Abstract
About 20% of patients with diabetes suffer from chronic pain with neuropathic characteristics. We investigated the multivariate associations between 92 neurology-related proteins measured in serum from 190 patients with painful and painless diabetic neuropathy. Participants were recruited from the Pain in Neuropathy Study, an observational cross-sectional multicentre study in which participants underwent deep phenotyping. In the exploration cohort, two groups were defined by hierarchical cluster analyses of protein data. The proportion of painless vs painful neuropathy did not differ between the two groups, but one group had a significantly higher grade of neuropathy as measured by the Toronto Clinical Scoring System (TCSS). This finding was replicated in the replication cohort. Analyzing both groups together, we found that a group of 11 inter-correlated proteins (TNFRSF12A, SCARB2, N2DL-2, SKR3, EFNA4, LAYN, CLM-1, CD38, UNC5C, GFR-alpha-1, and JAM-B) were positively associated with TCSS values. Notably, EFNA4 and UNC5C are known to be part of axon guidance pathways. To conclude, although cluster analysis of 92 neurology-related proteins did not distinguish painful from painless diabetic neuropathy, we identified 11 proteins which positively correlated to neuropathy severity and warrant further investigation as potential biomarkers.
Similar content being viewed by others
Introduction
Neuropathic pain is defined as pain arising from a lesion or disease of the somatosensory nervous system1. Diabetes is one of the diseases which can cause neuropathic pain. About 20% of diabetic patients suffer from chronic pain with neuropathic characteristics2. Such neuropathic pain is associated with the development of distal symmetrical polyneuropathy (DSP)3,4,5. However, 50–75% of patients with diabetic DSP do not develop neuropathic pain4,5. Although there are well-known risk factors for the development of painful DSP (obesity, glycemic burden, and female sex6,7, and although there is an association between the severity of neuropathy and neuropathic pain8, it is still unclear why some patients with diabetic DSP develop neuropathic pain while others do not9. We have previously reported that, in patients with diabetic DSP, it was possible to identify a higher-inflammation subgroup in which high levels of hepatocyte growth factor, colony-stimulating factor 1, CD40 and 11 other inflammation-related proteins were associated with more severe neuropathy and higher pain intensity10.
Even when evidence-based first-line medicines such as tricyclics/duloxetine or gabapentinoids are prescribed adequately, only a minority of patients with neuropathic pain get substantial pain relief, the numbers needed to treat for > 30–50% pain relief ranging between 4 and 811. For a majority of neuropathic pain patients, adequate pain relief will not be achieved. Importantly, there is a substantial “translational gap” between the achievements of preclinical (rodent) models of neuropathic pain and clinical reality12,13,14. In this context of deeply unmet medical needs, it has been suggested that human biomarker studies could be a way to bridge the translation gap15, e.g., by conducting proteomic studies16. Another way to explore the pathophysiology of different neurological conditions in humans is to use panels of pre-selected proteins such as, for instance, the Olink Neurology panel17. The 92 proteins of the Olink Neurology panel are a mix of established markers related to neurobiological processes and neurological diseases (e.g., neural development, axon guidance, synaptic function, or specific conditions such as Alzheimer’s disease), as well as some more exploratory proteins with broader roles in processes such as cellular regulation, immunology, development, and metabolism18.
The aim of this exploration and replication study was to investigate the multivariate associations between 92 neurology-related proteins measured in serum from diabetic DSP patients and clinical characteristics including pain intensity and neuropathy severity. Study participants were recruited as part of the Pain in Neuropathy Study (PiNS)8 and dichotomized into painful and painless diabetic DSP.
Methods
Overview and study rationale
Before any statistical analysis, the 190 study participants were randomized into an exploration (n = 95) and a replication (n = 95) cohort by using the random function in Microsoft Excel. The randomization was “frozen” in a pdf file on 20 May 2020. An underlying assumption in the present work is that (partly) different pathophysiological mechanisms might be at work in subgroups of patients suffering from painful diabetic DSP10. It has been suggested that many clinical disease entities may be umbrella terms encompassing several molecular mechanisms that share prominent signs and symptoms19. Therefore, our strategy in the present paper was to use cluster analysis to first define subgroups of patients based on the correlation structure of the analysed neurology-related proteins, the hypothesis being that such subgroups would be clinically meaningful. Such a strategy partly resembles that of Baron et al.20 who clustered peripheral neuropathic pain patients using quantitative sensory testing (QST). However, our subgrouping strategy is based not on psychophysical but on biological data, i.e., on protein levels. This approach is consistent with a systems medicine perspective, in which groups of interest are defined using “mechanism-based stratification”19 instead of the more conventional focus on signs and symptoms.
Patients and clinical data
PiNS is an observational cross-sectional multicentre study in which participants underwent deep phenotyping that included neuropathy screening tools, extensive symptom and function questionnaires, neurological examination, nerve conduction studies, quantitative sensory testing, and skin biopsy for intraepidermal nerve fibre density assessment (IENFD) in a sub-set of patients8. Patients with diabetes mellitus aged above 18 years with diagnosed DSP, or patients with symptoms and signs suggestive of DSP were included. Exclusion criteria were pregnancy, coincident major psychiatric disorders, poor or no English language skills, severe pain at recruitment from a cause other than DSP (to prevent potential confounding influence on pain reporting as well as psychological and quality-of-life reported outcomes), patients with documented central nervous system lesions, or patients with insufficient mental capacity to provide informed consent or to complete questionnaires. Many of the study participants were recruited from primary care practices in London and Oxford. Study participants were also recruited from diabetes and other clinics at Chelsea and Westminster Hospital NHS Foundation Trust (London), Sheffield Teaching Hospitals and Oxford University Teaching Hospitals, neurology clinics at King’s College Hospital (London), and through advertisements.
Participants were included consecutively in PiNS until target number was reached. In PiNS, participants are dichotomized in painless and painful diabetic DSP. The methods and questionnaires have been previously described in detail8. Participants included in the present biomarker study were those where serum, and neuropathic pain grading according to IASP/NeuPSIG, were available21. We applied the NeupSIG grading system for neuropathic pain to pain in the feet as being the plausible anatomical distribution when separating those with painful versus painless diabetic neuropathy. In the present study, the following clinical variables were available for both painless and painful neuropathy patients:
-
Age and sex
-
Data pertaining to diabetes and metabolic control (Body Mass Index (BMI; kg/m2), diabetes type 1 or type 2, HbA1c)
-
Data related to neuropathy—the Toronto Clinical Scoring System (TCSS) correlates with diabetic neuropathy severity22. Based on TCSS, patients can be classified as having no DSP (TCSS 0–5), mild DSP (TCSS 6–8), moderate DSP (TCSS 9–11), or severe DSP (TCSS 12–19)23.
-
Douleur Neuropathique en 4 Questions (DN4) which can be used as a screening tool for neuropathic pain24.
Clinical variables available in patients with painful neuropathy were Brief Pain Inventory (BPI) severity scores25, Neuropathic Pain Symptoms Inventory (NPSI)26, and PainDetect27.
Protein data
A 10 ml blood sample (BD Vacutainer SST Tubes) was drawn from each participant. After 30 min, to allow blood to clot, the sample was centrifuged at 3000 rpm for 10 min at a temperature of 4 °C. Serum was then aliquoted into 1.8 ml Nunc CryoTubes and stored at – 80 °C.
The Olink Neurology panel (product number 95801, v. 8012) provides a high-throughput, multiplex immunoassay enabling the analysis of 92 neurology-related protein biomarkers at the same time using a Proximity Extension Assay (PEA) technology28,29,30,31. PEA means that a pair of oligonucleotide-labelled antibodies bind to their respective target protein. When the two antibodies are close to each other, a polymerase chain reaction (PCR) is initiated which is then quantified by real time PCR. Results are expressed as Normalized Protein eXpression (NPX), which is relative quantification between samples, on a Log2 scale. A high NPX value equals a high protein concentration. Because NPX is a Log2 scale, a difference of 1 in NPX means a doubling of protein concentration. If needed, NPX values can be converted into a linear scale according to 2NPX = linear NPX. A complete list of the 92 neurology-related proteins, including their UniProt ID, is found in Supplemental Digital Content 1 (see Supplementary Information 1). The URL leading to validation data provided by Olink is available here: https://www.olink.com/content/uploads/2021/09/olink-neurology-validation-data-v2.1.pdf (Access date April 30, 2024).
Statistics
Data are expressed as median (IQR), unless stated otherwise. SIMCA (version 16, Sartorius Stedim Biotech, Umeå, Sweden) was used for multivariate data analysis (MVDA). SPSS (version 26, IBM Corporation, Route 100 Somers, New York, USA) was used for all other analyses (Mann–Whitney U test, Chi-Square test, Spearman’s rho for bivariate correlations, and multiple linear regression (MLR), as appropriate). A significance level of 0.05 was chosen.
The same procedures were conducted in the exploration (n = 95) and in the replication (n = 95) cohorts. Details concerning MVDA methodology32,33 have been described in previous publications30,34,35,36,37,38,39. Briefly, we performed principal component analysis (PCA), hierarchical clustering analysis (HCA) and, based on the groups defined by HCA, orthogonal partial least squares (-discriminant analysis) (OPLS and OPLS-DA). PCA is a technique that models the correlation structure of a dataset, and thereby enables the identification of multivariate outliers32,33. Principal components (PC) extract relevant information found in the data, reducing a high-dimensional space (high number of variables) to a few “summary variables”. After outlier detection with PCA (strong outliers defined as Hotelling’s T2>>T2Crit(99%) and moderate outliers as DModX>2*DCrit), we applied a bottom-up HCA to the principal component score vectors using the default Ward linkage criterion to identify relevant subgroups of patients. HCA complements PCA in the sense that while PCA identifies distinct clusters in multivariate space, HCA can find subtle clusters. In the resulting dendrogram, interesting patient subgroups were identified, and clinical data were compared between subgroups to ascertain the clinical relevance of the subgroups. Then, OPLS-DA was performed using group belonging as Y-variables and protein data as predictors (X-variables). To identify the proteins most relevant for group discrimination, the OPLS-DA models analyzed and identified associations between the X-variables and group belonging. X-variables with |p(corr)|≥ 0.5 are usually considered important for group discrimination32, the sign of p(corr) denoting the direction of the association (described in text in each case). However, in some cases, a tougher cut-off of |p(corr)|≥ 0.6 was used instead in this study. P(corr) is the loading of each X-variable scaled as a correlation coefficient that is comparable between models. MVDA analyzes all variables simultaneously, using the overall correlation pattern present in the data, hence separating information from “noise”. Hence, the protein data in the present study were not primarily analyzed by multiple univariate testing, thereby minimizing the multiple testing problem. In a third step, both cohorts were analyzed together in an OPLS model with TCSS as outcome (Y) variable—see text below for rationale. For this third step, a false discovery rate (FDR) at the 10% level was applied using the Benjamini–Hochberg procedure40.
Ethics
The study was approved by the National Research Ethics Service of the United Kingdom (No.:10/H07056/35). All study participants signed written consent before participating. The research was conducted in accordance with the Declaration of Helsinki.
Results
Two proteins out of 92 had > 20% missing values and were therefore excluded from all analyses. All results are based on the remaining 90 proteins. An overview of clinical data in painless vs. painful patients is presented in Table 1.
First phase of protein analyses: exploration cohort
The exploration cohort consisted of 95 patients. Two patients (ID 30483 and ID 30519) were excluded because of quality warning from Olink Bioscience (Uppsala, Sweden). On the remaining 93 patients, a PCA was done using the 90 proteins as X-variables (4 PCs, R2 = 0.52, Q2 = 0.38); no outlier was found. By HCA, 2 groups were defined (Group 1, n = 37 and Group 2, n = 56). Then, the clinical variables were compared between the two groups, i.e., we wanted to see if they seemed clinically meaningful. In the exploration cohort (Table 2, left side), TCSS was significantly higher in Group 2 (11 (8–15) vs. 8.5 (6–12), p = 0.027). The other clinical variables did not differ between groups in the exploration cohort. Finally, an OPLS-DA was done with group belonging (Group 1 vs 2) as Y-variable; the model had 2 latent variables (one predictive and one orthogonal component), R2 = 0.69, Q2 = 0.57, and p < 0.001 by CV-ANOVA. The proteins most responsible for group discrimination, i.e., with |p(corr)|≥ 0.6 for the first (predictive) latent variable, are listed in Table 3, left column.
Second phase of protein analyses: replication cohort
After an initial PCA on the 95 patients of the replication cohort using the 90 proteins as X-variables, one patient (ID 30087) was excluded for being a multivariate outlier by Hotelling’s T2. Hence, the new PCA model had 94 patients, with 4 PCs, R2 = 0.53, Q2 = 0.40. By HCA, 2 groups were defined (Group 1, n = 31 and Group 2, n = 63). Then, we tested the hypothesis that TCSS scores would differ between Group 1 and 2. We found that, just as in the exploration cohort, Group 2 had significantly higher TCSS scores: (12.5 (9–14) vs. 10 (8.5–12), p = 0.016) (Table 2, right side). Age was also significant (p = 0.003) (Table 2). Hence, the findings concerning TCSS were replicated. Finally, an OPLS-DA was done with group belonging (Group 1 vs 2) as Y-variable; the model had 1 latent variable (i.e., one predictive component), R2 = 0.56, Q2 = 0.53, and p < 0.001 by CV-ANOVA. The proteins most responsible for group discrimination, i.e., with |p(corr)|≥ 0.6, are listed in Table 3, right side. Notably, 70% of the top ten proteins of the exploration cohort were top 10 in the replication cohort (see text in red in Table 3) and 85% of the top 20 proteins of the exploration cohort were top 20 in the replication cohort (see text in blue in Table 3).
Third phase: in-depth analysis of TCSS in all patients
In third phase of the study, we focused on TCSS, using both cohorts taken together (n = 186; TCSS was missing in one patient). Using TCSS as Y-variable and the 90 proteins as X-variables, we computed an OPLS model which had 2 latent variables (one predictive and one orthogonal), R2 = 0.31, Q2 = 0.10, p < 0.001 by CV-ANOVA. The proteins most associated with TCSS are tabulated in Table 4; the overlap with the two OPLS-DA models in Table 3 is also illustrated.
Because of a possible age issue (see Table 2), we next computed a new OPLS model, with age as Y variable to be able to exclude age-related proteins from the results of Table 4. This age model had 3 latent variables (one predictive and two orthogonal), n = 186, R2 = 0.64, Q2 = 0.45, p < 0.001 by CV-ANOVA. We found 4 proteins with |p(corr)|≥ 0.4 (see note in Table 4 for choice of p(corr) level), indicating a possible association with age, and EDA2R, the top protein in Table 4, had the highest p(corr) in the age-model (positive correlation with age and p(corr) = 0.5). Therefore, EDA2R was excluded from the main results of the study (see below).
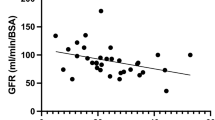
Hence, the 11 proteins with p(corr) ≥ 0.5 in Table 4 (i.e., excluding EDA2R as per above) were the main findings of the present study, and all correlated positively with TCSS in multivariate space. Additionally, we also computed bivariate correlations between TCSS and the 11 proteins, finding that the 11 proteins had highly significant correlations with TCSS, with rho ranging from 0.19 to 0.32. These 11 correlations remained significant when applying a false discovery rate (FDR) of 10% (calculated for 90 bivariate correlations between TCSS and each protein). The 11 proteins also all inter-correlated significantly with each other (all p-values < 0.001) with rho ranging from 0.51 to 0.88—hence confirming the validity of this cluster of proteins which together correlated positively with TCSS (as per the OPLS model above). The 11 proteins are described briefly together with their Uniprot ID in Table 5. To further descriptively get a sense the effect sizes involved, we calculated the percentage increases of median values of linearized NPX in those having severe DSP compared to those not having DSP (defined as TCSS < 6, n = 18), see Table 5. Rho-values (i.e., correlation with TCSS) are also listed in Table 5. Also, the relationship between the 11 proteins and TCSS is visualized in Supplemental Digital Content 2 (see Supplementary Figures).
Using the 11 proteins as per above, we computed a PCA model, n = 186, 1 PC, R2 = 0.77, Q2 = 0.72. We used the scores of the PC of the PCA model as a “summary” variable of the 11 proteins, here called PC1_11prot. We did a multiple linear regression (MLR) with TCSS as outcome variable (dependent variable) and with the following variables as predictors: PC1_11prot, sex, age, BMI, and HbA1c. The MLR model was significant (adjusted R2 = 0.155 and p < 0.001) and PC1_11prot was significant (p = 0.001 with a positive coefficient, i.e., a positive correlation between PC1_11prot and TCSS) when adjusted for sex, age, BMI and HbA1c.
Fourth phase: in-depth analysis of BPI scores in patients with painful neuropathy
Finally, we did an in-depth analysis of BPI scores in patients with painful neuropathy. In the exploratory cohort, only “BPI now” differed when comparing Groups 1 and 2, Group 2 (n = 28) having statistically significant higher levels than Group 1 (n = 15): 6,5 (4–8) vs. 3 (1, 5–6), p = 0.019; this remained significant at FDR 10%, the critical value being 0.02. In the replication cohort however, none of the BPI scores differed between Groups 1 and 2. “BPI now” in the replication cohort was 6 (4–7) in Group 1 (n = 14) vs 4 (2–6) in Group 2 (n = 33), p = 0.205 (i.e., a non-significant tendency for “BPI now” to be lower in Group 2). Hence, the findings of “BPI now” in the exploratory cohort could not be replicated.
Discussion
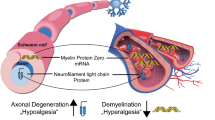
A panel of 92 neurology-related proteins was used to investigate potential biomarkers of painful and painless diabetic DSP in a deeply phenotyped cohort. We found that 11 proteins were associated with the severity of neuropathy (but not with the presence of neuropathic pain). These 11 proteins have a variety of biological functions such as inflammatory processes, growth factors, adhesion molecules and axon guidance (Table 5). Neuropathic pain is known to positively correlate with the severity of peripheral neuropathy8. However, given its complex aetiology involving multiple pathophysiological drivers in the central as well as peripheral nervous system41, it is not surprising that we may find molecular correlates of neuropathy severity that are independent of neuropathic pain.
One biological process that was highlighted in our findings was axon guidance with the identification of EFNA4 and UNC5C. Ephrins, to which EFNA4 belongs, is one of five known families of axon guidance proteins42. Axon guidance pathways seem to be involved in diabetic DSP43. Interestingly, Evdokimov et al.44 studied EFNA4 in skin biopsies from fibromyalgia patients vs. controls, finding that the expression of EFNA4 was higher in fibromyalgia patients. Axon guidance proteins are detected by a structure at the tip of growing axons—the growth cone42. Different receptors are present on the growth cone, one of them being UNC5C, which is another of the main findings listed in Table 5. UNC5C in turn binds to the netrin family of axon guidance proteins42. In diabetic DSP, both nerve degeneration and regeneration are present45, and the question therefore arises if EFNA4 and UNC5C can perhaps be seen as potential biomarkers for nerve de- and/or re-generation in this setting? This is of course highly speculative and should be investigated in further studies. It should also be noted that ephrins and netrins have been implicated in central processes related to (neuropathic) pain46,47,48,49, and that UNC5C has been investigated in the context of endometriosis-related (and supposedly neuropathic) pain50. Moreover, although it was not associated to TCSS as per Table 4, the ephrin EPHB6 was nonetheless a main finding in both the exploration and the replication cohorts as per Table 3.
Given previous finding about chronic inflammation in painful and painless diabetic DSP10, our findings about GFR-alpha-1 and CD38 are also interesting (Table 5). CD38 is immunomodulatory51 and has been deemed to be a possible pharmacological target. In mice, Gil and co-workers studied CD38 in the context of osteoarthritis, concluding that inhibition of CD38 could potentially be a novel therapeutic approach for the treatment of osteoarthritis and associated pain52. GFR-alpha-1 is the receptor for GDNF—which in turn is connected to inflammation53. GDNF has also been shown to have neuroprotective actions on sensory neurons following traumatic axotomy54 and in experimental models of diabetic neuropathy55. Hence, although the pain literature contains scarce information about the potential biomarkers listed in Table 5, at least five of them can be related to neuropathy/pain in different ways. It should be noted that Neurofilament light chain, a potential biomarker ford diabetic DSP56, was not part of the panel of proteins in the present study.
In our opinion, the present study has some obvious strengths. Before any statistical analysis of the data, the material was dichotomized into two cohorts, enabling us to implement an exploration-replication strategy which confirmed that the subgroup characterized by high levels of the proteins listed in Table 3 had higher levels of neuropathy as expressed by TCSS (Table 2). Hence, although this paper is hypothesis-generating in the sense that it used a panel of neurology-related proteins (and thus no specific candidate proteins), there is also an element of confirmatory methodology inherent in the exploration-replication design. Moreover, as in previous work10, we used an unbiased clustering approach to subgroup the patient on biological grounds. Hence, instead of merely comparing painful and painless participants, we stratified the material according to a systems biology perspective—and this stratification was then shown to be clinically relevant, albeit not directly pain-wise. The idea behind this approach is that there might be different mechanisms at play in different patients who have the same symptoms and signs, and that a simple comparison based on phenotype might thus blur the picture more than a comparison of clusters based on biology. Whether this “mechanism-based stratification”19 approach is really advantageous will of course have to be confirmed or falsified in future studies. Concerning the fact that we did not find a pain signal, it is of course important to remember the subjective and biopsychosocial nature of the pain experience. Elucidating the biology underlying the subjective experience is a task as difficult as it is important15,57,58. Pain biomarker studies are undertaken with methods from different fields, e.g., imaging methods59, electrophysiology60, or ‘omics16. Recent advances concerning the role of calcitonin gene-related peptide (CGRP) in migraine61 should give pain researchers some confidence that the search for biomarkers reflecting the pathophysiology of different chronic pain conditions is hopefully not a futile task.
Obvious study limitations include the cross-sectional design and the possibility of confounders such as for instance concomitant medication (although our findings seem robust when it comes to the influence of sex, age, BMI and HbA1c). The possibility of there being a systematic error in the material cannot be ruled out. Also, even if our results would turn out to be valid in the sense that they really reflect neuropathy-related pathophysiology, it is still important to consider whether the described “fingerprint” relates directly to the pathophysiology of neuropathy, or if perhaps it is a risk factor that was present prior to the development of neuropathy. A third possibility could be that the fingerprint is an epiphenomenon, perhaps more related to co-morbidities such as insomnia or depression. Disentangling the contribution of potentially mutually interacting factors is a challenge and will require longitudinal studies. Fourth, when measuring multiple analytes in a single experiment, antibody specificity is an important issue to be aware of. The PEA technology28,29,30,31 builds on dual recognition, i.e., a pair of oligonucleotide-labelled antibodies have to bind to their respective target protein to generate a signal, leading to higher specificity compared to methods based on a single antibody. This fact notwithstanding, the question marks raised by the specificity issue remain a major limitation in the present work. The findings should therefore be interpreted cautiously, warranting further replication studies using alternative methods of detection.
To conclude, in Table 5 we present a list of 11 inter-correlated proteins who were positively correlated to the severity of neuropathy in DSP patients but not to the presence of neuropathic pain. These may have potential as novel biomarkers for diabetic neuropathy which are increasingly important as new understanding of axon degeneration has led to novel drug targets to prevent axon degeneration. The validity and clinical relevance of these putative neuropathy biomarkers will need to be confirmed in future longitudinal studies.
Data availability
Data cannot be made publicly available because of the lack of ethical permission. If the corresponding author is contacted, reasonable data requests can be considered.
References
Finnerup, N. B. et al. Neuropathic pain: An updated grading system for research and clinical practice. Pain 157, 1599–1606. https://doi.org/10.1097/j.pain.0000000000000492 (2016).
Bouhassira, D., Letanoux, M. & Hartemann, A. Chronic pain with neuropathic characteristics in diabetic patients: A French cross-sectional study. PLoS One 8, e74195. https://doi.org/10.1371/journal.pone.0074195 (2013).
Ziegler, D. Diabetic polyneuropathy. Internist (Berl.) 61, 243–253. https://doi.org/10.1007/s00108-020-00770-8 (2020).
Van Acker, K. et al. Prevalence and impact on quality of life of peripheral neuropathy with or without neuropathic pain in type 1 and type 2 diabetic patients attending hospital outpatients clinics. Diabetes Metab. 35, 206–213. https://doi.org/10.1016/j.diabet.2008.11.004 (2009).
Abbott, C. A., Malik, R. A., van Ross, E. R., Kulkarni, J. & Boulton, A. J. Prevalence and characteristics of painful diabetic neuropathy in a large community-based diabetic population in the UK. Diabetes Care 34, 2220–2224. https://doi.org/10.2337/dc11-1108 (2011).
Rosenberger, D. C., Blechschmidt, V., Timmerman, H., Wolff, A. & Treede, R. D. Challenges of neuropathic pain: Focus on diabetic neuropathy. J. Neural Transm. (Vienna) 127, 589–624. https://doi.org/10.1007/s00702-020-02145-7 (2020).
Elliott, J. H. et al. Female sex is a risk factor for Painful-Diabetic Peripheral Neuropathy: The EURODIAB Prospective Diabetes Complications Study for the EURODIAB Prospective Complications Study Group. Diabetologia 67, 190 (2023).
Themistocleous, A. C. et al. The Pain in Neuropathy Study (PiNS): A cross-sectional observational study determining the somatosensory phenotype of painful and painless diabetic neuropathy. Pain 157, 1132–1145. https://doi.org/10.1097/j.pain.0000000000000491 (2016).
Shillo, P. et al. Painful and painless diabetic neuropathies: What is the difference?. Curr. Diab. Rep. 19, 32. https://doi.org/10.1007/s11892-019-1150-5 (2019).
Bäckryd, E. et al. Hepatocyte growth factor, colony-stimulating factor 1, CD40, and 11 other inflammation-related proteins are associated with pain in diabetic neuropathy: Exploration and replication serum data from the Pain in Neuropathy Study. Pain 163, 897–909. https://doi.org/10.1097/j.pain.0000000000002451 (2022).
Finnerup, N. B. et al. Pharmacotherapy for neuropathic pain in adults: A systematic review and meta-analysis. Lancet Neurol. 14, 162–173. https://doi.org/10.1016/S1474-4422(14)70251-0 (2015).
Eisenach, J. C. & Rice, A. S. C. Improving preclinical development of novel interventions to treat pain: Insanity is doing the same thing over and over and expecting different results. Anesth. Analg. 135, 1128–1136. https://doi.org/10.1213/ane.0000000000006249 (2022).
Rice, A. S. C., Finnerup, N. B., Kemp, H. I., Currie, G. L. & Baron, R. Sensory profiling in animal models of neuropathic pain: A call for back-translation. Pain 159, 819–824. https://doi.org/10.1097/j.pain.0000000000001138 (2018).
Andrews, N. A. et al. Ensuring transparency and minimization of methodologic bias in preclinical pain research: PPRECISE considerations. Pain 157, 901–909. https://doi.org/10.1097/j.pain.0000000000000458 (2016).
Bäckryd, E. Pain in the blood? Envisioning mechanism-based diagnoses and biomarkers in clinical pain medicine. Diagnostics 5, 84–95 (2015).
Gerdle, B. & Ghafouri, B. Proteomic studies of common chronic pain conditions—a systematic review and associated network analyses. Expert Rev. Proteom. 17, 483–505. https://doi.org/10.1080/14789450.2020.1797499 (2020).
Harris, S. E. et al. Neurology-related protein biomarkers are associated with cognitive ability and brain volume in older age. Nat. Commun. 11, 800. https://doi.org/10.1038/s41467-019-14161-7 (2020).
Olink for Neurology Applications (2022, accessed 26 Oct 2022). https://www.olink.com/application/olink-for-neurology-studies/.
Comte, B. et al. Network and systems medicine: position paper of the European Collaboration on science and technology action on open multiscale systems medicine. Netw. Syst. Med. 3, 67–90. https://doi.org/10.1089/nsm.2020.0004 (2020).
Baron, R. et al. Peripheral neuropathic pain: A mechanism-related organizing principle based on sensory profiles. Pain 158, 261–272. https://doi.org/10.1097/j.pain.0000000000000753 (2017).
Treede, R. D. et al. Neuropathic pain: redefinition and a grading system for clinical and research purposes. Neurology 70, 1630–1635. https://doi.org/10.1212/01.wnl.0000282763.29778.59 (2008).
Bril, V. & Perkins, B. A. Validation of the Toronto Clinical Scoring System for diabetic polyneuropathy. Diabetes Care 25, 2048–2052. https://doi.org/10.2337/diacare.25.11.2048 (2002).
Hashem, M. M., Esmael, A., Nassar, A. K. & El-Sherif, M. The relationship between exacerbated diabetic peripheral neuropathy and metformin treatment in type 2 diabetes mellitus. Sci. Rep. 11, 1940. https://doi.org/10.1038/s41598-021-81631-8 (2021).
Bouhassira, D. et al. Comparison of pain syndromes associated with nervous or somatic lesions and development of a new neuropathic pain diagnostic questionnaire (DN4). Pain 114, 29–36. https://doi.org/10.1016/j.pain.2004.12.010 (2005).
Tan, G., Jensen, M. P., Thornby, J. I. & Shanti, B. F. Validation of the Brief Pain Inventory for chronic nonmalignant pain. J. Pain 5, 133–137. https://doi.org/10.1016/j.jpain.2003.12.005 (2004).
Bouhassira, D. et al. Development and validation of the neuropathic pain symptom inventory. Pain 108, 248–257. https://doi.org/10.1016/j.pain.2003.12.024S030439590400003X (2004).
Freynhagen, R., Baron, R., Gockel, U. & Tölle, T. R. painDETECT: A new screening questionnaire to identify neuropathic components in patients with back pain. Curr. Med. Res. Opin. 22, 1911–1920. https://doi.org/10.1185/030079906x132488 (2006).
Assarsson, E. et al. Homogenous 96-plex PEA immunoassay exhibiting high sensitivity, specificity, and excellent scalability. PLoS One 9, e95192. https://doi.org/10.1371/journal.pone.0095192 (2014).
Lundberg, M., Eriksson, A., Tran, B., Assarsson, E. & Fredriksson, S. Homogeneous antibody-based proximity extension assays provide sensitive and specific detection of low-abundant proteins in human blood. Nucleic Acids Res. 39, e102. https://doi.org/10.1093/nar/gkr424 (2011).
Bäckryd, E. et al. High levels of cerebrospinal fluid chemokines point to the presence of neuroinflammation in peripheral neuropathic pain: A cross-sectional study of 2 cohorts of patients compared with healthy controls. Pain 158, 2487–2495. https://doi.org/10.1097/j.pain.0000000000001061 (2017).
Nordberg, N. & Ohlsson, S. Advancing Precision Medicine: Current and Future Proteogenomic Strategies for Biomarker Discovery and Development, vol. 31 (Science/AAAS, 2017).
Eriksson, L., Byrne, T., Johansson, E., Trygg, J. & Vikström, C. Multi- and Megavariate Data Analysis: Basic Principles and Applications, 3rd edn (MKS Umetrics AB, 2013).
Wheelock, A. M. & Wheelock, C. E. Trials and tribulations of ’omics data analysis: Assessing quality of SIMCA-based multivariate models using examples from pulmonary medicine. Mol Biosyst. 9, 2589–2596. https://doi.org/10.1039/c3mb70194h (2013).
Bäckryd, E., Ghafouri, B., Carlsson, A. K., Olausson, P. & Gerdle, B. Multivariate proteomic analysis of the cerebrospinal fluid of patients with peripheral neuropathic pain and healthy controls—a hypothesis-generating pilot study. J. Pain Res. 8, 321–333. https://doi.org/10.2147/JPR.S82970 (2015).
Gerdle, B., Ghafouri, B., Ghafouri, N., Backryd, E. & Gordh, T. Signs of ongoing inflammation in female patients with chronic widespread pain: A multivariate, explorative, cross-sectional study of blood samples. Med. Baltim. 96, e6130. https://doi.org/10.1097/MD.0000000000006130 (2017).
Bäckryd, E., Persson, E. B., Larsson, A. I., Fischer, M. R. & Gerdle, B. Chronic pain patients can be classified into four groups: Clustering-based discriminant analysis of psychometric data from 4665 patients referred to a multidisciplinary pain centre (a SQRP study). PLoS One 13, e0192623. https://doi.org/10.1371/journal.pone.0192623 (2018).
Gerdle, B., Backryd, E., Falkenberg, T., Lundstrom, E. & Ghafouri, B. Changes in inflammatory plasma proteins from patients with chronic pain associated with treatment in an interdisciplinary multimodal rehabilitation program—an explorative multivariate pilot study. Scand. J. Pain 20, 125–138. https://doi.org/10.1515/sjpain-2019-0088 (2019).
Bäckryd, E., Tanum, L., Lind, A. L., Larsson, A. & Gordh, T. Evidence of both systemic inflammation and neuroinflammation in fibromyalgia patients, as assessed by a multiplex protein panel applied to the cerebrospinal fluid and to plasma. J. Pain Res. 10, 515–525 (2017).
Olausson, P. et al. Protein alterations in women with chronic widespread pain—an explorative proteomic study of the trapezius muscle. Sci. Rep. 5, 11894. https://doi.org/10.1038/srep11894 (2015).
Glickman, M. E., Rao, S. R. & Schultz, M. R. False discovery rate control is a recommended alternative to Bonferroni-type adjustments in health studies. J. Clin. Epidemiol. 67, 850–857. https://doi.org/10.1016/j.jclinepi.2014.03.012 (2014).
Jensen, T. S. et al. Painful and non-painful diabetic neuropathy, diagnostic challenges and implications for future management. Brain J. Neurol. 144, 1632–1645. https://doi.org/10.1093/brain/awab079 (2021).
Van Battum, E. Y., Brignani, S. & Pasterkamp, R. J. Axon guidance proteins in neurological disorders. Lancet Neurol. 14, 532–546. https://doi.org/10.1016/s1474-4422(14)70257-1 (2015).
Guo, K. et al. Genome-wide profiling of DNA methylation and gene expression identifies candidate genes for human diabetic neuropathy. Clin. Epigenet. 12, 123. https://doi.org/10.1186/s13148-020-00913-6 (2020).
Evdokimov, D. et al. Pain-associated mediators and axon pathfinders in fibromyalgia skin cells. J. Rheumatol. 47, 140–148. https://doi.org/10.3899/jrheum.190248 (2020).
Bönhof, G. J. et al. Patterns of cutaneous nerve fibre loss and regeneration in type 2 diabetes with painful and painless polyneuropathy. Diabetologia 60, 2495–2503. https://doi.org/10.1007/s00125-017-4438-5 (2017).
Li, J., Wang, G., Weng, Y., Ding, M. & Yu, W. Netrin-1 contributes to peripheral nerve injury induced neuropathic pain via regulating phosphatidylinositol 4-kinase IIa in the spinal cord dorsal horn in mice. Neurosci. Lett. 735, 135161. https://doi.org/10.1016/j.neulet.2020.135161 (2020).
Vasileiou, I., Adamakis, I., Patsouris, E. & Theocharis, S. Ephrins and pain. Expert Opin. Ther. Targets 17, 879–887. https://doi.org/10.1517/14728222.2013.801456 (2013).
Damo, E. & Simonetti, M. Axon guidance molecules and pain. Cells 2022, 11. https://doi.org/10.3390/cells11193143 (2022).
Khangura, R. K., Sharma, J., Bali, A., Singh, N. & Jaggi, A. S. An integrated review on new targets in the treatment of neuropathic pain. Korean J. Physiol. Pharmacol. 23, 1–20. https://doi.org/10.4196/kjpp.2019.23.1.1 (2019).
Ding, S. et al. Macrophage-derived netrin-1 contributes to endometriosis-associated pain. Ann. Transl. Med. 9, 29. https://doi.org/10.21037/atm-20-2161 (2021).
Piedra-Quintero, Z. L., Wilson, Z., Nava, P. & Guerau-de-Arellano, M. CD38: An immunomodulatory molecule in inflammation and autoimmunity. Front. Immunol. 11, 597959. https://doi.org/10.3389/fimmu.2020.597959 (2020).
Gil Alabarse, P., Chen, L. Y., Oliveira, P., Qin, H. & Liu-Bryan, R. Targeting CD38 to suppress osteoarthritis development and associated pain after joint injury in mice. Arthrit. Rheumatol. Hobok. N. J. https://doi.org/10.1002/art.42351 (2022).
Kotliarova, A. & Sidorova, Y. A. Glial cell line-derived neurotrophic factor family ligands, players at the interface of neuroinflammation and neuroprotection: Focus onto the glia. Front. Cell. Neurosci. 15, 679034. https://doi.org/10.3389/fncel.2021.679034 (2021).
Bennett, D. L. et al. A distinct subgroup of small DRG cells express GDNF receptor components and GDNF is protective for these neurons after nerve injury. J. Neurosci. 18, 3059–3072. https://doi.org/10.1523/jneurosci.18-08-03059.1998 (1998).
Akkina, S. K., Patterson, C. L. & Wright, D. E. GDNF rescues nonpeptidergic unmyelinated primary afferents in streptozotocin-treated diabetic mice. Exp. Neurol. 167, 173–182. https://doi.org/10.1006/exnr.2000.7547 (2001).
Maalmi, H. et al. Serum neurofilament light chain: A novel biomarker for early diabetic sensorimotor polyneuropathy. Diabetologia 66, 579–589. https://doi.org/10.1007/s00125-022-05846-8 (2023).
Davis, K. D. et al. Discovery and validation of biomarkers to aid the development of safe and effective pain therapeutics: Challenges and opportunities. Nat. Rev. Neurol. 16, 381–400. https://doi.org/10.1038/s41582-020-0362-2 (2020).
Tracey, I., Woolf, C. J. & Andrews, N. A. Composite pain biomarker signatures for objective assessment and effective treatment. Neuron 101, 783–800. https://doi.org/10.1016/j.neuron.2019.02.019 (2019).
Lee, M. C. & Tracey, I. Imaging pain: A potent means for investigating pain mechanisms in patients. Br. J. Anaesth. 111, 64–72. https://doi.org/10.1093/bja/aet174 (2013).
Serra, J. Microneurography: Towards a biomarker of spontaneous pain. Pain 153, 1989–1990. https://doi.org/10.1016/j.pain.2012.07.008 (2012).
Juhasz, G., Gecse, K. & Baksa, D. Towards precision medicine in migraine: Recent therapeutic advances and potential biomarkers to understand heterogeneity and treatment response. Pharmacol. Therapeut. 2023, 108523. https://doi.org/10.1016/j.pharmthera.2023.108523 (2023).
Acknowledgements
E. Bäckryd reports grants from ALF Grants, Region Östergötland, and from NEURO Sweden (EB).
Funding
Open access funding provided by Linköping University.
Author information
Authors and Affiliations
Contributions
Conceptualization: EB, AT, AL, TG, ASCR, ST, DLB, BG. Data curation: EB, AT. Formal analysis: EB, BG. Writing—original draft: EB. Writing—review & editing: EB, AT, AL, TG, ASCR, ST, DLB, BG.
Corresponding author
Ethics declarations
Competing interests
A.T., A.L., E.B., B.G., and T.G. have no conflict of interest to declare. Andrew SC Rice (ASCR) was a Principal Investigator/director of the Wellcome Trust funded London Pain Consortium through which the PiNS study was funded. ASCR declares the following interests unrelated to this manuscript occurring in last 36 months: Employee Imperial College London. Hon Consultant Chelsea and Westminster Hospital NHS Foundation Trust. ASCR undertakes consultancy and advisory board work for Imperial College Consultants- in the last 36 months this has included remunerated work for: Confo, Combigene, Vertex, Novartis, Orion, Shanghai SIMR Biotech & Science Practice (Wellcome Trust). ASCR is named as an inventor on patents: Rice A.S.C., Vandevoorde S. and Lambert D.M Methods using N-(2-propenyl)hexadecanamide and related amides to relieve pain. WO 2005/079771. Okuse K. et al. Methods of treating pain by inhibition of vgf activity EP13702262.0/ WO2013 110945. Member Joint Committee on Vaccine and Immunisation- varicella sub-committee. Analgesic Clinical Trial Translation: Innovations, Opportunities, and Networks (ACTTION) steering committee member. Medicines and Healthcare products Regulatory Agency (MHRA), Commission on Human Medicines—Neurology, Pain & Psychiatry Expert Advisory Group. Grants and studentships—UKRI (Medical Research Council & BBSRC), Versus Arthritis, Alan and Sheila Diamond Trust, Royal British Legion, European Commission, Ministry of Defence, Dr Jennie Gwynn Bequests, The British Pain Society, Royal Society of Medicine. Royal College of Anaesthetists—Heritage and Archives Committee (2020—date). Lecture honoraria: MD Cancer Cancer Center -2021, University California San Francisco. CSF12th Pediatric Pain Master Class (USA) Dec 2021, Bioevents – Controversies in Neuropathic pain – 2021, Royal Marsden Hospital 2019, Indonesian Neurological Association Pain Study Group International Lecture Series Donated to (Association of Southeast Asian Pain Societies (ASEAPS) –Oct 2022, Malaysian Society of Anaesthesiologists – July 2022, Siriraj Hospital Bangkok international relations programme- visiting Professorship Nov 2022 – used for expenses. Royal Pharmaceutical Society- British National Formulary- ongoing. International Association Study of Pain: Executive Committee (President-elect). David L Bennett (DLB) was a Principal Investigator/director of the Wellcome Trust funded London Pain Consortium through which the PiNS study was funded. DLB declares the following interests unrelated to this manuscript occurring in last 36 months: DLB is a member of the NeupSIG executive committee. DLB has received grant funding from UKRI, Lilly, AstraZeneca, Wellcome, EU and Diabetes UK. DLB has acted as a consultant in the last 2 years for AditumBio, Amgen, Biointervene, Bristows, LatigoBio, GSK, Ionis, Lexicon therapeutics, Lilly, Neuvati, Olipass, Regeneron, Replay and Theranexus on behalf of Oxford University Innovation. DLB has been named on a patent ‘a method for the treatment or prevention of pain, or excessive neuronal activity, or epilepsy’ Application No. 16/337,428. Solomon Tesfaye has received: honoraria from Procter & Gamble, Viatris, Grunenthal, Novo Nordisk, Pfizer, Merck, Eva Pharma, Hikma, Astellas Pharma, Abbott, AstraZeneca, Berlin-Chemie, Worwag Pharma, Nevro, Haisco Pharmaceutical Group, for educational meetings; consultancy fees for advisor board membership from Angelini, Bayer, GSK, Worwag Phrama and Nevro; research equipment donated to Sheffield Teaching Hospitals from Impeto Medical and Neurometrix; and unrestricted, competitive research grants from Viatris and Procter and Gamble.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bäckryd, E., Themistocleous, A., Larsson, A. et al. Eleven neurology-related proteins measured in serum are positively correlated to the severity of diabetic neuropathy. Sci Rep 14, 17068 (2024). https://doi.org/10.1038/s41598-024-66471-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-66471-6
- Springer Nature Limited