Abstract
The aim of this study is to examine the frequency of maxillary sinus pathologies and their relationship with each other using cone beam computed tomography (CBCT) and to make a new grade according to the number of affected walls. 1000 maxillary sinuses of 500 patients with CBCT images were included in the study. Anatomical variations and pathological formations of the maxillary sinuses were examined. Images were evaluated for the presence of flat, polypoidal, partial and generalized mucosal thickening, partial and total opacification, polyps and mucous retention cysts. Maxillary sinus pathologies were graded according to the number of walls affected. In the examined CBCT images, no pathology was found in 54.2% of the maxillary sinuses, while pathology was observed in 45.8%. The most common sinus pathologies were mucous retention cyst (12.3%) and polypoidal thickening (12.2%). While pneumatization, ostium obstruction, and the presence of sinus-related roots were associated with sinus pathology, no relationship was found with nasal septum deviation and the presence of septa. Before dental implant and sinus surgery applications, the presence of sinus pathologies and their relationship with anatomical variations can be evaluated with CBCT, a three-dimensional technique, and complications such as sinus membrane perforation, infection, failure to break the bone window due to the presence of antral septa, graft loss and oroantral fistula formation can be reduced.
Similar content being viewed by others
Introduction
The paranasal sinuses are air cavities located in the bones of the skull surrounding the nasal cavity. The importance of the paranasal sinuses has increased because they are covered with mucosa and connected to the nasal cavity. Being lined with mucosa and connected to the nasal cavity, these sinuses are associated with many important functions, including respiratory infections, allergic reactions, and mucus drainage. Therefore, the health of the paranasal sinuses is critical to overall nasal and respiratory health. The most obvious function of the paranasal sinuses, which are assumed to have many functions such as reducing skull weight, resonance of sound, absorption of trauma, heat insulation, adjustment of intranasal pressure and many others, is ventilation and drainage1,2,3. Paranasal sinuses are complex structures that are difficult to examine because they vary in size, shape and volume4,5.
The maxillary sinuses are the most interesting region among the paranasal sinuses due to their large volume, neighborhood and variations. The maxillary sinuses begin to develop between the second and third months of pregnancy and enlarge with the eruption of permanent teeth. Their inner walls are covered with Schneiderian membrane. The thickness of the Schneiderian membrane varies between 0.13 and 0.5 mm, but various etiologic conditions may cause an increase in membrane thickness6,7.
Inflammatory lesions and cystic conditions are among the most widespread maxillary sinus pathologies in the literature8. Maxillary sinus retention cysts (MSRCs) are the most common in this group. Although most of them are small and asymptomatic, they may increase in size and obstruct the ostium of the maxillary sinus in some cases9. Various inflammatory conditions may also cause opacification by thickening the mucosa and increasing the opacity in the region. Thus, the amount of air decreases and the osteomeatal opening may be narrowed or obstructed10.
Cystic lesions in the maxillary sinus are also among the most common conditions. Retention cysts occur when the seromucinous gland canals in the sinus mucosa become blocked. These are lesions that cause symptoms such as headache, nasal congestion, and runny nose10. Appropriate imaging is crucial for diagnosis.
With the advancement of technology, imaging methods have also improved. In recent years, CBCT has been preferred because it is inexpensive and minimizes radiation exposure11. In addition to understanding the complex anatomical structure of the maxillary sinuses, CBCT is the best imaging method that can be used in this field, providing three-dimensional (3D) imaging to identify and measure pathologic conditions and variations in the region. The fact that it provides detailed imaging especially in bone tissue facilitates both surgical interventions and the detection of variations5. The maxillary sinus is a significant anatomical structure in the clinical practice of dentistry. This structure should be evaluated in terms of pathologic lesions and variations during implant planning, especially in cases of maxillary posterior edentulism.
In this study, we aimed to contribute to the literature by analysing the prevalence and interrelationships of maxillary sinus pathologies using CBCT and by making a new grading according to the number of affected walls.
Material and method
Before starting the study, approval was received from the Harran University Clinical Research Ethics Committee (approval number: 23.09.12). Additionally, this study was conducted in accordance with the principles defined in the Declaration of Helsinki. In retrospective studies, the ethics committee waived the informed consent form. In this study, the images obtained with the Castellini X Radius Trioplus (imola, ITALY) device in 2022–2023 in the archive of the Dentomaxillofacial Radiology department were used. Sample size was calculated using the G Power 3.1 program. The minimum sample size was found to be 220 when α = 0.05 and test power 1-β = 0.95. Multiplanar images were obtained with a voxel size of 0.3 mm3, slice thickness of 1 mm, and 13 × 16 FOV (field of view).
Inclusion criteria were CBCT images without any distortion and artifacts with clear visualization of the maxillary sinuses.
Exclusion criteria: Images with odontogenic cysts, tumors, facial growth defects, trauma affecting the midface and maxillary sinuses were excluded. Images containing diseases affecting the bone such as Paget, fibrous dysplasia and osteopetrosis were excluded. Additionally, those with a history of maxillofacial surgery were excluded from the study.
Image analysis
IRYS version 15.1 was used to analyze the images. CBCT images were evaluated on the right and left sides for the presence of polyps, mucosal thickening (flat, polypoid, partial and generalized), opacification (partial and total), and mucous retention cysts. All images were analyzed by a dentomaxillofacial radiologist (MED) with 5 years of experience. Undecided cases were excluded. Observation and examination were performed in all planes to avoid missing inflammatory pathologies of the maxillary sinus as follows.
Normal
No pathologic changes in the mucosa and internal structure of the maxillary sinus (Fig. 1a).
Polyps
These are rounded and stalked folds of tissue with smooth borders, originating from thickened maxillary sinus mucosa with chronic inflammation, isolated in a single area or present in different areas within the sinus12 (Fig. 1b).
Mucosal thickening
These are thickenings in the form of a diffuse radiopaque line parallel to the maxillary sinus wall, with clear borders and non-cortical13. If the mucosal thickness is 1 mm or more, it is considered as mucosal thickening. Mucosal thickening of more than 2 mm is considered of sinus inflammation 14. It was classified as flat and polypoidal according to the shape of thickening of the mucosa, and as partial and generalized according to the region affected. (Fig. 1c,d, e, f).
Partial and total opacification
Diffuse opacification in which more than three walls of the maxillary sinus are affected is called partial opacification, while opacification that fills the entire sinus cavity and has no air space is called total opacification15 (Fig. 1 g,h).
Mucous retention cyst
It is formed by the secretions accumulated as a result of the blockage of the secretory ducts of the seromucinous glands in the maxillary sinus mucosa. It is homogeneous, convex, well-circumscribed, dome-shaped, radiopaque lesions not surrounded by cortical bone2,13 (Fig. 1 ı).
Maxillary sinus pathologies were graded according to the number of walls affected as follows.
Normal: No affected wall.
Grade 1: single wall affected.
Grade 2: affected both walls.
Grade 3: three walls affected.
Grade 4: affected four walls and above.
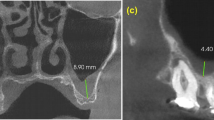
Pneumatization
The relationship of the posterior tooth roots present in the dental arch with the maxillary sinus floor was investigated and if the sinus floor is displaced between the tooth roots, pneumatization was stated to be present. In addition, the presence of pneumatization in patients with no posterior teeth was recorded when the distance between the nasal floor and the maxillary sinus floor was more than 5 mm16.
Relationship between sinus and tooth root
The topographic relationship between the maxillary sinus and each apex of the upper posterior teeth was evaluated. The relationship of the root to the maxillary sinus was determined as follows: roots in the maxillary sinus and roots outside the maxillary sinus (apexes in contact or not with the borders of the maxillary sinus cortex)17.
Statistical analysis
SPSS 25 (IBM Armonk, NY, USA) package program was used in statistical analysis. Descriptive statistics were used to calculate the number, percentage, mean and standard deviation values of the parameters. Chi-square test was used in pairwise comparisons. P < 0.05 was accepted as importance level.
Results
Data from 1000 maxillary sinuses were evaluated in 500 CBCT patients, 222 (44.4%) males and 278 (55.6%) females aged between 17 and 91 years with a mean age of 40.69 ± 15.88 years. 542 (54.2%) maxillary sinuses were free of pathology while 458 (45.8%) showed pathologic changes. As shown in Table 1, the most widespread of these maxillary sinus pathologies was mucous retention cyst 12.3%, followed by polypoidal thickening 12.2%, polyp 6.6%, flat thickening 4.7%, partial opacification 4.2%, generalized thickening 3.4%, partial thickening 1.5% and total opacification 0.9%. Pneumatization (66.0%) and septum deviation (54.1%) were the most common variations. When the relationship between the affected walls and pathology was examined, it was seen that the most affected wall was inferior with 20.6% (p < 0.001). A statistically significant correlation was found between patients with ostium obstruction and maxillary sinus pathologies (p < 0.05).
Especially in patients with partial opacification, ostium obstruction was observed more frequently. When the impact of nasal septum deviation on sinus pathology was analyzed, no statistically significant difference was found (p > 0.05). The absence of any pathology in patients without a tooth root associated with the maxillary sinus was found to be high and statistically significant (p < 0.05). There was no correlation between the presence of septa in the sinus and sinus pathologies (p > 0.05). However, when the pathological sinus changes observed in the maxillary sinuses with pneumatization were examined, the mucous retention cyst was found to be 9.9% more common than all other pathologies and there was a statistically significant relationship (p < 0.05) (Table 2). When the presence of right and left side maxillary sinus pathologies was analyzed comparatively, no statistically significant difference was found (p > 0.05). When the pathological findings of the maxillary sinus were categorized according to the number of walls they affected, the most common pathology was Grade 1 and the most common pathology found at this grade was mucous retention cyst 9.1% and statistically significant (p < 0.05) (Table 3). In addition, sinus pathologies were most commonly observed in the inferior wall and there was a statistically significant relationship (p < 0.05).
Discussion
In studies conducted in various populations, maxillary sinus abnormalities were found to be 14.3–82%18. In the population we examined, maxillary sinus pathologies were found to be 45.8% in parallel with these studies.
In this study, pneumatization was the most common maxillary sinus variation in accordance with the literature19,20. Although the age range of the studied population was similar to the study of Sanchez perez et al.19, ıt has been suggested that tooth loss and aging increase the likelihood of the presence of pneumatization. Maxillary sinus pneumatization may complicate implant planning and worsen the problem of bone loss caused by atrophy of the maxilla to the extent that alveolar bone remains a few millimeters21. The maxillary sinus septa are cortical bone barriers that separate the sinus into multiple compartments. They may be formed following maxillary development (primary), or they may be present as bony protrusions (secondary) between alveolar crest resorption, which increases with tooth loss, and progressive sinus pneumatization22.
The presence of septa complicates lateral window opening and sinus wall inversion in sinus floor elevation surgery23. The presence of maxillary sinus septa was reported as 32.67% by Li et al.24, 33.2% by Neugebauer et al.25 and 58% by Orhan et al.26. The rate of 37% in this study performed in the Turkish population is compatible with other studies in the literature. Regarding the effect of the presence of septa on sinus pathologies, no significant relationship was observed and this result is similar to the study of Taşssöker27 and Kocak28 who used the same imaging method.
Nasal septum deviation (NSD) is the displacement of the nasal septum, which is normally located in the midline of the face, to the left or right. NSD disrupts sinus drainage by narrowing the middle meatus and decreasing nasal air passage. Avsever et al.29 found the incidence of NSD to be 13.1% and Kaya et al.28 found it to be 89.7%. Many studies have examined the relationship between NSD and sinus pathologies27,30,31,32,33,34 Poorey31 and Taghiloo32 observed a significant correlation, while Taşsoker27, Kaya30, Balikci33 and Köse34 did not observe a correlation. In this study, NSD was found to be 54.1% and there was no significant correlation with sinus pathologies.
The paranasal sinuses are normally lined with 1 mm thick respiratory epithelium. It has been reported that the mucosa may thicken up to 10–15 times the normal thickness in case of inflammation. Some authors have accepted ≥ 1 mm, ≥ 2 mm, > 3 mm mucosal thickening as pathologic13,35,36. The prominent features of inflammatory sinus diseases are mucosal thickening, opacification and air-fluid level in the sinus20. In one study, mucosal thickening between 2 and 5 mm was found in 24.3%37. In this study, mucosal thickening above 2 mm was accepted as pathologic and 21.8% of them were found to be compatible with previous studies. When the factors causing mucosal thickening are eliminated with appropriate treatments before implant applications and sinus membrane perforations are repaired, there will be no risk for implant and graft applications38.
Mucous retention cysts are radiopacities which are usually asymptomatic and incidentally observed on radiographs extending dome-shaped from the sinus wall due to obstruction of the mucus-secreting glands of the maxillary sinus. Since mucous retention cysts regress spontaneously in most cases or do not cause serious volume change, follow-up is recommended if they do not lead to any complications10,39. The prevalence of mucous retention cysts has been evaluated in various studies; Aghaee et al.39 found 5.6%, Gracco et al.35 5.75%, and Phothikhun et al.40 10%. In the Turkish subpopulation we studied, this value was 12.3%. In this study, it was seen that the wall most affected by pathologies was significantly inferior. The wall to which retention cysts are attached will be important when sinus floor elevation technique will be applied, which makes our study valuable. This study will guide maxillofacial surgeons and otolaryngologists.
With the change in the air-fluid level in the maxillary sinus, the normally radiolucent maxillary sinus will appear more radiopaque20. In addition to Lana et al.20 who found partial or total opacification in the maxillary sinus at a rate of 1.8%, Rege et al.41 reported this rate as 7.8% and Raghav et al.42 reported this rate as 16.6%. In our study, this value was compatible with the literature with 5.1%.
The ostium has a major role in the drainage and ventilation of the maxillary sinus. When the maxillary ostium is obstructed, the amount of oxygen required to maintain metabolic activity of the sinus mucosa decreases. Thus, with the increase in anaerobic reactions, the necessary environment for bacterial proliferation is created43. This leads to mucosal thickening and increased radiopacity associated with inflammation and edema in the mucosa. Dobele et al.44 found the prevalence of ostium obstruction to be 26.5% in their study and stated that the relationship with mucosal thickening was significant. Carmeli et al.45, who had similar results with this study, calculated the prevalence of ostium obstruction as 15% and observed mucosal thickening in 65.48% and opacification in 34.52% of patients with obstruction. In this study, 39.6% of patients with ostium obstruction (10.6%) had opacification in the sinus, while 38.68% had mucosal thickening.
The close relationship of the maxillary posterior tooth roots with the sinus may cause pathogenic microorganisms and toxins in the oral cavity to reach the sinus through the spongiose bone and cause inflammation of the mucosa and sinusitis symptoms46,47. Kuligowski et al.47 who reached a similar conclusion with this study, found that mucosal thickening was higher in maxillary sinuses associated with tooth roots.
The limitation of this study was that the pediatric population could not be evaluated because only young and adult patients were included in the study. In addition, the medicine history of the patients could not be accessed. Future studies can be performed in a multicenter and larger sample to represent the general population.
Conclusion
CBCT, a three-dimensional method, can be used to evaluate anatomical and pathological changes in the maxillofacial region. Pneumatization was the most common anatomical variation while mucous retention cyst was the most common sinus pathology. Sinus pathologies were particularly associated with pneumatization, sinus-associated tooth roots and obstruction of the ostium. Before dental implant and sinus surgery applications, detecting the presence of variations and pathologies can reduce complications such as sinus membrane perforation, infection, failure to break the bone window due to the presence of antral septa, graft loss and oroantral fistula formation. Otorhinolaryngologist consultation may be required if symptoms of sinusitis are present as opposed to being asymptomatic.
Data availability
If there is a valid reason, data can be obtained by contacting the corresponding author.
References
Jankowski, R. et al. Sinusology. Eur. Ann. Otorhinolaryngol. Head Neck Dis. 133(4), 263–268 (2016).
Parks, E. T. Cone beam computed tomography for the nasal cavity and paranasal sinuses. Dent. Clin. North Am. 58(3), 627–651 (2014).
Dereköy, S. & Güçlü, O. Üst solunum yolu enfeksiyonları. Klinik tıp aile hekimliği 8(4), 33–43 (2016).
Ozdemir, M., Kavak, R. P., Ocal, B. A. & Soysal, H. A novel anatomical classification of the frontal sinus: Can it be useful in clinical approach to frontal sinusitis?. Egypt. J. Otolaryngol. 37, 34 (2021).
Djorić, I. et al. Multidetector CT of the nasal cavity and paranasal sinuses variations in 73 patients. Indian J. Otolaryngol. Head Neck Surg. 74(3), 4653–4665 (2022).
Testori, T. et al. Maxillary Sinus Surgery and Alternatives in Treatment (Quintessence, 2009).
Rak, K. M. et al. Paranasal sinuses on MR images of the brain: Significance of mucosal thickening. AJR Am. J. Roentgenol. 156, 381–384 (1991).
Hsiao, Y. J., Yang, J., Resnik, R. R. & Suzuki, J. B. Prevalence of maxillary sinus pathology based on cone-beam computed tomography evaluation of multiethnicity dental school population. Implant Dent. 28(4), 356–366 (2019).
Hong, S. L., Cho, K. S. & Roh, H. V. Maxillary sinus retention cysts protruding into the inferior meatus. Clin. Exp. Otorhinolaryngol. 7(3), 226–228 (2014).
Wang, J. H., Jang, Y. J. & Lee, B. J. Natural course of retention cysts of the maxillary sinus: Long-term follow-up results. Laryngoscope 117, 341–344 (2007).
Ata-Ali, J. et al. What is the frequency of anatomical variations and pathological findings in maxillary sinuses among patients subjected to maxillofacial cone beam computed tomography? A systematic review. Med. Oral Patol. Oral y Cirugia Bucal 22(4), e400 (2017).
Larheim, T. A., Abrahamsson, A. K., Kristensen, M. & Arvidsson, L. Z. Temporomandibular joint diagnostics using CBCT. Dentomaxillofac. Radiol. 44(1), 20140235 (2015).
White, S. & Pharaoh, M. Oral Radiology Principles and Interpretation (Elsevier, 2014).
Capelli, M. & Gatti, P. Radiological study of maxillary sinus using CBCT: Relationship between mucosal thickening and common anatomic variants in chronic rhinosinusitis. J. Clin. Diagn Res. 10(11), MC07-MC10 (2016).
Karabaş, H. Ç., Özcan, İ, Göksel, S., Taşyapan, S. & Güray, B. Antrolitin konik ışınlı bilgisayarlı tomografi ile retrospektif olarak değerlendirilmesi. 7tepe Klinik. 18(1), 50–53 (2022).
Ketenci, F., Yeler, D. Y., Koraltan, M. & Ünal, Y. 2019 Evaluation of alveolar pneumatization in maxillary sinus and related factors by panoramic and CBCT imaging methods. 7tepe Klinik. 15(3), 339–344 (2019).
Roque-Torres, G. D., Ramirez-Sotelo, L. R., Vaz, S. L. D. A., Bóscolo, S. M. D. A. D. & Bóscolo, F. N. Association between maxillary sinus pathologies and healthy teeth. Braz. J. Otorhinolaryngol. 82, 33–38 (2016).
Vogiatzi, T., Kloukos, D., Scarfe, W. C. & Bornstein, M. M. Incidence of anatomical variations and disease of the maxillary sinus as identified by cone beam computed tomography: A systematic review. Int. J. Oral Maxillofac. Implant. 29, 1301–1314 (2014).
Sánchez-Pérez, A., Boracchia, A. C., López-Jornet, P. & Boix-García, P. Characterization of the maxillary sinus using cone beam computed tomography A retrospective radiographic study. Implant Dent. 25(6), 762–769 (2016).
Pelinsari Lana, J. et al. Anatomic variations and lesions of the maxillary sinus detected in cone beam computed tomography for dental implants. Clin. Oral Implants Res. 23(12), 1398–1403 (2012).
Blake, F. A. S., Blessmann, M., Pohlenz, P. & Heiland, M. A new imaging modality for intraoperative evaluation of sinus floor augmentation. Int. J. Oral Maxillofac. Surg. 37(2), 183–185 (2008).
Ulm, C. W., Solar, P., Krennmair, G., Matejka, M. & Watzek, G. Incidence and suggested surgical management of septa in sinus-lift procedures. Int. J. Oral Maxillofac. Implants. 10(4), 144–151 (1995).
Betts, N. J. & Miloro, M. Modification of the sinus lift procedure for septa in the maxillary antrum. J. Oral Maxillofac. Surg. 52, 332–333 (1994).
Li, J. et al. An anatomical study of maxillary sinus septum of Han population in Jiangsu region using cone-beam CT. Shanghai Kou Qiang Yi Xue 22(1), 52–57 (2013).
Neugebauer, J. et al. Evaluation of maxillary sinus anatomy by cone-beam CT prior to sinus floor elevation. Int. J. Oral Maxillofac. Implants 25, 258–265 (2010).
Orhan, K. et al. Cone beam CT evaluation of maxillary sinus septa prevalence, height, location and morphology in children and an adult population. Med. Princ. Pract. 22(1), 47–53 (2013).
Tassoker, M. What are the risk factors for maxillary sinus pathologies? A CBCT study. Oral Radiol. 36, 80–84 (2020).
Kocak, N., Alpoz, E. & Boyacıoglu, H. Morphological assessment of maxillary sinus septa variations with cone-beam computed tomography in a Turkish population. Eur. J. Dent. 13(01), 042–046 (2019).
Avsever, H., Gunduz, K., Karakoç, O., Akyol, M. & Orhan, K. Incidental findings on cone-beam computed tomographic images: Paranasal sinus findings and nasal septum variations. Oral Radiol. 34, 40–48 (2018).
Kaya, M., Çankal, F., Gumusok, M., Apaydin, N. & Tekdemir, I. Role of anatomic variations of paranasal sinuses on the prevalence of sinusitis: Computed tomography findings of 350 patients. Niger. J. Clin. Pract. 20(11), 1481–1488 (2017).
Poorey, V. K. & Gupta, N. Endoscopic and computed tomographic evaluation of influence of nasal septal deviation on lateral wall of nose and its relation to sinus diseases. Indian J. Otolaryngol. Head Neck Surg. 66(3), 330–335 (2014).
Taghiloo, H. & Halimi, Z. The frequencies of different types of nasal septum deviation and their effect on increasing the thickness of maxillary sinus mucosa. J. Dent Res. Dent. Clin. Dent Prospects 13(3), 208–214 (2019).
Balikci, H. H., Gurdal, M. M., Celebi, S., Ozbay, I. & Karakas, M. Relationships among concha bullosa, nasal septal deviation, and sinusitis: Retrospective analysis of 296 cases. Ear Nose Throat J. 95(12), 487–491 (2016).
Köse, E., Canger, E. M. & Göller-Bulut, D. Cone beam computed tomographic analysis of paranasal variations, osteomeatal complex disease, odontogenic lesion and their effect on maxillary sinus. Meandros Med. Dent. J. 19, 310–316 (2018).
Gracco, A., Incerti Parenti, S., Ioele, C., Alessandri Bonetti, G. & Stellini, E. Prevalence of incidental maxillary sinus findings in Italian orthodontic patients: a retrospective cone-beam computed tomography study. Korean J. Orthod. 42, 329–334 (2012).
Lu, Y. et al. Associations between maxillary sinus mucosal thickening and apical periodontitis using cone-beam computed tomography scanning: A retrospective study. J. Endod. 38, 1069–1074 (2012).
Block, M. S. & Dastoury, K. Prevalence of sinus membrane thickening and association with unhealthy teeth: A retrospective review of 831 consecutive patients with 1,662 cone-beam scans. J. Oral Maxillofac. Surg. 72, 2454–2460 (2014).
Becker, S. T. et al. Prospective observation of 41 perforations of the Schneiderian membrane during sinus floor elevation. Clin. Oral Implants Res. 19, 1285–1289 (2008).
Aghaee, F., Moudi, E., Vahdani, N., Bijani, A. & Haghanifar, S. Evaluation of anatomical variations of the maxillary sinus in patients with and without mucous retention cyst. Ear Nose Throat J https://doi.org/10.1177/01455613231206284 (2023).
Phothikhun, S., Suphanantachat, S., Chuenchompoonut, V. & Nisapakultorn, K. Cone-beam computed tomographic evidence of the association between periodontal bone loss and mucosal thickening of the maxillary sinus. J. Periodontol. 83(5), 557–564 (2012).
Rege, I. C., Sousa, T. O., Leles, C. R. & Mendonça, E. F. Occurrence of maxillary sinus abnormalities detected by cone beam CT in asymptomatic patients. BMC Oral Health 12, 30 (2012).
Raghav, M., Karjodkar, F. R., Sontakke, S. & Sansare, K. Prevalence of incidental maxillary sinus pathologies in dental patients on cone-beam computed tomographic images. Contemp. Clin. Dent. 5(3), 361–365 (2014).
Schlosser, R. J. et al. Effects of fibrin sealant-containing antibiotics in a rabbit model of chronic sinusitis. Am. J. Rhinol. 14(4), 233–240 (2000).
Dobele, I., Kise, L., Apse, P., Kragis, G. & Bigestans, A. Radiographic assessment of findings in the maxillary sinus using cone-beam computed tomography. Stomatologija 15, 119–122 (2013).
Carmeli, G., Artzi, Z., Kozlovsky, A., Segev, Y. & Landsberg, R. Antral computerized tomography pre-operative evaluation: Relationship between mucosal thickening and maxillary sinus function. Clin. Oral Implants Res. 22(1), 78–82 (2011).
Nascimento, E. H. et al. Association between odontogenic conditions and maxillary sinus disease: A study using cone-beam computed tomography. J. Endod. 42(10), 1509–1515 (2016).
Kuligowski, P. et al. Association between odontogenic and maxillary sinus conditions: A retrospective cone-beam computed tomographic study. J. Clin. Med. 10(13), 2849 (2021).
Author information
Authors and Affiliations
Contributions
MED conceived the research. MED and NU collected and provided the data. NU and MED analyzed the clinical and imaging data. MED and SDY designed the study. NU and MED drafted the manuscript. MED conducted the statistic analysis. MED reviewed the final manuscript. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Dogan, M.E., Uluısık, N. & Yuvarlakbaş, S.D. Retrospective analysis of pathological changes in the maxillary sinus with CBCT. Sci Rep 14, 15529 (2024). https://doi.org/10.1038/s41598-024-66527-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-66527-7
- Springer Nature Limited