Abstract
Globally, hip fractures represent a significant and growing public health concern, particularly as the elderly population increases. The timing for surgery following hospitalization for hip fractures is a crucial indicator of acute quality care following recommended surgical guidelines of within two days to minimize complications and mortality. However, factors influencing delayed surgery and its outcomes remain debated. This study, used a national administrative database in South Korea, aimed to examine surgery performed within two days of hospitalization and investigate factors affecting delayed surgical interventions and associated outcomes. Of the hip fracture patients analyzed, 40.6% underwent surgery within two days of hospitalization. Factors associated with delayed surgery included: male patients (OR 1.190; 95% CI 1.022 ~ 1.385), medical aid beneficiary (OR 1.385; 95% CI 1.120 ~ 1.713), higher comorbidity index (OR 1.365; 95% CI 1.163 ~ 1.603, OR 1.612, 95% CI 1.327 ~ 1.958), weekends admission (OR 2.384; 95% CI 2.804 ~ 2.729), admission via outpatient department (OR 1.298, 95% CI 1.071 ~ 1.574). ORIF (OR 0.823, 95% CI 0.691 ~ 0.980) was associated with a significantly low risk of late surgery. While early surgery did not significantly impact in-hospital mortality or complications, it was associated with short and postoperative lengths of stay. This study underscores the need for prompt surgical intervention, particularly in high-risk patient populations, as well as highlights the importance of further research to elucidate the relationship between the timing of surgery and postoperative outcomes.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
The estimated worldwide incidence of hip fractures in 2000 was 1.6 million1. The number of hip fractures is estimated to nearly double to 2.6 million in 2025 and 4.5 million in 20502. The Organization for Economic Co-operation and Development (OECD) predicted that hip fractures will become an important health problem in the future as life expectancy increases3. Hip fracture contributes to both morbidity and mortality in the elderly4. In addition, it accounts to one of the highest medical costs personally and nationally among single fractures due to long-term bed rest and limitation of independent daily living5,6.
As one of the nations with the fastest aging trend in the world, the frequency of senile hip fractures in South Korea has increased sharply from 35,735 in 2010 to 89,730 in 2019, about 25% annually 7,8. In 2017, hip replacement was the 16th most common surgery performed in South Korea, and the length of stay per case was 19.6 days, the second longest among other pathologies in the country9.
The best treatment for hip fracture is a surgical intervention to repair or replace hip10. The timing for surgery is an indicator of the quality of acute care. The OECD evaluates surgical performance rate within 2 days (48 h) of hospitalization as an indicator for the quality of hip fracture patients care3. Generally, it is agreed that surgery for hip fractures should be performed within two days (48 h) of hospitalization11. The National Institute for Health and Care Excellence (NICE) clinical guidelines recommended that, hip fracture surgery be performed on the day of hospitalization or the next day12. However, research by Alejandro Lizaur-Utrilla, suggests that delaying surgery for up to 4 days does not affect morbidity or mortality for hip fracture. Therefore, it demands a greater focus on optimizing the patient's condition before surgery rather than adhering strictly to a universal surgical timing.
Postulates have shown conflicting results on the relationship between early surgery and survival after hip fracture in older patients 3,4,6,13,14,15,16,17,18. While some studies argued that the timing of surgery is not related to mortality13, others have shown that early surgery has reduced hospitalization, complications, and pain14.
However, in South Korea, there is almost no discussion about the timing of hip fractures using national data. Therefore, this study aimed to examine surgery performed within two days of hospitalization and investigate factors affecting delayed surgical interventions and associated outcomes South Korea.
Materials and methods
This is a retrospective study aimed at distinguishing patients’ characteristics with differences in the period from admission to surgery among hip fracture individuals using the Korean National Hospital Discharge In-depth Injury Survey (KNHDIIS) data. This data identifies the characteristics and risk factors of hip fractures for individuals hospitalized through the emergency room using the medical information of discharged patients. KNHDIIS is managed by the Korea Disease Control and Prevention Agency.
Using a systematic sampling method and about 9% extraction of all discharged patients, the KNHDIIS selected 170 institutions representing 30.3% of hospitals nationwide for all patients discharged from a hospital with more than 100 beds, including general hospitals, hospitals, and healthcare centers19.
Selection criteria
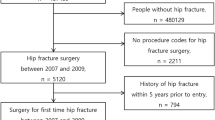
A total of 1,281,606 cases were registered in KHIDIIS from 2015 to 2019. The study subjects were primarily cases of hip fractures requiring hospitalization and surgery. Patients under 65 and over 100 years of age were excluded (Fig. 1)."
Methods
The duration from admission to surgery can be distinguished in hours or days. The data used in this study are collected in days. The OECD indicator for hip fracture patients measures the period from admission to surgery based on a 2-day threshold. Therefore, this study calculated the duration from admission to surgery for hip fracture patients as the surgery date. Subsequently, cases within 2 days were classified as the early surgery group, while cases beyond 3 days were classified as the late surgery group.
Among the reviewed variables, we considered independent variables for gender, age, medical aid beneficiary (no, yes), comorbidity (Charlson Comorbidity Index; 0 points, 1–2 points, 3 points or more), type of injury (falls, traffic accidents, others), admission day(weekdays, weekends), admission via outpatient department (no, yes), type of femur fracture (neck; ICD-10 code S72.0, pertrochanteric; ICD-10 code S72.1), type of surgical procedure (closed reduction of fracture with internal fixation (CRIF); ICD-9-CM 79.1, open reduction of fracture with internal fixation (ORIF); ICD-9-CM 79.3, hemiarthroplasty (HAP); ICD-9-CM 81.4, total hip arthroplasty (THA); ICD-9-CM 81.5)20,21. The three-level Charlson Comorbidity Index (CCI) was used to proxy for case mix complexity15. Admission day was categorized into weekdays and weekends, with Friday, Saturday, and Sunday as weekends.
Outcomes from femur fracture surgery are in-hospital mortality, total length of stay, length of stay after surgery, and complications. In-hospital mortality included in-hospital death and hopeless discharge. The complications were defined by International Classification of Diseases-10 codes indicating a complication (appendix 1).
Statistical methods
Data were presented and analyzed from the frequency of patients by 0, 1, and 2 days by fracture types and surgical procedures performed. Patient characteristics grouped into early and late surgery were compared using analysis of variance (ANOVA) for the continuous variables and Pearson’s chi-squared test for the categorical variables. In the analysis of factors associated with late surgery, multiple logistic regression analysis was performed. Frequency outcomes, including mortality, complications, and total length of stay (median and quartiles), multiple logistic regression analysis was performed (Table 1).
We conducted a post-hoc power analysis referencing two studies, using the following assumed values for the power calculation: Alpha (type I error) = 0.05, N (sample size) = 4049 (as reported in the studies), P (event rate) = 0.536 (late surgery rate reported in the studies), OR (odds ratio) = 1.271 (average OR from Table 2). The resulting power was over 0.99, indicating that the analysis was performed with a sufficient sample size to identify variables related to late surgery.
All statistical analysis was performed with STATA 15.0 (StataCorp, College Station, Texas). A p-value < 0.05 was considered to be statistically significant.
Ethical approval and consent to participate
All methods were performed in accordance with the ethical standards as laid down in the Declaration of Helsinki and its later amendments or comparable ethical standards. This research was approved by the National Health Insurance Ilsan Hospital Institutional Review Board (IRB) file number NHIMC 2024-04-023. All of the materials used in the article were only publicly available data. Moreover, all of those data are non-identifying data, and anyone can use them. In cases where participants were to be contacted for detailed information regarding their hospitalization, a written informed consent was solicited and approval obtained before proceeding with data collection with animosity respected.
Results
Hip fracture surgery initiation after hospitalization to the hospital
As shown on Fig. 2, 40.6% of all patients who underwent surgery within two days of hospitalization was presented. The surgery rate on the day of hospitalization was 5.8%, and 28.6% within 1 day. Depending on the fracture type classification, the surgical rate within 2 days was 43.6% for neck and 48.5% for pertrochanteric. Depending on the surgical procedure type classification, the surgical rate within 2 days varied from 42.7% to 52.2% depending on the surgical procedure type classification.
Factors associated with early surgery and late surgery
Of the 4,049 patients with hip fracture surgery, 2,171 (53.6%) underwent late surgery. Table 1, presents the characteristics stratified into early and late surgery subgroups. Compared with the early surgery group, patients in the late surgery group were significantly more likely to be: male (p < 0.05), Medical aid beneficiaries (p < 0.01), multiple comorbidity (< 0.001), admitted on weekdays (p < 0.001), admission via outpatient department (p < 0.01), neck fracture (p < 0.01) and had the procedure of HAP, THA (p < 0.001).
Table 2 shows the adjusted odds ratio (OR) and 95% confidence intervals (95% CI) for late surgery, as determined by multivariate logistic analysis. We adjusted for gender, age, medical aid beneficiary, comorbidity, type of injury, admission day, admission via outpatient department, type of fracture, and type of surgical.
The occurrence of the late surgery was significantly higher in male patients (OR 1.190; 95% CI 1.022 ~ 1.385), medical aid beneficiary (OR 1.385; 95% CI 1.120 ~ 1.713), multiple comorbidity (OR 1.365; 95% CI 1.163 ~ 1.603, OR 1.612, 95% CI 1.327 ~ 1.958), weekends admission (OR 2.384; 95% CI 2.804 ~ 2.729), admission via outpatient department (OR 1.298, 95% CI 1.071 ~ 1.574). ORIF (OR 0.823, 95% CI 0.691 ~ 0.980) was associated with a significant lower risk of late surgery.
Peri-operative outcomes associated with late surgery
The study examined whether there were statistically significant differences in in-hospital mortality, total length of stay, postoperative length of stay, and complication rates based on the timing of surgery after admission (Table 3). Before statistical adjustment, there were statistically significant differences in both early and late surgery groups for total length of stay, postoperative length of stay, and complications. However,
after statistical adjustment with independent variables, statistically significant differences remained only for total length of stay and postoperative length of stay. The total length of stay was 5.8 days longer (median 5 days) in the late surgery group compared to the early surgery group. The postoperative length of stay was 1.1 days longer (median 1 day) in the late surgery group compared to the early surgery group.
Discussion
This study analyzed surgical intervention time after hospitalization in patients with hip fractures and examined the factors affecting late surgery (operation after 2 days of hospitalization) and associated outcomes. However, the various categories of health facilities that were use had similar conditions and procedures. The time taken to initiate hip fracture surgery after hospitalization is widely considered to be a clinically meaningful process indicator of the quality of acute care received by patients with hip fractures3. Therefore, existing guidelines related to hip surgery recommend early surgery within two days of hospitalization to reduce length of stay, complications, and mortality. Time to surgery for hip fracture patients is influenced by associated factors such as patient, fracture pattern, institution, policies, etc.16.
In this study, 40.6% of hip fracture patients underwent surgery before 2 days of hospitalization. This is congruent with studies performed in Portugal and Latvia that showed 43.5% and 40.6%, respectively, for surgery of hip fractures executed within two days, with Norway, Denmark, and the Netherlands among the countries with more than 95% hip fracture surgery performed within two days21. In 2007, Korea operated a medical service performance reporting system for partial hip fracture replacement surgery, and the re-admission rate and length of hospitalization decreased. However, this was widely opposed by medical institutions as the timing for surgery was not considered but taken as a newly admitted cases22,23. To reduce the average length of hospital stays for inpatients, introducing a system to manage the period from admission to surgery should be considered. Such a change is expected to optimize patient treatment duration and enhance the efficiency of medical services.
The findings of this study suggest the need for further research to investigate whether there are differences in surgical accessibility based on gender and medical insurance status. Therefore, it can be inferred that it is necessary to improve policies and systems related to healthcare service accessibility based on gender and insurance type. Factors that delayed surgery were classified into patient-side factors, clinical factors, and systematic aspects of medical institutions. Based on some of these factors, it showed that there were delayed surgery for men rather than women and recipients of medical aid beneficiaries. This differs from similar studies that revealed that patients who underwent early surgery are usually younger and healthier4,18,24, and the same result as in delayed surgery in the case of men18.
Regarding clinical factors and similarly with previous studies, the higher the comorbidity index, the more the probability for delayed surgery was observed with some associated conditions such as; anticoagulant or antiplatelet medication, medical resources, preoperative cardiac tests, or administrative/organization responses18,25 and can further be exacerbated if the patient had heart disease, chronic obstructive pulmonary disease, or previous cancer history as well as the duration of laboratory test25,26.
On weekends, a systemic problem was observed that is different from that of weekdays, which included the unavailability of operating room of up to 60.7% and 33.1% of acute medical problems was the reason for delays for hip fracture surgery more than 48 h13. One of the frequent reason for surgical delay in this study was the lack of an available operating room within 48 h of admission, which accounted for more than one-half of the delays18. This finding indicates that organizational improvement is needed and represents a target for interventions aimed at improving the efficiency of the model of care. A study performed in 2016, shows a low performance rate within 2 days of hospitalization when performing ASA > 2, Charlson > 2, and anticoagulant therapy, but medical complication was not significant with delayed surgery more than 2 days29. Policies aimed at adjusting surgical facilities and medical staffing to accommodate the disease characteristics of elderly patients would minimize surgical delays and provide more prompt and effective medical services to patients, even on weekends.
Hagino et al. (2017) revealed in their study that trochanteric fractures occurred more frequently than neck fractures, with more often delayed surgeries25. Trochanteric practices and neck Fx. are associated with age-related in local porosity28. In this study, HAP and THA based on CRIF factors were not types of practices and procedures that delayed surgery. This means that patient's clinical factors do not significantly affect the delay in surgery. In this study, the type of fractures and type of procedures were not factors that slowed surgery in HAP and THA compared to CRIF. Through this, it can be deduced that the patient's clinical factors do not significantly affect the delay in surgery. However, early surgery was useful for improving mobility, but showed a higher mortality rate in patients with a compromised somatic condition at the time of the injury. For independent patients with a stabilized somatic condition, surgery should be performed within 24 h. For unstable cases, we believe it is better to provide early surgery after stabilizing the patient's condition to the greatest possible extent30.
This study reveals that, the total length of stay from admission to discharge and length of stay after surgery were a factor influenced by the time of surgery after controlling for other factors. Screening on administration for American Society of Anesthesiologists grade, Abbreviated Mental Test Score and mobility state of the length of stay and care tailored to match needs31. Therefore, time management for surgery will also project the management of the length of stay during hospitalization.
Complications were observed after univariate analysis, but were not parallelized in multivariate analysis, and the entire hospital stay was affected by both univariate and multivariate, so if surgery was delayed, the hospital stay was long. The timing of the operation did not affect mortality in the hospital, the number of days of hospital stay after surgery, and complications. There was no relationship between surgery after 24 h and a 6-month mortality study13. The relationship between the timing of surgery and the occurrence of complications and mortality rates is complex and could involve various factors. Further research and analysis are needed to better understand this relationship. Considering these results, it will be essential to determine patient treatment plans and policies accordingly32.
The limitations of this study include: Firstly, it primarily focuses on South Korea, which may constrain the applicability of the results to other countries or regions with different healthcare systems, population characteristics, and socioeconomic factors. Therefore, caution is needed when generalizing the results to other population groups. Secondly, this study relies on secondary data, which could affect the completeness, accuracy, and potential biases or missing information that may influence the research findings and conclusions. Thirdly, not all potential variables that could impact surgical outcomes or patient treatment were encompassed. Additionally, since the data only targeted surgical durations based on fractures, further research is needed to explore outcomes such as mortality rates or readmissions due to complications at specific periods after surgery, such as 6 months or 1-year post-surgery. Hence, a broader consideration of factors influencing surgical decisions and patient outcomes is required during result interpretation.
Conclusion
The incidence of hip fractures is rapidly increasing alongside the aging population, yet there remains controversy regarding the relationship between the optimal timing of surgery and postoperative outcomes. According to the findings of this study, surgery within 2 days of admission did not affect outcomes such as in-hospital mortality and complications. However, the severity of the patient's condition was a factor delaying surgery. It suggests the need for a rapid collaborative system for patients requiring medical correction. Furthermore, to extend beyond the limitations of the study data, which were confined to the duration of hospitalization at the time of surgery, additional research exploring the relationship between the timing of surgery and mortality and complications is necessary to clarify the correlation further.
Data availability
Data and materials are available to other parties for research purposes after a data sharing agreement plan is agreed to and signed. Those interested should contact the corresponding author.
References
Johnell, O. & Kanis, J. A. An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos. Int. https://doi.org/10.1007/s00198-006-0172-4 (2006).
Gullberg, B., Johnell, O. & Kanis, J. A. World-wide projections for hip fracture. Osteoporos. Int. 7(5), 407–413 (1997).
OECD. “Waiting times for hip fracture surgery”, in Health at a Glance 2015: OECD Indicators (OECD Publishing, 2015).
Dhanwal, D. K., Dennison, E. M., Harvey, N. C. & Cooper, C. Epidemiology of hip fracture: Worldwide geographic variation. Indian J. Orthop. 45(1), 15–22 (2011).
Leal, J. et al. Impact of hip fracture on hospital care costs: a population-based study. Osteoporos Int. 27(2), 549–558 (2016).
Johnell, O. & Kanis, J. A. An estimate of the worldwide prevalence, mortality and disability associated with hip fracture. Osteoporos Int. 15(11), 897–902 (2004).
Statistical Yearbook of Health Insurance, (2010).
Statistical Yearbook of Health Insurance, (2019).
National Health Insurance Service, Surgery statistics, (2017).
Menzies, I. B., Mendelson, D. A., Kates, S. L. & Friedman, S. M. Prevention and clinical management of hip fractures in patients with dementia. Geriatr. Orthop. Surg. Rehabil. 1(2), 63–72 (2010).
National Clinical Guideline Centre, The management of hip fracture in adults, National Clinical Guideline Centre, London, http://www.ncgc.ac.uk, (2011).
National Institute for Health and Care Excellence (2014), “Hip Fracture: The Management of Hip Fracture in Adults”, NICE Clinical Guideline No. 124, issued June 2011, last modified March 2014.
Bretherton, C. P. & Parker, M. J. Early surgery for patients with a fracture of the hip decreases 30-day mortality. Bone Joint J. https://doi.org/10.1302/0301-620X.97B1.35041 (2015).
Orosz, G. M. et al. Association of timing of surgery for hip fracture and patient outcomes. JAMA 291(14), 1738–1743 (2004).
Deyo, R. A., Cherkin, D. C. & Ciol, M. A. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J. Clin. Epidemiol. 45(6), 613–619 (1992).
Siciliani, L. et al. (eds) Waiting Time Policies in the Health Sector: What Works? (OECD Publishing, 2013).
Mariconda, M. et al. The determinants of mortality and morbidity during the year following fracture of the hip: A prospective study. Bone Joint J. https://doi.org/10.1302/0301-620X.97B3.34504 (2015).
Vidán, M. T. et al. Causes and effects of surgical delay in patients with hip fracture: A cohort study. Ann. Intern. Med. 155(4), 226–233 (2011).
Ministry of Health and Welfare. 2015 In-depth Discharge Injury Survey Raw Data Usage Guidelines
Tsuda, Y. et al. Association between dementia and postoperative complications after hip fracture surgery in the elderly: Analysis of 87,654 patients using a national administrative database. Arch Orthop Trauma Surg. 135(11), 1511–1517 (2015).
OECD, Health at a Glance 2019: OECD Indicators, Hip and knee surgery https://www.oecd-ilibrary.org/sites/e7af69ca en/index.html?itemId=/content/component/e7af69ca-en
Health Insurance Review and Assessment Service, www.hira.or.k
Jungwoo Shin, Current Status of Health Care in the OECD Health Statistics 2020 and Improvements of Health Statistics. Health and Welfare Forum 2020.8
Flikweert, E. R. et al. Complications after hip fracture surgery: are they preventable?. Eur. J. Trauma Emerg. Surg. 44(4), 573–580 (2018).
Hagino, H. et al. Survey of hip fractures in Japan: Recent trends in prevalence and treatment. J. Orthop. Sci. 22(5), 909–914 (2017).
Orosz, G. M. et al. Hip fracture in the older patient: Reasons for delay in hospitalization and timing of surgical repair. J. Am. Geriatr. Soc. 50(8), 1336–1340 (2002).
Forni, S. et al. Mortality after hip fracture in the elderly: The role of a multidisciplinary approach and time to surgery in a retrospective observational study on 23,973 patients. Arch. Gerontol. Geriatr. 66, 13–17 (2016).
Mautalen, C. A., Vega, E. M. & Einhorn, T. A. Are the etiologies of cervical and trochanteric hip fractures different?. Bone 18(3 Suppl), 133S-137S (1996).
Lizaur-Utrilla, A. et al. Early surgery within 2 days for hip fracture is not reliable as healthcare quality indicator. Injury 47(7), 1530–1535 (2016).
Yonezawa, T., Yamazaki, K., Atsumi, T. & Obara, S. Influence of the timing of surgery on mortality and activity of hip fracture in elderly patients. J. Orthop. Sci. 14(5), 566–573 (2009).
Richards, T., Glendenning, A., Benson, D., Alexander, S. & Thati, S. The independent patient factors that affect length of stay following hip fractures. Ann R Coll Surg Engl. 100(7), 556–562 (2018).
Pailleret, C. et al. A retrospective comparison between delayed and early hip fracture surgery in patients taking clopidogrel: same total bleeding but different timing of blood transfusion. Int. Orthop. 41(9), 1839–1844 (2017).
Author information
Authors and Affiliations
Contributions
D.S., made substantial contributions to the conception and design of the work and acquired the data. S.M.K, performed data analysis. T.E.T., contributed to the interpretation of data and drafted the manuscript which was reviewed and substantively revised.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Shin, D., Tandi, T.E. & Kim, S.M. Factors influencing hip fracture surgery after two days of hospitalization using a national administrative database. Sci Rep 14, 17466 (2024). https://doi.org/10.1038/s41598-024-67747-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-67747-7
- Springer Nature Limited