Abstract
The association between composite dietary antioxidant index (CDAI) and asthma remains unclear. Our study aimed to investigate the association of CDAI with asthma in children aged 3–18 years in the United States. Cross-sectional analyses were carried out on 18,118 children aged 3–18 years old. Data was obtained from the National Health and Nutrition Examination Survey (NHANES) conducted between 2003 and 2020. The Composite Dietary Antioxidant Index (CDAI) was measured by assessing the consumption of six dietary antioxidants (vitamin A, vitamin C, vitamin E, zinc, selenium and carotenoids). The association between CDAI and asthma was explored using multivariate weighted logistic regression, subgroup analyses, and sensitivity analyses. Among the 18,118 participants, 2045 (11.3%) reported a diagnosis of asthma by a healthcare provider. In both the crude and adjusted models, the odds ratios (ORs) for asthma with CDAI were not significant. Specifically, in the fully adjusted model, the OR for T2 was 0.98 (95% CI 0.83, 1.17) and the OR for T3 was 1.00 (95% CI 0.76, 1.31). Subgroup analyses by sex, age and BMI category also showed no significant associations. Sensitivity analyses, including weighted logistic multivariate analyses adjusting for family history of asthma, confirmed the absence of a significant association between CDAI and asthma. Our study showed no significant association between CDAI and asthma in children and adolescents.
Similar content being viewed by others
Introduction
Asthma, a chronic disease marked by episodic wheezing, coughing, and breathlessness due to airway hyperresponsiveness and inflammation, is prevalent among American children. About 7.7% of adolescents under the age of 18 are affected1,2,3. This condition has significant implications for health, development, and daily life4. Furthermore, the worldwide prevalence of asthma is increasing, emphasising the importance of identifying modifiable factors associated with its onset5. In recent years, a growing body of research has highlighted the role of dietary nutrients in the prevention and comprehensive management of asthma6.
The Composite Dietary Antioxidant Index (CDAI) is an antioxidant index consisting of dietary antioxidants such as vitamins A, C, and E, carotenoids, selenium, and zinc. It is an essential tool for evaluating antioxidant-rich diets and estimating the overall dietary antioxidant intake of an individual7. CDAI has been linked to oxidative stress, inflammation biomarkers, and health outcomes, with mounting evidence supporting the association8. However, the association between the Composite Dietary Antioxidant Index (CDAI) and childhood asthma has received limited attention. Previous research has focused on the effects of individual dietary antioxidants like vitamin A, vitamin C, vitamin E, zinc, and dietary carotenoids on asthma9,10, but the combined use of these antioxidants has not been comprehensively evaluated. Previous studies of the relationship between dietary antioxidants and asthma have produced inconsistent results. Some epidemiological studies have suggested that high intakes of certain antioxidants may be associated with a reduced risk of asthma and improved lung function, while other studies have found no significant associations11,12. These differences may be due to differences in study design, population characteristics, dietary assessment methods and confounding factors. Therefore, it is imperative to conduct a comprehensive exploration of the association between dietary antioxidants and asthma.
This cross-sectional study utilized data from the National Health and Nutrition Examination Survey (NHANES), offering a representative sample size. It represents the first large-scale investigation into the association between CDAI and asthma. The aim of our study was to explore whether an association exists between CDAI and asthma in children aged 3–18 years in the U.S. By adjusting for a variety of potential confounders in weighted logistic regression modelling analyses and sensitivity analyses, we sought to provide a robust assessment of this association that could inform dietary recommendations and public health strategies for the prevention and management of asthma.
Materials and methods
Data source and study population
This cross-sectional study utilized data from the National Health and Nutrition Examination Survey (NHANES) spanning the years 2003 to 2020, conducted by the Centers for Disease Control and Prevention13. The NHANES project aimed to evaluate the health and nutritional status of non-institutionalized Americans through a stratified, multistage probability survey14. Demographic and comprehensive health information were gathered during home visits, screening, and laboratory tests administered by a mobile examination center (MEC). Approval for NHANES was obtained from the National Center for Health Statistics Ethics Review Committee, and all participants provided written informed consent before participating in the study. Additional Institutional Review Board (IRB) approval was deemed unnecessary for this secondary analysis15. The study utilized the NHANES dataset, accessible on the official NHANES website (accessed on October 1, 2023). Our study included children aged 3–18 years who completed the interview, but excluded those with missing asthma questionnaires and any variables data.
Asthma
We consulted previous references, the evaluation of asthma was based on information gathered from the questionnaire segment of the US National Health Interview Survey. NHANES collects information on asthma and related symptoms using a self-administered questionnaire16. Participants were defined as having current asthma if they answered ‘yes’ to the following two questions (by proxy if under 16 years of age): ‘Has a doctor or other health professional ever told you that you have asthma?’ and ‘Do you still have asthma?’ Controls were defined as participants who did not currently have asthma and answered ‘no’ to these questions.
The composite dietary antioxidant index (CDAI)
The NHANES dietary survey implemented a fully computerized recall system featuring standardized questions and response options customized for food-related inquiries. This methodology was devised to guarantee a meticulous and precise collection of dietary information. Accurate dietary information for each participant was obtained through the utilization of the Continuing Survey of Food Intakes by Individuals (CSFII) and the Automated Multiple-Pass Method (AMPM)17. The NHANES Dietary Interviewers Procedure Manuals were utilized as a comprehensive guide, offering detailed insights into the dietary survey methodology.
In the dietary survey conducted as part of NHANES, participants were asked to recall details of their diet over the previous 24 h. The study incorporated six dietary antioxidants: vitamin A, vitamin C, vitamin E, zinc, selenium, and carotenoids. The calculations of dietary antioxidant intake excluded antioxidants from supplements, medications, or regular drinking water. To evaluate the collective exposure from dietary antioxidant intake, we employed a modified version of the Dietary Antioxidant Composite Index (CDAI) developed by Wright et al.7,18 These values were first normalised by subtraction of the mean value and then division by the standard deviation (SD):
Finally, the CDAI was categorized into tertiles for analysis. Tertile 1 (T1) served as the reference category, indicating CDAI below the 33rd percentile. Tertile 2 (T2) included participants with a CDAI between the 33rd and 67th percentiles, while tertile 3 (T3) included participants with a CDAI above the 67th percentile.
Covariates
We aimed to minimise potential confounding biases in the analyses by selecting covariates based on previous research and clinical validity. Selected covariables included sex, race and ethnicity, poverty income ratio (PIR), body mass index category (BMIC), familial asthma, white blood cell count (WBC), eosinophil percentage (EOPC), total energy/protein/sugar/carbohydrate/fibre/fat intake and serum cotinine. A detailed description of the measurement procedures can be found at https://www.cdc.gov/nchs/nhanes and has been accessed on 1 October, 2023. In particular, race and ethnicity (Mexican–American, Other Hispanic, non-Hispanic White, non-Hispanic Black, and Other race) were collected13. The PIR was determined by dividing family (or individual) income by the poverty threshold for the survey year. In accordance with a US government report, family income was classified into three categories based on PIR: low (PIR ≤ 1.3), medium (PIR > 1.3–3.5), and high (PIR > 3.5)19. For the BMI Category (BMIC): underweight (BMI < 5th percentile), normal weight (BMI 5th-85th percentile), overweight (BMI 85-95th percentile) and obese (BMI ≥ 95th percentile). Blood samples from all participants underwent complete blood count (CBC) using the Beckman Coulter DxH 800 instrument at the NHANES MEC. Cotinine, a nicotine metabolite, gauged secondhand smoke exposure in those aged 3 years and older. Serum cotinine levels were determined using isotope dilution high-performance liquid chromatography/atmospheric pressure chemical ionization tandem mass spectrometry (ID HPLC-APCI MS/MS). To reduce bias from missing data, we excluded samples with missing covariates (PIR, WBC, EOPC, BMIC, familial asthma, and serum cotinine).
Statistical analysis
Sample weights, strata and primary sampling units were used in accordance with NHANES analytical guidelines to account for the complex survey design. Differences in baseline characteristics between the asthma and non-asthma groups were compared using the independent samples t-test for continuous variables and the χ2 test for categorical variables. Categorical data were expressed as unweighted numbers (weighted percentages), whereas continuous data were expressed as means (standard error [SE]). NHANES provides a set of special weights (WTDRD1) for an analysis using data from the first 24-h dietary recall. The WTDRD1 weights were constructed by taking the MEC sample weights (WTMEC2YR) and further adjusting for additional non-response and differential allocation by day of the week for dietary recall. Further details can be found elsewhere: https://wwwn.cdc.gov/Nchs/Nhanes/2003-2004/DR1IFF_D.htm#WTDRD120. Multivariate weighted logistic regression analyses were performed for the association between CDAI and asthma, and 95% confidence intervals (CIs) and odds ratios (ORs) were calculated. Three adjustment models were adjusted for in the multivariable logistic regression analysis: Model 1 was unadjusted; Model 2 included gender, age, race and ethnicity, PIR, BMIC, and serum cotinine. Model 3 was further adjusted for variables such as WBC, EOPC, total energy intake, total protein intake, total sugar intake, total carbohydrate intake, total fibre intake, total fat intake, and cycle year.
Additionally, we performed subgroup analyses employing stratified logistic regression models. The interaction across subgroups was assessed using the likelihood ratio test. To improve the reliability of our findings, we performed sensitivity analyses, first assessing the association between CDAI and asthma using unweighted Logstic multifactor analysis of the full data series and adjusting for confounders. We then added the covariate of familial asthma (only data between 2007 and 2020) to exclude missing variables, and finally included 10,520 participants in the analyses and assessed the association between CDAI and asthma using weighted Logstic multifactorial analyses, adjusting for confounders and familial asthma. Eventually, multiple estimation of covariates with missing data (PIR, WBC, EOPC, BMIC, familial asthma and serum cotinine) was used to minimise the bias that missing data may introduce into the results. Specifically, the MICE algorithm described by Van Buuren and Groothuis Oudshoorn, using the full conditional specification (FCS) (2011, https://doi.org/10.18637/iss.v045i03) was used. These data were finally used to assess the association between CDAI and asthma.
No prespecified statistical power estimates were performed, as sample size was determined solely on the basis of available data. Analyses were performed using the R statistical software package (http://www.R-project.org, The R Foundation) and Free Statistics software version 1.9.221. For all participants, descriptive statistics were performed using two-tailed tests with a significance level of P < 0.05.
Ethical approval
Ethical review and approval for this study were not required as it involved a secondary analysis and did not require additional institutional review board approval. The National Health and Nutrition Examination Survey (NHANES) was approved by the Ethics Review Committee of the National Center for Health Statistics (NCHS). Written informed consent was obtained from all participants before their participation in the survey. Statement attesting to informed consent from a parent and/or legal guardian for study participation: In accordance with the ethical guidelines for research involving minors, informed consent was obtained from a parent or legal guardian for all study participants. Prior to participation, parents or guardians provided documented signed consent, and minors aged 7–15 provided additional signed assent. Copies of the signed consent forms and informative brochures were given to all participants and their guardians. The detailed consent process follows the established procedures and complies with all federal regulations and ethical standards. For more details, please see the NHANES website: https://www.cdc.gov/nchs/nhanes/irba98.htm and https://www.cdc.gov/nchs/data/series/sr_02/sr02_163.pdf.
Impact statement
This study provides a comprehensive evaluation of the association between the Composite Dietary Antioxidant Index (CDAI) and asthma prevalence. Despite the well-documented role of oxidative stress and inflammation in asthma pathophysiology, our findings reveal no significant relationship between overall dietary antioxidant intake and asthma risk. This null association persisted even after rigorous adjustments for confounding factors and sensitivity analyses, including familial asthma history. These results suggest that simply increasing dietary antioxidant intake may not be sufficient for asthma prevention. This study underscores the importance of considering the complex interplay between diet, genetics, and environmental factors in asthma research and may guide future dietary recommendations and public health strategies for asthma management. Further research is needed to explore these interactions in greater detail and to identify more effective dietary interventions for asthma prevention and control.
Results
Study population and baseline characteristics
A total of 65,046 participants were successfully interviewed between 2003 and 2020 in this study. We excluded participants over 19 years of age and under 3 years of age (n = 38,851), those with missing asthma surveys (n = 78), and those with missing data on dietary intake and covariates (n = 7999). Therefore, 18,118 participants were included in the final analysis, of whom 2045 (11.3%) had asthma (Fig. 1). Baseline characteristics of all subjects by asthma and non-asthma status are shown in Table 1. Statistically significant differences were observed between the asthma and non-asthma groups in terms of age, race and ethnicity, PIR, BMIC, WBC, EOPC, serum cotinine, total energy/protein/carbohydrate/vitamin E/zinc/selenium intake (p < 0.05).The asthma group had a mean age of 11.0 years (non-asthma: 12.0 years, p < 0.001) and 51.6% were male (non-asthma: 52.57%, p = 0.6205). However, no statistically significant differences (p > 0.05) were observed with regard to cycle year/total sugars/total fiber/total fat/vitamin A/vitamin C/carotenoids and CDAI (Table 1).
Association between CDAI and asthma
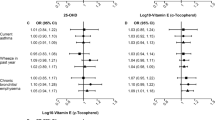
In the weighted multivariate logistic regression analyses stratifying the Comprehensive Dietary Antioxidant Index (CDAI) into tertiles, there was no statistically significant association between CDAI and asthma, even after careful adjustment for potential confounders. In the unadjusted model, the odds ratios (ORs) for asthma in the second (T2) and third (T3) tertiles compared with the reference tertile (T1) were 1.02 (95% CI 0.86, 1.20; P = 0.848) and 1.14 (95% CI 0.95, 1.38; P = 0.153), respectively. Adjustments for potential confounders in models 2 and 3 did not significantly change these results. In model 3, which included comprehensive adjustments, the ORs for T2 and T3 were 0.98 (95% CI 0.83, 1.17; P = 0.862) and 1.00 (95% CI 0.76, 1.31; P = 0.994), respectively. P-values for trend tests were not significant in all models, indicating no trend between CDAI and asthma prevalence (Table 2).
Stratified analyses based on additional variables and sensitivity analysis
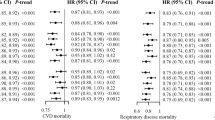
The analyses showed no significant association between the combined dietary antioxidant index (CDAI) and asthma across subgroups. Subgroup analyses by sex, age, and body mass index category (BMIC) also showed no significant associations, except for a potential interaction of sex (P = 0.039 for interaction). Overall, increased levels of dietary antioxidants did not significantly affect the likelihood of asthma development as measured by the CDAI (Fig. 2).
Sensitivity analyses were performed to assess the robustness of the association between the Composite Dietary Antioxidant Index (CDAI) and asthma prevalence. First, a logistic multivariate analysis was performed on the complete unweighted data set, adjusting for potential confounders. The results showed no statistically significant association between CDAI and asthma after model adjustment (Table S1). The analysis was then refined to include family history of asthma, a variable only available for the period 2007–2020. This adjustment reduced the data set to 10,520 participants. A weighted logistic multivariate analysis was then performed, adjusting for confounders and family history of asthma. The results remained consistent, with no statistically significant association found between CDAI and asthma prevalence (Table S2). Finally, using the dataset after multiple interpolation and adjusting for confounders, we found that CDAI remained uncorrelated with asthma (Table S3).
Discussion
This cross-sectional study analysed representative population data of children and adolescents aged 3–18 years in the United States, including 9242 males and 8876 females. Our analyses across models and subgroups consistently showed no significant association between higher CDAI scores and asthma in children and adolescents, a finding that remained robust to sensitivity analyses with various adjustments for potential confounders.
Oxidative stress arises due to a disparity between the synthesis of antioxidants and pro-oxidants, leading to harm to tissues and organs. Reactive oxygen species (ROS) buildup can cause the oxidation of DNA, proteins, carbohydrates, and lipids, giving way to cell apoptosis and organ malfunction22. As an extrinsic element, diet operates the plasma redox status by averting ROS and reactive nitrogen species. To maintain a stable biochemical redox state, antioxidative agents may intercept oxidants and thus prevent oxidative stress23. The use of exogenous antioxidants has the potential to prevent oxidative stress24. This study looked at dietary antioxidants: vitamins A, C, E, selenium, zinc and carotenoids. Previous research has looked at individual nutrient-asthma associations, causality and mechanisms. A Korean study of 6293 adults (20–49 years) found a inverse association between dietary vitamin C and asthma prevalence in subjects with elevated hs-CRP (≥ 1 mg/L). However, this association wasn’t significant in those with hs-CRP < 1 mg/L. Participants with vitamin C ≥ 75 mg/day had an OR for asthma of 1.44 (95% CI 0.66–3.16), while vitamin A showed no association9. Carotenoids are found in many fruits, vegetables and algae. Previous studies have reported associations between carotenoids and asthma25. Research by Zhang et al. suggests that dietary intake of carotenoids (dietary α-carotene, dietary β-carotene, dietary β-cryptoxanthin, total lutein + zeaxanthin, total lycopene) in US adults may reduce the incidence of asthma and prevent its occurrence11. In addition, increased consumption of carotenoids, tomatoes and carotenoid-rich vegetables was associated with a lower risk of asthma in a cross-sectional study of 68,535 women26. Our study focuses on the Composite Dietary Antioxidant Index (CDAI), which provides a comprehensive measure of an individual's antioxidant status by incorporating several dietary antioxidants with anti-inflammatory properties27. Previous research has used the Total Antioxidant Capacity (TAC) method to study the combined antioxidant effects of the diet. For example, Elena Rodríguez-Rodríguez found that higher TAC, measured using methods such as ferric reducing antioxidant power (FRAP), Trolox equivalent antioxidant capacity (TEAC) and radical-trapping antioxidant parameter (TRAP), significantly reduced the likelihood of asthma attacks in children28. A study by A Gref et al. in the Swedish birth cohort BAMSE found no significant association between TAC and asthma incidence, but observed a significant inverse association with allergic asthma (OR 0.57, 95% CI 0.34–0.94)29. These findings provide valuable insights for further research and highlight the need for standardised assessment of dietary antioxidant capacity in future studies.
Asthma, a chronic condition marked by airway inflammation and hyperresponsiveness, involves a crucial interplay with composite dietary antioxidants. These antioxidants play an essential role in mitigating oxidative stress damage and fostering overall health30. Serving as bioactive compounds in food, antioxidants possess the capacity to neutralize free radicals and diminish oxidative damage31. Vitamin C, vitamin E, selenium, and other antioxidants are generally considered the primary components of CDAI. Currently, oxidative stress-induced physiological damage, triggered by reactive oxygen species (ROS), is believed to play a significant role in the chronic inflammation associated with asthma32. Carotenoids, as dietary antioxidants, have antioxidant properties that reduce ROS activity and thereby reduce airway inflammation in asthma patients while improving lung function. Previous studies have shown that β-carotene can scavenge highly reactive free radicals such as superoxide anions, releasing electrons to reduce free radical molecules and prevent oxidative damage33. In addition, in animal models of allergic asthma, lycopene inhibits Th2 responses and reduces lung eosinophil infiltration and egg-white-induced airway inflammation34. In addition, selenium plays a role in antioxidant capacity. Selenium is a component of several enzymes involved in the regulation of intracellular redox balance and antioxidant pressure. These enzymes, namely glutathione peroxidase (GPx), selenium-binding protein P (SelP), and selenium-binding protein W (SelW). Selenium serves as a cofactor for these enzymes, amplifying their antioxidant capabilities and contributing to overall cellular protection against oxidative damage35,36. Zinc enhances the phagocytic, chemotactic and bactericidal functions of phagocytes, plays a crucial role in maintaining the integrity of epithelial cells and tissues, and has antioxidant effects such as scavenging free radicals and protecting cell membranes37.
In this cross-sectional survey of 18,118 participants aged 3–18 years, we examined the relationship between the CDAI and asthma, using weighting and different models to adjust for confounders. In particular, higher total energy intake was associated with higher CDAI values, and as energy may be an important potential confounder influencing the relationship between CDAI and asthma38, we adjusted for it in model, and finally the results showed no significant association between CDAI and asthma. This suggests that adjusting for dietary antioxidant levels does not have a significant effect on the management of asthma. Our findings are consistent with several previous studies that have investigated the role of dietary antioxidants in asthma28,29,39,40. Although some studies suggest that antioxidants may reduce the risk of asthma through their anti-inflammatory properties, the evidence is inconclusive11. Many observational studies have failed to find a significant protective effect of dietary antioxidants on the prevalence or severity of asthma41,42. Our study adds to this evidence by providing a reliable dietary antioxidant index (CDAI) and a comprehensive analysis of a large representative sample.
There are several possible explanations for the lack of association observed in our study. First, it is possible that dietary antioxidants are not sufficient to significantly influence asthma risk. Asthma is a complex, multifactorial disease influenced by genetic, environmental and lifestyle factors43. Interactions between these factors may mask the potential protective effects of dietary antioxidants. Second, measurement limitations may also lead to negative results: the CDAI, although comprehensive, may not capture all relevant dietary antioxidants or their bioavailability and interactions in vivo. In addition, dietary intake data are often subject to recall bias and inaccuracies, which may attenuate observed associations. Finally, the timing and duration of antioxidant intake are likely to be important factors. Short-term dietary assessments may not fully reflect long-term dietary habits, which are more relevant to chronic diseases such as asthma. Longitudinal studies with detailed dietary records may provide additional insights into the potential long-term effects of antioxidants on asthma risk.
This study has several strengths, including the use of a large, nationally representative sample and a composite index (CDAI) to assess dietary antioxidant intake. The use of weighting and multiple models to adjust for a wide range of potential confounders and the inclusion of sensitivity analyses increased the robustness of our findings. Nonetheless, we must take into account limitations of our research. The cross-sectional design of the study limited the ability to infer causality. Despite rigorous analyses, residual confounding and reporting bias may remain. In addition, reliance on self-reported dietary data may introduce recall bias and measurement error, and future studies need prospective designs and objective measures of antioxidant intake and biomarkers. Given the variations in body composition, lifestyle, and dietary habits among residents of different countries and regions, it is essential to conduct multicenter randomized controlled trials to validate our research findings.
In conclusion, our study found no significant association between CDAI and asthma in children and adolescents aged 3–18 years in the U.S. Further research is needed to explore the complex interactions between dietary, genetic and environmental factors and to identify potential dietary interventions for the prevention and management of asthma.
Data availability
Publicly available datasets are available online for this study. The repository names and accession numbers are available online at http://www.cdc.gov/nchs/nhanes.htm (accessed on 1 October 2023).
References
Lancet, T. Asthma in US children. Lancet 391(10121), 632. https://doi.org/10.1016/S0140-6736(18)30258-7 (2018).
Zanobetti, A. et al. Childhood asthma incidence, early and persistent wheeze, and neighborhood socioeconomic factors in the ECHO/CREW consortium. JAMA Pediatr. 176(8), 759–767. https://doi.org/10.1001/jamapediatrics.2022.1446 (2022).
CDC. Most recent asthma data available from CDC (Centers for Disease Control and Prevention. Published March 25, 2019, accessed October 22, 2023); https://www.cdc.gov/asthma/most_recent_data.htm
Sullivan, P. W. et al. The national burden of poorly controlled asthma, school absence and parental work loss among school-aged children in the United States. J. Asthma 55(6), 659–667. https://doi.org/10.1080/02770903.2017.1350972 (2018).
2023 GINA Main Report (Global Initiative for Asthma—GINA, accessed December 1, 2023); https://ginasthma.org/2023-gina-main-report/
Nuzzi, G. et al. Primary Prevention of pediatric asthma through nutritional interventions. Nutrients 14(4), 754. https://doi.org/10.3390/nu14040754 (2022).
Wright, M. E. et al. Development of a comprehensive dietary antioxidant index and application to lung cancer risk in a cohort of male smokers. Am. J. Epidemiol. 160(1), 68–76. https://doi.org/10.1093/aje/kwh173 (2004).
Luu, H. N. et al. Are dietary antioxidant intake indices correlated to oxidative stress and inflammatory marker levels?. Antioxid. Redox Signal. 22(11), 951–959. https://doi.org/10.1089/ars.2014.6212 (2015).
García-García, C., Kim, M. & Baik, I. Associations of dietary vitamin A and C intake with asthma, allergic rhinitis, and allergic respiratory diseases. Nutr. Res. Pract. 17(5), 997–1006. https://doi.org/10.4162/nrp.2023.17.5.997 (2023).
Zhang, W., Li, W. & Du, J. Association between dietary carotenoid intakes and the risk of asthma in adults: A cross-sectional study of NHANES, 2007–2012. BMJ Open. 12(6), e052320. https://doi.org/10.1136/bmjopen-2021-052320 (2022).
Moreno-Macias, H. & Romieu, I. Effects of antioxidant supplements and nutrients on patients with asthma and allergies. J. Allergy Clin. Immunol. 133(5), 1237–1244. https://doi.org/10.1016/j.jaci.2014.03.020 (2014).
Chen, M., Sun, Y. & Wu, Y. Lower circulating zinc and selenium levels are associated with an increased risk of asthma: Evidence from a meta-analysis. Public Health Nutr. 23(9), 1555. https://doi.org/10.1017/S1368980019003021 (2020).
NHANES Questionnaires, Datasets, and Related Documentation. Accessed June 29, 2023. https://wwwn.cdc.gov/nchs/nhanes/Default.aspx
Zipf, G. et al. National health and nutrition examination survey: Plan and operations, 1999–2010. Vital Health Stat. 1(56), 1–37 (2013).
NHANES—NCHS Research Ethics Review Board Approval (Published August 25, 2022. accessed June 30, 2023); https://www.cdc.gov/nchs/nhanes/irba98.htm
Ke, J., Qiu, F., Fan, W. & Wei, S. Associations of complete blood cell count-derived inflammatory biomarkers with asthma and mortality in adults: A population-based study. Front. Immunol. 14, 1205687. https://doi.org/10.3389/fimmu.2023.1205687 (2023).
FoodData Central (accessed June 26, 2023); https://fdc.nal.usda.gov/
Wu, D. et al. Association between composite dietary antioxidant index and handgrip strength in American adults: Data from National Health and Nutrition Examination Survey (NHANES, 2011–2014). Front. Nutr. 10, 1147869. https://doi.org/10.3389/fnut.2023.1147869 (2023).
What We Eat In America (WWEIA) Database | Ag Data Commons (Accessed June 30, 2023); https://data.nal.usda.gov/dataset/what-we-eat-america-wweia-database
Zhang, L. et al. Multivitamin consumption and childhood asthma: A cross-sectional study of the NHANES database. BMC Pediatr. 24, 84. https://doi.org/10.1186/s12887-024-04540-5 (2024).
Yang, Q. et al. Association between preadmission metformin use and outcomes in intensive care unit patients with sepsis and type 2 diabetes: A cohort study. Front Med. 8, 640785. https://doi.org/10.3389/fmed.2021.640785 (2021).
Roumeliotis, S., Roumeliotis, A., Dounousi, E., Eleftheriadis, T. & Liakopoulos, V. Dietary antioxidant supplements and uric acid in chronic kidney disease: A review. Nutrients 11(8), 1911. https://doi.org/10.3390/nu11081911 (2019).
Demmig-Adams, B. & Adams, W. W. Antioxidants in photosynthesis and human nutrition. Science 298(5601), 2149–2153. https://doi.org/10.1126/science.1078002 (2002).
Liakopoulos, V., Roumeliotis, S., Bozikas, A., Eleftheriadis, T. & Dounousi, E. Antioxidant supplementation in renal replacement therapy patients: Is there evidence?. Oxid. Med. Cell Longev. 2019, 9109473. https://doi.org/10.1155/2019/9109473 (2019).
Manochkumar, J., Singh, A., Efferth, T. & Ramamoorthy, S. Untapping the protective role of carotenoids against respiratory diseases. Phytomedicine 104, 154286. https://doi.org/10.1016/j.phymed.2022.154286 (2022).
Romieu, I. et al. Fruit and vegetable intakes and asthma in the E3N study. Thorax 61(3), 209–215. https://doi.org/10.1136/thx.2004.039123 (2006).
Ma, R. et al. Association between composite dietary antioxidant index and coronary heart disease among US adults: A cross-sectional analysis. BMC Public Health 23, 2426. https://doi.org/10.1186/s12889-023-17373-1 (2023).
Rodríguez-Rodríguez, E., Ortega, R. M., González-Rodríguez, L. G., Peñas-Ruiz, C. & Rodríguez-Rodríguez, P. Dietary total antioxidant capacity and current asthma in Spanish schoolchildren: A case control-control study. Eur. J. Pediatr. 173(4), 517–523. https://doi.org/10.1007/s00431-013-2197-y (2014).
Gref, A. et al. Dietary total antioxidant capacity in early school age and subsequent allergic disease. Clin. Exp. Allergy 47(6), 751–759. https://doi.org/10.1111/cea.12911 (2017).
Aleksandrova, K., Koelman, L. & Rodrigues, C. E. Dietary patterns and biomarkers of oxidative stress and inflammation: A systematic review of observational and intervention studies. Redox Biol. 42, 101869. https://doi.org/10.1016/j.redox.2021.101869 (2021).
Zhong, Q. et al. The antioxidant activity of polysaccharides derived from marine organisms: An overview. Mar. Drugs. 17(12), 674. https://doi.org/10.3390/md17120674 (2019).
Checa, J. & Aran, J. M. Airway redox homeostasis and inflammation gone awry: From molecular pathogenesis to emerging therapeutics in respiratory pathology. Int. J. Mol. Sci. 21(23), 9317. https://doi.org/10.3390/ijms21239317 (2020).
Guilleminault, L. et al. Diet and asthma: Is it time to adapt our message?. Nutrients 9(11), 1227. https://doi.org/10.3390/nu9111227 (2017).
Hazlewood, L. C., Wood, L. G., Hansbro, P. M. & Foster, P. S. Dietary lycopene supplementation suppresses Th2 responses and lung eosinophilia in a mouse model of allergic asthma. J. Nutr. Biochem. 22(1), 95–100. https://doi.org/10.1016/j.jnutbio.2009.12.003 (2011).
Cai, Z., Zhang, J. & Li, H. Selenium, aging and aging-related diseases. Aging Clin. Exp. Res. 31(8), 1035–1047. https://doi.org/10.1007/s40520-018-1086-7 (2019).
Bjørklund, G. et al. Selenium: An antioxidant with a critical role in anti-aging. Molecules 27(19), 6613. https://doi.org/10.3390/molecules27196613 (2022).
袁皛, 钱素云. 锌缺乏与感染性疾病相关研究进展. 中华实用儿科临床杂志. 2012;27(10):789–791. https://doi.org/10.3969/j.issn.1003-515X.2012.10.025
Wood, L. G. Diet, obesity, and asthma. Ann. Am. Thorac. Soc. 14(Supplement_5), S332–S338. https://doi.org/10.1513/AnnalsATS.201702-124AW (2017).
Hu, J., Sang, J., Hao, F. & Liu, L. Association between vitamin a and asthma: A meta-analysis with trial sequential analysis. Front. Pharmacol. 14, 1100002. https://doi.org/10.3389/fphar.2023.1100002 (2023).
Burney, P. et al. A case-control study of the relation between plasma selenium and asthma in European populations: A GAL2EN project. Allergy 63(7), 865–871. https://doi.org/10.1111/j.1398-9995.2008.01716.x (2008).
Bishopp, A. et al. Biomarkers of oxidative stress and antioxidants in severe asthma: A prospective case-control study. Ann. Allergy Asthma Immunol. 118(4), 445–451. https://doi.org/10.1016/j.anai.2017.02.004 (2017).
AbdulWahab, A., Zeidan, A., Avades, T., Chandra, P. & Soliman, A. Serum zinc level in asthmatic and non-asthmatic school children. Children (Basel) 5(3), 42. https://doi.org/10.3390/children5030042 (2018).
Wang, J. et al. Age-related clinical characteristics, inflammatory features, phenotypes, and treatment response in asthma. J. Allergy Clin. Immunol. Pract. 11(1), 210-219.e3. https://doi.org/10.1016/j.jaip.2022.09.029 (2023).
Funding
This research did not receive any specific grants from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Z.T., X.L., Y.H., X.Z. contributed to the study design, data collection, analysis, interpretation of results, and manuscript preparation. All the authors have read and approved the final version of the manuscript. Conceptualization, Z.Y., Y.J. and X.L.; Data curation, X.Y., X.L.; Formal analysis, Z.Y., Y.J. and X.Y.; Methodology: Z.Y., Y.J., X.Y. and X.L.; Writing original draft: Z.Y.; Writing review and editing: X.L., Y.J., and X.Y. All authors have read and agreed to the published version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Tian, Z., Li, X., Han, Y. et al. The association between the composite dietary antioxidant index and asthma in US children aged 3–18 years: a cross-sectional study from NHANES. Sci Rep 14, 17204 (2024). https://doi.org/10.1038/s41598-024-67702-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-67702-6
- Springer Nature Limited