Abstract
This study was aimed to evaluate the impact of community pharmacy (CP)-based medication therapy management (MTM) program on clinical and humanistic outcomes in patients with uncontrolled diabetes. An open label, parallel-group randomised controlled trial was undertaken at a community pharmacy in Riyadh city, Kingdom of Saudi Arabia. Patients with a diagnosis of uncontrolled diabetes (HbA1c of ≥ 8%) meeting the eligibility criteria were randomised to receive either the MTM programme provided by pharmacists or standard care. The primary outcome was change in HbA1c over 6 months. Secondary outcomes included: changes in clinical parameters (blood pressure (BP), lipid profile, serum creatinine (SCr) and albumin-to- creatinine ratio (ACR)), types of drug-related problems (DRPs), health service utilization (HSU), adherence, diabetes distress and overall patient satisfaction with the service at 6-month. A sufficiently powered sample of 160 participants with a mean age was 50 years (SD ± 11.9) was recruited. The majority of the patients (68.1%) were male and had diabetes for more than eight years [IQR 3, 14]. After adjusting for baseline HbA1c, compared to the control group, the mean HbA1c level was 0.02% (p = 0.929) and 0.2% (p = 0.47) lower in the intervention arm at 3-month and 6-month respectively. However, these differences were not statistically significant. Nonetheless, within each arm, there was a significant improvement in HbA1c from baseline. Furthermore, the intervention arm demonstrated improvement in BP control (SBP lowered by 3.2 mmHg (p = 0.05) and DBP lowered by 3.8 mmHg (p = 0.008)). During the study period, none of the participants in the intervention group reported hospitalization or ER visits compared to 14 patients in the control group [OR 0.069 (95% CI 0.004, 1.3)]. Patient satisfaction as measured by Patient Satisfaction with Pharmacist Services Questionnaire 2.0 (PSPSQ 2.0) was significantly higher among MTM program participants compared to standard care (p = 0.00001). Patients in the MTM program were eight times more likely to be adherent compared to the patients in the standard care [OR 7.89 (95% CI 3.6, 17.4)]. MTM program metrics showed that per patient, the pharmacists spent a median of 35 [IQR 30, 44.5] minutes at the initial visit and 20 [IQR 10, 25] minutes during the 6-month visit. The number of DRPs had significantly dropped in the intervention arm at 3 and 6-month (p = 0.0001). In conclusion, CP-based MTM program can improve health outcomes and prevent hospitalisations in patients with diabetes. These findings support the implementation of CP-based MTM services for patients with diabetes in the Kingdom of Saudi Arabia.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Introduction
Community pharmacies (CPs) are one of the most accessible healthcare settings1. For example, in the UK, approximately 90% of the public live within 20-min walk of a community pharmacy (CP). These pharmacies are strategically distributed, often located in areas with higher levels of deprivation, ensuring that a large number of people have access to their services2,3,4. In the past decade, community pharmacists have emerged as a focal point for the modernization of primary and community healthcare services4. Literature demonstrates that expanding the roles of community pharmacists resulted in numerous patient-related benefits including improving the standard of care, optimising medicines use, reducing the workload of general practitioners (GPs), and lowering the cost of long-term healthcare, drug-related problems (DRPs) and hospital readmissions3,5,6.
Medication therapy management (MTM) is a patient-centered pharmaceutical care inspired cognitive service delivered by the pharmacist with the aim of optimizing therapeutic outcomes through efficient drug management7. It was officially recognized in the Medicare Prescription Drug, Improvement and Modernization Act (MMA) approved by the US Congress in 20038. MTM consists of five core elements7: medication therapy review (MTR), personal medication record (PMR), medication-related action plan (MAP), intervention and/or referral and documentation and follow-up. MTM was introduced as a program intervention for chronic disease patients, showing a significant improvement in clinical and healthcare utilisation outcomes9.
The practice of CP in Kingdom of Saudi Arabia (KSA) until now is primarily a commercial endeavour, with a focus on selling and dispensing of medications10. In line with the transformation agenda set under the umbrella of the Saudi Vision 2030, there has been great emphasis on shifting most pharmaceutical care services from inpatient to ambulatory care. This expanded role of ambulatory care (including community practice) is gaining traction and providing support for innovative pharmacy services3.
In parallel, the 2019 new regulatory changes have enabled community pharmacists in KSA to provide more direct patient care functions, thereby encouraging CP contributions to Saudi society's health and wellbeing and assisting them in taking on more responsibilities within the overall delivery of health care11,12,13. There have been some initiatives in delivering patient-oriented services14,15, however, such activities are still individualized and dispersed efforts4,16,17,18,19,20.
This study comes at a time when there is growing emphasis on improving the quality of healthcare delivery in the KSA. This paper describes the development, implementation, and evaluation of a community-pharmacy-based MTM program. The aim of this study was to assess the effectiveness of the CP-based MTM program, first of its kind in the KSA, compared with standard care in improving patient healthcare outcomes.
Method
Study protocol and registration
The trial protocol is available and has been published21 and registered on 09–12-2022 with the International Standard Randomised Controlled Trial Network (ISRCTN) (ISRCTN60703981, https://doi.org/10.1186/ISRCTN60703981 )22.
Ethical approval
This study obtained ethical approvals from the Ethical Review Boards at University of Birmingham (Approval # ERN_20-0768), Princess Nourah bent Abdulrahman University (Approval # 20–0240) and King Fahad Medical City (Approval # 20-388E). In addition, site owner (Innova Saudi Health Care Company) provided approval to participate in the study. All participants signed informed consent. This study was conducted in accordance with CONSORT guidelines23.
Study Design
This study is part of a large mixed-methods study with an embedded design, a randomised controlled study (RCT) embedded with qualitative interviews. The RCT study was set up as a randomised, 6-month, 2-arm, open-label, parallel-group, investigation. The two arms included an active arm where participants received the MTM program and a control arm where participants received standard care. The study was conducted between April 2021 and June 2022.
Setting
The research was carried out at a CP adjacent to a medical center in a neighbourhood just east of Riyadh City. The medical center has 19 out-patient clinics covering a wide range of specialties. It has its own laboratory services as well as an electronic health record system for patients for the purpose of brief documentation and billing. Within the pharmacy, a private room was set aside for the MTM program. A collaborative agreement was signed after introducing the project to the physicians at the center.
Patient recruitment
All eligible patients who visited the medical center during the study period were informed about the study by their physicians during patient consultations. Posters describing the service were displayed inside the clinics and in the lobby of medical center, as well as, the front of pharmacy counter. The patients were screened for eligibility by a research pharmacist (not involved in patient care) according to the following eligibility criteria:
Inclusion criteria
Adult patients with uncontrolled diabetes (defined as having glycated haemoglobin blood (HbA1c) ≥ 8%), able to speak either Arabic or English, able to provide informed consent and with a continuous active status with the medical center (defined as having a record of at least one visit in the 6-month before screening).
Exclusion criteria
Patients with severe mental illness or dementia or significant cognitive impairment and patients with unstable acute complications/illness requiring hospitalisation or gestational diabetes were excluded.
Intervention group
The MTM was performed by a certified ambulatory care pharmacist (GB and AQ). To ensure that the pharmacists worked similarly, the service process was carried out in a structured way with framework compiled from the American Pharmacists Association and the National Association of Chain Drug Stores Foundation framework for implementing effective MTM services in a CP setting7.
The MTM arm received the five core elements of MTM; Initial face to face visit with the MTM-pharmacist to conduct a comprehensive medication review (CMR), a personalized medication record (PMR), medication-related action plan (MAP) and referral to other healthcare services if needed.
Follow-up visits were scheduled at week 4, 8, 16 and 20 either by phone calls or clinic visits, in addition to the 3-month and 6-month visits. During these visits, pharmacists assessed patient understanding of their medications, reviewed medications and home monitoring data (blood glucose, blood pressure), if applicable, identified and resolved any new DRPs, provided an additional education session and refereed patients to healthcare providers, if needed. Pharmacist documented patient visits and phone calls in the patients’ medical record.
Control group
In this study, we chose to offer what we believed to be a reasonable standard of care that should be provided by community pharmacists to the target population, rather than just the usual care. The standard of care in the study providing education on newly dispensed medications, advice on minor ailments, regularly answer patient questions and provide education about healthy lifestyle. All patients had unrestricted access to the pharmacist for advice duirng the whole study period. The control group received no intervention related other than the mentioned education.
Outcomes measures
The primary outcome for this study was change in HbA1c (%) from baseline. Secondary outcomes included assessment of clinical parameters, health services utilization, MTM metrics (such as pharmacist consultation time per participant, number of follow up visits, number and types of DRPs, and number of referrals), patient medication adherence, diabetes distress, and patient satisfaction with pharmacist services. The outcomes were assessed at baseline, 3 and 6-month. Table 1 summarizes the study outcomes measures and scales used. All participants had one face-to-face visit at baseline and two follow-up assessment visits, at weeks 12 and 24. During these encounters, data on HbA1c, lipid profile, blood pressure, and healthcare utilization were obtained from the patient and the medical records. Furthermore, all patients completed the Medication Adherence Report Scale (MARS-5)24 and Diabetes Distress Scale (DDS)25) at baseline and the end of the study. Patient Satisfaction was assessed using Patient Satisfaction with Pharmacist Services Questionnaire 2.0 (PSPSQ 2.0)26 administered at the end of study.
Sample size
Initially, the sample size was calculated using Cohen’s power table28 as described in the study protocol21. However, reviewer’s comments led to a change in the methods of analysis for the primary and other continuous outcomes. Consequently, a new power calculation was performed retrospectively. Assuming standard deviations of HbA1c of 1.5, and correlations between HbA1c measurements within participant of 0.5, significance level set at 5%, a study with 64 participants in each arm gave ~ 80% power to detect a mean difference of 0.6 in HbA1c. However, a sample of 160 patients was assumed to be enough to compensate for a 20% attrition rate.
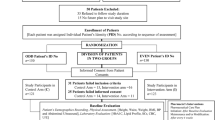
Randomization
Randomization was provided by an independent statistician not involved in the study. Consenting participants were randomized in a 1:1 ratio to either MTM services or control group. Recruitment was conducted until the required number of participants were enrolled. An allocation sequence was based on a computer-generated list of random numbers and sequentially numbered tamper-proof opaque sealed envelopes were used to conceal sequence allocation.
Blinding
Neither patients nor pharmacists delivering the intervention were blinded due to the nature and characteristic of the intervention. However, the data collection process was double-checked by two researchers and data analysis were performed by an independent blinded statistician. Physicians who referred the patients to the MTM program were not informed about the patients’ randomization.
Statistical analysis
All analyses were conducted using Stata/SE 17 to analyse the impact of the intervention by comparing baseline, 3- and 6-month changes in HbA1c between the intervention and control group. Data were analysed according to the ‘‘intention-to-treat’’ principle.
In the baseline characteristics table outcomes for count and categorical variables were compared using Chi-square tests and reported as numbers and percentages. While the continuous variables were analysed using t-tests if normally distributed data and reported as means (standard deviation (SD)) and Mann Whitney test if non-normally distributed data and reported as medians (interquartile range (IQR)). P-values with two-tailed significance levels of 0.05 were used.
To allow for a varying treatment effect over time, a time by treatment interaction parameter was included in the model as standard (estimates of differences between groups at the relevant time will be taken from the model including this interaction parameter).
For continuous outcomes the difference between group means and associated confidence intervals at each time point were estimated using a mixed effects linear regression model allowing for repeated measurements at 3-month and 6-month assessment times and adjusting for baseline score. Parameters allowing for treatment group, baseline score, and time were included as fixed effects with a random effect for participant. A time by treatment interaction term is included with a p-value based on a likelihood ratio test. Heavily positively skewed outcomes (SBP, ACR, TG and Scr) were (natural) log transformed. All models were fit using maximum likelihood estimation with robust standard errors. Logistic regression was used for binary variable (MARS-5 questionnaire) and ordinal logistic regression was used to measure more than two categories (DDS questionnaires). Additionally, Firth-type logistic regression was used for healthcare utilization due to the small number of events.
Results
Recruitment and follow-up
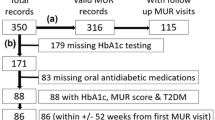
A total of 661 patients were screened for eligibility. Three hundred fifty-seven eligible patients were contacted for recruitment. One hundred ninety-seven did not respond, leaving 160 patients agreeing to participate who were randomly assigned to the control group (standard of care) or the intervention group (MTM program). Recruitment continued over 19-weeks (from April 13, 2021 to September 8, 2021). The data were collected from April 2021 to June 2022 (14-month period). Of the intervention group, 65 (81.25%) of the participants completed all follow-up visits and 64 (80%) of the participants completed all follow-up visits in the control group. Patients’ recruitment and flow throughout the study are shown in Fig. 1.
Baseline characteristics
Table 2 shows the socio-demographic and clinical characteristics of participants at baseline. Overall participants had comparable sociodemographic characteristics at the point of recruitment between the two arms. The majority of participants were male [109 (68.1%)], mean age in both groups was 50 (SD ± 11.9) years, a median duration of diabetes of 8 [IQR 3, 14] years, and HbA1c 9.8% [IQR 8.9, 11.2]. Per participant, the median number of medications prescribed was 5 [IQR 3, 7].
Clinical outcomes
Primary outcome (glycated haemoglobin blood)
There was no evidence of a treatment-time interaction for HbA1c. Both the intervention and control groups experienced reductions in HbA1c levels. After adjusting for baseline HbA1c, the mean HbA1c level in the intervention arm was 0.02% (95% CI, 0.6 – 0.5, P = 0.929) lower compared to the control arm at 3-month and 0.2% (95% CI, -0.8 – 0.3, P = 0.47) lower at 6-month. However, there was a significant reduction in the HbA1c in the intervention arm at 6-month visit compared to the baseline visit (from mean ± (SD) 10.3 ± (1.9) to 8.6 ± (1.7), p < 0.0001).
In addition, more individuals in the intervention group (11 (15.3%)) than in the control group (8 (11.8%)) achieved a HbA1c of 7% or lower at 3-month follow-up (p = 0.544). At 6-month, the participants achieving HbA1c of < 7% in both arms were similar (intervention group 9 (13.9%) and control group (9 (14.1%), p = 0.972).
Secondary outcomes
There was a significant reduction in systolic and diastolic blood pressure readings at 6-month in the intervention group compared to the control group (-3.2; 95% CI, -6.4 – 0.0 and -3.8; 95% CI, -6.6 – -1.0), respectively. For renal parameter, there was a significant reduction in SCr readings at 6-month in the intervention group compared to the control group (-9.6; 95% CI, -16.4 – -2.3). For lipid and ACR despite significant missing values in some outcomes, there was a trend towards lower levels in the intervention arm compared to the control arm at 6-month; however, evidence was uncertain. There was evidence of a treatment-time interaction for the outcomes of DBP, SBP, and Scr. There was no evidence of an interaction for LDL, TC, ACR and TG. Table 3 and Figs. 2 and 3 summarize the impact of the MTM program on specified clinical outcomes at 3- and 6-month assessment points.
Clinical outcomes (secondary) result for both trial groups across trial visits. (a) Mean Systolic blood pressure results for both trial groups across trial visits. (b) Mean diastolic blood pressure results for both trial groups across trial visits. (c) Mean low-density lipoproteins results for both trial groups across trial visits. (d) Median triglyceride results for both trial groups across trial visits. (e) Mean total-cholesterol results for both trial groups across trial visits. (f) Median serum creatinine results for both trial groups across trial visits. (g) Median Albumin-to- creatinine ratio results for both trial groups across trial visits.
MTM metrics
Consultation time
The median consultation time pharmacists spent with each patient varied based on study time point. At baseline the mean time was longer since the first visits require comprehensive medication review. However, in the two follow up visits, the encounter went faster (Table 4).
DRPs
During the study period, in the intervention group, the pharmacist identified 191 DRPs at baseline with an average of 2.39 DRPs per patient. There was a significant drop (p = 0.0001) in DRPs at 3-month (0.96 DRP per patient, 64% overall drop of DRP) and 6-month (0.92 DRP per patient, 69% overall drop in DRP) follow-up. The most reported DRPs over the follow-up visits included additional drug therapy needed (96 (31.6%)), noncompliance (91 (29.9%)) and drug dose too low (60 (19.7%)) (Table 4 and Fig. 4).
Follow-up visits
Overall, the number of planned monthly patient follow-ups in the intervention was low. The median number of monthly follow-ups per patient was 1 [IQR, 0, 1]. Only 3% of patients had three monthly follow-ups, 15% had two, 36% had only one, and 45% had no monthly follow-ups at all.
Referrals
During the study, the pharmacist made 68 referrals in the intervention group; 52 (65%) at baseline visit, 11 (15%) at the 3-month visit, and 6 (9%) at 6-the month visit. Most referrals were made to ophthalmologists (n = 41) followed by primary physician (n = 19) and dietitian (n = 4) (Table 4).
Health service utilization
During the study period, none of the participants in the intervention group reported hospitalization or ER visits compared to 14 participants in the control group (8 participants at 3-month and 6 at 6-month). The odds of healthcare utilization were 95.1% lower (95% CI, 0.003–0.9) (p = 0.04) in the MTM program group compared to the standard care group at 3-month. While at 6-month the reduction in odds of healthcare utilization was 93.1% (95% CI, 0.004–1.3) (p 0.07) in MTM program group. Data are illustrated in Table 5.
Medication adherence, diabetes distress and satisfaction
Three questionnaires were used throughout the study. MARS-5 questionnaire to assess patients’ reported medication adherence24. The odds of the patient’s adherence improvement in the MTM program group at 6-month were 8 times (95% CI, 3.6 – 17.4) higher than the standard care group (p < 0.001). MARS-5 scores showed that more participants in the intervention group (76.9%) scored ≥ 24 (adhere) compared to the control group (29.7%), as shown in Tables 5 and Fig. 5a.
Adherence, Diabetes Distress and Patient Satisfaction results for both trial groups across trial visits. (a)Median Reported adherence using MARS-5 Q for both trial groups across trial visits. (b) Median Reported distress using DDQ for both trial groups across trial visits. (c) Participant satisfaction with pharmacist services at six-month follow-up.
Similar results were seen with the diabetes distress questionnaire25, the MTM program significantly reduced the odds of patients’ distress by 93.4% (95% CI, 0.03 – 0.2) compared to standard care (p < 0.001). As shown in Table 5 and Fig. 5b. Furthermore, data shows that after 6-month of follow-up, 72% of the patients in the MTM program group likely did not suffer from any distress compared to the control group where 39% of the patients have moderate or high distress.
Scores on PSPS 2.026 showed that participants in the MTM program group were more satisfied with pharmacist services than participants in the control group (p = 0.001). Data are illustrated in Table 5 and Fig. 5c.
Discussion
This study was undertaken to investigate the effectiveness of a CP-based MTM program on health outcomes for patients with uncontrolled diabetes in KSA. One hundred sixty patients were enrolled and 80% completed the study.
The main findings of this study indicate that establishing MTM program in KSA is feasible and can be delivered in the community setting. Indeed, the program can potentially improve clinical outcomes, optimize the use of medications by identifying and resolving DRPs, reduce healthcare utilization and consequently reduce distress and improve medication adherence and patient’s satisfaction.
Although the present study was conducted in KSA, its findings were comparable to those of previous studies in different countries and health systems9. Our study shows that the provision of MTM programs to patients with diabetes has the potential to reduce the HbA1c by 0.2% (95% CI, -0.8 – 0.4) after 6-month of follow-up. This is lower than previous literature that demonstrated a value of 0.6% drop in HbA1c with similar MTM program9. Aside from chance, there are several possible reasons for this difference . First, the time effect suggested that gradual improvement in HbA1c was possible29. Data comply with the systematic review9, 4 out 6 studies30,31,32,33, introduced the intervention for more than 6-month while the duration of the current study was only 6 months. Second, we chose to provide the standard of care for the control group instead of usual care, to facilitate the study recruitment and impove patient retention and to represent the ideal role of pharmacist. This may have affected results and reduced the difference in the primary outcome. Third, the overall number of monthly follow-up and referrals were lower and most of the patients refused to take the PMR, which may have affected the quality-of-service delivery. Finally, the impact of pharmacist intervention is greatest among those with higher baseline levels of HbA1c34. Data aligns with the current study’s data, where the median HbA1c level at baseline was 9.9% in control group and 9.6% in the intervention group. These factors may have minimized the overall difference between the two groups. Indeed, within each group the improvement of HbA1c was significantly better than from the baseline.
Globally, various medication review services have been introduced as a program intervention for patients with chronic disease, all demonstrating a significant positive impact on patients’ health outcomes9. However, this study describes the first-of-its-kind service not previously introduced or even evaluated in the KSA. The evidence generated from this study will help to assess the extent to which the international MTM program can be adapted for national implementation by developing a framework tailored to the specific needs of the people in KSA. It also underscores the pharmacist’s role as an integral member of primary care services, enhancing the quality of care provided.
This study has several limitations. First, this study is a single RCT in a single CP, and therefore results may not be generalisable to all Saudi community pharmacy practices. However, a cluster randomised design was not feasible because of MTM program is a new program introduced in the Saudi CP and availability of qualified pharmacists to deliver MTM was limited. In addition, the study aim was to test the effectiveness, applicability and implantability of MTM program in CP in KSA.
Second, a degree of caution should be considered when interpreting results and applying to a wider population because this research has focused solely on patients with diabetes, and therefore views might not be generalisable to other chronic diseases. Furthermore, the recruitment was from customers of one-health center so as to ensure follow up was possible and give the pharmacist access to patients’ records, which may not be the case in other CP.
Third, same pharmacists who delivered the MTM program, also managed the control group, so contamination of effect can not be excluded and could have skewed the treatment effect towards the null.
Fourth, few patients’ referrals were made by the GPs in the medical center to the MTM program due to their workload. Fifth, owing to the nature of pharmacists’ interventions in this study, participants and the pharmacists could not be blinded to the study intervention. However, the data collection and analyses were performed by a blinded principal researcher and statistician. Finally, the follow-up reported here is limited to 6 months. A longer follow-up may provide more insights on the longer term effects of the MTM program.
Implications for Community pharmacy practice in Saudi and Middle East and North Africa (MENA) region
Data from this study could help benchmark practice. We hope that this pioneered intervention will become incorporated into the mainstream of Saudi CP practice. The integration of MTM service into routine CP practice will be of significant interest to the growing number of organisations attempting to implement such advanced services to improve the practice and to support MOH strategies for pharmaceutical care.
This study provides possible directions for clinical practice and policy. Many of the lessons learned from this study will likely be of use in informing the implementation of similar complex interventions in the MENA region. This service would trigger a series of reforms and encourage other community pharmacists in other countries to expand their scope of practice.
Conclusion
In conclusion, CP-based MTM program can be implemented in KSA and potentially improve outcomes for patients with uncontrolled diabetes. In addition to reducing diabetes distress and improving medication adherence, such CP-based service can potentially not only reduce DRPs but also reduce the burden on the health system by reducing ER visits and hospitalization. Nevertheless, there are several areas that need further investigation and new opportunities for future work to shape up the role of community pharmacists in delivering patient care activities.
Data availability
The data that support the findings of this study are available from the corresponding author, [Hadi, MA], upon reasonable request.
References
United Nations Interagency Task Force on the Prevention and Control of Noncommunicable Diseases. The investment case for noncommunicable disease prevention and control in the Kingdom of Saudi Arabia: return on investment analysis & institutional and context analysis. Geneva: World Health Organization (2017)
Todd, A., Copeland, A., Husband, A., Kasim, A. & Bambra, C. The positive pharmacy care law: an area-level analysis of the relationship between community pharmacy distribution, urbanity and social deprivation in England. BMJ Open https://doi.org/10.1136/bmjopen-2014-005764 (2014).
Smith, M., Giuliano, M. R. & Starkowski, M. P. In Connecticut: improving patient medication management in primary care. Health Aff. 30(4), 646–654 (2011).
Alfadl, A. A., Alrasheedy, A. A. & Alhassun, M. S. Evaluation of medication counseling practice at community pharmacies in Qassim region Saudi Arabia. SPJ 26, 258–262 (2018).
Giberson, S., Yoder, S. & Lee, M.P. Improving patients and health system outcomes through advanced pharmacy practice. A report to the U.S. Surgeon General. http://www.accp.com/docs/positions/misc/Improving_Patient_and_Health_System_Outcomes.pdf (2011)
Buss, V. H., Shield, A., Kosari, S. & Naunton, M. The impact of clinical services provided by community pharmacies on the Australian healthcare system: a review of the literature. J. Pharm. Policy Pract. https://doi.org/10.1186/s40545-018-0149-7 (2018).
American Pharmacists Association and the National Association of Chain Drug Stores Foundation. Medication therapy management in pharmacy practice: core elements of an MTM service model (version 20). JAPhA. 48, 341–353 (2008).
Medicare prescription drug, improvement, and modernization act of 2003 (pub. L. no. 108–173, 117 stat. 2066). http://www.gpo.gov/fdsys/pkg/PLAW-108publ173/html/PLAW-108publ173.htm (2003).
Al-Babtain, B., Cheema, E. & Hadi, M. A. Impact of community-pharmacist-led medication review programmes on patient outcomes: A systematic review and meta-analysis of randomised controlled trials. RSAP. 18(4), 2559–2568 (2022).
Health sector transformation strategy. Saudi Ministry of Health. https://www.moh.gov.sa/en/Ministry/vro/Documents/Healthcare-Transformation-Strategy.pdf (2017).
Babiker, A. H., Carson, L. & Awaisu, A. Medication use review in Qatar: are community pharmacists prepared for the extended professional role?. Int. J. Clin. Pharm. 36(6), 1241–1250 (2014).
Bawazir, S. Consumer attitudes towards community pharmacy services in Saudi Arabia. IJPP 12, 83–89 (2004).
Ministry of health. Healthcare Licensing Services, https://www.moh.gov.sa/en/eServices/Licences/Pages/Licences.aspx (2019).
Alomi, Y. A. New pharmacy model for Vision 2030 in Saudi Arabia. JPPCM 3(3), 194–196 (2017).
National Transformation Program 2020. http://www.vision2030.gov.sa/en/ntp (2016)
Ministry of Health. Regulation-of-Pharmaceutical-Products-and-Institutions. https://www.moh.gov.sa/eServices/Licences/Pages/01.aspx (2019).
MOH; Appendix 4. Requirements and procedures for providing pharmaceutical care services in pharmacies. 1st ed. Saudi Arabia: Ministry of Health (2019).
Alanazi, A., Alfadl, A. & Hussain, A. Pharmaceutical care in the community pharmacies of Saudi Arabia: Present status and possibilities for improvement. SJMMS 4(1), 9–14 (2016).
Dib, J. G. & Abdulmohsin, S. A. Establishing a pharmaceutical care clinic in a Saudi Arabian health center. AJHP 64(1), 107–109 (2007).
Siddique, A., Ahmed, E., Al Zoghabi, M., Alsaif, E. & Alhawshani, F. Exploring community pharmacist’s knowledge, attitude, and practice toward the provision of pharmaceutical care. A prospective cross-sectional study from Saudi Arabia. J. Pharm. Bioallied. Sci. 14, 13 (2022).
Albabtain, B. et al. Evaluation of a community pharmacy-based medication therapy management programme: A study protocol of a pilot randomized controlled trial with an embedded qualitative study. SPJ 29, 706–712 (2021).
Albabtain, B. et al. Impact of medication therapy management programme on diabetes healthcare outcomes in a community pharmacy setting. ISRCTN Registry: ISRCTN60703981. Preprint at: https://doi.org/10.1186/ISRCTN60703981 (2022).
Schulz, K. F., Altman, D. G. & Moher, D. CONSORT 2010 Statement: updated guidelines for reporting parallel group randomised trials. BMJ https://doi.org/10.1136/bmj.c332 (2010).
Horne, R., Weinman, J. & Hankins, M. The beliefs about medicines questionnaire: the development and evaluation of a new method for assessing the cognitive representation of medication. Psychol Health 14, 1–24 (1999).
Polonsky, W. H. et al. Assessing psychosocial distress in diabetes: Development of the diabetes distress scale. Diabetes Care. 28, 626–631 (2005).
Sakharkar, P. et al. Development and validation of PSPSQ 2.0 measuring patient satisfaction with pharmacist services (RSAP, 2015).
Cipolle, R. J., Strand, L. M. & Morley, P. C. Pharmaceutical Care Practice 3rd edn. (McGraw-Hill Book Co, 1998).
Cohen, J. Statistical power analysis for the behavioral sciences (Routledge, 2013).
Paulo, P. T. C. et al. A Randomized Clinical Trial Of The Impact Of Pharmaceutical Care On The Health Of Type 2 Diabetic Patients. Lat. Am. J. Pharm. 35, 1361–1368 (2016).
Clifford, R. M., Davis, W. A., Batty, K. T. & Davis, T. M. E. Effect of a pharmaceutical care program on vascular risk factors in type 2 diabetes: the Fremantle diabetes study. Diabetes Care 28, 771–776 (2005).
Doucette, W. R., Witry, M. J., Farris, K. B. & Mcdonough, R. P. Community pharmacist-provided extended diabetes care. Ann. Pharmacother. 43, 882–889 (2009).
Ali, M. et al. Impact of community pharmacy diabetes monitoring and education programme on diabetes management: a randomized controlled study. Diabet. Med. https://doi.org/10.1111/j.1464-5491.2012.03725.x (2012).
Planas, L. G., Crosby, K. M., Farmer, K. C. & Harrison, D. L. Evaluation of a diabetes management program using selected HEDIS measures. J. Am. Pharm. Assoc. 52, e130-138 (2012).
Osborn, C. Y. et al. Development and Implementation of a Culturally Tailored Diabetes Intervention in Primary Care. Transl Behav Med. 1(3), 568–479 (2011).
Acknowledgements
M.J.P. is supported by the National Institute for Health Research Birmingham Biomedical Research Center.
The views expressed are those of the investigators and not necessarily those of the NHS, NIHR or the Department of Health and Social Care. Open access publication charges were funded by QU Health, Qatar University.
Author information
Authors and Affiliations
Contributions
Basmah Albabtain conceptualization, data curation, project administration, formal analysis, methodology, Writing – Original Draft Preparation, Ghada Bawazeer & Abdulaziz Alqahtani resources, data curation, supervision, validation, Writing – Review & Editing, Vibhu Paudyal methodology; funding acquisition, supervision, formal analysis, Writing – Review & Editing, Ejaz Cheema conceptualization, methodology, supervision, Writing – Review & Editing, Ahmed Bahatheq resources, project administration, Writing – Review & Editing, Malcolm J Price formal analysis, resources, Writing – Review & Editing, Muhammad Abdul Hadi conceptualization, methodology, project administration, supervision, validation, formal analysis, Writing – Review & Editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Albabtain, B., Bawazeer, G., Paudyal, V. et al. Impact of a community pharmacy-based medication therapy management program on clinical and humanistic outcomes in patients with uncontrolled diabetes: a randomised controlled trial. Sci Rep 14, 17818 (2024). https://doi.org/10.1038/s41598-024-65759-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-65759-x
- Springer Nature Limited