Abstract
Contemporary medical approaches for opioid addiction often include medication-assisted therapy, utilizing methadone and buprenorphine. However, factors influencing patient preferences for starting buprenorphine or methadone therapy are poorly understood. This study aims to explore whether variances in personality traits and attachment styles are related to treatment preferences among individuals undergoing buprenorphine and methadone maintenance therapies. 300 participants completed the Big Five Questionnaire for personality traits and sub-dimensions and the Experiences in Close Relationship Scale for assessing attachment styles. The results indicated that patients with higher levels of Dynamism, Conscientiousness, and Perseverance personality traits were more likely to choose buprenorphine over methadone for achieving and maintaining abstinence. Although attachment styles showed a greater ability to differentiate between groups compared to personality traits, the differences were not significant. However, Conscientiousness stood out for its high discriminant validity, suggesting that scores in this personality dimension could significantly distinguish between groups, with individuals in the buprenorphine group showing higher levels of Conscientiousness compared to the methadone group. The study suggests a partial association between individuals' preference for abstinence therapy and their personality traits. These findings could be considered useful indicators when choosing maintenance therapy to help opiate-addicted patients achieve and maintain abstinence.
Similar content being viewed by others
Introduction
Substance addiction has been conceptualized as a brain disease, substantiated by the alterations induced by drugs in the structure and functionality of the brain1. Characterized as a chronic, recurrent disease, addiction is proposed to arise from the interaction between the organism and the drug, driving behavioral and other changes driven by an irresistible internal compulsion to continue drug intake, despite awareness of harmful consequences (loss of control)2. As such, etiological models, including the biopsychosocial model of addiction3, conceptualize addiction as a multifaced disorder, wherein this internal compulsion is attributed not only to biological factors but also to psychological and social factors3. These psychosocial factors encompass individual psychological traits, such as personality and coping mechanisms, as well as social determinants such as environmental influences, socioeconomic status, and cultural norms4. Together, these components interact to shape an individual's susceptibility to addiction, the development of addictive behaviors, and the effectiveness of prevention and treatment strategies5,6. Contemporary medical practices for addressing opioid addiction frequently involve the application of medication-assisted therapy, notably utilizing methadone and buprenorphine, with the aim of managing addictive behaviors and facilitating the cessation of opiate use7. Methadone (MET), functioning as a full µ-opioid receptor agonist, engages with the brain's receptors identical to those targeted by opioids such as heroin or prescription pain medications, whereas buprenorphine (BUP), as a partial opioid agonist, attaches to opioid receptors exhibiting ceiling effect, meaning that beyond a specific dosage, it does not impart further effects, thereby diminishing the potential for misuse8,9. The literature underscores the importance of methadone and buprenorphine in alleviating withdrawal symptoms and cravings by acting on opioid receptors10,11. Notably, some patients prefer buprenorphine over methadone, finding it more useful and effective in treating opioid dependence, including the blockage of cravings12.
However, collaborative therapy decisions involve both the psychiatrist and the patient, with the choice of a specific therapy setting contingent upon various factors, including but not limited to the patient’s health status, medication availability, potential side effects, risk of abuse and overdose, cost considerations, and long-term effects13,14. Despite these considerations, limited knowledge exists regarding other decisive factors influencing patients' preference for initiating buprenorphine or methadone therapy. One such factor that may influence the preference of medication-based therapy is the individual's traits15,16. So far, existing research underscores the significant variability in personality traits among individuals with different substance use tendencies17,18,19. Individuals exhibiting elevated levels of neuroticism and high extraversion are more inclined towards the usage of cocaine/crack, heroin, and stimulants; heightened openness to experience demonstrates an association with cannabis use, while low levels of agreeableness links to cocaine/crack use and the illicit consumption of opioids20,21,22. Given the intricate nature of these associations, it is plausible to argue that personality traits may also play a significant role in shaping patients' inclination toward the choice of medication-based therapy for opioid addiction.
Another factor that offers a valuable framework for comprehending the origins of addictions and may be influencing the preference for medication-based therapies is the attachment style23. Attachment theory posits that early-life interactions with caregivers promotes the development of mental representation of self and others, as well as support systems received during vulnerable moments24. For instance, signaling distress and seeking proximity to a health care provider as well as negotiating for therapy in times of illness is likely to be expressed in a way that is consistent with attachment characteristics25, particularly in individuals with Substance Use Disorder (SUD)26. Although the literature regarding attachment styles and patients’ preference of methadone or buprenorphine therapy option is lacking, there are extensive links between attachment and substance dependency27,28, specifically examining highly insecure attachment patterns indicating divergent developmental trajectories among various groups of substance abusers. Particularly, the prevalence of a fearful–avoidant attachment pattern emerges prominently among individuals with heroin addiction29.
Given that addiction is widely recognized as a chronic, relapsing disease, and opioid addiction presents as a particularly challenging chronic condition, exploring the association between personality traits, attachment style, and treatment preference for buprenorphine and methadone therapies holds significant promise in optimizing addiction treatment outcomes. The provision of substitution therapy, such as buprenorphine and methadone, plays a crucial role in harm reduction approaches for individuals with addiction, facilitating early stabilization and functional improvement in familial and work environments12,30,31. Furthermore, by aligning treatment preferences with patients' personality traits and attachment styles, clinicians can increase treatment retention and satisfaction, as well as decrease the risks associated with illegal "self-medication," involvement in criminal activities, and exposure to additional health risks32,33. This can be achieved by offering therapies that resonate with patients' psychological and emotional needs, thereby reducing dropout rates and enhancing long-term recovery prospects34.
The present study
Research addressing the distinct personality traits and attachment styles of individuals undergoing medication-based therapy for opioid addiction, particularly those receiving methadone and buprenorphine therapy, is currently lacking. Therefore, our study seeks to: (a) elucidate variations in personality traits and attachment styles within the subset of individuals undergoing buprenorphine and methadone maintenance therapy, and (b) investigate whether these individuals differ in personality traits and attachment styles depending on their choice of the maintenance therapy. Given the empirical evidence on personality traits and insecure attachment style within the context of addiction, we expect that the choice of methadone or buprenorphine therapy by individuals with opioid addiction will be influenced, in part, by their personality traits and attachment patterns. We also expect that individuals opting for buprenorphine maintenance therapy (considered more useful and effective in treating opioid dependence) will exhibit a less pronounced insecure attachment style and more favorable personality traits, reflected by higher scores on five major dimensions of personality, in comparison to their counterparts receiving methadone maintenance therapy.
Methods
Participants and procedures
The research was initiated by a qualified psychiatrist at the Service for Mental Health, Addiction Prevention, and Outpatient Treatment in Split, Croatia. The data were collected by a trained researcher during regular outpatient consultation times. Before starting the survey, participants were informed about the objectives and procedure of the research study, and they acknowledged that their participation was voluntary and confidential. All participants were provided with informed consent to take part in the study, agreeing to have their data used for analysis. To prevent coercion or undue influence, regular monitoring of psychiatrist-patient dynamics was maintained throughout the study. The study included 300 individuals with heroin addiction, divided evenly into two distinct groups. Group 1 consisted of 150 individuals receiving methadone maintenance therapy for heroin addiction, while Group 2 comprised of 150 individuals undergoing buprenorphine maintenance therapy. Inclusion criteria were defined as follows: a diagnosis of opioid dependence (ICD-10 Code F11.2)35, a documented 12-month abstinence from heroin as indicated in medical records maintained by the mental health support service, a negative result in the urine drug test taken prior the study assessment, and a positive test for the prescribed maintenance therapy on the day of administering the measurement instruments. This positive result was determined through the use of the panel drug test for detecting consumption of opioids such as heroin, morphine, and codeine present in a urine sample at a concentration of at least 300 ng/ml (MOP), for detecting buprenorphine at a concentration of 10 ng/ml (BUP) and for detecting methadone (Heptanone, substitution therapy) at a concentration of 300 ng/ml (MTD). Exclusion criteria included failure to register with the Croatian National Register of Treated Psychoactive Drug Addicts at the Croatian Institute of Public Health and the presence of cognitive impairment or intellectual disability.
Ethical approval for the study was obtained from the Ethics Committee of the School of Medicine, University of Zagreb, aligning with research activities conducted at the Teaching Institute of Public Health, County of Split Dalmatia, Service of Mental Health, one of the main educational and research bases within the University, operating under valid permits of the competent University authorities. All participants provided written informed consent before participating.
Measures
The Big Five Questionnaire (BFQ) was utilized to assess the personality traits27, The BFQ, aligned with the five-factor model of personality, examines five principal dimensions, each encompassing two sub-dimensions: Energy (Dynamism and Dominance), Agreeableness (Cooperativeness/Empathy and Warmth/Friendliness), Conscientiousness (Scrupulousness and Perseverance), Emotional Stability (Emotional Control and Impulse Control), and Openness (Cultural Openness and Openness to Experience) and a Lie scale. The inventory contains 132 statements that are distributed across the dimensions and sub-dimensions. Each dimension includes 24 statements, while sub-dimensions consist of 12 statements each, scored on a 5-point scale (1 = 'not at all true'; 5 = 'exactly true'). Total scores are derived by summing the scores for specific items within each sub-dimension, facilitating the computation of total scores for the BFQ dimensions36.
To evaluate distinct dimensions of attachment within friendships, a shortened version of the Experiences in Close Relationships Scale (ECR) was employed. The scale had been validated among a Croatian population37, containing identical psychometric characteristics to the original scale38, (detailed in37). The scale, comprising 18 statements, evaluates individuals' feelings, thoughts, and behavior in close relationships. Participants rate each item on a 7-point scale, ranging from 'strongly disagree' to 'strongly agree,' based on how well it reflects their own experiences with friends in general. The scale consists of two subscales, Anxiety and Avoidance, each comprising 9 items, demonstrating high reliability (Cronbach’s alpha: 0.86 for Avoidance, 0.83 for Anxiety). The orthogonal subscales strongly correlate with their underlying factors (r = 0.08).
Data analysis
The characteristics of the studied groups were described using descriptive parameters. Pearson’s correlation coefficient was used to explore associations between personality traits and attachment styles, providing insights into the relationships within the buprenorphine and methadone groups. To examine significant differences between the two groups including demographic characteristics as well as group means pertaining to personality traits and attachment styles, T-test and χ2 test scores were employed. Finally, to examine whether two groups of participants differ on a set of variables and determine which variables contribute most to group separation, discriminant analyses were employed. Initially, the potential differentiation of the two groups was investigated based on their scores on the BFQ questionnaire and subsequently on the ECR questionnaire. Three discriminant analyses were conducted, one for each of the three groups of variables: traits of the five-factor personality model (5 variables) and individual sub-dimensions of the traits of the five-factor personality model (10 variables), followed by dimensions of attachment (2 variables).
Ethics approval
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000 (5). Ethical clearance for the study was obtained from the Ethics Committee of the School of Medicine, University of Zagreb.
Results
The total sample included 300 participants. 150 participants belonged to the buprenorphine group (mean age = 38.6; SD = 5.9; 86% male) and 150 participants belonged to the methadone group (mean age = 41.5; SD = 7.4; 79% male). There was a significant difference in age between the two groups (χ2 = 3.681, p < 0.001). The methadone group had a higher average age compared to the buprenorphine group. Additionally, there was a significant difference in marital status between the two groups (χ2 = 10.587, p = 0.032). Specifically, the buprenorphine group had a lower percentage of patients who are not married compared to the methadone group. (See descriptive statistics in Table 1).
The bivariate correlations between personality traits and dimensions of attachment in both groups are presented in Supplemental Table 1. According to Cohen39, effect size of 0.10 is small, 0.30 is medium, and 0.50 is a large effect size.
Differences in personality traits and attachment styles
While the majority of sub-dimensions of the BFQ exhibited a tendency towards higher mean values in the buprenorphine maintenance therapy group, statistically significant distinctions were observed between the two groups in Dynamism (t = 2.020; p = 0.044), Conscientiousness (t = 2.759; p = 0.006), and Perseverance (t = 3.589; p < 0.001). The difference in Agreeableness approached statistical significance (t = 1.943; p = 0.053). In all instances, the average score was notably higher in the buprenorphine maintenance therapy group (Table 2). No statistically significant differences were identified between the groups concerning scores on either dimension of attachment-related anxiety or avoidance (Table 2).
Discriminant analysis of group differentiation in the five-factor model of personality and attachment styles
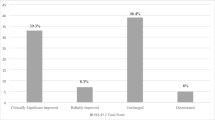
The discriminant function initially classifying participants as treated with buprenorphine or methadone based on the five major personality traits of the five-factor personality model was not significant (χ2 = 10.453; p = 0.063). However, a canonical correlation between group membership and the obtained discriminant function was 0.186, with the Conscientiousness trait loading most strongly on the discriminant function. The data revealed that 56% of participants were correctly classified by the discriminant function (i.e., if groups were not known a priori, 56% of participants would have been correctly classified based on their scores on the five-factor model). The accuracy was 6% better than the maximum using random guessing (which yielded a 50% overall classification accuracy). The accuracy was slightly better for the methadone maintenance therapy group than for the buprenorphine group. The values and coefficients of the test and the results of the discriminant analysis are displayed in Table 3.
Additionally, when classifying participants as treated with buprenorphine or methadone based on the sub-dimensions of the five-factor personality model, the discriminant analysis approached significance levels (χ2 = 18.06; p = 0.054). A canonical correlation between group membership and the obtained discriminant function was 0.244, with the Perseverance sub-dimension (corresponding to the major Conscientiousness personality trait) loading most strongly on the discriminant function. The data revealed that 59.3% of participants were correctly classified by the discriminant function, indicating 9.3% better accuracy than the maximum using random guessing. Thus, the accuracy was again slightly better for the methadone maintenance therapy group than for the buprenorphine group. The values and coefficients of the test and the results of the discriminant analysis are displayed in Table 4.
Lastly, the discriminant function classifying participants as treated with buprenorphine or methadone based on the anxiety and avoidant attachment style significantly distinguishes the group on buprenorphine from the group on methadone, with a canonical correlation of 0.352. The obtained discriminant function allows us to correctly classify 67.0% of the participants based on the results of anxiety and attachment dimensions. This is 17% better than random guessing, which, when distinguishing between two groups, is 50% overall classification accuracy. The values and coefficients of the test and the results of the discriminant analysis are displayed in Table 5.
Discussion
This study investigated personality traits and attachment styles in individuals undergoing buprenorphine and methadone maintenance therapy. It aimed to explore differences in these traits based on the selected maintenance therapy, considering the influence of personality and attachment patterns on therapy choices in substance addiction. The findings revealed that individuals on buprenorphine maintenance therapy showed higher levels of Conscientiousness and slightly elevated Agreeableness compared to those on methadone therapy. Additionally, buprenorphine recipients exhibited significantly increased levels of Dynamism and Perseverance. Concerning the attachment dimension, no statistically significant distinction was found between the two groups.
The Conscientiousness dimension within the Big Five Questionnaire (BFQ) stands out for its high discriminant validity, indicating that scores in this personality dimension can reveal significant differences between groups. Conscientiousness, reflecting self-regulation and self-control, includes traits such as reflexivity, orderliness, precision, and persistence36. Notably, individuals opting for buprenorphine therapy showed elevated Conscientiousness levels, suggesting a preference for this treatment, while those with lower Conscientiousness tended to select methadone.
Despite the statistical approach of the discriminant function based on the five-factor model of personality, the classification accuracy marginally favored the methadone maintenance group. The discriminant analysis results indicated that just over half of individuals undergoing buprenorphine therapy were correctly classified, with a corresponding classification accuracy of 57.3% for the methadone group. The group prediction classifier relying on BFQ scores demonstrated slightly superior performance compared to random guessing, achieving an accuracy of 56%. While the BFQ exhibited some predictive validity, the modest improvement over random guessing emphasizes the ongoing need for research and refinement in comprehending the intricate relationship between personality traits and treatment choices.
Previous studies have depicted individuals with opioid addiction as commonly exhibiting traits such as anxiety, vulnerability, sensitivity, impulsivity, impatience, and irritability, often coupled with tendencies towards passivity, uncooperativeness, lack of empathy, and low levels of conscientiousness and perseverance40,41. Interestingly, those on buprenorphine therapy for opioid addiction diverge from these typical addiction profiles as the mentioned personality traits expressed in this group describe them as being active, energetic, and talkative, as well as demonstrating higher levels of conscientiousness, orderliness, precision, and perseverance compared to their counterparts on methadone, aligning with our initial hypothesis. Furthermore, these traits have been noted in non-drug users when compared to users42, which further aligns with the personality traits exhibited by participants undergoing buprenorphine therapy. Conversely, in a study of different groups of psychoactive substance users, the results showed that the profiles of cocaine/heroin users achieve very high vulnerability in the dimension of neuroticism (emotional instability), and very low competence and success as well as achievement orientation in the dimension of conscientiousness of the five-factor model of personality43. These personality traits better correspond to the characteristics of our participants on methadone therapy. It is thus possible that precisely individuals with opioid addiction exhibiting high Conscientiousness and Perseverance, coupled with proactive behavior, may be inclined to choose buprenorphine—a partial opioid receptor antagonist—in their pursuit of abstinence.
Conscientiousness as a personality trait appears to play a pivotal role in guiding individuals towards buprenorphine. Its partial opioid receptor antagonism potentially serves as a motivating factor for individuals to stabilize in abstinence quickly—aiming not just to avoid withdrawal crises, but to achieve absolute chemical control of addiction, thereby accepting the absence of relapse readily. Similarly, the heightened Dynamism and Perseverance observed in these individuals further influence their preference for buprenorphine therapy, as they may take responsibility for independent daily medication. These traits are integral to their everyday functioning and may influence their choice towards buprenorphine. Importantly, it is emphasized that their motivation is not driven by seeking the 'high' associated with methadone, as noted in previous studies44. Instead, these individuals seek a 'clear-headed' state, as highlighted in the work of Whelan and Remski45. Conversely, the fact that no significant difference in Emotional Stability and Mental Openness between the two groups of participants was found may indicate that they are equally sensitive and open to new experiences. It is possible that these characteristics may lead them into risky behavior and subsequently into addiction.
In terms of attachment dimensions and personality traits predicting the choice between buprenorphine and methadone therapy for opioid addiction, discriminant analysis results indicated that attachment styles exhibited superior discriminatory efficacy compared to personality traits. The predictive validity was notably elevated, particularly for the methadone group, where 70% of individuals were accurately classified. The classifier relying on attachment dimensions questionnaire scores demonstrated a predictive validity of 67%, marking a significant 17% improvement over random guessing.
Existing research consistently highlights attachment insecurity among individuals with diverse mental disorders, including addiction24,46,47. Notably, individuals with heroin addiction often display a general inclination toward insecure attachment, predominantly characterized by a fearful–avoidant attachment style48,49. Based on the aforementioned results, we assumed differences between groups of individuals with heroin addiction undergoing different types of substitution therapy in a way that individuals on buprenorphine have a more secure attachment style and are less insecurely attached compared to individuals on methadone maintenance therapy. However, despite this general inclination, the specific choice between buprenorphine and methadone treatment did not emerge as a distinctive factor depending on attachment styles in this particular cohort. The decision-making process for choosing opioid addiction therapy is complex, with attachment style representing just one facet within a broader context. While attachment style can influence interpersonal dynamics and mental health, its predictive power in determining the specific choice of therapy may be limited due to the multitude of factors considered by individuals and healthcare professionals in the treatment decision-making process50.
The strength of our current study underscores distinctions between individuals undergoing buprenorphine and methadone maintenance therapy concerning personality traits and attachment styles—a novel investigation, particularly in the context of Croatia. The research involved a substantial patient population receiving treatment from specialized physicians authorized to prescribe opioid substitution therapy, including psychiatrists, epidemiologists, and school and adolescent medicine doctors. These specialists underwent standardized training, mitigating potential biases in physician attitudes that might impact patients' choices between methadone and buprenorphine substitution therapy. However, the study has limitations, primarily its cross-sectional nature, which restricts inferences about the causal effects of therapy selection. Furthermore, while the observed differences in age and marital status between the buprenorphine and methadone treatment groups may offer valuable insights into the characteristics of the study population, understanding the complex relationships between demographic factors, treatment choice, and outcomes requires further investigation. Exploring potential confounding variables, such as socioeconomic status, comorbidities, or prior treatment history, in future studies can enhance our understanding of the nuanced factors influencing treatment decisions and outcomes. Additionally, the inability to ascertain whether disparities in personality traits predated substance use initiation or were instead associated with the therapy provided poses a common methodological challenge in studies on personality traits in individuals with opioid addiction. Nevertheless, this study marks the initiation of a quest for psychological tests and measurements aiming to expedite and enhance specialists' precision in selecting appropriate substitution therapies. The study's effort seeks to streamline the therapeutic process, fostering intervention, stabilization, and optimal functional outcomes for individuals grappling with addiction.
In sum, this study is the first to investigate the differences in personality traits and attachment styles between recipients of buprenorphine and methadone maintenance therapy among individuals with heroin addiction. The findings suggest that personality traits and attachment styles may serve as viable, objective, and quantifiable criteria for the judicious selection between methadone and buprenorphine therapy. If subsequent research substantiates the outcomes of this study, psychometric tests may emerge as valuable tools for formulating more precise guidelines in prescribing substitution therapy. Future research should explore additional psychological attributes, and investigate potential factors influencing the choices of substitution therapies among individuals with heroin addiction. This expanded focus would contribute to a more comprehensive understanding of the interplay of psychological elements in therapy selection, thus advancing the refinement of therapeutic interventions and informing evidence-based policies.
Data availability
The data that support the findings of this study are available on request from the corresponding author A.G. The data are not publicly available due to privacy or ethical restrictions.
References
Heilig, M. et al. Addiction as a brain disease revised: Why it still matters, and the need for consilience. Neuropsychopharmacol. 46, 1715–1723. https://doi.org/10.1038/s41386-020-00950-y (2021).
Zou, Z. Definition of substance and non-substance addiction. Adv. Exp. Med. Biol. 1010, 21–41. https://doi.org/10.1007/978-981-10-5562-1_2 (2017).
Marlatt, G. A., Baer, J. S., Donovan, D. M. & Kivlahan, D. R. Addictive behaviors: Etiology and treatment. Annu. Rev. Psychol. 39, 223–252. https://doi.org/10.7334/psicothema2017.303 (1988).
McKillop, J., & Rayt, L. A. The etiology of addiction: A contemporary biopsychosocial approach. In Integrating Psychological and Pharmacological Treatments for Addictive Disorders: An Evidence-Based Guide 32–53 (Routledge/Taylor & Francis Group, 2018).
Becoña, E. Brain disease or biopsychosocial model in addiction? Remembering the Vietnam Veteran Study. Psicothema 30, 270–275. https://doi.org/10.7334/psicothema2017.303 (2018).
Wangensteen, T. & Hystad, J. A comprehensive approach to understanding substance use disorder and recovery: Former patients’ experiences and reflections on the recovery process four years after discharge from SUD treatment. J. Psychosoc. Rehabil. Ment. Health. 9, 45–54. https://doi.org/10.1007/s40737-021-00233-9 (2022).
Degenhardt, L. et al. Buprenorphine versus methadone for the treatment of opioid dependence: A systematic review and meta-analysis of randomised and observational studies. Lancet Psychiatry 10, 386–402. https://doi.org/10.1016/S2215-0366(23)00095-0 (2023).
Mello, N. K. & Mendelson, J. H. Behavioral pharmacology of buprenorphine. Drug. Alcohol. Depend. 14, 283–303. https://doi.org/10.1016/0376-8716(85)90062-6 (1985).
Sivils, A., Lyell, P., Wang, J. Q. & Chu, X. P. Suboxone: History, controversy, and open questions. Front. Psychiatry 13, 1046648. https://doi.org/10.3389/fpsyt.2022.1046648 (2022).
Piske, M. et al. Comparative effectiveness of buprenorphine-naloxone versus methadone for treatment of opioid use disorder: A population-based observational study protocol in British Columbia, Canada. BMJ Open 10, e036102. https://doi.org/10.1136/bmjopen-2019-036102 (2020).
Lim, J., Farhat, I., Douros, A. & Panagiotoglou, D. Relative effectiveness of medications for opioid-related disorders: A systematic review and network meta-analysis of randomized controlled trials. PLoS ONE 17, e0266142. https://doi.org/10.1371/journal.pone.0266142 (2022).
Yarborough, B. J. et al. Methadone, buprenorphine and preferences for opioid agonist treatment: A qualitative analysis. Drug Alcohol. Depend. 160, 112–118. https://doi.org/10.1016/j.drugalcdep.2015.12.031 (2016).
Garcia-Portilla, M. P., Bobes-Bascaran, M. T., Bascaran, M. T., Saiz, P. A. & Bobes, J. Long term outcomes of pharmacological treatments for opioid dependence: Does methadone still lead the pack?. Br. J. Clin. Pharmacol. 77, 272–284. https://doi.org/10.1111/bcp.12031 (2014).
Reist, C. et al. Collaborative mental health care: A narrative review. Medicine 101, e32554. https://doi.org/10.1097/MD.0000000000032554 (2022).
Russo, S. et al. Understanding patients’ preferences: A systematic review of psychological instruments used in patients’ preference and studies. ISPOR 22, 491–501. https://doi.org/10.1016/j.jval.2018.12.007 (2019).
Law, E. H., Jiang, R., Kaczynski, A., Mühlbacher, A. & Pickard, A. S. The role of personality in treatment-related outcome preferences among pharmacy students. Am. J. Pharm. Educ. 83, 6891. https://doi.org/10.5688/ajpe6891 (2019).
Zilberman, N., Yadid, G., Efrati, Y., Neumark, Y. & Rassovsky, Y. Personality profiles of substance and behavioral addictions. Addict. Behav. 82, 174–181. https://doi.org/10.1016/j.addbeh.2018.03.007 (2018).
Chen, F., Yang, H., Bulut, O., Cui, Y. & Xin, T. Examining the relation of personality factors to substance use disorder by explanatory item response modeling of DSM-5 symptoms. PLoS ONE 14, e0217630. https://doi.org/10.1371/journal.pone.0217630 (2019).
Fehrman, E. et al. Drug use and personality profiles. In Personality Traits and Drug Consumption (Springer, 2019).
Terracciano, A., Löckenhoff, C. E., Crum, R. M., Bienvenu, O. J. & Costa, P. T. Five-Factor Model personality profiles of drug users. BMC Psychiatry 8, 22. https://doi.org/10.1186/1471-244X-8-22 (2008).
Christi, D. M. The Big Five Inventory, Substance Abuse History, and Academic Success Among Students Majoring in Substance Abuse Counseling. [Dissertation]. (St. Mary’s University, 2019).
Dash, G. F., Martin, N. G. & Slutske, W. S. Big Five personality traits and illicit drug use: Specificity in trait–drug associations. Psychol. Addict. Behav. 37, 318–330. https://doi.org/10.1037/adb0000793 (2023).
Adams, G. C., McWilliams, L. A., Wrath, A. J., Adams, S. & Souza, D. Relationships between patients’ attachment characteristics and views and use of psychiatric treatment. Psychiatry Res. 256, 194–201. https://doi.org/10.1016/j.psychres.2017.06.050 (2017).
Mikulincer, M. & Shaver, P. R. An attachment perspective on psychopathology. World Psychiatry 11, 11–15. https://doi.org/10.1016/j.wpsyc.2012.01.003 (2012).
Maunder, R. G. & Hunter, J. J. Can patients be “attached” to healthcare providers? An observational study to measure attachment phenomena in patient-provider relationships. BMJ Open 6, e011068. https://doi.org/10.1136/bmjopen-2016-011068 (2016).
Rübig, L. L. et al. Attachment and therapeutic alliance in substance use disorders: Initial findings for treatment in the therapeutic community. Front. Psychiatry 12, 730876. https://doi.org/10.3389/fpsyt.2021.730876 (2021).
Alvarez-Monjaras, M., Mayes, L. C., Potenza, M. N. & Rutherford, H. J. A developmental model of addictions: Integrating neurobiological and psychodynamic theories through the lens of attachment. Attach. Hum. Dev. 21, 616–637. https://doi.org/10.1080/14616734.2018.1498113 (2019).
Fairbairn, C. E. et al. A meta-analysis of longitudinal associations between substance use and interpersonal attachment security. Psychol. Bull. 144, 532–555. https://doi.org/10.1037/bul0000141 (2018).
Schindler, A. Attachment and substance use disorders-theoretical mmodels, empirical evidence, and implications for treatment. Front. Psychiatry 10, 727. https://doi.org/10.3389/fpsyt.2019.00727 (2019).
Mielau, J., Vogel, M., Gutwinski, S. & Mick, I. New approaches in drug dependence: Opioids. Curr. Addicti. Rep. 8, 298–305. https://doi.org/10.1007/s40429-021-00373-9 (2021).
Sud, A. et al. Beyond harm-producing versus harm-reducing: A qualitative meta-synthesis of people who use drugs’ perspectives of and experiences with the extramedical use and diversion of buprenorphine. J. Subst. Abuse Treat. 135, 108651. https://doi.org/10.1016/j.jsat.2021.108651 (2022).
Petronzi, G. J. & Masciale, J. N. Using personality traits and attachment styles to predict people’s preference of psychotherapeutic orientation. Couns. Psychother. Res. 15, 298–308. https://doi.org/10.1002/capr.12036 (2015).
Portilla, M. P. G., Bascaran, M. T. B., Bascaran, M. T., Saiz, P. A. & Bobes, J. Long term outcomes of pharmacological treatments for opioid dependence: Does methadone still lead the pack?. Br. J. Clin. Pharmacol. 77, 272–284 (2014).
Windle, E. et al. Association of patient treatment preference with dropout and clinical outcomes in adult psychosocial mental health Interventions: A systematic review and meta-analysis. JAMA Psychiatry 77, 294–302. https://doi.org/10.1001/jamapsychiatry.2019.3750 (2020).
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders 5th edn. (American Psychiatric Publishing, 2013).
Caprara, G. V., Barbaranelli, C., Borgogni, L. & Perugini, M. The, “big five questionnaire”: A new questionnaire to assess the five-factor model. Pers. Individ. Differ. 15, 281–288. https://doi.org/10.1016/0191-8869(93)90218-r (1993).
Kamenov, Ž & Jelić, M. Validation of adult attachment measures in various types of close relationships: Modification of Brennan’s experiences in close relationship inventory. Suv Psihol. 6, 73–91 (2003).
Cohen, J. A power primer. Psychol. Bull. 112, 155–159. https://doi.org/10.1037/00332909.112.1.155 (1992).
Brennan, K. A., Clark, C. L. & Shaver, P. R. Self-report measurement of adult attachment: An integrative overview. In Attachment theory and close relationships (eds Simpson, J. A. & Rholes, W. S.) 46–76 (The Guilford Press, 1998).
Kornør, H. & Nordvik, H. Five-factor model personality traits in opioid dependence. BMC Psychiatry https://doi.org/10.1186/1471-244x-7-37108 (2007).
Malouff, J. M., Thorsteinsson, E. B., Rooke, S. E. & Schutte, N. S. Alcohol involvement and the Five-Factor Model of personality: A meta-analysis. J. Drug Educ. 37, 277–294. https://doi.org/10.2190/de.37.3.d (2007).
Dubey, C., Arora, M., Gupta, S. & Kumar, B. Five factor correlates: A comparison of substance abusers and non-substance abusers. JIAAP 36, 107–114 (2010).
Terracciano, A., Löckenhoff, C. E., Crum, R. M., Bienvenu, O. J. & Costa, P. T. Five-factor model personality profiles of drug users. BMC Psychiatry 8, 22 (2008).
Rothman, R. An open-label study of a functional opioid κ antagonist in the treatment of opioid dependence. J. Subst. Abuse. Treat. 18, 277–281. https://doi.org/10.1016/s0740-5472(99)00074-4 (2000).
Whelan, P. J. & Remski, K. Buprenorphine vs methadone treatment: A review of evidence in both developed and developing worlds. JNRP 3, 45–50. https://doi.org/10.4103/0976-3147.91934 (2012).
Platts, H., Tyson, M. & Mason, O. Adult attachment style and core beliefs: Are they linked?. Clin. Psychol. Psychother. 9, 332–348. https://doi.org/10.1002/cpp.345 (2002).
Borhani, Y. Substance abuse and insecure attachment styles: A relational study. Lux 2, 1–13. https://doi.org/10.5642/lux.201301.04 (2013).
Schindler, A., Thomasius, R., Petersen, K. & Sack, P. M. Heroin as an attachment substitute? Differences in attachment representations between opioid, ecstasy and cannabis abusers. Attach. Hum. Dev. 11, 307–330. https://doi.org/10.1080/14616730902815009 (2009).
Thorberg, F. A. & Lyvers, M. Attachment, fear of intimacy and differentiation of self among clients in substance disorder treatment facilities. Addict. Behav. 31, 732–737. https://doi.org/10.1016/j.addbeh.2005.05.050 (2006).
Kriegler, J. et al. Decision making of individuals with heroin addiction receiving opioid maintenance treatment compared to early abstinent users. Drug Alcohol Depend. 205, 107593. https://doi.org/10.1016/j.drugalcdep.2019.107593 (2019).
Acknowledgements
We are grateful to prof. Dolores Britvić for the supervision and support of the research study.
Author information
Authors and Affiliations
Contributions
A.G.: formal analyses, writing-original draft, review and editing, visualization; V.A.: approved final draft, statistical consultation; I.B.G.: conceptualization and methodology, supervision, resources, data curation, investigation, project administration, writing-original draft, review and editing, approved final draft. All authors approved the submission of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gizdic, A., Antičević, V. & Brajević-Gizdić, I. The role of attachment and personality traits in choosing opiate addiction replacement therapy. Sci Rep 14, 14623 (2024). https://doi.org/10.1038/s41598-024-65695-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-65695-w
- Springer Nature Limited