Abstract
This retrospective study aimed to investigate the progression of central retinal vein occlusion (CVO) prior to treatment initiation and its impact on prognosis. Of the 54 studied eyes with acute CVO, the average logMAR visual acuity (VA) at the initial visit was 0.65 ± 0.49 with an average time to treatment of 14.9 ± 14.5 days. VA at the initial treatment was identified as a stronger predictor of VA at the final visit compared to VA at the first visit or other factors. Patients who received treatment more than 28 days after the initial visit experienced a significant decline in VA compared to those treated within 28 days (0.21 ± 0.35 vs. 0.04 ± 0.13, p = 0.006). Additionally, patients who were treated between 15 and 28 days showed a greater decrease in VA compared to those treated within 14 days (0.12 ± 0.46 vs. 0.018 ± 0.02, p = 0.026). These findings from the current retrospective analysis suggesting that there is a possibility of VA decline at the initial treatment associating with worse prognosis even when treatment is administered within a month should be further investigated in the prospective study. Also, it may be crucial to consider frequent monitoring of acute CVO patients for initiating treatment at the optimal timing.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Introduction
Retinal vein occlusion (RVO) is the second most common retinal vascular disease with a global prevalence of 28 million1. According to the Hisayama study, the prevalence of RVO is 2.1% in Japan, with branch RVO (BVO) at 2.0% and central RVO (CVO) at 0.2%, which is higher than in other countries2. Macular edema (ME) is the most frequent cause of visual loss after RVO. ME has been treated with sub-tenon triamcinolone acetonide or vitrectomy. Since the approval of anti-vascular endothelial growth factor (VEGF) therapy in 2013, many patients have been treated with anti-VEGF injections. The BRAVO and CRUISE studies evaluated the efficacy of intravitreal injections of ranibizumab, while the COPERNICUS and GALILEO studies evaluated the efficacy of intravitreal injections of aflibercept (IVA)3,4,5,6. However, there are individual differences in visual prognosis and treatment frequency. Some studies suggest a relationship between age and visual acuity (VA), while others contradict this7,8.
In clinical practice, some patients cannot be treated immediately due to the time lag between referral to a specialist hospital, complications, untreated hypertension, and refraining from medical examinations due to the pandemic. The KRVO study suggested no significant correlation between ME duration and visual outcomes9. However, the study included patients with BVO or CVO who were treated with bevacizumab or triamcinolone9. In contrast, several analyses from anti-VEGF trials suggested that the visual outcome is better with a shorter duration of edema. The CRYSTAL study suggested the visual prognosis of eyes treated within 3 months was better compared to those treated > 3 months from diagnosis10. The COPERNICUS study, which evaluated the efficacy of IVA for CVO, indicated that visual prognosis was worse and irreversible retinal damage occurred when treatment was started after 6 months compared to immediate treatment after onset. Furthermore, the visual prognosis of patients who started treatment within 2 months was better than those who initiated treatment after 2 months5. The guideline in 2022 suggested that time to initial evaluation and treatment should be not more than 2–4 weeks from presentation, and that treatment should be initiated within 1–2 weeks of assessment in an appropriate facilities for intravitreal injection11. However, to the best of our knowledge, there has not yet been published literature to investigate the association between visual outcome and the time to treatment that was shorter than 2 months. Considering the rapid progress in some cases with CVO, detailed information on the influence of the time lag to treatment, even if it is 2 months or shorter, on the visual prognosis should be helpful.
Also, the COPERNICUS study was designed to recruit patients with macular edema with the central subfield thickness of 250 μm or greater in three-dimensional OCT. Best-corrected visual acuity of the participants was restricted between 20/40 (equivalent of 0.3 logMAR) and 20/320 (1.2 logMAR)5. However, in the real-world practice, some patients with CVO may present with little or no macular edema, or with very good visual acuity at presentation, which might lead to prolongation of time to treatment. Therefore, information on the backgrounds of the patients with or without immediate anti-VEGF treatment should be helpful to making a strategy in the management for CVO.
Herein, we hypothesized that visual outcome might be associated with time to treatment even if it was within 1 or 2 months, and investigated the relationship between treatment outcomes and time from the first visit to the first treatment in CVO patients treated with anti-VEGF agents. The backgrounds of the patients who took relatively longer time before initiating treatment were also analyzed.
Results
During the recruitment period, 60 eyes of 60 patients presented and were diagnosed as CVO. Three of them refused to undergo anti-VEGF treatment though it was explained as a primary option for treating macular edema, and underwent sub-Tenon injection of steroid. One patient had vitreous hemorrhage due to retinal neovascularization that needed prompt laser therapy. Two patients had treatment history. The remaining 54 treatment-naive patients underwent anti-VEGF therapy and all of them were followed up for at least one year. These 54 eyes of 54 patients were included in the study. Demographic and background factors were shown in Table 1. There was no significant difference between VA at the initial visit or at the initial treatment and VA at the last visit (p = 0.15 or 0.45, respectively). However, if the patients with VA better than 20/40 were excluded, the VA at the initial treatment was significantly better than that at the last visit (N = 41, 0.86 ± 0.39 and 0.70 ± 0.67, p = 0.034). 36 (56%), 13 (24%), and 9 (17%) patients had hypertension, diabetes, and dyslipidemia that required treatments. None of the studied patients had iris neovascularization or neovascular glaucoma at the initial visit.
Firstly, VA at the first visit was the only factor significantly associating with VA change from the first visit to the last visit (Table 2). On the other hand, VA at the initial treatment and lens status was factors significantly associated with VA at the last visit (Table 2).
Secondly, considering that VA at the initial treatment was a key factor for VA at the last visit, we analysed associating factors with VA at initial treatment. As a result, only VA at the first visit and time to initial treatment were significantly independently associated with VA at the initial treatment (Table 2 and Fig. 1). Systemic comorbidities such as hypertension, diabetes, and dyslipidemia did not show significant association with any of these outcome variables.
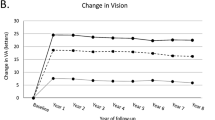
Additionally, we classified patients based on the time to treatment, and compared demographic characteristics and outcomes. Compared with patients treated within 28 days, those with > 28 days were found to show better VA at the first visit, worse VA change during the time from the first visit to initial treatment, smaller CST at the first visit, and a greater proportion of eyes without ME at the first visit (Table 3 and Fig. 2a). Moreover, compared with patients treated within 14 days, those treated after 15–28 days showed better VA, worse VA change from the first visit to initial treatment, and smaller CST at the first visit (Table 3 and Fig. 2b).
Among nine cases exceeding 28 days, five cases did exhibit no ME on initial presentation. Two patients presented minimal ME and refused immediate treatment with expectation of natural remission. One case experienced a delay due to surgery in another department, and one case required treatment for hypertension (systolic BP > 180 and diastolic BP > 100). The representative case was shown in Fig. 3.
A representative case. A fifty-eight-year-old man presented with visual disturbance of the right eye. The diagnosis of CVO was made from disseminated retinal hemorrhages and dilated retinal vein (a). Because there is no edema (b) with good VA of 0.1 logMAR, no treatment was given at that time except referring to the internal physician for hypertension. On the following visit thirty-seven days after the initial presentation, his BP improved but hemorrhages worsened with development of ME (c and d). VA was 0.4 logMAR. Anti-VEGF therapy was initiated. After 1-year of totally three injections, hemorrhages and ME resolved (e and f). VA was 0.7 logMAR.
Lastly, no factors were associated with the number of treatments in 1 year (Table 4).
Discussion
We evaluated the association between treatment outcomes and the duration to the first treatment in CVO patients treated with anti-VEGF agents. VA at the last visit was significantly and strongly associated with VA at the initial treatment. VA at the first visit and the time to initial treatment were independently associated with VA at the initial treatment. Compared to the patients treated within 28 days, those of 28 days or longer had a worse VA change from the first visit to the initial treatment. Similarly, compared to the patients treated within 14 days, those treated after 15–28 days had a worse VA change from the first visit to the initial treatment. No factors were found to be associated with the number of treatments within 1 year.
In the present analysis, we firstly found that VA change from the first to the last visit was associated with VA at the first visit. VA change is usually evaluated to determine treatment efficacy. However, due to the possibility of a ceiling effect, it is highly likely that VA change can be associated with baseline VA. This was supported by the results of the current study that the VA change from the initial treatment to the last visit was not significant, although it became significantly better when the patients with VA better than 20/40 was excluded as they would be in the previous large clinical trials. In this study, to directly evaluate VA prognosis, we investigated possible predictors of the final VA rather than of the final VA change.
Consequently, VA at the last visit was associated with VA at the initial treatment rather than VA at the first visit in the multivariate analysis. The correlation between the VA at initial treatment and the final VA was also reported by Sen et al., and the results of this study were similar to ours12. This result emphasizes the importance of initiating anti-VEGF treatment with good VA in patients with CVO.
Next, we investigated factors associated with VA at the initial treatment. As a result, time from the first visit to the initial treatment, as well as VA at the first visit, was independently associated with VA at the initial treatment. The analysis showed that better VA at the first visit and a shorter duration before the first treatment were significantly associated with better VA at the initial treatment. Although the time from the first visit to the initial treatment was relatively short (14.4 ± 14.3 days) in the cohort of the present study, the results suggested possible VA change from the first visit to the initiation of treatment within approximately a month.
Additionally, when we compared the group with a time to treatment of > 28 days with the group with a time of treatment within 28 days, the former had a worse change in VA from the first visit to initial treatment. Furthermore, when we compared the group with a time to treatment of 15–28 days with the group with a time to treatment within 14 days, the former also showed a worse change in VA from the first visit to initial treatment. Therefore, a shorter time from the first visit to initial treatment leads to better VA at the initial treatment, and the results suggested that difference in duration of 2 weeks could affect the visual outcome. Generally, there have been previous studies suggesting that prompt initiation of treatment is recommended. The latest report examined visual outcome of CVO patients with poor initial visual acuity, and suggests that if a delay from the symptom onset to the first injection was 30 days or longer, a higher incidence of detrimental events could be predicted. The authors recommended more frequent follow-ups, ideally every 1–2 weeks, to ensure optimal timing of initial treatment13. However, there have been little information regarding the relationship between VA at the first visit and the duration before treatment in the entire population of CVO patients including good initial visual acuity. As observed in this study, longer days before the initial treatment may lead to a decrease in VA at the initial treatment, and thus may result in a worse visual prognosis.
In the present analysis, a large part of patients with longer time to treatment showed no or minimal macular edema, or had better VA at the initial visit. Anti-VEGF therapy is not entirely risk-free and is approved only for patients with ME in Japan. Furthermore, there have been reports of natural improvement in ME without any treatment. In the previous study, Lee et al.14 reported in 2010 that they studied the clinical course of relatively young patients with CVO accompanying with mild or no edema and found that most patients recovered without any specific treatment. It is commonly acknowledged that some patients with CVO, especially with no or mild ME, naturally recovered without any treatments. Therefore, the indication or the optimal timing to initiate treatment for CVO is sometimes difficult especially in patients with mild or very little anatomical/functional impairment. Due to this dilemma, determining the optimal timing for starting treatment for CVO is thought to be challenging. The results of the present study may imply that CVO can rapidly progress in some patients even they had very little anatomical or visual changes, and very frequent follow-ups (as often as every 1–2 weeks) may be recommended to ensure optimal timing for treatment initiation.
The limitations of this study include its retrospective design, which may have introduced selection bias. Patients who did not undergo anti-VEGF treatments were not included in the analysis. Additionally, there are factors such as differences in the time until treatment initiation for each patient, even if they have the same degree of VA and ME. There was also variation among patients in the time from symptom onset to visit to our hospital, although it was thought to be generally short considering the nature of this disease. Detailed information on the degree of ischemia, that might be one of the factors predicting visual prognosis, was unavailable in the current study.
In conclusion, a delay of 14–28 days or longer to the initial treatment may be associated with worse VA at the initial treatment and unfavourable visual prognosis in patients with CVO. For the CVO patients, if their anatomical or visual changes are minimal, very frequent follow-ups (as often as every 1–2 weeks) may be recommended to ensure optimal timing for treatment initiation.
Materials and methods
Study design
This retrospective study was conducted in accordance with the Declaration of Helsinki and was approved by the institutional review board (IRB) of the University of Tokyo (No. 2217, approved on 3/Feb/2023). The need for written informed consent was waived by the IRB. However, participants who did not authorize the use of their medical records for research purposes were excluded from the study.
Participants
The inclusion criteria were as follows: patients who sought treatment at the University of Tokyo Hospital between April 2010 and May 2022, diagnosed with central vein occlusion (CVO) for the first time, and treated with intravitreal anti-VEGF injections. The exclusion criteria were as follows: patients who were followed up for less than 1 year, those who received their first anti-VEGF injection 90 days or more after their initial visit, those who had previously undergone CVO therapy before coming to our institution, those with ocular comorbidities that affected their visual acuity at presentation, and those who had undergone vitrectomy. All patients underwent a standard examination that included measurement of best-corrected visual acuity (BCVA), slit-lamp biomicroscopy, funduscopy, and spectral-domain optical coherence tomography (OCT) (Spectralis; Heidelberg Engineering, Heidelberg, Germany) or swept-source OCT (Atlantis; Topcon, Japan) at each visit. Macular edema was qualitatively defined as the presence of inner retinal fluid within a 1 mm-diameter central macular area. Central subfield thickness (CST) was measured as the mean thickness within the central subfield with the diameter of 1 mm. Serous retinal detachment (SRD) in the fovea at the initial visit was also assessed. BCVA was measured using the Landolt C chart, and the values were converted into the logarithm of the minimal angle of resolution (logMAR). Dye angiography was recommended but not necessarily performed.
Treatments
After the diagnosis of CVO was made, the natural course and the treatment options (mainly anti-VEGF treatment) were explained to the patients. The possibility of natural regression especially when the presentation was mild and the possibility of rapid progress resulting in the irreversible visual dysfunction (blindness in some cases) were also explained. After obtaining informed consent, all the patients received ranibizumab (0.5 mg) or aflibercept (2 mg). The choice of drug was at the physician's discretion considering patients' preferences after the details of each drug were explained. The patients were monthly followed up with the pro re nata protocol, where additional injections were administered if macular edema revealed by OCT persisted or recurred during periodic follow-ups. Grid laser photocoagulation was not performed to treat the macular edema.
Statistical analysis
The outcomes evaluated were VA/VA change at the initial treatment, VA/VA change at the last visit, number of treatments in 1 year, and absence of macular edema at the first visit. VA at the initial visit, at the initial treatment, and at the last visit were compared. Correlation analyses were conducted using the VA change from the first to the last visit, VA at the last visit, or VA at the initial treatment as the outcome variables, and age, sex, VA at the first visit, time from the initial visit to initial treatment, CST at the first visit, foveal SRD at the first visit, and lens status as explanatory variables.
Additionally, age, sex, VA at the first visit, presence or absence of macular edema at the first visit, change in VA from the first visit to initial treatment, CST at the first visit, no ME at the first visit were analyzed between the two groups based on the number of days from the first visit to initial treatment: within 28 days and > 28 days or 0–14 days and 15–28 days. Lastly, correlation analysis was conducted using the number of treatments in one year as the outcome variable, and age, sex, VA at the first visit, time to the initial treatment, CST at the first visit, and lens status as explanatory variables.
For independent numerical variables and paired data, t-tests and paired t-tests, respectively, were used. Univariate and multivariate correlation analyses were conducted. If multiple explanatory variables were significantly associated, multiple regression analysis with model selection was performed. The explanatory variables were evaluated using a linear model, and the optimal linear model was selected from all possible combinations of predictors, resulting in 2^4 to 2^5 patterns based on the second-order bias-corrected Akaike Information Criterion index (denoting the optimal model)15. The significance level was set at p < 0.05. In detecting difference of 0.2 logMAR between two patient groups classified based on the time to treatment, we found 34 subjects in total (17 in each group) would be required with expected standard deviation of 0.2, power of 0.80, alpha of 0.05. The analysis was performed using JMP® 16 (SAS Institute Inc.).
Ethics declarations
This study involves human participants and was approved by the Institutional Board of University of Tokyo School of Medicine (Ethics approval number: 2217).
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Song, P., Xu, Y., Zha, M., Zhang, Y. & Rudan, I. Global epidemiology of retinal vein occlusion: A systematic review and meta-analysis of prevalence, incidence, and risk factors. J. Glob. Health 9, 010427 (2019).
Yasuda, M. et al. Prevalence and systemic risk factors for retinal vein occlusion in a general Japanese population: The Hisayama study. Investig. Ophthalmol. Vis. Sci. 51, 3205–3209 (2010).
Campochiaro, P. A. et al. Ranibizumab for macular edema following branch retinal vein occlusion: Six-month primary end point results of a phase III study. Ophthalmology 117, 1102-1112.e1 (2010).
Brown, D. M. et al. Ranibizumab for macular edema following central retinal vein occlusion: Six-month primary end point results of a phase III study. Ophthalmology 117, 1124-1133.e1 (2010).
Brown, D. M. et al. Intravitreal aflibercept injection for macular edema secondary to central retinal vein occlusion: 1-year results from the phase 3 COPERNICUS study. Am. J. Ophthalmol. 155, 429-437.e7 (2013).
Holz, F. G. et al. VEGF trap-eye for macular oedema secondary to central retinal vein occlusion: 6-month results of the phase III GALILEO study. Br. J. Ophthalmol. 97, 278–284 (2013).
Daien, V. et al. Visual acuity outcome and predictive factors after bevacizumab for central retinal vein occlusion. Eur. J. Ophthalmol. 22, 1013–1018 (2012).
Dewan, K. S. et al. Age-related differences in presentation and outcomes of anti-VEGF treatment of retinal vein occlusion. Can. J. Ophthalmol. J. Can. Ophtalmol. 56, 96–104 (2021).
Yoon, Y. H. et al. Improved visual outcome with early treatment in macular edema secondary to retinal vein occlusions: 6-month results of a Korean RVO study. Jpn. J. Ophthalmol. 58, 146–154 (2014).
Larsen, M. et al. Individualized ranibizumab regimen driven by stabilization criteria for central retinal vein occlusion: Twelve-month results of the CRYSTAL study. Ophthalmology 123, 1101–1111 (2016).
Nicholson, L., Talks, S. J., Amoaku, W., Talks, K. & Sivaprasad, S. Retinal vein occlusion (RVO) guideline: Executive summary. Eye 36, 909–912 (2022).
Sen, P. et al. Predictors of visual acuity outcomes after anti-vascular endothelial growth factor treatment for macular edema secondary to central retinal vein occlusion. Ophthalmol. Retina 5, 1115–1124 (2021).
Light, J. G., Tian, J. & Wenick, A. S. Outcomes in retinal vein occlusions presenting with poor visual acuity treated with anti-vascular endothelial growth factor therapy: Prognosis and predictive factors. Ophthalmol. Retina 5, 888–900 (2021).
Lee, D.-H., Lee, S.-J. & Yoon, I.-N. Clinical progress in impending central retinal vein occlusion. Korean J. Ophthalmol. 24, 83–88 (2010).
Azuma, K. et al. The association of choroidal structure and its response to anti-VEGF treatment with the short-time outcome in pachychoroid neovasculopathy. PLoS One 14, e0212055 (2019).
Acknowledgements
We would like to thank Asako Ogawa-Murano, Kayoko Komatsu, Shoko Abe, Natsuki Maetani for technical assistance.
Author information
Authors and Affiliations
Contributions
R.O. and C.A. contributed to the conception or designed the study and the acquisition of the data. R.O. and C.A. wrote the main manuscript. S.A., K.K., K.A, R.F., and T.I. contributed the analysis and the interpretation of the data. All authors read and approved the submitted version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
Ryo Obata received honoraria for speaking/consulting from Santen, Bayer, Novartis, Chugai, Senju and Boehringer Ingelheim. All the other authors declare no competing interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Agata, C., Aoki, S., Kitamoto, K. et al. Time to initiate anti-vascular endothelial growth factor therapy and visual outcome in central retinal vein occlusion. Sci Rep 14, 16974 (2024). https://doi.org/10.1038/s41598-024-67925-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-67925-7
- Springer Nature Limited