Abstract
The clinical impact of soluble molecules in pleural effusion (PE) is unclear in patients with malignant pleural mesothelioma (MPM). In this single-center, retrospective, observational study, we assessed soluble forms of cytotoxic T-lymphocyte-associated protein 4 (CTLA-4), programmed cell death protein 1 (PD-1), and PD-1 ligand 1 (PD-L1) using enzyme-linked immunosorbent assays; three TGF-β isoforms were measured via multiplex assay in PE of patients with fibrinous pleuritis (FP) or MPM, to assess relationships between the levels of six molecules, clinicopathological characteristics, and efficacy of immune checkpoint inhibitors. Soluble forms of CTLA-4, PD-L1, PD-1, TGF-β1, TGF-β2, and TGF-β3 were variably produced in PE of FP (n = 34) and MPM (n = 79); we found significant relationships between the six molecules and clinicopathological features. Although none of the three soluble immune checkpoint molecules showed diagnostic or prognostic effects in patients with MPM, TGF-β2 level in PE is a useful differential diagnostic marker between FP and MPM. Both TGF-β1 and TGF-β3 levels are promising prognostic markers for MPM. Moreover, we found that higher baseline levels of PD-1 soluble forms predicted the response to anti-PD1 monotherapy. Our findings identify novel diagnostic, prognostic, and predictive biomarkers for anti-PD1 therapy in patients with MPM.
Similar content being viewed by others
Introduction
Malignant pleural mesothelioma (MPM) is an aggressive solid tumor whose onset is strongly associated with asbestos exposure-induced chronic inflammation1. Recently, immune checkpoint inhibitors (ICIs) targeting programmed cell death protein 1 (PD-1)/PD-1 ligand-1 (PD-L1) axis and cytotoxic T-lymphocyte-associated protein 4 (CTLA-4) have shown improved clinical outcomes in patients with MPM2, indicating that immune escape from host immunity is a primary mechanism of MPM tumor progression. Clinical studies revealed that PD-L1-overexpressed tumors showed better clinical responses compared to PD-L1 low-expressing tumors in several malignancy types3,4, suggesting that PD-L1 overexpression in tumor tissues is a potential biomarker for ICI targeting PD-1/PD-L1; however, an objective response was seen in both PD-L1 negative and positive MPM2, implying that the MPM tumor immune escape mechanism is complicated. Other than PD-L1 expression, meta-analytical studies have explored predictive factors for ICI; notably, the development of immune-related adverse events was associated with a durable response and survival benefit in patients with solid malignancies5. Furthermore, pretreatment hematological markers such as a lower neutrophil-to-lymphocyte ratio or higher albumin levels also predicted a better clinical outcome6,7. Importantly, clinical benefits were similarly observed between cases with Eastern Cooperative Oncology Group performance status 0 and 18. Currently, none of these factors can be used in the decision-making process with ICI.
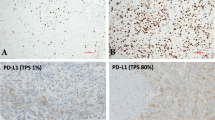
The tumor immune microenvironment (TIME), consisting of tumor, immune, vascular, and stromal cells, is important for facilitating the tumor cell escape from anti-tumor immunity via immune suppressive molecules such as immune checkpoint molecules (ICMs) and immune suppressive cytokines9. The TIME is an important topic for cancer research because other than the PD-L1 status, TIME can predict ICI efficacy in melanoma10. Although studying TIME of MPM is difficult because of its rarity, several studies have shown that PD-L1 overexpression in tumor tissue using immunohistochemical staining (IHC) predicts poor prognosis11,12, whereas many other studies could not show any impact of PD-L1 status on the prognosis of patients with MPM13,14.
In many cases, MPM is accompanied by pleural effusion (PE), which could also be considered as a TIME. To date, only a single assessment of the soluble form of CTLA-4 (sCTLA-4) or PD-L1 (sPD-L1) has been conducted in the PE of MPM15,16, and the simultaneous evaluation of multiplex soluble ICMs has not been reported. Transforming growth factor (TGF)-β is rich in MPM17,18, and drives epithelial-mesenchymal transition (EMT) and inactivates anti-cancer immunity, making its involvement in PE worth investigating19,20. TGF-β has three isoforms; TGF-β1, TGF-β2, and TGF-β321. Only one report has evaluated TGF-β levels in PE, wherein more than 10 cases of MPM were investigated18; however, levels of the three TGF-β isoforms in PE of MPM have not been reported.
Here, we first evaluate concentrations of multiplex soluble ICMs: sCTLA-4, sPD-L1, and PD-1 soluble form (sPD-1), and three TGF-β isoforms in PE of fibrinous pleuritis (FP) or MPM. TGF-β2 was higher in PE of MPM than in PE of FP, suggesting that TGF-β2 levels in PE could be a useful tool for differential diagnosis between MPM and FP. The three soluble ICMs did not show any prognostic impact, whereas higher concentrations of both TGF-β1 and TGF-β3 predicted poor overall survival (OS) in patients with MPM. Moreover, we found that a higher baseline level of sPD-1 in PE predicted the response to anti-PD-1 monotherapy in patients with MPM.
Materials and methods
Patients
This was a single-center, retrospective, observational study. PE samples were collected for cytology and/or biochemistry tests from patients with FP or MPM prior to treatment, except for three patients with postoperative recurrence for whom extrapleural pneumonectomy with or without perioperative chemotherapy was performed, between February 2007 and July 2022. The residual PE samples were centrifuged at 800 × g at 4 °C for 10 min and the supernatants were frozen at − 80 °C until analysis. All cases were histologically diagnosed as FP or MPM by experienced pathologists using IHC. The 5-year OS was estimated from the date of PE collection to death from any cause or the last follow-up. The requirement of written informed consent for using medical records, tissue samples, and PE samples was waived, and the opt-out method on the website was used to obtain patient consent. This observational study adhered to the principles of the Declaration of Helsinki and complied with relevant guidelines and regulations, and it was approved by the Yamaguchi Ube Medical Center Ethics Committee (No. 28-13, 30-5, and 2020-17).
Clinical variables
The following patient characteristics were obtained from medical records for analysis: age, sex, histological subtype, clinical stage (cStage), and treatment (surgery, radiotherapy, chemotherapy, and ICIs). The follow-up period was set at a maximum of five years (60 months). Histological subtype and cStage were determined according to the criteria from the World Health Organization 201522 and the eighth edition of the TNM stage classification system23,24,25, respectively. The last follow-up date was August 31, 2023, and the median length of follow-up for censored cases was 13.4 months (range, 4.7–33.4 months).
BAP1 status and tumor infiltrating CD8 T cell (TIL) using IHC
Formalin-fixed and paraffin-embedded blocks of MPM were obtained from the institution archives. IHC for BRCA1 associated protein 1 (BAP1) was performed on surgically removed tissues using an automated immunostainer (Ventana BenchMark GX; Roche Diagnostics, Basel, Switzerland). Briefly, slides were deparaffinized using the EZ buffer (Roche Diagnostics) for 1 min at 75 °C and antigen was retrieved using Cell Conditioning 1 buffer (Roche Diagnostics) at 100 °C for 60 min. In addition, a mouse monoclonal anti-BAP1 antibody (1:50, clone C-4, Santa Cruz Biotechnology, Dallas, TX) was used as the primary antibody at 37 °C for 32 min, followed by secondary antibody and detection using the Ventana UltraView Universal DAB detection kit (Roche Diagnostics) as per manufacturer’s instructions. Loss of BAP1 was defined as the absence of BAP1 staining in the MPM cell nuclei. Immunoreactivity for BAP1 (loss or retention) was assessed by experienced pathologists (T.M. or E.I.). Nucleus staining for BAP1 in lymphocytes and vascular endothelial cells was used as an internal positive control for BAP1 expression. IHC for CD8 TIL was performed as double staining with rabbit anti-CD8α IgG antibody (clone D8A8Y, Cell Signaling Technology, Danvers, MA) and mouse anti-EGFR IgG2a antibody (clone A-10, Santa Cruz Biotechnology); the status of CD8 TIL was judged by two scorers (R.O. and T.S.) following previously described protocol14.
ELISA
The levels of sCTLA-4, sPD-L1, and sPD-1 in PE were measured using enzyme-linked immunosorbent assays (ELISA) using a Human CTLA-4 Quantikine HS ELISA kit (#HSCT40, R&D Systems, Minneapolis, MN), Human/Cynomolgus Monkey B7-H1/PD-L1 Quantikine ELISA kit (#DB7H10, R&D Systems), and Human PD-1 Quantikine HS ELISA kit (#DPD10, R&D Systems), respectively, as per manufacturer’s instructions. The minimum detectable doses of sCTLA-4, sPD-L1, and sPD-1 were 0.13, 4.52, and 3.27 pg/ml, respectively. The plates were read at 450 nm using a Multiskan FC (Thermo Fisher Scientific, Waltham, MA).
Multiplex cytokine detecting assay
TGF-β1,2,3 levels in PE were measured via multiplex assay using Bio-Plex Pro Human TGF-β 3-plex panel (#171W4001M, Bio-Rad, Hercules, CA), as per manufacturer’s instructions. The minimum detectable doses of TGF-β1, TGF-β2, and TGF-β3 were 3.9, 1.9, and 0.5 pg/ml, respectively. Plates were read using a Bio-Plex 200 system (Bio-Rad).
Statistical analysis
The cutoff values of each parameter were individually determined according to the receiver operating characteristic (ROC) curves for differential diagnosis between FP and MPM or for predicting 2-year survival or response to ICI in cases of MPM. A t-test was performed to compare the levels of the six PE parameters between the FP and MPM groups or the historical subtypes of MPM. A chi-square test was performed to evaluate the relationship between patient characteristics and TIME parameters. Spearman’s rank correlation test was performed for correlation analysis between the levels of the six PE parameters. Kaplan–Meier survival analysis was used to determine the association between the status of each parameter and the 5-year OS until death or last follow-up. The significant differences in the 5-year OS between groups were assessed using the log-rank test. Statistical analyses were performed using GraphPad Prism 6.01 (GraphPad Software, La Jolla, CA). Univariate and multivariate analyses were performed with the Cox proportional hazards model to identify independent prognostic factors using the SPSS statistical package (version 17.0; SPSS, Chicago, IL). In all cases, statistical significance was set at p < 0.05.
Ethics approval and consent to participate
This research was approved by the Yamaguchi Ube Medical Center Ethics Committee (No. 28-13, 30-5 and 2020-17), followed the principles of the Declaration of Helsinki, and complied with the relevant guidelines and regulations. The requirement for written informed consent for the use of medical records was waived and an opt-out method on the website was used to obtain patient consent.
Results
Patient cohort
Overall, 113 patients were enrolled and our cohort comprised 34 and 79 patients with FP and MPM, respectively. A definitive pathological diagnosis was performed via pleural biopsy in all patients with MPM at our hospital (72) or elsewhere (7). Patient backgrounds are shown in Table 1.
Levels of three soluble ICMs and TGF-β 1,2,3 in PE of FP or MPM
The mean (± standard deviation) concentrations of the three soluble ICM (sCLTA-4, sPD-L1, and sPD-1) and three TGF-β (TGF-β1, TGF-β2, and TGF-β3) isoforms in PE of FP were 13.64 ± 17.46, 173.0 ± 74.50, 1040 ± 966.2, 9277 ± 5709, 159.0 ± 69.53, and 33.30 ± 21.16 pg/ml, whereas those in PE of MPM were 15.51 ± 18.91, 269.4 ± 324.5, 1163 ± 1978, 11,465 ± 10,967, 545.8 ± 858.1, and 39.78 ± 32.55 pg/ml, respectively. TGF-β2 was significantly higher in PE of MPM than in PE of FP (p = 0.011). The sPD-L1 level in PE of MPM tended to be higher than that in PE of FP, although the difference was not significant (p = 0.090). No difference was observed between FP and MPM in the other four parameters (Fig. 1a and Supplementary Table S1). Optimal cutoff values for differential diagnosis between FP and MPM were determined via ROC analyses as follows: 9.19 pg/ml for sCTLA-4, 163.46 pg/ml for sPD-L1, 581.15 pg/ml for sPD-1, 8413.45 pg/ml for TGF-β1, 177.99 pg/ml for TGF-β2, and 28.56 pg/ml for TGF-β3. The higher TGF-β2 level was a significant diagnostic parameter for MPM (p = 0.0004), whereas the other five parameters were not significant (Supplementary Fig. S1).
Levels of six parameters in PE of patients with FP or MPM. (a) Each dot represents the levels of sCTLA4, sPD-L1, sPD-1, TGF-β1, TGF-β2, and TGF-β3 in the PE of FP or MPM, (b) in the PE of epithelioid, biphasic, or sarcomatoid MPM, and (c) in the PE of FP, epithelioid, or non-epithelioid (biphasic and sarcomatoid) MPM. Data were analyzed using a t-test. Bars: Mean ± SD. *p < 0.05, **p < 0.001. PE pleural effusion, FP fibrinous pleuritic, MPM malignant pleural mesothelioma, sCTLA-4 soluble CTLA-4, sPD-L1 soluble PD-L1, sPD-1 soluble PD1, Epi. epithelioid MPM, Bi. biphasic MPM, Sar. sarcomatoid MPM, SD standard deviation, n.s. not significant.
The six parameters in each MPM histology type were analyzed. The sPD-L1 level in PE of sarcomatoid MPM was significantly higher (565.4 ± 805.6 pg/ml) than that in PE of epithelioid MPM (232.8 ± 247.8 pg/ml, p = 0.027) and higher, although not significantly, than that in PE of biphasic MPM (255.4 ± 184.3 pg/ml, p = 0.077). TGF-β1 in PE of sarcomatoid MPM (26,084 ± 20,975 pg/ml) was higher than that in PE of epithelioid MPM (8649 ± 8929 pg/ml, p = 0.0003) or biphasic MPM (12,667 ± 6978 pg/ml, p = 0.009) (Fig. 1b). When comparing levels of the six parameters between epithelioid and non-epithelioid (biphasic + sarcomatoid) MPM, significant differences were observed in sPD-L1 levels between FP and non-epithelioid MPM (323.2 ± 410.9 pg/ml, p = 0.040), TGF-β1 levels between non-epithelioid MPM (15,602 ± 12,434 pg/ml) and FP (p = 0.010) or epithelioid MPM (p = 0.005), and TGF-β2 levels between FP and epithelioid MPM (472.2 ± 802.8 pg/ml, p = 0.029) or non-epithelioid MPM (657.4 ± 938.2 pg/ml, p = 0.003) (Fig. 1c).
Correlations between the six PE parameters in patients with MPM
Correlations between each soluble ICM and TGF-β1,2,3 were assessed. Significant positive correlations were observed between sCTLA-4 and sPD-L1 [Spearman’s rank correlation coefficient (Rs): 0.207, p < 0.0001], sCTLA-4 and sPD-1 (Rs: 0.755, p < 0.0001), sPD-L1 and sPD-1 (Rs: 0.125, p = 0.001), sPD-L1 and TGF-β1 (Rs: 0.053, p = 0.040), TGF-β1 and TGF-β3 (Rs: 0.190, p < 0.0001), and TGF-β2 and TGF-β3 (Rs: 0.193, p < 0.0001) (Supplementary Fig. S2) levels. The correlation between sCTLA-4 and sPD-1 was strong, whereas that between sCTLA-4 and sPD-L1 was moderate; correlations between sPD-L1 and sPD-1, sPD-L1 and TGF-β1, TGF-β1 and TGF-β3, and TGF-β2 and TGF-β3 were weak.
Relationships between the six PE parameters and BAP1 and CD8 TIL statuses in MPM
Proteomic data from MPM showed that BAP1-deficient tumors were characterized by inflammatory TIME and activation of immune checkpoint mechanisms26. Therefore, the relationship between the six PE parameters and the statuses of BAP1 and CD8 TIL in MPM was analyzed. Tissue blocks from 72 patients with MPM were obtained from the institution archives, whereas blocks from the other seven cases could not be assessed because the biopsy was performed outside our hospital. Representative images of BAP1 and CD8 + TILs are shown in Supplementary Figure S3. The BAP1 status was considered a “loss” in 46 cases and “retained” in 26 cases of MPM, whereas the CD8 TILs were negative in 36 cases and positive in 36 cases of MPM. TGF-β1 in PE of MPM was significantly lower in cases with BAP1 loss tumors (9218 ± 6776 pg/ml) than in cases with BAP1-retained tumors (15,474 ± 15,944 pg/ml, p = 0.023). The sPD-L1 level in PE of MPM was lower in BAP1 loss tumors (208.0 ± 167.4 pg/ml) than in BAP1-retained tumors (338.7 ± 457.4 pg/ml, p = 0.085), although the difference was not significant (Supplementary Fig. S4a). The sCTLA-4 level in PE of MPM was lower in cases without CD8 TILs (10.41 ± 8.390 pg/ml) than in those with CD8 TILs (19.70 ± 25.35 pg/ml. p = 0.041), whereas TGF-β1 in PE of MPM was higher in cases without CD8 TILs (14,105 ± 14,598 pg/ml) than in those with CD8 TILs (8849 ± 5646 pg/ml, p = 0.048) (Supplementary Fig. S4b).
OS stratified by the six PE parameters, BAP1, and CD8 TIL in MPM
Optimal cutoff values for each parameter in predicting 2-year survival determined using ROC analyses were as follows: 9.56 pg/ml for sCTLA-4, 165.73 pg/ml for sPD-L1, 601.50 pg/ml for sPD-1, 8100.75 pg/ml for TGF-β1, 198.28 pg/ml for TGF-β2, and 28.56 pg/ml for TGF-β3. Both TGF-β1 (p = 0.008) and TGF-β3 (p = 0.004) significantly predicted the 2-year survival in patients with MPM, whereas the other four PE parameters did not (Supplementary Fig. S5). Kaplan–Meier survival analysis demonstrated that higher TGF-β1 (p < 0.0001) and TGF-β3 (p = 0.028) levels were associated with poorer OS than were lower levels of these molecules, whereas none of the other four PE parameters and statuses of BAP1 and CD8 TIL showed any impact on the 5-year OS (Fig. 2).
Associations of the six parameters and BAP1 and CD8 TIL statuses in PE with 5-year overall survival in patients with MPM. Kaplan–Meier plots showing 5-year overall survival in patients with low or high sCTLA-4 (cutoff: 9.555 pg/ml), sPD-L1 (cutoff: 165.73 pg/ml), sPD-1 (cutoff: 601.5 pg/ml), TGF-β1 (cutoff: 8100.75 pg/ml), TGF-β2 (cutoff: 198.275 pg/ml), and TGF-β3 (cutoff: 28.555 pg/ml) levels in PE; loss or retention of BAP1 and negative or positive for CD8 TIL in tumor tissues of patients with MPM. HR hazard ratio, CI 98% confidence interval, PE pleural effusion. *p < 0.05, **p < 0.001.
Relationship between statuses of the six PE parameters and patient characteristics in MPM
If the six PE parameters were divided as low or high levels following cutoff values for 2-year survival via the ROC curve, significant relationships were observed between statuses of sCTLA-4 and sPD-L1 (p < 0.001), sCTLA-4 and sPD-1 (p < 0.001), sCTLA-4 and TGF-β1 (p = 0.032), sPD-L1 and histology (p = 0.035), sPD-L1 and sPD-1 (p < 0.001), sPD-L1 and TGF-β1 (p = 0.010), sPD-1 and TGF-β1 (p = 0.010), TGF-β1 and histology (p < 0.001), TGF-β1 and TGF-β2 (p = 0.001), TGF-β1 and TGF-β3 (p < 0.001), and TGF-β2 and histology (p = 0.014), respectively (Supplementary Table S2).
Univariate or multivariate analysis of the six PE parameters for 5-year OS
Cox regression analysis was performed to determine the predictive value of clinical variables for the 5-year OS. Prognostic impacts of the three soluble ICMs and three TGF-β isoforms in PE of MPM were assessed independently via univariate and multivariate analyses, with the ICMs and isoforms as confounding factors. The parameter number was set to six, as the multivariate analysis for soluble ICM and TGF-β cohorts included 72 cases with 61 events and 70 cases with 60 events, respectively. The other five parameters were sex27, histological subtype27,28, and TNM Stage25, which were broadly recognized as prognostic factors for MPM, including BAP1 and CD8 TIL statuses. In comparison, both BAP1 and CD8 TIL statuses were undecidable in seven cases, as biopsy was performed outside our hospital, and the TGF-β2 or TGF-β3 levels in PE were undetected in the other two cases. Univariate analysis of the soluble ICM cohort showed that histological subtype, cStage, and BAP1 status were significantly associated with 5-year OS, and multivariate analysis showed that histology and cStage were independent poor prognostic factors for 5-year OS in soluble ICM cohorts, whereas none of the soluble ICMs had any impact on 5-year OS (Supplemental Table S3). Conversely, univariate analysis for the TGF-β cohort showed histological subtype, cStage, BAP1 status, TGF-β1, and TGF-β3 to be significantly associated with 5-year OS, and multivariate analysis showed that histology and cStage were independent poor prognostic factors for 5-year OS in TGF-β cohort; both TGF-β1 and TGF-β3 were also significantly associated with 5-year OS, while TGF-β2 did not affect OS (Table 2).
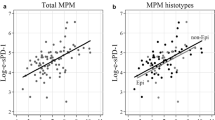
Relationships between statuses of six PE parameters and ICI efficacy in patients with MPM
We determined the predictive impact of these six parameters on ICI efficacy in patients with MPM. In our cohort, seven patients received anti-PD-1 monotherapy, two patients were administered a combination of anti-PD-1 and -CTLA4 therapies, and one patient was treated with a combination of anti-PD-1 therapy and cytotoxic chemotherapy for MPM. The six PE parameters were divided into low or high levels using the ROC curve following the cutoff values for response to anti-PD-1 monotherapy: responder (partial response or stable disease for > 6 months) or non-responder (progressive disease or stable disease for < 6 months) as per modified RECIST criteria29 (Supplementary Fig. S6). We found that higher sPD-1 in PE was significantly associated with responders in patients treated with anti-PD-1 monotherapy via chi-squared test, although no significant relationship was observed between the other five PE parameters and response to anti-PD-1 monotherapy or all six PE parameters and response to patients treated with ICI (Table 3).
Discussion
PE, which could reflect the TIME of MPM, is easy to collect under local anesthesia. The most popular diagnostic marker for PE in MPM is hyaluronic acid; however, its accuracy is insufficient to provide a definitive diagnosis. To assess diagnostic markers of MPM in PE, we simultaneously assessed three ICMs and three TGF-β isoforms in PE from FP and MPM. We found that PE in MPM had higher TGF-β2, suggesting it is a diagnostic biomarker to distinguish between FP and MPM.
A detailed understanding of the TIME in PE of MPM is important. Positive correlations were observed between levels of sCTLA-4 and sPD-L1, sCTLA-4 and sPD-1, and sPD-L1 and sPD-1 in PE of MPM. The Rs was particularly high for the relationship between sCTLA4 and sPD-1. Both CTLA-4 and PD-1 are expressed in exhausted T cells, suggesting that soluble ICMs originate from tumor-infiltrating exhausted T cells. These findings suggest that not only single ICM but multiplex ICMs help tumors to escape host immunity, which is a potential reason for the limited efficacy of ICI therapy in patients with MPM. We assessed only three soluble ICMs; however, the three soluble ICM levels positively correlated with each other, suggesting unexamined ICMs may also be rich in the PE of MPM. If CD8 + TILs are exhausted with higher multiplex soluble forms of ICM in the PE of MPM, ICI monotherapy-mediated activation of antitumor immunity may be difficult with high probability. We found that sCTLA-4 was higher in cases with CD8 + TIL than in those without CD8 + TIL, supporting the hypothesis that CD8 + TILs in the TIME of MPM were exhausted.
We assessed the relationship between clinicopathological features and six parameters in the PE of patients with MPM. We found that BAP1 status was significantly associated with TGF-β1 levels in PE of MPM and was associated with sPD-L1 via t-test, although not significantly. BAP1 is not only a tumor suppressor gene30 but also a regulator of proteins involved in DNA damage repair, cell differentiation, cell proliferation, and immune response31,32. BAP1 loss reflects BAP1 mutation33. Proteomic data from malignant peritoneal mesothelioma showed BAP1-deficient tumors characterized by an inflammatory TIME and immune checkpoint activation26. In PE of MPM with BAP1 loss, sPD-L1 was slightly lower than that in PE of MPM with BAP1 expression, suggesting that BAP1 function loss because of gene mutation directly decreased sPD-L1 secreting or indirectly inhibited membrane binding PD-L1 shedding in PE. TGF-β1 levels in PE were significantly lower in MPM with BAP1 loss than in MPM with BAP1 expression. This indicates that BAP1 function loss inhibits TGF-β1 secretion in PE, thus implying that BAP1 alterations affect the EMT and tumor immunoescape34, although its clinical significance remains unknown. Another potential reason for the observed significant difference in TGF-β1 levels between cases with BAP1 loss and retention might be that it is independent of BAP1 function but rather reflects variations in histological subtypes. Notably, BAP1 loss is strongly associated with the epithelioid subtype of MPM, which is significantly correlated with lower TGF-β1 levels. We also found that TGF-β1 in PE was higher in cases without CD8 TIL than in those with CD8 TIL. TGF-β1 is an immune suppressor that causes CD8 T cell exclusion from tumors in TIME35. The effects of BAP1 loss on EMT and tumor immune escape should be further investigated.
The potential of the six PE parameters in predicting MPM prognosis is worth considering. Although none of the three ICMs affected prognosis in patients with MPM, high TGF-β1 and TGF-β3 levels predicted poor prognoses. Our findings suggest that TGF-β may represent a promising target for MPM treatment, as it appears to fulfill dual roles in EMT and immune suppression19,20, which contribute to the worsening of MPM prognoses. Functional differences among three TGF-β isoforms should be investigated. TGF-β1 knockout mice develop a spontaneous fatal inflammatory syndrome until 3–4 weeks of age36, whereas both TGF-β2 and TGF-β3 knockout mice die as fetuses. TGF-β2 knockout mice showed developmental defects in multiple organs including cardiovascular, respiratory, and skeletal organs36, whereas TGF-β3 knockout mice exhibited retarded growth in lungs with normal cardiovascular development37. Theoretically, TGF-β is a promising target for anti-cancer therapy; however, the pan-TGF-β inhibitor has not been used clinically because of cardiotoxicity in animal models38. We showed that the three TGF-β isoforms indicated different consequences in MPM; a selective inhibition strategy for one or two of the three TGF-β isoforms may be feasible for MPM treatment. An antisense oligonucleotide targeting TGF-β2 inhibits lung metastasis in a preclinical in vivo mouse model39, which supports this strategy. The relationship between the six PE parameters and ICI efficacy in patients with MPM was of interest. Although our findings support that a higher baseline status of sPD-1 in PE predicts the response to anti-PD-1 monotherapy in patients with MPM, these findings should be interpreted with caution because of the small sample size. Therefore, further re-evaluation is warranted after accumulating a larger number of cases.
Our study has several strengths. First, this is the first study to evaluate the multiplex soluble forms of ICM and three TGF-β isoforms in PE of MPM simultaneously. Second, to the best of our knowledge, this is the largest study to evaluate sCTLA4, sPD-L1, sPD-1, and TGF-β in PE of MPM. PE sampling can be performed under local anesthesia without hospitalization and provides rapid results compared to pleural biopsy. This method may facilitate earlier diagnosis and prognosis prediction in patients with MPM. However, this study has some limitations. First, the sample size was small compared with that in similar studies on common cancer types; however, obtaining data for many patients with MPM was difficult because of its rarity. Another limitation of our study was the assessment of only six PE molecules despite the presence of numerous soluble factors in PE. Future studies should consider comprehensive PE analysis to identify diagnostic, prognostic, and predictive markers.
In conclusion, we found positive correlations among all combinations of the three soluble ICMs. In addition, positivity for CD8 + TIL in the tumor tissue was associated with higher levels of sCTLA-4 in the PE of MPM. Although none of the three soluble forms of ICMs showed a prognostic impact in patients with MPM, the baseline sPD-1 levels in PE predicted the response to anti-PD-1 monotherapy. Conversely, TGF-β2 in PE is a differential diagnostic marker between FP and MPM, and TGF-β1 and TGF-β3 levels are promising prognostic biomarkers for MPM.
Data availability
The datasets used and/or analyzed in the current study are available from the corresponding author upon reasonable request.
Abbreviations
- BAP1:
-
BRCA1 associated protein 1
- CD8 TIL:
-
Tumor infiltrating CD8 T cell
- cStage:
-
Clinical stage
- CTLA-4:
-
Cytotoxic T-lymphocyte-associated protein 4
- ELISA:
-
Enzyme-linked immunosorbent assay
- EMT:
-
Epithelial-mesenchymal transition
- FP:
-
Fibrinous pleuritis
- ICI:
-
Immune checkpoint inhibitor
- ICM:
-
Immune checkpoint molecule
- IHC:
-
Immunohistochemistry
- MPM:
-
Malignant pleural mesothelioma
- OS:
-
Overall survival
- PD1:
-
Programmed cell death protein 1
- PD-L1:
-
Programmed cell death protein 1 ligand-1
- PE:
-
Pleural effusion
- ROC:
-
Receiver operating characteristic
- Rs:
-
Spearman’s rank correlation coefficient
- sCTLA-4:
-
Soluble form of cytotoxic T-lymphocyte-associated protein 4
- sPD-1:
-
Soluble form of programmed cell death protein 1
- sPD-L1:
-
Soluble form of programmed cell death protein 1 ligand-1
- TGF-β:
-
Transforming growth factor-β
- TIME:
-
Tumor immune microenvironment
References
Pinato, D. J. et al. Inflammation-based prognostic indices in malignant pleural mesothelioma. J. Thorac. Oncol. 7, 587–594. https://doi.org/10.1097/JTO.0b013e31823f45c1 (2012).
Baas, P. et al. First-line nivolumab plus ipilimumab in unresectable malignant pleural mesothelioma (CheckMate 743): A multicentre, randomised, open-label, phase 3 trial. Lancet 397, 375–386. https://doi.org/10.1016/S0140-6736(20)32714-8 (2021).
Topalian, S. L. et al. Safety, activity, and immune correlates of anti-PD-1 antibody in cancer. N. Engl. J. Med. 366, 2443–2454. https://doi.org/10.1056/NEJMoa1200690 (2012).
Borghaei, H. et al. Nivolumab versus docetaxel in Advanced nonsquamous non-small-Cell Lung Cancer. N. Engl. J. Med. 373, 1627–1639. https://doi.org/10.1056/NEJMoa1507643 (2015).
Dall’Olio, F. G. et al. Immortal time bias in the association between toxicity and response for immune checkpoint inhibitors: A meta-analysis. Immunotherapy 13, 257–270. https://doi.org/10.2217/imt-2020-0179 (2021).
Tan, Q., Liu, S., Liang, C., Han, X. & Shi, Y. Pretreatment hematological markers predict clinical outcome in cancer patients receiving immune checkpoint inhibitors: A meta-analysis. Thorac. Cancer 9, 1220–1230. https://doi.org/10.1111/1759-7714.12815 (2018).
Guven, D. C. et al. The association between albumin levels and survival in patients treated with immune checkpoint inhibitors: A systematic review and meta-analysis. Front. Mol. Biosci. 9, 1039121. https://doi.org/10.3389/fmolb.2022.1039121 (2022).
Mollica, V. et al. The impact of ECOG performance status on efficacy of immunotherapy and immune-based combinations in cancer patients: The MOUSEION-06 study. Clin. Exp. Med. 23, 5039–5049. https://doi.org/10.1007/s10238-023-01159-1 (2023).
Binnewies, M. et al. Understanding the tumor immune microenvironment (TIME) for effective therapy. Nat. Med. 24, 541–550. https://doi.org/10.1038/s41591-018-0014-x (2018).
Tumeh, P. C. et al. PD-1 blockade induces responses by inhibiting adaptive immune resistance. Nature 515, 568–571. https://doi.org/10.1038/nature13954 (2014).
Cedrés, S. et al. Analysis of expression of programmed cell death 1 ligand 1 (PD-L1) in malignant pleural mesothelioma (MPM). PLoS ONE. 10, e0121071. https://doi.org/10.1371/journal.pone.0121071 (2015).
Kao, S. C. et al. Tumor suppressor microRNAs contribute to the regulation of PD-L1 expression in malignant pleural mesothelioma. J. Thorac. Oncol. 12, 1421–1433. https://doi.org/10.1016/j.jtho.2017.05.024 (2017).
Sobhani, N. et al. Tumour infiltrating lymphocytes and PD-L1 expression as potential predictors of outcome in patients with malignant pleural mesothelioma. Mol. Biol. Rep. 46, 2713–2720. https://doi.org/10.1007/s11033-019-04715-9 (2019).
Okita, R. et al. Effects of tumor-infiltrating CD8+ T cells, PD1/PD-L1 axis, and expression patterns of HLA class I on the prognosis of patients with malignant pleural mesothelioma who underwent extra-pleural pneumonectomy. Cancer Immunol. Immunother. 72, 865–879. https://doi.org/10.1007/s00262-022-03292-4 (2023).
Roncella, S. et al. CTLA-4 in mesothelioma patients: Tissue expression, body fluid levels and possible relevance as a prognostic factor. Cancer Immunol. Immunother. 65, 909–917. https://doi.org/10.1007/s00262-016-1844-3 (2016).
Carosio, R. et al. Characterization of soluble PD-L1 in pleural effusions of mesothelioma patients: Potential implications in the immune response and prognosis. J. Cancer Res. Clin. Oncol. 147, 459–468. https://doi.org/10.1007/s00432-020-03457-7 (2021).
Maeda, J. et al. Transforming growth factor-beta 1 (TGF-beta 1)- and beta 2-like activities in malignant pleural effusions caused by malignant mesothelioma or primary lung cancer. Clin. Exp. Immunol. 98, 319–322. https://doi.org/10.1111/j.1365-2249.1994.tb06144.x (1994).
Stockhammer, P. et al. Detection of TGF-beta in pleural effusions for diagnosis and prognostic stratification of malignant pleural mesothelioma. Lung Cancer 139, 124–132. https://doi.org/10.1016/j.lungcan.2019.11.013 (2020).
Bierie, B. & Moses, H. L. Tumour microenvironment: TGFbeta: The molecular Jekyll and Hyde of cancer. Nat. Rev. Cancer 6, 506–520. https://doi.org/10.1038/nrc1926 (2006).
Massagué, J. & Sheppard, D. TGF-beta signaling in health and disease. Cell. 186, 4007–4037. https://doi.org/10.1016/j.cell.2023.07.036 (2023).
Cheifetz, S. et al. Distinct transforming growth factor-beta (TGF-beta) receptor subsets as determinants of cellular responsiveness to three TGF-beta isoforms. J. Biol. Chem. 265, 20533–20538 (1990).
Travis, W. D., International Agency for Research on C. WHO Classification of Tumours of the Lung, Pleura, Thymus and Heart (International Agency for Research on Cancer, 2015).
Nowak, A. K. et al. The IASLC mesothelioma staging project: Proposals for revisions of the T descriptors in the forthcoming eighth edition of the TNM classification for pleural mesothelioma. J. Thorac. Oncol. 11, 2089–2099. https://doi.org/10.1016/j.jtho.2016.08.147 (2016).
Rice, D. et al. The IASLC Mesothelioma Staging Project: Proposals for revisions of the N descriptors in the forthcoming eighth edition of the TNM classification for pleural mesothelioma. J. Thorac. Oncol. 11, 2100–2111. https://doi.org/10.1016/j.jtho.2016.09.121 (2016).
Rusch, V. W. et al. The IASLC mesothelioma staging project: Proposals for the M descriptors and for revision of the TNM stage groupings in the forthcoming (eighth) edition of the TNM classification for mesothelioma. J. Thorac. Oncol. 11, 2112–2119. https://doi.org/10.1016/j.jtho.2016.09.124 (2016).
Shrestha, R. et al. BAP1 haploinsufficiency predicts a distinct immunogenic class of malignant peritoneal mesothelioma. Genome Med. 11, 8. https://doi.org/10.1186/s13073-019-0620-3 (2019).
Rusch, V. W. & Venkatraman, E. S. Important prognostic factors in patients with malignant pleural mesothelioma, managed surgically. Ann. Thorac. Surg. 68, 1799–1804. https://doi.org/10.1016/s0003-4975(99)01038-3 (1999).
Okada, M. et al. Radical surgery for malignant pleural mesothelioma: Results and prognosis. Interact. Cardiovasc. Thorac. Surg. 7, 102–106. https://doi.org/10.1510/icvts.2007.166322 (2008).
Byrne, M. J. & Nowak, A. K. Modified RECIST criteria for assessment of response in malignant pleural mesothelioma. Ann. Oncol. 15, 257–260. https://doi.org/10.1093/annonc/mdh059 (2004).
Jensen, D. E. et al. BAP1: A novel ubiquitin hydrolase which binds to the BRCA1 ring finger and enhances BRCA1-mediated cell growth suppression. Oncogene 16, 1097–1112. https://doi.org/10.1038/sj.onc.1201861 (1998).
Wang, A., Papneja, A., Hyrcza, M., Al-Habeeb, A. & Ghazarian, D. Gene of the month: BAP1. J. Clin. Pathol. 69, 750–753. https://doi.org/10.1136/jclinpath-2016-203866 (2016).
Louie, B. H. & Kurzrock, R. BAP1: Not just a BRCA1-associated protein. Cancer Treat. Rev. 90, 102091. https://doi.org/10.1016/j.ctrv.2020.102091 (2020).
Righi, L. et al. BRCA1-associated protein 1 (BAP1) immunohistochemical expression as a diagnostic tool in malignant pleural mesothelioma classification: A large retrospective study. J. Thorac. Oncol. 11, 2006–2017. https://doi.org/10.1016/j.jtho.2016.06.020 (2016).
Ladanyi, M., Sanchez Vega, F. & Zauderer, M. Loss of BAP1 as a candidate predictive biomarker for immunotherapy of mesothelioma. Genome Med. 11, 18. https://doi.org/10.1186/s13073-019-0631-0 (2019).
Mariathasan, S. et al. TGFbeta attenuates tumour response to PD-L1 blockade by contributing to exclusion of T cells. Nature 554, 544–548. https://doi.org/10.1038/nature25501 (2018).
Kulkarni, A. B. et al. Transforming growth factor beta 1 null mutation in mice causes excessive inflammatory response and early death. Proc. Natl. Acad. Sci. USA 90, 770–774. https://doi.org/10.1073/pnas.90.2.770 (1993).
Proetzel, G. et al. Transforming growth factor-beta 3 is required for secondary palate fusion. Nat. Genet. 11, 409–414. https://doi.org/10.1038/ng1295-409 (1995).
Mitra, M. S. et al. A potent pan-TGFbeta neutralizing monoclonal antibody elicits cardiovascular toxicity in mice and cynomolgus monkeys. Toxicol. Sci. 175, 24–34. https://doi.org/10.1093/toxsci/kfaa024 (2020).
Huber-Ruano, I. et al. An antisense oligonucleotide targeting TGF-beta2 inhibits lung metastasis and induces CD86 expression in tumor-associated macrophages. Ann. Oncol. 28, 2278–2285. https://doi.org/10.1093/annonc/mdx314 (2017).
Acknowledgements
The authors thank all physicians and medical staff who diagnosed and treated the patients. We are also extremely grateful to the Soujinkai Laboratory Center for the immunohistochemistry. We would like to thank Editage (www.editage.com) for editing the English language.
Funding
This work was supported by the Japan Society for the Promotion of Science (JSPS) Kakenhi Grant [grant number 22K08991]. The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
Riki Okita: Conceptualization, data curation, formal analysis, funding acquisition, investigation, methodology, project administration, resources, supervision, validation, visualization, writing–original draft, writing–review, and editing. Tomoya Senoo: Data curation, formal analysis, investigation, writing—review and editing. Yuka Mimura-Kimura: Investigation, methodology, validation, writing—review and editing. Yusuke Mimura: Investigation, methodology, resources, supervision, validation, writing—review and editing. Tomoyuki Murakami: Investigation, methodology, validation, writing—review and editing. Eiji Ikeda: Investigation, writing—review and editing. Masanori Okada: Resources, writing—review and editing. Hidetoshi Inokawa: Resources, writing—review and editing. Keisuke Aoe: Conceptualization, data curation, resources, supervision, writing, reviewing, and editing. All authors had full access to the study data and take responsibility for the integrity of the data and accuracy of the data analysis. All the authors have read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
Dr. Keisuke Aoe has received grants and personal fees from Ono Pharmaceutical, Bristol-Myers Squibb, and AstraZeneca, and grants from Eli Lilly, Novartis, MSD, Pfizer, and Sanofi. The remaining authors declare no conflict of interest. All the funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Okita, R., Senoo, T., Mimura-Kimura, Y. et al. Characterizing soluble immune checkpoint molecules and TGF-β1,2,3 in pleural effusion of malignant pleural mesothelioma. Sci Rep 14, 15947 (2024). https://doi.org/10.1038/s41598-024-66189-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-66189-5
- Springer Nature Limited