Abstract
This study aimed to explore the relationship between shift-working nurses’ social jetlag and body mass index (BMI) and provide a theoretical basis for nursing managers to develop appropriate health interventions. Shift work is unavoidable in nursing and is associated with circadian rhythm disorders. Social jetlag is prevalent in shift-working nurses and is associated with adverse health outcomes (particularly metabolism-related indicators). BMI is a significant metabolic indicator, and research has demonstrated its effectiveness in predicting the formation of metabolic syndrome. The relationship between social jetlag and BMI can be explained by considering physiological, psychological, and behavioral factors. However, most studies on social jetlag and health status are focused on non-shift nurse populations, with fewer studies on shift workers. Five tertiary hospitals located at similar latitudes in Southwest China were selected for the study. We surveyed 429 shift-working nurses using sociodemographic data, the Munich Chronotype Questionnaire for Shift Workers, and BMI. The restricted cubic spline model was used to analyze the relationship between social jetlag and BMI among shift-working nurses, and segmented linear regression was performed around the inflection point using multiple linear regression analysis. The results revealed that social jetlag (82.0 [85.0] min) was experienced by 64.6% of the shift-working nurses. After controlling for confounding variables, the model with seven knots had the lowest accepted Akaike information criterion value, and there was a U-shaped relationship between shift-working nurses’ BMI and social jetlag in this model; its inflection (lowest) point of 20.7 was considered the cut-off point. Segmented regression showed that for BMI < 20.7, BMI was significantly negative with standardized social jetlag; whereas with BMI > 20.7, BMI was significantly positive with standardized social jetlag. BMI has a U-shaped relationship with social jetlag, and attention should be paid to overweight or underweight shift-working nurses to detect early circadian rhythm disorder. Shift-working nurses with high social jetlag tended to have higher/lower BMI, which should be further investigated in the future, to minimize metabolic diseases among them.
Similar content being viewed by others
Introduction
Shift work in hospitals providing 24-h care service is inevitable because of continued nursing need (López-Soto in drugi33). A large body of evidence suggests that long-term shiftwork can lead to circadian rhythm disorder (Boivin in drugi3, Hulsegge in drugi21, Rosa in drugi45). Rhythmic disorders can result in infectious diseases, metabolic disorders, cardiovascular diseases, neurodegenerative diseases, and other systemic diseases, ultimately impacting an individual's lifespan (Fitzgerald in drugi13, Yang in drugi54). Social jetlag has emerged as a novel indicator of persistent circadian rhythm disorders. The concept of social jetlag was initially introduced by Wittmann (Wittmann in drugi53). They defined social jetlag as a circadian rhythm disorder arising from the difference between sleep–wake patterns on workdays and rest days. Caliandro et al., further elucidated that individuals possess social characteristics. Most individuals find themselves constrained by work or study commitment, which necessitates adherence to a predetermined schedule. Conversely, during periods of rest, individuals tend to exhibit a sleep–wake pattern that aligns with their inherent circadian rhythm preferences. This misalignment between contemporary lifestyles and an individual's biological clock is commonly referred to as social jetlag (Caliandro in drugi5). Wittmann et al.53 conducted an additional quantification of the assessment of social jetlag and utilized the absolute difference between the midpoint of sleep on days of rest (MSF) and the midpoint of sleep on weekdays (MSW) (Wittmann in drugi53). The former is based on an individual's biological clock, whereas the latter is influenced by societal factors. The severity of social jetlag increases as the difference between the two sleep midpoints widens. The scheduling of changeable shifts and the frequent rotation of shifts in the context of shift-working nurses contribute to the regular alteration of their sleep midpoint (Uekata in drugi52), which gives rise to a notable inclination toward social jetlag.
Social jetlag can be assessed using both subjective and objective measurements. Objective measurements are used to determine the midpoint of sleep by assessing specific indicators of circadian rhythms, such as the degree of melatonin production, known as dim light melatonin onset (DLMO), and core body temperature (CBT) (Shawa in drugi47). Nevertheless, objective measurements are often associated with a multitude of confounding variables, substantial expenses, and limited availability and have been used sparingly in academic investigations. Subjective measurements depend on the use of questionnaires, Roenneberg and other researchers (Roenneberg in drugi41) built the Munich Chronotype Questionnaire (MCTQ) as an instrument of assessing an individual's chronotype and social jetlag, being the most commonly used (Roenneberg in drugi44). This questionnaire primarily assesses the midpoint of sleep time and sleep duration while signifying social jetlag by calculating the absolute difference between the midpoint of sleep on weekdays and rest days, and it was demonstrated a strong correlation between questionnaire responses and various measures such as sleep logs, wrist dynamics, and physiological rhythms. Similarly, Burgess and Eastman investigated the predictive capability of the midpoint of the MCTQ in estimating melatonin release levels under dim light conditions, even when individuals had irregular sleep schedules (Burgess in Eastman4). Nevertheless, the utilization of this survey was primarily limited to those with stable work schedules, posing challenges in assessing shift workers with highly unpredictable work patterns. Juda et al.25 introduced the MCTQ for shift workers (MCTQshift) as a tool to assess the impact of social jetlag on shift workers (Juda in drugi25). This questionnaire employed six visual aids and seven questions to evaluate the sleep patterns of the participants at different time intervals during various shift schedules and on days off. The formula for calculating the social jetlag of shift workers is as follows: it involves summing the product of each shift social jetlag and the corresponding number of shifts, and then dividing this sum by the total number of days over which the computation is performed. Cheng et al., conducted a study in which they adapted the MCTQshift to suit the Chinese cultural context. Subsequently, they assessed the applicability of this scale on a sample of 288 shift workers. Cheng and Hang concluded that the scale had a high level of reliability and validity (Cheng in Hang8).
Currently, the definitive aspects of social jetlag among shift workers are unclear. Typically, a 1-h difference is employed as a benchmark in studies involving the general adult population. Specifically, when the absolute value of the difference between the midpoints of sleep was less than 1 h, it was indicative of the absence of a social jetlag. Conversely, if the absolute value was equal to or greater than 1 h, it signified the presence of social jetlag. Survey findings on the incidence of social jetlag among people in different nations are inconsistent. An Australian study revealed that 31.1% of individuals without underlying health conditions experienced a social jetlag exceeding 1 h (Lang in drugi27). In Brazil, a study revealed that 14% of participants experienced a social jetlag ranging from one to 2 h, whereas 10% reported a social jetlag equal to or above 2 h (Mota in drugi36). From the Netherlands, a study reported that 63% of the participants had a social jetlag of over 1 h (Rutters in drugi46). A comprehensive study conducted in Europe also observed that social jetlag has the potential to impact the everyday routines of approximately 70% of the European population (Roenneberg in drugi40). There is a scarcity of research on social jetlag in the nursing profession. To address this gap, Hulsegge et al., conducted a study of 197 nurses, consisting of 120 shift workers and 74 non-shift workers. The findings revealed that non-shift workers experienced a social jetlag of 1.0 ± 1.4 h, but shift workers experienced a social jetlag of 3.1 ± 3.0 h (P < 0.05) (Hulsegge in drugi21. Lee et al. conducted a study with a sample of 190 shift-working nurses in South Korea. The study indicated that the average social jetlag among shift workers was 4 h 29 min ± 1 h 14 min. Additionally, 25.3% of shift workers experienced social jetlag exceeding 5 h 13 min (Lee in Jang28). Hwang et al., examined 183 shift-working nurses in South Korea and reported that the average social jetlag among these individuals was calculated to be 3 h 31 min ± 1 h 19 min (Hwang in drugi22). Uekata et al., examined 1,253 shift-working nurses and midwives in Japan and reported an average social jetlag of 1 h 30 min of the shift timings was 16 h, an average social jetlag of 1 h 20 min of the shift timings was 12.5 h. In contrast, shift-working nurses with an 8 h shift timing had an average social jetlag of 1h, whereas those with working day shifts had an average social jetlag of 45 min (Uekata in drugi52). The data indicate a potential correlation between the timing of shift work and social jetlag among shift-working nurses.
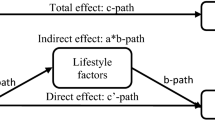
The presence of a significant social jetlag can have adverse effects on several physiological systems of individuals who work in shifts, particularly in relation to metabolic markers. In a study conducted by Hwang et al., the average duration of social jetlag was 3 h 31 min. Additionally, the research revealed that the likelihood of detecting obesity in shift workers with a social jetlag exceeding 3 h 31 min remained 8.44 times higher even after accounting for potential confounding variables (95% CI: 1.66–42.99)(Hwang in drugi22). Similarly, Garrido et al., examined 36 overweight female nurses who worked shifts and found a positive correlation between increased social jetlag and higher levels of HDL and cholesterol (Garrido in drugi14). Furthermore, McMahon et al., observed a significant correlation between elevated levels of social jetlag and the onset of major chronic ailments such as obesity, metabolic syndrome, and heart disease (Mcmahon in drugi34). The physiological, psychological, and behavioural factors are the mechanisms that associate social jetlag and abnormal BMI. High levels of social jetlag can lead to abnormal release of melatonin (González in drugi16) and change of circadian genes' rhythm (González in drugi16, Takahashi in drugi51). High level of social jetlag can resulting in increased levels of perceived stress, anxiety and depression (Ciobanu in drugi9, Jokubauskas in drugi24). Individuals with high social jetlag tend to show decreased physical activity and adopt bad eating habits (Huang in drugi19, Kyung in drugi26). These physiological, psychological, and behavioural alterations can all lead to abnormal BMI. Notably, the manifestation of these diseases may take a while, perhaps spanning many decades. The mean age of nurses in shiftwork tended to be lower, and it is worth noting that even nurses without metabolism-related disorders may still face significant risks. Thus, the potential negative impact of social jetlag on nurses’ metabolic function during shift work may increase.
Although the existing body of research has extensively examined the effects of social jetlag on health (Gentry in drugi15, Roenneberg in drugi43), most studies have concentrated on individuals who do not work in shift-based occupations (Zhang in drugi56). Consequently, there is a relative scarcity of information on the correlation between social jetlag and body mass index (BMI), particularly in relation to shift work, among those who with a more severe degree of social jetlag. Prior research has established a correlation between social jetlag and higher body weight or obesity (Li in drugi29, Liang in drugi30, Parsons in drugi39), warranting further investigation into the potential link between social jetlag and lower body weight. Prior studies indicate that a high level of social jetlag may be related to unhealthy habits, such as poor dietary choices and lack of physical activity (Drăgoi in drugi10, Huang in drugi20. These variables may contribute to nutritional imbalances (Mititelu in drugi35), which can lead to individuals becoming underweight (Oshita in drugi38). Thus, a high level of social jetlag might lead to BMI polarization, either towards being overweight or underweight, whereas a moderate level of social jetlag is connected with a predisposition towards maintaining a normal BMI. This study employed a cross-sectional design to evaluate the social jetlag experienced by nurses working shift schedules in Southwest China. Because our hypothesise that a high level of social jetlag is associated with either a greater or lower level of BMI among shift nurses, resulting in a polarisation effect. This polarisation could potentially result in a movement towards the median value of BMI when examining the correlation between high social jetlag and BMI, thereby impacting the research hypothesis. Therefore, we examined the association between BMI and social jetlag in order to investigate their interaction. This study aimed to uncover both linear and nonlinear associations between social jetlag and BMI among shift-working nurses. The ultimate goal of this study was to enhance the well-being of nurses working shift schedules.
Materials and methods
Study participants
To ensure comparability of the research subjects, we selected shift nurses working in hospitals with similar latitudes, work intensity and scheduling methods for this study. Registered certified nurses were eligible if they were simultaneously responsible for the day, evening, and night shifts on the shiftwork schedule for at least six months (Hwang in drugi23). Before the study, all eligible nurses were informed of the purpose and procedures. Participants were excluded if they had a chronic noncommunicable disease, were enrolled in a weight-loss program or were pregnant. Sample Size Calculation: According to the formula \({\text{n}} = \frac{{\upmu_{{{\upalpha }/2}}^{2} \pi \left( {1 - \uppi } \right)}}{{\updelta^{2} }}\), which states that the abnormal BMI (underweight, overweight and obesity) rate in similar research is 33% (Hwang in drugi23), \(\uppi \) is set at 0.33 and \(\updelta \) at 0.05. The minimum required sample size is an amount of 340 examples. Sampling Methodology: In order to reduce the influence of latitude on social jet lag, a survey was conducted at five tertiary institutions located at similar latitudes in the Southwest region. The selection method employed was convenience sampling, whereby a total of 450 shift nurses were picked from a total of 82 nursing units from July to September 2023.
Our study procedures were performed in accordance with the ethical standards of the responsible committee on human experimentation (institutional or regional) and the Declaration of Helsinki of 1975, as revised in 2000. This study was approved by the Institutional Review Board of The Second People’s Hospital of Neijiang City (approval number: 202323). Written informed consent was obtained from all the participants.
Instrumentation
The survey tools included a demographic data questionnaire, the MCTQShift and BMI.
Sociodemographic data
Sociodemographic data on each subject, such as sex, age, marital status, work experience, smoking and alcohol use history, and family responsibilities (any children or disabled needing care), were collected.
In the field of shift work, three domains of shift work (timing, intensity, and speed) were derived from published work schedules collected (Lin in drugi32). Shift timing was a day-level measure based on the time when a participant started their work-shift (e.g., day or evening shifts). Shift intensity was assessed using two day-level measures: number of consecutive work-shifts and number of consecutive night shifts. The number of consecutive work-shifts or “work-shift intensity was measured daily by retrospectively counting the total number of consecutive work-shifts (including all-day, evening, and night shifts) over two weeks. Any off-duty day stopped the accumulation of work-shift intensity and was considered as a day with a work-shift intensity of “0.” Shift speed was a person-level measure and was assessed by evaluating how many changes in shift timing (i.e., one change: from days to evenings, two changes: from days to evenings, then from evenings to nights, or from evenings to days) a participant had in the past two weeks, according to the published work schedules collected during the visit. Based on Hall et al.'s schema, we categorized shift speed as slow (i.e., up to one change), medium (i.e., two to three changes), or rapid (i.e., four or more changes). All research was conducted in a quiet room in the ward using one-on-one questionnaires by the researchers in our group.
Social Jetlag assessment
Roenne et al., developed the MCTQ in 2003. This questionnaire measures the midpoint of sleep and sleep duration and describes social jetlag based on the absolute difference between the midpoint of sleep on weekdays and weekends (Roenneberg in drugi44). Juda et al. developed the MCTQ for shift workers (MCTQshift) (Juda in drugi25), Wan-Ju Cheng et al. translated the MCTQshift into Chinese and found a high level of validity after testing it on 288 shift workers. In this study, we used the MCTQshift (Chinese version) (Cheng in Hang8).
BMI
The heights and weights of the participants were measured. The measurement process prevented interference from unrelated persons and ensured the participants’ privacy. BMI was calculated by the researcher after on-site investigation using the following formula: weight (kg)/[height (m)]2. BMI was graded in this study based on the Guidelines for the Prevention and Control of Overweight and Obesity in Chinese Adults (2021). BMI < 18.5 is considered underweight, 18.5–23.9 is normal weight, 24.0–27.9 is overweight, and ≥ 28.0 is obesity.
Research process
The interviewer conducted an in-person survey promptly after the nurse's night shift finished and the handover was completed. The survey was conducted in a designated interview room located within the nurse's ward and had a time requirement of 15–20 min.
Statistical analysis
Descriptive statistics were used to analyze participants’ sociodemographic data. Normally distributed continuous parameters are described as mean and standard deviation (SD). Those with a non-normal distribution are presented as median and interquartile range (IQR). Categorical variables were summarized using participant counts and percentages. Normality was assessed using the Kolmogorov–Smirnov test. Using t-tests and one-way ANOVA for univariate analysis for finding confounding variables that require control. The Kruskal–Wallis H was used to compare social jetlag among different BMI grades. The restricted cubic spline (RCS) model was used to analyze the Nonlinear relationship between shift nurses' BMI and social jetlag. Multiple linear regression was used to analyze the effect of standardized BMI on social jetlag from different segments of the curve. Statistical significance was defined as a two-tailed P-value < 0.05. All statistical analyses were performed using SPSS 25.0 (IBM Corp., Armonk, N.Y., USA) and R software 4.2.2.
Results
Sociodemographic data of subjects
The study was conducted at five tertiary medical centers and study sample was selected from 82 nursing units. Our team researched 450 shift nurses and retrieved 429 valid questionnaires with a validity rate of 95.5%. Among the shift nurses, 75.8% were between the ages of 20 and 29 years, and 92.3% were female, and 60.1% had a bachelor’s or postgraduate degree. More than half of the participants had a household income (per capita) of approximately 5000–10,000 yuan. While 44.3% had less than five years of experience, 59.0% were married, and 28.7% had family responsibility. In addition, only 4.4% smoked, 26.4% consumed alcohol, and 49.3% had a history of coffee consumption. In the domains of shift work, 86.2% of participants had 8 h shift timing, 42.4% had a shift intensity of 4, and 37.1% had a shift intensity of 5. We categorized 19.3% of the participants’ shift speeds as rapid. The BMI levels of shift nurses are influenced by age, gender, Marital status, family responsibility, smoking, alcohol using, drinking coffee, shift timing and shift intensity, which is a confounding variable that should be controlled, as demonstrated by t-tests or one-way ANOVA.The results are summarized in Table 1.
Comparison of social jetlag among different BMI grade
The social jetlag of shift nurses was 82.0 (85.0) min, and the BMI was 20.8 (3.7) kg/m2. Of these shift nurses, 64.6% experienced social jetlag. BMI grading revealed that 17.2% of the participants were underweight, 67.1% were normal, 13.5% were overweight, and 2.1% were obese. There were significant differences between BMI grades for social jetlag (H = 220.822, P < 0.01). The results are summarized in Table 2.
Nonlinear relationship between BMI and social jetlag
By the restricted cubic spline analysis, there was a significant nonlinear relationship between BMI and social jetlag (P < 0.01). Knots between 3 and 7 were tested, and the model with the lowest Akaike information criterion value was selected for the RCS. Finally, an RCS with seven knots was used. Adjusting for the effects of age, gender, education level, family responsibility, household income, smoking, alcohol using and drinking coffee, it suggested an “U-shaped” association of BMI with social jetlag. Using the cutoff point, the data were stratified into two groups: BMI < 20.7 and BMI ≥ 20.7. The results are shown in Fig. 1.
Effect of BMI on standardized Social Jetlag from segmented linear regression analysis
The segmented linear regression allowed for a more nuanced understanding of the relationship between BMI and standardized social jetlag, as it accounted for distinct patterns of association in different parts of the curve. Segmented regression was then performed on each group by cutoff point (BMI < 20.7 OR BMI ≥ 20.7). When BMI < 20.7, it showed significant negative correlation with standardized social jetlag (β = − 0.81, 95%CI − 0.89 ~ − 0.72, P < 0.01), BMI ≥ 20.7 showed significant positively correlation (β = 0.80, 95%CI 0.70 ~ 0.90, P < 0.01). After controlling for confounding variables, When BMI < 20.7, it showed significant negative correlation with standardized social jetlag (β = − 0.77, 95%CI − 0.85 ~ − 0.68, P < 0.01), BMI ≥ 20.7 showed significant positively correlation (β = 0.84, , 95%CI 0.77 ~ 0.91, P < 0.01). The results are summarized in Table 3.
Discussion
Our research indicated a social jetlag of 82 (85) min, which was less than the amount obtained in the study by Lee et al., (211 min) (Lee in Jang28. Human resources for nursing are in low supply in Southwest China because of the region's less-developed economy compared to its eastern counterpart (Chen in Fang7. Consequently, the “APN” shiftwork schedules are widely used by nursing units. A shiftwork schedule arranges shifts A (8:00–16:00), P (16:00–0:00/the next day), and N (0:00–8:00) in alternating order. Shift intensity and speed increased with the schedule. This shiftwork schedule may have resulted in a delayed sleep midpoint during the workday for 83.7% of the nurses in our study who had a shift intensity of four or higher and all nurses who had a medium or quick shift speed. Furthermore, our study's median age for nurses was 26 years, meaning that 75.8% of the nurses were between the ages of 20 and 29. Some studies note that the chronotype changes with age, peaking at age 25–29 and occurring later in adolescence (Druiven in drugi11, Roenneberg in drugi41. Consequently, the sleep midpoint during the rest of the day may occur later. According to the concept of social jetlag, there was not much absolute difference in sleep midpoints between workdays and weekends, which resulted in a lower value of social jetlag compared to similar studies. Notably, our study's social jetlag was less than that of Lee et al., (Lee in Jang28 and the percentage of abnormal BMI (underweight, overweight or obese) was 32.9%, which was similar with that of their research (33.3%). This might imply that the relationship between social jetlag and chronotype affects BMI. Further investigation into this association is needed.
Higher or lower BMI was associated with high social jetlag. Social jetlag and BMI showed a U-shaped relationship. To the best of our knowledge, this is the first study to explore the relationship between social jetlag and underweight shift workers. Roenneberg et al., split the participants into groups based on BMI and found that in the BMI < 25 kg/m2 group, social jetlag did not correlate with BMI, whereas in the BMI ≥ 25 kg/m2 group, the higher social jetlag was associated with higher participant obesity rates (Roenneberg in drugi40. On one hand, the study did not find a nonlinear relationship,it was unclear whether there were junction points among groups with BMIs lower than 25 kg/m2. However, as our study focused on the social jetlag of nurses in shift work, their focus on people without shift work may have a distinct impact on the study population (Casjens in drugi6,Hebl in drugi17.
Exercise (Alves in drugi1,Skjåkødegård in drugi49, eating habits (Mota in drugi37,Silva in drugi48, rhythmic gene temporal abnormalities (Finger in Kramer12,Hodge in drugi18,Takahashi in drugi51, melatonin production (González in drugi16,Roenneberg in Lucas42, Zerbini in drugi55 have all been linked to social jetlag caused overweight or obesity. Jetlag and being underweight are related,however, the exact mechanism remains unknown. Previous research has shown a link between circadian disorders caused by night shifts and unfavorable dietary practices (Soltanieh in drugi50. Additionally, shift workers may turn to sugary beverages or unhealthy meals as a coping mechanism for mood disorders caused by circadian dysrhythmia and night-shift fatigue (Lin in drugi32. A study indicated that nurses working night shifts are more likely to eat unhealthy food (Lin in drugi31. Therefore, underweight may have metabolic implications for unhealthy eating habits. More research is needed to understand the processes behind underweight and social jetlag. It is essential to note that our study only examined the relationship between social jetlag and BMI, which is a crucial measure of metabolic status. Further research is required to determine how social jetlag affects other metabolic markers in shift workers.
There is a linear connection on both sides, with the intercept at the lowest point of the U-shaped curve. Nurses who work shifts and have very high or low body weight experience severe social jetlag. The BMI of 20.7, which is within the typical BMI range, corresponds to the lowest point of the social jetlag. This result is consistent with that of Bodur et al. (Bodur in drugi2. Many detrimental effects on health may result from a high degree of social jetlag. Particular attention should be paid to the high social jetlag status of nurses as a result of their shift employment since the early detection of nurses with high social jetlag is important. Early treatment is necessary to prevent serious adverse health effects.
Limitation
The first limitation of our study is its cross-sectional design, which may limited to examining the association between two variables and cannot demonstrate a cause-and-effect link. Secondly, despite our team's efforts to increase the sample size, it remained rather small due to constraints related to staffing and available resources during the execution of the in-person study with shift nurses. Thirdly, most nurses working shift schedules in Chinese hospitals are young women. As a result, it is important to note that the results of this study may not be applicable to older women or males. Moreover, Due to different shift work method across target countries (such as in Japan, where there are two 12-h shifts and three 8-h shifts), variations in work schedules that are not measurable by the MCTQ should be further considered. While we have taken into account the confounding factors that could influence the study outcomes, it is important to acknowledge that there may still be additional potential confounders that were not evaluated.
Conclusions
This study was an original investigation into the nonlinear correlation between social jetlag and BMI among nurses working shift schedules. Our study revealed the widespread occurrence of social jetlag among shift nurses and further demonstrated a U-shaped association between shift nurses’ BMI and their level of social jetlag. In addition, there was linear correlation on both sides of the U-shaped curve, emphasizing the need to monitor the circadian rhythm status of shift nurses who are either underweight or overweight. Furthermore, it is essential to investigate the potential relationship between social jetlag and BMI among shift-working nurses, as they may experience either elevated or reduced BMI. Further research is required to understand the underlying processes involved in this association.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Alves, M. S. et al. Social jetlag among night workers is negatively associated with the frequency of moderate or vigorous physical activity and with energy expenditure related to physical activity. J. Biol. Rhythms 32(1), 83–93. https://doi.org/10.1177/0748730416682110 (2017).
Bodur, M. & Baspinar, B. A cross-sectional evaluation of the relationship between social jetlag and diet quality. Chronobiol. Int. 38(11), 1557–1568. https://doi.org/10.1080/07420528.2021.1935990 (2021).
Boivin, D. B. & Boudreau, P. Disturbance of the circadian system in shift work and its health impact. J. Biol. Rhythms 37(1), 3–28. https://doi.org/10.1177/07487304211064218 (2022).
Burgess, H. J. The dim light melatonin onset following fixed and free sleep schedules. J. Sleep Res. 14(3), 229–237. https://doi.org/10.1111/j.1365-2869.2005.00470.x (2005).
Caliandro, R., Streng, A. A., van Kerkhof, L. W., van der Horst, G. T. & Chaves, I. Social jetlag and related risks for human health: a timely review. Nutrients 13(12), 4543. https://doi.org/10.3390/nu13124543 (2021).
Casjens, S. et al. Social jetlag and sleep debts are altered in different rosters of night shift work. PLoS ONE 17(1), e0262049. https://doi.org/10.1371/journal.pone.0262049 (2022).
Chen, Y. M. Correlation between nursing work environment and nurse burnout, job satisfaction, and turnover intention in the Western region of Mainland China. Hu Li Za Zhi 63(1), 87–98. https://doi.org/10.6224/jn.63.1.87 (2016).
Cheng, W. J. Late chronotype and high social jetlag are associated with burnout in evening-shift workers: assessment using the Chinese-version MCTQ(shift). Chronobiol Int 35(7), 910–919. https://doi.org/10.1080/07420528.2018.1439500 (2018).
Ciobanu, D. et al. Lifestyle factors, dietary patterns, and social determinants of social and eating jetlag: a cross-sectional survey. Chronobiol Int 41(2), 248–258. https://doi.org/10.1080/07420528.2023.2298700 (2024).
Drăgoi, C. M. et al. Circadian rhythms, chrononutrition, physical training, and redox homeostasis—molecular mechanisms in human health. Cells 13(2), 138. https://doi.org/10.3390/cells13020138 (2024).
Druiven, S. J. et al. Chronotype changes with age; seven-year follow-up from the Netherlands study of depression and anxiety cohort. J. Affect. Disord. 1(295), 1118–1121. https://doi.org/10.1016/j.jad.2021.08.095 (2021).
Finger, A. M. Mammalian circadian systems: organization and modern life challenges. Acta Physiol (oxf) 231(3), e13548. https://doi.org/10.1111/apha.13548 (2021).
Fitzgerald, G. A., Yang, G., Paschos, G. K. & Liang, X. Molecular clocks and the human condition: approaching their characterization in human physiology and disease. Diabetes Obes. Metab. 17, 139–142. https://doi.org/10.1111/dom.12526 (2015).
Garrido, A. L. F. et al. Eating habits, sleep, and a proxy for circadian disruption are correlated with dyslipidemia in overweight night workers. Nutrition 83, 111084. https://doi.org/10.1016/j.nut.2020.111084 (2021).
Gentry, N. W., Ashbrook, L. H., Fu, Y. H. & Ptáček, L. J. Human circadian variations. J. Clin. Invest. https://doi.org/10.1172/jci148282 (2021).
González, S. et al. Circadian-related heteromerization of adrenergic and dopamine D₄ receptors modulates melatonin synthesis and release in the pineal gland. PLoS Biol. 10(6), e1001347. https://doi.org/10.1371/journal.pbio.1001347 (2012).
Hebl, J. T. & Velasco, J. Work around the clock: how work hours induce social jetlag and sleep deficiency. Clin. Chest Med. 43(2), 249–259. https://doi.org/10.1016/j.ccm.2022.02.003 (2022).
Hodge, B. A. et al. The endogenous molecular clock orchestrates the temporal separation of substrate metabolism in skeletal muscle. Skelet. Muscle 5, 17. https://doi.org/10.1186/s13395-015-0039-5 (2015).
Huang, W. C., Chang, S. H. & Hsueh, M. C. Relationship of sleep regularity with device-based sedentary behavior time and physical activity time in working adults. Sleep Health 9(1), 86–92. https://doi.org/10.1016/j.sleh.2022.10.002 (2023).
Huang, W. Y., Feng, J., Zheng, C. & Jiao, J. Associations of social jetlag with physical activity and sedentary behaviour in children and adolescents: a systematic review and meta-analysis. J. Sleep Res. 33(1), e13997. https://doi.org/10.1111/jsr.13997 (2024).
Hulsegge, G., Loef, B., van Kerkhof, L. W., Roenneberg, T. & van der Beek, A. J. Shift work, sleep disturbances and social jetlag in healthcare workers. J. Sleep Res. 28(4), e12802. https://doi.org/10.1111/jsr.12802 (2019).
Hwang, K. R. & Lee, M. Social jetlag and body mass index among shift-working nurses in Korea: a cross-sectional study. Int. J. Nurs. Knowl. https://doi.org/10.1111/2047-3095.12410 (2023).
Hwang, K. R. & Lee, M. Social jetlag and body mass index among shift-working nurses in Korea: a cross-sectional study. Int. J. Nurs. Knowl. 35(2), 195–202. https://doi.org/10.1111/2047-3095.12410 (2024).
Jokubauskas, L., Baltrušaitytė, A. & Pileičikienė, G. Interrelationships between distinct circadian manifestations of possible bruxism, perceived stress, chronotype and social jetlag in a population of undergraduate students. Chronobiol. Int. 36(11), 1558–1569. https://doi.org/10.1080/07420528.2019.1660356 (2019).
Juda, M. & Vetter, C. The Munich ChronoType Questionnaire for Shift-Workers (MCTQShift). J. Biol. Rhythms 28(2), 130–140. https://doi.org/10.1177/0748730412475041 (2013).
Kyung, M., Park, S., Park, C. G. & Hong, O. Association between sleep duration, social jetlag, and the metabolic syndrome by shift works. Int. J. Environ. Res. Public Health 21(6), 668. https://doi.org/10.3390/ijerph21060668 (2024).
Lang, C. J. et al. Sociodemographic and behavioural correlates of social jetlag in Australian adults: results from the 2016 National Sleep Health Foundation Study. Sleep Med. 51, 133–139. https://doi.org/10.1016/j.sleep.2018.06.014 (2018).
Lee, H. Social jetlag and depression in female rotating-shift nurses: a secondary analysis. Perspect. Psychiatr. Care 58(4), 2246–2254. https://doi.org/10.1111/ppc.13054 (2022).
Li, T. M. & Pien, L. C. Direction and magnitude of social jetlag are associated with obesity: results from a sample of hospital employees. Chronobiol. Int. 39(9), 1242–1248. https://doi.org/10.1080/07420528.2022.2090953 (2022).
Liang, F. et al. Associations of social jetlag with dietary behavior, physical activity and obesity among chinese adolescents. Nutrients 14(3), 510. https://doi.org/10.3390/nu14030510 (2022).
Lin, T. T. et al. Shift work relationships with same- and subsequent-day empty calorie food and beverage consumption. Scand J. Work Environ. Health 46(6), 579–588. https://doi.org/10.5271/sjweh.3903 (2020).
Lin, T. T. et al. Shift work domains and their interactions with empty calorie food/beverage consumption: a 14-day intensive longitudinal study. Int. J. Nurs. Stud. 141, 104490. https://doi.org/10.1016/j.ijnurstu.2023.104490 (2023).
López-Soto, P. J. et al. Chronotype, nursing activity, and gender: a systematic review. J. Adv. Nurs. 75(4), 734–748. https://doi.org/10.1111/jan.13876 (2019).
McMahon, D. M. et al. Relationships between chronotype, social jetlag, sleep, obesity and blood pressure in healthy young adults. Chronobiol. Int. 36(4), 493–509. https://doi.org/10.1080/07420528.2018.1563094 (2019).
Mititelu, M. et al. Evaluation of the consumption of junk food products and lifestyle among teenagers and young population from Romania. Nutrients 16(11), 1769. https://doi.org/10.3390/nu16111769 (2024).
Mota, M. C., Silva, C. M., Balieiro, L. C. T. & Fahmy, W. M. Social jetlag and metabolic control in non-communicable chronic diseases: a study addressing different obesity statuses. Sci. Rep. 7(1), 6358. https://doi.org/10.1038/s41598-017-06723-w (2017).
Mota, M. C., Silva, C. M., Balieiro, L. C. T., Gonçalves, B. F. & Fahmy, W. M. Association between social jetlag food consumption and meal times in patients with obesity-related chronic diseases. PLoS ONE 14(2), e0212126. https://doi.org/10.1371/journal.pone.0212126 (2019).
Oshita, K., Ishihara, Y. & Seike, K. Associations of body composition with physical activity, nutritional intake status, and chronotype among female university students in Japan. J. Physiol. Anthropol. 43(1), 13. https://doi.org/10.1186/s40101-024-00360-9 (2024).
Parsons, M. J. et al. Social jetlag, obesity and metabolic disorder: investigation in a cohort study. Int. J. Obes. (lond) 39(5), 842–848. https://doi.org/10.1038/ijo.2014.201 (2015).
Roenneberg, T., Allebrandt, K. V. & Merrow, M. Social jetlag and obesity. Curr. Biol. 22(10), 939–943. https://doi.org/10.1016/j.cub.2012.03.038 (2012).
Roenneberg, T. et al. Epidemiology of the human circadian clock. Sleep Med. Rev. 11(6), 429–438. https://doi.org/10.1016/j.smrv.2007.07.005 (2007).
Roenneberg, T. Light, endocrine systems, and cancer–a view from circadian biologists. Neuro. Endocrinol. Lett. 23(Suppl 2), 82–83 (2002).
Roenneberg, T., Pilz, L. K., Zerbini, G. & Winnebeck, E. C. Chronotype and Social Jetlag: a (Self-) critical review. Biology 8(3), 54. https://doi.org/10.3390/biology8030054 (2019).
Roenneberg, T. & Wirz-Justice, A. Life between clocks: daily temporal patterns of human chronotypes. J. Biol. Rhythms 18(1), 80–90. https://doi.org/10.1177/0748730402239679 (2003).
Rosa, D., Terzoni, S. & Dellafiore, F. Systematic review of shift work and nurses’ health. Occup. Med. (lond) 69(4), 237–243. https://doi.org/10.1093/occmed/kqz063 (2019).
Rutters, F. et al. Is social jetlag associated with an adverse endocrine, behavioral, and cardiovascular risk profile?. J. Biol. Rhythms 29(5), 377–383. https://doi.org/10.1177/0748730414550199 (2014).
Shawa, N. & Rae, D. E. Impact of seasons on an individual’s chronotype: current perspectives. Nat. Sci. Sleep 10, 345–354. https://doi.org/10.2147/nss.S158596 (2018).
Silva, C. M., Mota, M. C., Miranda, M. T., Paim, S. L. & Waterhouse, J. Chronotype, social jetlag and sleep debt are associated with dietary intake among Brazilian undergraduate students. Chronobiol. Int. 33(6), 740–748. https://doi.org/10.3109/07420528.2016.1167712 (2016).
Skjåkødegård, H. F. et al. Beyond sleep duration: sleep timing as a risk factor for childhood obesity. Pediatr. Obes. 16(1), e12698. https://doi.org/10.1111/ijpo.12698 (2021).
Soltanieh, S., Solgi, S., Ansari, M. & Santos, H. O. Effect of sleep duration on dietary intake, desire to eat, measures of food intake and metabolic hormones: a systematic review of clinical trials. Clin. Nutr. ESPEN 45, 55–65. https://doi.org/10.1016/j.clnesp.2021.07.029 (2021).
Takahashi, M. et al. Chronotype and social jetlag influence human circadian clock gene expression. Sci. Rep. 8(1), 10152. https://doi.org/10.1038/s41598-018-28616-2 (2018).
Uekata, S., Kato, C., Nagaura, Y. & Eto, H. The impact of rotating work schedules, chronotype, and restless legs syndrome/Willis-Ekbom disease on sleep quality among female hospital nurses and midwives: a cross-sectional survey. Int. J. Nurs. Stud. 95, 103–112. https://doi.org/10.1016/j.ijnurstu.2019.04.013 (2019).
Wittmann, M., Dinich, J. & Merrow, M. Social jetlag: misalignment of biological and social time. Chronobiol. Int. 23(1–2), 497–509. https://doi.org/10.1080/07420520500545979 (2006).
Yang, G., Paschos, G., Curtis, A. M., Musiek, E. S. & McLoughlin, S. C. Knitting up the raveled sleave of care. Sci. Transl. Med. 5(212), 212rv213. https://doi.org/10.1126/scitranslmed.3007225 (2013).
Zerbini, G. & Kantermann, T. Strategies to decrease social jetlag: reducing evening blue light advances sleep and melatonin. Eur. J. Neurosci. 51(12), 2355–2366. https://doi.org/10.1111/ejn.14293 (2020).
Zhang, R. et al. The association between metabolic parameters and evening chronotype and social jetlag in non-shift workers: a meta-analysis. Front. Endocrinol. (lausanne) 13, 1008820. https://doi.org/10.3389/fendo.2022.1008820 (2022).
Funding
This work was supported by 2023 Sichuan Province Nursing Research Program (grant: H23044).
Author information
Authors and Affiliations
Contributions
All authors contributed to the design of the study, the distribution of questionnaires, the collection of data, the writing of the manuscript, and the submission of contributions. All authors contributed to the article and approved the submitted version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhu, H., Xu, Y., Lin, D. et al. Relationship between social jetlag and body mass index in nurses working shift schedules: a cross-sectional study. Sci Rep 14, 16911 (2024). https://doi.org/10.1038/s41598-024-67644-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-67644-z
- Springer Nature Limited