Abstract
The study's goal was to compare and evaluate the benefits of deep friction massage and ultrasonic therapy (US) vs extracorporeal shockwave therapy (ESWT) for people with lateral epicondylitis. This double-blind, parallel-arm randomized clinical trial was conducted after ethical approval on a sample of 80 subjects with lateral epicondylitis. Participants were enrolled based on predefined eligibility criteria. They were randomly allocated to groups A and B. Group A received ESWT, while Group B received the US combined with deep friction massage. Data was collected using the Numeric Pain Rating Score (NPRS) and Patient-rated tennis elbow evaluation questionnaire (PRTEE) at baseline, at 3rd, and at 7th week of treatment. On the basis of the normality of the data, a non-parametric test was applied to evaluate between-group and within-group differences. P value ≤ 0.05 was considered significant. There was a significant difference between groups (p < 0.001). Comparisons of PRTEE scores at 3rd week and 7th week of intervention were found significant for both groups (p < 0.001). While considering between-group comparisons based on percentile scores of PRTEE at baseline, 3rd and 7th week of intervention, in group A Median (IQR) at the baseline was 24.00 (5.00), at 3rd week, 10.00 (5.00) and 7th week was 1.50 (2.50) and in group B Median (IQR) at the baseline was 25.00 (4.00), at 3rd week 19.50 (4.50) and at 7th week was 11.50 (2.50). The results were significant in both groups (p = 0.000), but between-group analysis revealed that ESWT is more effective in patients with lateral epicondylitis.
Similar content being viewed by others
Introduction
Lateral epicondylitis is one of the common ailments in the elbow region, affecting 1–3% of the adult population every year1. The common presentation of epicondylitis is in the form of elbow pain caused by inflammation or degeneration of the Common extensor tendon, usually due to repeated activity. Female gender, smoking history, repeated activity and ipsilateral scapulothoracic dysfunction are common associated factors2,3. The clinical examination, functional impairment, and positive provocation tests like Cozen's test and Mills's test form the basis of diagnostic criteria for lateral epicondylitis4. Musculoskeletal ultrasound is one of the gold standards for detection of Lateral epicondylitis5.
Patients suffering from lateral epicondylitis are treated with many interventions ranging from conservative to surgical6. Most preferred interventions include iontophoresis, friction massage, electrotherapy, strengthening exercises and corticosteroid injections. These treatment strategies show long-term results, whereas oral medications show short-term results7. Ultrasound therapy and friction massages are routinely used to treat the swollen tendon and underlying adhesions. The thermal effects caused by ultrasound boost metabolic activity in the area, improving blood flow, whereas its nonthermal effects include collagen synthesis and tissue repair8. Transverse friction massage is used to break adhesions, increase blood flow and reduce inflammation in chronic tendinopathies9.
There is a recent surge in the use of Extracorporeal shock wave therapy (ESWT) in the treatment of tendinopathies such as lateral epicondylitis. Shockwave therapy (SWT) is believed to stimulate tissue repair and regeneration in chronic tendinopathies like lateral epicondylitis (LE) through several mechanisms like neovascularization, cell proliferation and anti-inflammatory effects10. The healing effects of ESWT are due to mechano-transduction, a process by which the body alters mechanical load into cellular one, which ultimately promotes structural change11. Both ESWT and ultrasonic therapy (US) show good results in the treatment of lateral epicondylitis by alleviating pain through increased blood flow to the area causing hyperstimulation analgesia12.
Evidence suggests that pain and functional abilities are improved in patients undergoing ESWT or ultrasound therapy; however, the most effective treatment strategy for the treatment of lateral epicondylitis is not well known, and there is a need to address optimal treatment parameters, long-term outcomes, comparative cost-effectiveness, and comprehensive patient-reported outcomes13.
This study aimed to compare the therapeutic effects of ESWT alone versus US and deep friction massage on pain relief and functional ability in patients diagnosed with lateral epicondylitis. The study hypothesized that there would be a significant difference between the therapeutic effects of ESWT alone and US with deep friction massage.
Materials and methods
Study design and settings
This parallel arm randomized clinical trial, conducted between December 2020 and December 2021, took place at two locations: the Physiotherapy Department of Syed Medical Complex, Sialkot, and the Physiotherapy Department of Sialkot College of Physical Therapy at Amin Welfare & Teaching Hospital, Sialkot. The trial followed a double-blind design, with both the patients and outcome assessors being unaware of the treatment assignments. Written informed consent was obtained from all participants in accordance with the principles outlined in the Declaration of Helsinki. The study received ethical approval from the ethics committee of Sialkot College of Physical Therapy CPT-IRB, with reference number IRB-SCPT-DPT-140-2020. Prior to enrolling the first participant, the trial was prospectively registered in the Iranian Registry of Clinical Trials (IRCT) with the registration number IRCT20201031049207N4 (date of registration 25/12/2020). The study adhered to the CONSORT guidelines for reporting clinical trials, and all procedures were performed in compliance with the relevant guidelines.
Sample size calculation
The sample size of 74 patients was calculated through the Giga Calculator with 95% confidence level and 80% power of the study. By adding a 10% attrition rate, the sample size was 80. The sample size was estimated based on the mean and standard deviation of pain scores in a study by Staples et al.14.
Participants, blinding, and eligibility criteria
Health conditions studied were lateral epicondylitis or Tennis Elbow ICD-10 code M77.10. Participants were recruited from a multicentre, and an initial screening form was filled out. A blind assessor explained the whole procedure and the right to draw from the research at any time. Male and female patients aged between 30 and 60 years, localised pain for more than eight weeks, and with positive Mill's and Cozen's tests were included in the study15. Patients with a history of trauma, surgery, prostheses in the elbow area, sensory deficit and those with use of analgesics in the last three weeks or on corticosteroid injections were excluded from the study.
Randomization and masking
Patients were divided into two groups randomly through the sealed envelope method. To ensure the concealment of allocation, a method known as sequentially numbered, opaque, sealed envelopes (SNOSE) was employed, following the guidelines outlined by Doig and Simpson16. The procedure involved an independent researcher who was not involved in the clinical aspects of the trial and prepared eighty opaque envelopes. Each envelope contained a folded paper indicating the assigned treatment, with an equal distribution of treatments. Randomized numbers were assigned to these envelopes, and they were thoroughly shuffled before being arranged in sequential order. The envelopes were then handed over to another independent researcher. The therapist recorded relevant information on each envelope, which was subsequently opened to reveal the assigned treatment, maintaining concealment. The assessor documented the post-treatment findings, and an additional independent analyst was responsible for data analysis. In this study, both the patients and the assessor were blinded to the allocation of treatment groups.
Intervention Group A
In group A, patients received extracorporeal shock wave therapy. The patient was seated with their elbow flexed and supported at the edge of the couch. ESWT with decompression (ESWT-Japan, Model JESL-2000 Shockwave Therapy System) was administered on the lateral side of the elbow, utilizing a frequency of 1 Hz, an energy level of 2.0, and a pressure bar of 2 as shown in Fig. 1a and b17. Each treatment session lasted for 5 min, and a total of 7 sessions were conducted with a 4-day interval between each session. Evaluations were performed at Week 0, the 3rd week, and the 7th week of the treatment for all participants.
Intervention Group B
In group B, patients received a combination of US and deep friction massage. The patient assumed a seated position with the elbow flexed and supported at the end of the couch. The US was administered through ITO-EU 941 (Japan) multi-frequency treatment head at a rate of 2.5w/sec2 for 3–5 min, using an intermittent mode, three times per week for a total of seven weeks, as shown in Fig. 2a and b18. The Deep friction massage was used as an adjunct to the US for 2–5 min, as shown in Fig. 2c. The massage was applied directly to the common extensor tendon at the lateral elbow in a perpendicular direction to the orientation of the tendon fibres. The pad of the thumb was used to apply firm, deep pressure in a transverse friction motion across the tendon. The intensity of the pressure was estimated to be 2.3 kg/cm2. All the patients were evaluated at baseline, 3rd and at 7th week of the treatment19.
Outcome measures
The clinical and functional outcomes of all patients were assessed at the beginning of the treatment, as well as at the 3rd and 7th weeks, using two measurement tools: the NPRS score and the Patient Rated Tennis Elbow Evaluation Questionnaire (PRTEE) score. The PRTEE is a specialized assessment tool designed for individuals with lateral epicondylitis. It comprises 15 items and is divided into three subgroups: pain, special activities, and daily living activities. Higher scores on the PRTEE indicate greater levels of pain and functional impairment, with a score of 0 indicating no disability. Numeric Pain Rating Scale (NPRS) was used to assess pain intensity on a scale of 0 to 10, having a moderate level of reliability with an ICC value of 0.67, indicating consistent and stable scores obtained from the measurement tool20,21.
Participant enrolment, randomization, and analysis details are given in the CONSORT flow diagram in Fig. 3. Patients with confirmed diagnoses of lateral epicondylitis visiting the Outpatient Physical Therapy departments of Syed Medical Complex and Sialkot College of Physical Therapy were screened for eligibility. Eligible patients were invited to participate in the study. The willing participants signed written informed consent. They were randomly divided into two groups using SNOOS. Initially, 95 patients were screened over, and 80 were included in the study to meet the sample of 74 subjects, eliminating the attrition. There came unequal distribution in two groups (Group A = 37 and Group B = 43). Treatment was continued as per protocol, and the data was taken at prescribed time points: at baseline, after the 3rd visit, and after the 7th visit in both groups using PRTEE. After 2nd visit, participants were lost in both groups: Group A n = 2, Group B n = 4. Therefore, the study was completed on 74 participants (group A = 35, group B = 39).
Data analysis
The normality of data was checked using the Shapiro–Wilk's test. The qualitative variables were presented in frequencies and percentages, whereas mean and standard deviation were used to present the mean difference between the quantitative variables. Since the data was not normally distributed, the non-parametric Mann–Whitney U test was used to compare the mean scores between Group A (ESWT) and Group B (control group), while chi-square was used to compare qualitative variables. Likewise, for the analysis of three mean ranks at baseline, after the 3rd and the 7th week, the Friedman test was employed and expressed as Mean (IQR). The statistical significance level in this study was P < 0.05. Data analysis was performed using the Statistical Package for Social Sciences (SPSS) software version 26.
Results
The mean age ± SD of the participants was 47.58 ± 8.017 years. Baseline and demographic characteristics are given in Table 1. As the data was not normally distributed, a non-parametric test was applied to compute the results. A between-group comparison of the scores PRTEE at baseline, in the 3rd week and the 7th week of treatment based on the Mann–Whitney U test is given in Table 2, while based on percentile scores, it is given in Table 4. Changes in outcomes within groups based on mean rank are expressed in Table 3.
Table 1 shows that there were 74 participants in total with mean age ± SD 47.58 ± 8.017 years, while 35 participants in group A (ESWT) with mean age ± SD 47.83 ± 9.096 years, and 39 participants in group B (US with deep friction massage) with 47.36 ± 7.024 years. Affected elbows were 30 (40.54%) on the right, 36 (48.64%) on the left side and 4 (10.81%) with bilateral elbows. In total, 22 (29.7%) were male, and 52 (70.3%) were females. Overall NPRS was 6.30 ± 3.063, with 6.75 ± 7.612 in group A and 7.45 ± 5.463 in group B. The average duration of onset of symptoms was 26 weeks.
Table 2 shows between-group comparisons of PRTEE scores at baseline, at the 3rd week and 7th week of intervention and was found significant at the 3rd and 7th week post-intervention (P < 0.001).
Table 3 shows a steady improvement within both groups A and B (P = 0.000). However, it is more consistent in group A, with a mean rank of 3.00 at baseline, 2.00 after 3rd week and 1.00 after 7th week of intervention in contrast with the mean rank in group B mean rank 2.99 at baseline, 2.01 at 3rd week and 1.00 at 7th week of intervention (Table 4).
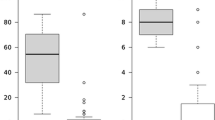
The table shows between-group comparisons based on percentile scores of PRTEE at baseline, after 3rd, and 7th week of intervention (Fig. 4). In group A, the Median (IQR) at the baseline was 24.00 (5.00), in the 3rd week, 10.00 (5.00) and in the 7th week, it was 1.50 (2.50). In group B, the Median (IQR) at the baseline was 25.00 (4.00), in the 3rd week, 19.50 (4.50), and in the 7th week was 11.50 (2.50). While the results were significant in both the groups (P = 0.000).
Discussion
Lateral epicondylitis is a chronic elbow joint condition which is mainly manifested as pain and tenderness over the lateral condyle of the elbow22. According to previous studies, there are plenty of treatment options, from conservative to surgical, for the treatment of lateral epicondylitis6. There is an increasing trend in the use of ESWT and US due to the noninvasive nature of the modalities23. This study was conducted to compare the effectiveness of ESWT and US for the treatment of lateral epicondylitis. The results of this study suggested that ESWT was more effective in treating pain and reducing disability as compared to US and deep friction massage.
The results of this study are in accordance with a systematic review in which 13 articles with 1035 participants were included. According to the results, ESWT was effective in reducing pain VAS (p = 0.0004) and improving grip strength (0.0001) caused by lateral epicondylitis. In another study, ESWT showed an 89.6% success rate at 3 months follow-up and a 93.7% success rate at 6 months follow-up in patients who failed the conservative treatment. In addition, at one-year follow-up, there was a 0% recurrence rate in patients who underwent treatment with ESWT24.
According to a study by Aldaja et al. ESWT had a superior effect as compared to conventional physical Therapy. In this RCT, forty participants completed the five sessions of the intervention program, and it was concluded that ESWT was effective in improving pain and enhancing upper extremity function25. The results of this study advocated the fact that ESWT has good analgesic effects. In our study, ESWT showed superior effects when compared to US.
In another study, the effects of dry needling were compared with ESWT in patients with lateral epicondylitis. The study advocated that the two treatments showed no significant difference at any assessment time point. In long-term follow-up, both treatment groups had significant improvement in pain score, whereas no significant difference was found in grip strength and functional impairment. This emphasizes the fact that this noninvasive process can equally benefit patients for pain relief26.
In a randomized clinical trial including acute and chronic cases of lateral epicondylitis, it was concluded that ESWT was equally effective in treating acute and chronic cases of lateral epicondylitis. In addition, it was observed that it prevented the acute cases from developing chronicity. The outcome measures were assessed on the 2nd, 6th and 24th week, a time good enough to observe the effects of ESWT27.
The superiority of ESWT over US has been reported in the literature. According to a meta-analysis, ESWT proved to be a more effective treatment than US in reducing pain and improving grip strength in patients with Lateral epicondylitis23. When compared to surgical intervention, ESWT is a cost-effective treatment depending on the number of sessions and the duration of treatment. It is feasible in terms of access and its noninvasive nature.
The limitation of the study lies in the fact that it is a small-scale study with limited outcome measurement tools. The addition of more sophisticated tools could add strength to the study. The randomization showed the unequal distribution of the participants in both groups, leaving some errors. Moreover, the baseline mean scores on the NPRS were around 6–7, indicating moderate pain levels. This suggests that many participants began the study with relatively low pain scores. Due to the floor effect, the NPRS may not adequately capture further reductions in pain, as participants have limited room to score lower within the scale. For instance, if a participant's pain level decreases from 6 to 4, it might be a significant improvement, but the scale's ability to reflect this change accurately is constrained by its lower bound. Statistical principles and previous research on pain measurement scales support that such floor effects can limit the sensitivity of the NPRS, potentially underestimating the true effectiveness of the treatment. Alternative measures with a wider range or different sensitivity might provide a more accurate assessment of pain reduction in these cases. Another major limitation is the lack of long-term follow-up beyond 7 weeks to assess sustained treatment effects.
Conclusion
The study comes up with the conclusion that both the interventions of ESWT and a combination of US and deep friction massage are effective in the management of patients with lateral epicondylitis.
Data availability
The data associated with the paper are not publicly available but are available from the corresponding author on reasonable request.
References
Cutts, S., Gangoo, S., Modi, N. & Pasapula, C. Tennis elbow: A clinical review article. J. Orthop. 17, 203–207 (2020).
Sayampanathan, A. A., Basha, M. & Mitra, A. K. Risk factors of lateral epicondylitis: A meta-analysis. Surgeon 18(2), 122–128 (2020).
Pathak, G. & Patil, C. Prevalence of scapulothoracic joint dysfunction in patients with lateral epicondylitis. Indian J. Public Health Res. Dev. 11(5), 109 (2020).
Scher, D. L., Wolf, J. M. & Owens, B. D. MAJ M: Lateral epicondylitis. Orthopedics 32(4), 276–282 (2009).
Latham, S. & Smith, T. The diagnostic test accuracy of ultrasound for the detection of lateral epicondylitis: A systematic review and meta-analysis. Orthop. Traumatol. Surg. Res. 100(3), 281–286 (2014).
Landesa-Piñeiro, L. & Leiros-Rodriguez, R. Physiotherapy treatment of lateral epicondylitis: A systematic review. J. Back Musculoskelet. Rehabil. 35(3), 463–477 (2022).
D’vaz, A. et al. Pulsed low-intensity ultrasound therapy for chronic lateral epicondylitis: A randomized controlled trial. Rheumatology 45(5), 566–570 (2006).
Smallcomb, M., Khandare, S., Vidt, M. E. & Simon, J. C. Therapeutic ultrasound and shockwave therapy for tendinopathy: A narrative review. Am. J. Phys. Med. Rehabil. 101(8), 801–807 (2022).
Landesa-Piñeiro, L. & Leirós-Rodríguez, R. Physiotherapy treatment of lateral epicondylitis: A systematic review. J. Back Musculoskelet. Rehabil. 35(3), 463–477 (2022).
Majidi, L., Khateri, S., Nikbakht, N., Moradi, Y. & Nikoo, M. R. The effect of extracorporeal shockwave therapy on pain in patients with various tendinopathies: A systematic review and meta-analysis of randomized control trials. BMC Sports Sci. Med. Rehabil. 16(1), 93 (2024).
Khan, K. M. & Scott, A. Mechanotherapy: How physical therapists’ prescription of exercise promotes tissue repair. Br. J. Sports Med. 43(4), 247–252 (2009).
Dedes, V. et al. Comparison of radial extracorporeal shockwave therapy with ultrasound therapy in patients with lateral epicondylitis. J. Med. Ultrasonics 47, 319–325 (2020).
Trudel, D. et al. Rehabilitation for patients with lateral epicondylitis: A systematic review. J. Hand Ther. 17(2), 243–266 (2004).
Staples, M. P., Forbes, A., Ptasznik, R., Gordon, J. & Buchbinder, R. A randomized controlled trial of extracorporeal shock wave therapy for lateral epicondylitis (tennis elbow). J. Rheumatol. 35(10), 2038–2046 (2008).
Karanasios, S. et al. Diagnostic accuracy of examination tests for lateral elbow tendinopathy (LET)—A systematic review. J. Hand Ther. 35(4), 541–551 (2022).
Clark, L., Mitchell, N., Hewitt, C. & Torgerson, D. Exploring engagement with authors of randomised controlled trials to develop recommendations to improve allocation concealment implementation and reporting. F1000Research 10, 83 (2021).
Yalvaç, B., Mesci, N., Külcü, D. G. & Yurdakul, O. V. Comparison of ultrasound and extracorporeal shock wave therapy in lateral epicondylosis. Acta orthopaedica et traumatologica turcica 52(5), 357–362 (2018).
Luo, D., Liu, B., Gao, L. & Fu, S. The effect of ultrasound therapy on lateral epicondylitis: A meta-analysis. Medicine 101(8), e28822 (2022).
Chaves, P. et al. Pressure applied during deep friction massage: Characterization and relationship with time of onset of analgesia. Appl. Sci. 10(8), 2705 (2020).
Hefford, C., Abbott, J. H., Arnold, R. & Baxter, G. D. The patient-specific functional scale: Validity, reliability, and responsiveness in patients with upper extremity musculoskeletal problems. J. Orthop. Sports Phys. Ther. 42(2), 56–65 (2012).
Rompe, J. D., Overend, T. J. & MacDermid, J. C. Validation of the patient-rated tennis elbow evaluation questionnaire. J. Hand Ther. 20(1), 3–11 (2007).
Johns, N. & Shridhar, V. Lateral epicondylitis: Current concepts. Austral. J. Gen. Pract. 49(11), 707–709 (2020).
Yan, C. et al. A comparative study of the efficacy of ultrasonics and extracorporeal shock wave in the treatment of tennis elbow: A meta-analysis of randomized controlled trials. J. Orthop. Surg. Res. 14(1), 1–12 (2019).
Marei, S., Soliman, S. G., Fathy, H., Yousef, M. A. & Ebied, A. Extracorporeal shockwave therapy versus steroid injection in treatment of tennis elbow. Menoufia Med. J. 35(4), 2057 (2022).
Aldajah, S., Alashram, A. R., Annino, G., Romagnoli, C. & Padua, E. Analgesic effect of extracorporeal shockwave therapy in individuals with lateral epicondylitis: A randomized controlled trial. J. Funct. Morphol. Kinesiol. 7(1), 29 (2022).
Wong, C.W.-Y. et al. Comparison of treatment effects on lateral epicondylitis between acupuncture and extracorporeal shockwave therapy. Asia-Pac. J. Sports Med. Arthrosc. Rehabil. Technol. 7, 21–26 (2017).
Koksal, I. et al. Comparison of extracorporeal shock wave therapy (eswt) in acute and chronic lateral epicondylitis. Acta Orthopaedica et Traumatologica Turcica 49(5), 465 (2015).
Acknowledgements
The authors extend their appreciation to the Deanship of Scientific Research, King Saud University for funding through Vice Deanship of Scientific Research Chairs; Rehabilitation Research Chair.
Funding
This study was funded by King Saud University, Deanship of Scientific Research, Vice Deanship of Scientific Research Chairs; Rehabilitation Research Chair.
Author information
Authors and Affiliations
Contributions
W. P., S. A., R. H., M. A. A., A. R., U. I., S. N., M.K., and A.H.A. conceptualized the study and its methodology. W. P., S. A., R. H., M. A. A., A. R., and U. I. were involved in data collection and curation. W. P., S. A., R. H., M. A. A., A. R., and U. I. did data analysis, interpreted the results, and wrote the original draft and final version. S.N., M.K., and A.H.A. were involved in supervision and critically reviewed the final version. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Perveen, W., Anwar, S., Hashmi, R. et al. Effects of extracorporeal shockwave therapy versus ultrasonic therapy and deep friction massage in the management of lateral epicondylitis: a randomized clinical trial. Sci Rep 14, 16535 (2024). https://doi.org/10.1038/s41598-024-67313-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-67313-1
- Springer Nature Limited