging. The aim of this study was to provide a summary of the clinical and ultrasound features as well as the precise location of female urethral caruncle. This study reviewed the clinical and ultrasonographic records of 20 consecutive women with pathologically confirmed urethral caruncle. Data on patient demographics, symptoms, and transperineal and transrectal ultrasound imaging features, including location, shape, margin, size, blood flow, and inner echo of the caruncle, were extracted. Each patient presented with only one mass at the urethral meatus. Most caruncles were located on the posterior lip (75%) of the urethra, presenting as oval (80%), mixed-echoic (50%), or hypo-echoic (40%) nodules with abundant linear (40%) or dendritic (60%) blood flow. The average distance between the bladder neck and the cranial end of the masses was 28 mm. Hyper-echogenic spots, cystic echo areas, and macrocalcifications were detected in thirteen caruncles (70%). This study shows that transperineal combined with transrectal ultrasound can be used to assess female urethral caruncle, and its relative location to the urethra can be accurately described, which is helpful for surgeons making preoperative localization and conversations.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
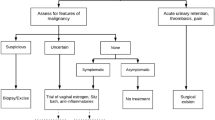
Urethral caruncle (UC) is a benign, polypoid, reddish, and highly vascular lesion that protrudes from the distal urethral mucosa, typically located on the posterior lip of the urethra1. It is often observed in women between 20 and 80 years of age, especially postmenopausal women, and rarely occurs in males and preadolescent girls2,3. Most patients are asymptomatic, making the exact prevalence of UC unclear4,5,6. Some patients will complain of bleeding or hematuria, pain, and dysuria4, but these symptoms are non-specific. Estrogen deficiency and chronic irritation of the urethral mucosa have been hypothesized as the most common predisposing factors6. UC needs to be differentiated from urothelial carcinoma, urethral adenocarcinoma, malignant melanoma, and UC with malignant transformation, which carries a risk of poor prognosis. Cases of malignant urethral tumors misdiagnosed as UC have been reported7,8,9,10. The management of UC, which includes conservative treatment and surgical resection, is controversial at present. While asymptomatic patients require only reassurance and education4, there is no consensus on the appropriate treatment for symptomatic patients.
A comprehensive examination is necessary to distinguish benign and malignant neoplasms on the external urethral meatus. Physical examination can provide a preliminary assessment of a mass located on the urethral meatus, but information about the internal status of mass and its relative position of the urethra is absent. Imaging techniques can compensate for these deficiencies and help with differential diagnoses and treatment planning. There is no recommended protocol for the accurate diagnosis of female urethral lesions, including UC, due to the poorly understanding of the condition4. As a widely available imaging method, studies on the ultrasonographic features of urethral and periurethral masses have been reported11,12. However, to our knowledge, no research has systematically summarized the ultrasonographic characteristics of female UC. The objective of this study was to review and analyze the ultrasonic images of UC, and hopefully to improve the understanding of female UC.
Methods
Patients
The research was conducted in accordance with the 1964 Helsinki Declaration and approved by 2022-KY-170(K) by the Ethics Committee of Shanghai Sixth People's Hospital Affiliated to Shanghai Jiao Tong University School of Medicine. Medical records of female patients who were pathologically diagnosed with UC in our center between March 2008 and April 2023 were retrospectively extracted. Among the patients, preoperative ultrasound (US) examinations were done in 20 patients. The demographics and ultrasound information were retrieved from the database. Written informed consent was obtained from the participants.
Ultrasonography
All the patients were examined using sonography with the HA710 US system (Hitachi Medical Corp., Tokyo, Japan) and the Mindray Eagus R9 US system (Mindray Co., Ltd, Shenzhen, China). The preoperative transperineal US was performed with an 8–12 MHz linear array probe, with the patient lying supine in the lithotomy position. The probe was covered with a piece of plastic film containing adequate gel and placed vertically in the center of the perineum, providing a mid-sagittal view of the urethra and peri-urethral tissue (Fig. 1). Besides, biplane transrectal US was performed using a biplane probe (3-9 MHz convex array and 4–13 MHz linear array) in eighteen women positioned in the left lateral decubitus position. The probe was covered with a condom containing a small amount of gel. The number, location, size, shape, margin, echogenicity, and color Doppler flow information (CDFI) of the mass were recorded on the transperineal US, and the distance between the bladder neck and the cranial end of the mass was measured on the transrectal US. The same examiner interpreted all the US features.
The location of the mass was recorded as being on the anterior or posterior lip of the urethra, or surrounding the urethra. The shape was classified on a sagittal section as oval or Y- shaped. The hemodynamics were assessed using CDFI, and Adler grading13 was adopted to record the degree of blood flow signals in the lesion.
Results
Clinical features
The mean age of the patients was 68 years (range: 53–80 years). All patients were discovered with a polypoid, dark red lesion at the urethral meatus. Pelvic floor organ prolapse was found in two women. Presenting complaints included hematuria (50%), pain (35%), urinary frequency/urgency (20%), and dysuria (10%). Eight (40%) patients were asymptomatic. Eighteen (90%) women underwent surgical excision, and two (10%) patients underwent biopsy. Pathological examinations of the twenty lesions revealed UC, with four (20%) cases showing focal urethritis glandularis, and one (5%) case displaying mild to moderate focal atypia of squamous epithelium.
US features
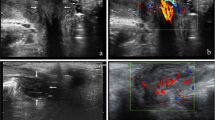
The ultrasonographic features for all participants are listed in Table 1. In all twenty female patients, a sole lesion was found at the urethral meatus, with fifteen (75%) cases located on the posterior lip of the urethra, four (20%) cases surrounding the urethra, and only one (5%) case on the anterior lip of the urethra. The distance between the bladder neck and the cranial end of the mass was detected in eighteen women, but two cases could not be revealed due to the gap between the probe to the urethral meatus. The average distance was 28 mm, ranging from 20 to 31 mm (Fig. 2a,c). The maximal diameter of the masses ranged from 8 to 32 mm, with a median of 17 mm. The neoplasms presented as oval nodules, except for four (20%) caruncles that surrounded the urethra with a Y-shape (Fig. 2b,d). In addition, thirteen (65%) masses showed unclear margins. The echogenicity of caruncles included hypo-echoic (40%), mixed echogenicity (50%), and iso-echoic (10%). Furthermore, thirteen masses showed hyper-echogenic spots (65%), two (10%) masses exhibited small cystic echo areas, and macrocalcifications were found in one (5%) case (Fig. 3a,b,c). Moderate (35%) or marked (65%) blood flow signals by CDFI were detected in all masses. The vascular morphology observed included dendritic (60%) and linear (40%) patternss (Fig. 4). Histologically, UC with focal urethritis glandular and atypia of squamous epithelium did not exhibit apparent differences on ultrasonic images in our study.
Location and shape of the UC in the sagittal section on transrectal (a, c) and transperineal US (b, d). (a) The distance between the bladder neck to the cranial end of the UC was 28 mm. (b) An oval hypoechoic lesion on the posterior lip of the urethra with a clear margin. (c) The distance between the bladder neck to the cranial end of the UC was 22 mm. (d) A “Y” shape-like mixed-echoic lesion surrounding the urethra. U = urethra; V = vaginal; PS = pubic symphysis; BN = bladder neck; The dotted line indicates the distance between the bladder neck to the cranial end of the UC; Arrows indicate the mass boundary.
The component of UC detected on US (a, b, c) and pathological sections (d, e, f). (a) Hyper-echogenic spots. (b) Small cystic echo areas. (c) A circular macrocalcification. (d, e, f) Pools of blood with organized thrombus, dilated vessels, fibrosis, and cystic or glandular luminal spaces. U = urethra; PS = pubic symphysis; Arrows indicate the mass boundary.
The CDFI of UC detected in the sagittal section on transperineal (a, b) and transrectal (c) US. (a) Dendritic vascular. (b) Linear vessels. (c) Compared with the same caruncle shown in (b), the blood flow was sparse on transrectal US. U = urethra; PS = pubic symphysis; Arrows indicate the mass boundary.
Discussion
UC is the most prevalent mass on the female urethral meatus14 and is occasionally discovered during gynecological examination. The majority of caruncles are typically situated on the posterior lip of the urethra in postmenopausal women and are generally asymptomatic or present with nonspecific symptoms15,16, which is consistent with our results. Detailed reviews of neoplasms on urethral meatus, including physical examination, imaging techniques, urethrocystoscopy, and even biopsy, are essential for excluding malignant neoplasms4,17, although female malignancy urethral tumors are exceptionally rare18,19,20. In our study, UC with urethritis glandularis (see Supplementary Fig. S1 online) and mild to moderate atypia squamous epithelium were found, suggesting potential for malignant transformation21. Physical examination is experience-dependent and inadequate for the evaluation of the entire urethra and the inside of mass. Urethrocystoscopy can accurately estimate the positional relationship between mass and urethra and identify any other lesions in the urethra and bladder. However, as an invasive examination, it carries the risk of damaging the urethral mucosa22 and does not aid in evaluating peri-urethral structure. Therefore, imaging examination is necessary for evaluating UC, informing surgical planning, and addressing patient inquiries. Imaging modalities include computed tomography (CT), magnetic resonance imaging (MRI), and ultrasonography. The relatively low spatial resolution of CT limits its utility in assessing the urethra. While MRI offers good spatial resolution and sensitivity in detecting urethral masses, it is costly and not available for patients with metal implants or claustrophobia. High-resolution two-dimensional ultrasound is radiation-free, cost-effective and convenient. Studies have found that US is comparable to MRI in diagnosing urethral lesions23.
Transvaginal, transperineal and transrectal US are available for assessing female urethral and periurethral masses, including UC. Owing to the beam of the probe being parallel to urethra, the urethra mucous cannot be clearly displayed through transvaginal US. Therefore, this approach is inadequate for evaluating urethral mass on urethral meatus, especially UC with a long and slender pedicle extending from the urethra mucosa5. Transrectal US can distinctly distinguish the different layers of urethra and vagina on account of the probe of biplane transrectal US emitting ultrasound perpendicular to the female urethra. It has been widely used in diagnosing female urethral and peri-urethral diseases, such as urethral diverticula, genital fistulas, and peri-urethral solid masses11,24. However, due to the gap between the probe and the external urethral orifice, the mass located in the urethral meatus may not be clearly and completely displayed, and sometimes only part of the cranial structure of the mass can be detected. Therefore, observing a mass located in the urethral meatus solely through the transrectal route is insufficient. Transperineal US using a linear array probe is the most general method to evaluate the lumps on urethral meatus, enabling clear detection of the location, shape, size and vascular signals. Studies have shown that UC predominantly appears as a round or oval hypoechoic solid mass with significant internal blood flow located on the posterior lip of urethra on US11,12. This is similar to the results of our study. However, in this study, 50% of UC showed mixed echogenicity, 40% were hypo-echoic, and hyper-echogenic spots, macrocalcification, and small cystic echo areas were visible. This may be attributed to our study’s larger sample size compared to previous studies, allowing for a more detailed delineation of the internal echo components of UC. Our study classifies the UC with hyper-echogenic spots, macrocalcification, or small cystic echo areas as mixed echogenicity. Pathological sections revealed possible causes of the diverse performance of UC16, including dilation of the subepithelial bold vessels, large blood pools, organized thrombus, fibrosis, and cystic or glandular luminal spaces in the stromal compartment of UC (Fig. 3d,e,f). One caruncle was accompanied by large blood pools and organized thrombus in our study, presenting as a cystic area within the mixed-echoic lesion (see Supplementary Fig. S2 online). However, as the transperineal US is parallel to the urethra with a shallow detection depth, it cannot clearly reveal the entire female urethra. Thus, the use of this method alone will miss the information about the proximal and middle sections of urethra.
Since it is unable to obtain complete US measurements and features of UC using any single approach mentioned above, our center decided to combine transperineal and transrectal US for a comprehensive evaluation of the female urethra and peri-urethra anatomical configuration. Transperineal US was performed first to observe the morphology and CDFI. Subsequently, transrectal US was completed to confirm the location of the mass, determine if additional masses were present in the urethra, and measure the distance between the bladder neck and the cranial end of the mass. In our study, 89% of UC could be detected through transrectal US. This may be attributed to obvious atrophy of the urethra and vagina in some elderly women, resulting in an increased gap between the probe and the external urethral orifice.
The female urethra is a short lumen structure, approximately 4 cm in length25. When the cranial end of UC is close to the internal urethral orifice, surgical eradication of the lump may damage the urethral mucosa, resulting in postoperative urinary incontinence or urethral stenosis26,27. Besides, a UC with a slender root may be neglected during surgery without prior imaging examination or urethrocystoscopy, leading to incomplete removal of the mass. Therefore, the specific location of UC measured by ultrasound before surgery is crucial for surgical plan-making and preoperative communication with patients.
An important strength of our study is that it is the largest study describing the ultrasound characteristics of UC. Besides, we proposed a combination of transperineal and transrectal US to evaluate the mass at the urethral meatus, allowing the obtaining of detailed information about the location of the mass. This study had several limitations. Firstly, because a large number of patients experience no discomfort and some symptomatic patients opt for conservative treatment, the number of patients is relatively small. Secondly, due to the scarcity of reports on ultrasound features of urethral masses, the knowledge of UC remains insufficient, preventing us from calculating diagnostic accuracy and misdiagnosis rates. We plan to figure up the accuracy and specificity of ultrasound in diagnosing UC based on our current work in the future. Furthermore, contrast-enhanced US has been extensively used in the diagnosis of tumors in all systems, providing more information about the blood flow of the mass, which aids in the differential diagnosis of benign and malignant masses28,29. Our center is exploring this method to further improve diagnostic efficiency, which is also one of our future research directions.
Conclusions
The female UC was mainly located on the posterior lip of the urethra and occurred in postmenopausal women. On transperineal US, female UC mostly appeared as oval hypoechoic or mixed echogenicity nodules with rich blood flow. Hyper-echogenic spots, small cystic echo areas, and macrocalcifications could also be detected. The relative location of the urethra to UC can be accurately described through the combination of transperineal and transrectal US, aiding in surgical planning and patient consultations.
Data availability
The datasets used and analyzed during the current study are available from the corresponding author upon reasonable request.
References
Becker, L. E. Urethral Caruncle: A Herald Lesion for Distal Urethral Stenosis?. J. Natl. Med. Assoc. 67, 228 (1975).
Chiba, M. et al. Urethral caruncle in a 9-year-old girl: a case report and review of the literature. J. Med. Case Reports 9, 71 (2015).
Kore, R. & Kore, R. Urethral caruncle in penile urethra in a young male. Indian J. Urol. 38, 65 (2022).
Zuo, S. W. & Napoe, G. S. Evaluation and management of urethral and periurethral masses in women. Curr. Opin. Obstet. Gynecol. https://doi.org/10.1097/GCO.0000000000000914 (2023).
Verma, V. & Pradhan, A. Management of urethral caruncle – A systematic review of the current literature. Eur. J. Obstet. Gynecol. Reprod. Biol. 248, 5–8 (2020).
Williamson, S. R. et al. Urethral caruncle: A lesion related to IgG4-associated sclerosing disease?. J. Clin. Pathol. 66, 559–562 (2013).
Taylor, C., Pedroso, J., Gutierrez, M. & Volker, K. Squamous Cell Carcinoma in a Urethral Caruncle. J. Minim. Invasive Gynecol. 22, S248 (2015).
Kaneko, G., Nishimoto, K., Ogata, K. & Uchida, A. A case of intraepithelial squamous cell carcinoma arising from urethral caruncle. Can. Urol. Assoc. J. https://doi.org/10.5489/cuaj.10027 (2011).
Algeri, P., Munné-Collado, J. & Algeri, M. Urethral Caruncle Masquerading a Primary Amelanotic Melanoma, the Risk of a Poor Prognosis due to Misdiagnosis. J. Fam. Reprod. Health https://doi.org/10.18502/jfrh.v16i3.10584 (2022).
Sonoda, K., Kato, R., Kojima, H. & Tokuda, Y. Urinary tract bleeding from a urethral caruncle mimicking genital tract bleeding. BMJ Case Rep. 12, e225540 (2019).
Wang, X. et al. The ultrasonographic characteristics of female periurethral solid masses. Int. Urogynecology J. 33, 605–612 (2022).
Yang, H. et al. Ultrasonographic Imaging Features of Female Urethral and Peri-urethral Masses: A Retrospective Study of 95 Patients. Ultrasound Med. Biol. 46, 1896–1907 (2020).
Adler, D. D., Carson, P. L., Rubin, J. M. & Quinn-Reid, D. Doppler ultrasound color flow imaging in the study of breast cancer: Preliminary findings. Ultrasound Med. Biol. 16, 553–559 (1990).
Maetzold, E. & Takacs, E. B. Urethral Pathology in Women. Curr. Urol. Rep. 23, 225–234 (2022).
Okeahialam, N. A., Taithongchai, A., Sultan, A. H. & Thakar, R. Transperineal and endovaginal ultrasound for evaluating suburethral masses: comparison with magnetic resonance imaging. Ultrasound Obstet. Gynecol. 57, 999–1005 (2021).
Conces, M. R. et al. Urethral caruncle: clinicopathologic features of 41 cases. Hum. Pathol. 43, 1400–1404 (2012).
Gakis, G. et al. European Association of Urology Guidelines on Primary Urethral Carcinoma—2020 Update. Eur. Urol. Oncol. 3, 424–432 (2020).
Djafari, A. A., Javanmard, B., Samenezhad, S., Eslami, A. H. & Rakhshan, A. Primary malignant melanoma of the female urethra A rare histopathology case report. Urol. Case Rep. 52, 102642 (2024).
Boughaleb, A., El Boté, H., Lakssir, J., Bellouki, O. & Soufiani, I. Primary diffuse large B-Cell lymphoma of the female urethra: A case report. Urol. Case Rep. 51, 102594 (2023).
Chen, X., Huang, S., Xu, Q. & Lin, H. Primary clear cell adenocarcinoma surrounds the female urethra: A case report and review of literature. Asian J. Surg. https://doi.org/10.1016/j.asjsur.2023.12.205 (2024).
Omotehara, S. et al. Ultrasonographic diagnosis of cystitis glandularis with severe intestinal metaplasia. J. Clin. Ultrasound https://doi.org/10.1002/jcu.23513 (2023).
Serafetinidis, E. et al. Summary Paper of the Updated 2023 European Association of Urology Guidelines on Urological Trauma. Eur. Urol. Focus https://doi.org/10.1016/j.euf.2023.08.011 (2023).
Chaudhari, V. V., Patel, M. K., Douek, M. & Raman, S. S. MR Imaging and US of Female Urethral and Periurethral Disease. RadioGraphics 30, 1857–1874 (2010).
Ying, T. et al. Value of Transrectal Ultrasonography in Female Traumatic Urethral Injuries. Urology 76, 319–322 (2010).
Livingston, B. P. Anatomy and Neural Control of the Lower Urinary Tract and Pelvic Floor. Top. Geriatr. Rehabil. 32, 280–294 (2016).
Atik, Y. T. et al. Female ventral-onlay buccal mucosal graft urethroplasty supported with martius labial fat pad flap: early results. Int. Urol. Nephrol. https://doi.org/10.1007/s11255-023-03909-2 (2024).
Yang, X. et al. The Anatomical Pathogenesis of Stress Urinary Incontinence in Women. Medicina 59, 5 (2022).
Dietrich, C. F. et al. Guidelines and Good Clinical Practice Recommendations for Contrast Enhanced Ultrasound (CEUS) in the Liver – Update 2020 – WFUMB in Cooperation with EFSUMB, AFSUMB, AIUM, and FLAUS. Ultraschall Med. - Eur. J. Ultrasound 41, 562–585 (2020).
Sidhu, P. et al. The EFSUMB Guidelines and Recommendations for the Clinical Practice of Contrast-Enhanced Ultrasound (CEUS) in Non-Hepatic Applications: Update 2017 (Long Version). Ultraschall Med. Eur. J. Ultrasound 39, e2–e44 (2018).
Funding
This work was funded by the National Natural Science Foundation of China (grant no. 81571699).
Author information
Authors and Affiliations
Contributions
Z.L. participated in study design, literature search, and manuscript writing. X.W. revised the article and participated in data collection and data analysis. W.S. contributed to data analysis and prepared the pictures. Y.Y., M.Z. and B.C. helped data collection. R.Z. revised the article and did the final approval of the version to be published. T.Y. helped in topic selection, funding acquisition and data interpretation. All authors give their consent to publish this article.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Liu, Z., Wang, X., Shui, W. et al. Ultrasonographic features of female urethral caruncle: a retrospective study of 20 patients. Sci Rep 14, 17431 (2024). https://doi.org/10.1038/s41598-024-68355-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-68355-1
- Springer Nature Limited