Abstract
In breast cancer radiation therapy, minimizing radiation-related risks and toxicity is vital for improving life expectancy. Tailoring radiotherapy techniques and treatment positions can reduce radiation doses to normal organs and mitigate treatment-related toxicity. This study entailed a dosimetric comparison of six different external beam whole-breast irradiation techniques in both supine and prone positions. We selected fourteen breast cancer patients, generating six treatment plans in both positions per patient. We assessed target coverage and organs at risk (OAR) doses to evaluate the impact of treatment techniques and positions. Excess absolute risk was calculated to estimate potential secondary cancer risk in the contralateral breast, ipsilateral lung, and contralateral lung. Additionally, we analyzed the distance between the target volume and OARs (heart and ipsilateral lung) while considering the treatment position. The results indicate that prone positioning lowers lung exposure in X-ray radiotherapy. However, particle beam therapies (PBTs) significantly reduce the dose to the heart and ipsilateral lung regardless of the patient’s position. Notably, negligible differences were observed between arc-delivery and static-delivery PBTs in terms of target conformity and OAR sparing. This study provides critical dosimetric evidence to facilitate informed decision-making regarding treatment techniques and positions.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Introduction
Breast cancer is the most frequently diagnosed malignancy and a leading cause of mortality among women1,2. Modern multidisciplinary treatment strategies, encompassing surgical resection, postoperative radiation, and preoperative or postoperative systemic therapy, have significantly enhanced the long-term survival prospects of breast cancer patients3. Notably, radiation therapy following breast-conserving surgery has exhibited outcomes on par with mastectomy4,5, especially for early-stage cases; this has led to an increased emphasis on improving patients’ long-term quality of life while minimizing radiation-induced malignancy.
The primary side effects of concern in breast cancer radiotherapy patients are radiogenic heart and lung damage6,7,8,9,10,11. A study by Darby et al. reported a linear increase of 7.4% per Gray (Gy) in the rate of major coronary events concerning the mean heart dose7. Furthermore, the reduction of the dose on the left anterior descending (LAD) artery has been shown to decrease the risk of radiation-induced stenosis in the heart12. Research has revealed that specific regions of the heart, including the heart apex or portions of the LAD artery, may receive high doses (up to 47.2 Gy) despite a low mean heart dose (below 3 Gy)13. Additionally, the risk of secondary cancer, often arising from irradiation of the contralateral breast or lungs, is a critical consideration14,15. For patients who survive beyond five years, breast cancer radiation therapy has been associated with a 14% increase in contralateral breast cancer risk, with younger patients and longer latency periods posing a higher risk15,16,17.
The clinical application of breast cancer radiation therapy has evolved from early three-dimensional conformal radiation therapy (3DCRT) to more precise techniques such as intensity-modulated radiotherapy and volumetric-modulated arc therapy (VMAT)18,19,20. Proton and carbon-ion radiation therapy (CIRT) has emerged as techniques that minimize dose deposition outside the clinical target volume (CTV)21,22. Additionally, the research on arc-delivery particle beam therapy (arc-delivery PBT), which holds promise for providing enhanced robustness, has been documented23,24. Studies have examined dosimetric variations among different treatment techniques to mitigate long-term radiation side effects in breast cancer radiation therapy and have assessed the effects of CTV size, organs at risk (OARs), target distances, treatment positions, and other factors on treatment planning25,26,27,28,29,30,31,32. However, there has been limited focus on arc-delivery PBT, including CIRT.
The current study aims to identify the optimal modality by comparing the dose characteristics of six external beam whole-breast irradiation techniques: 3DCRT, VMAT, intensity-modulated proton therapy (IMPT), proton arc therapy (PAT), intensity-modulated carbon-ion therapy (IMCT), and carbon arc therapy (CAT). We investigate the impact of treatment position, breast size, and the heart’s proximity to the breast on dose characteristics and the risks associated with secondary cancer.
Materials and methods
Patient selection and computed tomography (CT) simulation
We prospectively enrolled fourteen breast cancer patients, evenly divided between left-sided and right-sided cases, who had undergone adjuvant whole-breast irradiation with free breathing. This study was approved by the institutional review board of the Kyung Hee University Hospital at Gangdong (KHNMC 2017-02-004), and all procedures were performed in accordance with the relevant guidelines and regulations. Written informed consent was obtained from all patients. While the standard patient position for breast cancer CT scans at the hospital in the present study was supine, we performed non-contrast CT scans in both supine and prone positions with the arms raised to gather additional information for effective radiotherapy planning. In the prone position, the contralateral breast was gently moved aside, away from the ipsilateral breast. The CT simulator (Brilliance 64, Philips Medical Systems, The Netherlands) utilized for planning CT scans featured a 3-mm slice thickness, and the resulting image set was imported into the RayStation (RaySearch Laboratories AB, Stockholm, Sweden) treatment planning system (TPS).
Planning parameters
The planning target volume (PTV) was defined as the breast contours with a 5-mm margin subtracted from the skin. Ipsilateral and contralateral lungs, the heart, and the contralateral breast were outlined as OARs. The prescribed dose was 50.4 Gy delivered in 28 fractions, covering 95% of the PTV. In the supine and prone positions, the PTV sizes ranged between 161–890 cc and 172–1156 cc, respectively. All plans were optimized to ensure target coverage and adhere to OAR dose constraints. For PTV, we required that 100% of the prescription doses cover over 95% of the PTVs, with the maximum dose limited to less than 110%. Regarding the ipsilateral lung, the V20Gy and V10Gy were kept below 10% and 20%, respectively, while the maximum point dose to the spinal cord was capped at 45 Gy. The maximum point dose to the heart was constrained to less than 7.5 Gy, and to mitigate the risk of secondary cancer, the volume of the heart receiving 1.0 Gy was limited to below 0.5%. Similarly, to reduce secondary cancer risks, the maximum point dose to the contralateral breast was restricted to less than 0.5 Gy. The maximum point dose was capped at less than 51.5 Gy for the ipsilateral chest wall, and for the contralateral chest wall, it was limited to less than 1.0 Gy. For robust optimization in particle beam therapy planning, the isotropic universal position uncertainty and range uncertainty were set at 5 mm and 3.5%, respectively, within RayStation TPS33,34. In CIRT planning, the relative radiobiological effectiveness (RBE) dose was computed using the modified microdosimetric kinetic model35,36,37.
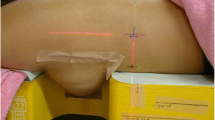
The 3DCRT plans utilized two tangential fields, while the VMAT plans comprised two arcs. Each collimator angle was chosen to provide additional degrees of freedom, enhancing the plan's quality. X-ray radiotherapy (XRT) treatment was implemented using the 6 MV photon beam from Electa VERSA-HD (Electa AB, Stockholm, Sweden) linear accelerator equipped with an Agility 160 multileaf collimator. Static-field particle beam therapy (static-field PBT) plans involved three field beams. In the supine position, the gantry angles for static-field PBT were 330°, 30°, and 90° for the left breast and 270°, 330°, and 30° for the right breast. In the prone position, these angles were 150°, 190°, and 240° for the left breast and 110°, 180°, and 220° for the right breast. The gantry angles for arc-delivery PBT ranged between 320°–110° and 50°–270° for the left breast and between 250°–40° and 100°–220° for the right breast in the supine and prone positions, respectively. As RayStation TPS (v10A) does not support arc-delivery PBT planning, we conducted simulations by arranging 13 to 16 beams consecutively at 10° intervals. The spot spacing ranged from 0.5 to 1.5 cm for the proton beam and 0.25 to 0.5 cm for the carbon-ion beam. Figure 1 illustrates the dose distributions for the six different external beam whole-breast irradiation plans in both supine and prone positions.
Comparison of dose characteristics based on dose-volume histograms (DVHs)
We employed DVHs, isodose distributions, and dosimetric indices for the lung, heart, LAD, contralateral breast, and skin to assess the quality of the treatment plans. The radiotherapy plans were evaluated with respect to the Homogeneity Index (HI) and Paddick Conformity Index (PCI) of the PTV38. HI provides insight into dose uniformity and is defined as HI = (|D2 − D98|/Rx) × 100, where D2 and D98 represent the doses received at 2% and 98% of the PTV, respectively, and Rx is the prescription dose39. Conversely, PCI describes dose conformity and is defined as PCI = (V95PTV × V95PTV)/(VPTV × V95), where V95PTV and V95 denote the volumes receiving a dose greater than 95% of the Rx within the PTV and the entire body, respectively40. Furthermore, we compared the mean lung dose and V20Gy to assess the risk of pneumonitis. We compared the mean heart dose and the maximum LAD dose to evaluate the probability of radiation-induced side effects, such as cardiovascular risk. Furthermore, we estimated and compared the mean contralateral breast dose and D2 at the skin.
Distance between target and OARs (lung and heart) considering treatment position
We examined the geometric variances in the supine and prone positions concerning the target and OARs. In particular, we assessed changes in the PTV volume and the minimum distance (the shortest distance from the PTV surface to the ipsilateral lung or heart) between the target and OARs based on the treatment position.
Secondary cancer risk estimates
The report on the Biological Effects of Ionizing Radiation (BEIR VII)41,42 with Schneider’s OED concept, which included the impact of fractionation and incorporated a repair and population parameter quantified excess absolute risk (EAR) for an individual exposed to radiation at a dose (D) at age (e) using the following formula:
where OED is the organ equivalent dose, β` represents the initial slope of the dose–response curve relationship of secondary cancer induction, agea is the attained age from the exposed age agex, and γe and γa denote age-modifying factors. All parameters utilized for calculating Excess Absolute Risks (EARs) were sourced from Schneider's work42. The initial computation of EARs was conducted for patients based on their actual ages of irradiation, under the presumption that they would live to be 70 years old. To mitigate the influence of varying irradiation ages on EAR findings, a standardization process was implemented by recalculating EARs for a specific cohort. This cohort consisted of individuals irradiated at the age of 30, with projections indicating they would achieve an age of 70. This adjustment allows for a more consistent comparison of EARs across different patient groups.
Organ equivalent dose (OED) was used to calculate EAR, utilizing a plateau dose–response model for estimating the OED of the contralateral breast as follows:
Upon the refinement of the plateau model, coupled with the consideration of the number of fractions in fractionated therapy, the OED for an organ, as per the full mechanistic model, was determined as follows:
where V represents the total volume of the organ at risk (including contralateral breast, ipsilateral lung, and contralateral lung) and Vi denotes a specific volume element that is subjected to an exposed dose element Di42,43. For the full mechanistic model, the parameter δ was determined to be 0.044 Gy−1 with R equaling 0.15 for the female breast, and δ is 0.042 Gy−1 with R set at 0.83 for the lung. These parameters were derived from a combined fit to the data from atomic bomb survivors and Hodgkin’s disease patients treated with single doses ranging from 2 to 40 Gy assuming an alpha/beta (α/β) value of 3 Gy.
Statistical analysis
To compare the dosimetric parameters and geometric distances for these treatment plans, we conducted paired two-tailed t-tests, with Bonferroni correction applied (utilizing SPSS, v26, Chicago, USA). The data were presented as mean values with standard deviations, and statistical significance was considered at p < 0.05.
Results
A total of 168 treatment plans from 14 patients were evaluated in this study. Figure 1 illustrates an example of axial CT images with dose distributions in the supine and prone positions of a patient for six treatment techniques. The dosimetric results of PTV and OARs for the treatment techniques are presented in Supplementary Table S1.
Dosimetric comparison of treatment techniques
Figure 2 displays the mean target coverage and differences in OAR doses among 14 patients for the six techniques. VMAT exhibited superior PCI coverage, albeit it recorded the highest mean dose to the contralateral breast. Notably, statistically significant reductions in mean heart dose, mean lung dose, and mean contralateral breast dose were observed with PBT compared to XRT (p < 0.05). However, a proclivity toward higher skin dose was noted in the case of PBT. Among the PBT techniques, proton therapy, encompassing IMPT and PAT, offered a lower mean heart dose compared to CIRT, which comprises IMCT and conventional active scanning CAT. Nevertheless, it is crucial to highlight that the average mean heart dose for all techniques remained below 0.5 Gy (RBE). Arc-delivery PBT yielded no benefits in terms of OARs sparing for the heart, ipsilateral lung, and contralateral breast compared to static-field PBT, and the target conformity was inferior (p < 0.05).
Dosimetric comparisons between supine and prone positions
Figure 3 illustrates the mean differences in dosimetric parameters for PTV and OARs between the supine and prone positions. In the prone position, the PTV's PCI surpassed that in the supine position for all treatment techniques. However, statistical significance was only observed in the case of XRT and proton therapy. Conversely, the supine position resulted in a statistically significant reduction in the mean heart dose for most treatment techniques. Furthermore, in the context of XRT, the prone position led to decreased mean lung dose and V20 values for the ipsilateral lung. In contrast, for PBT, these values remained minimal, regardless of the patient's position.
Distance between target and OARs (lung and heart) considering treatment position
The difference in geometric distances between the PTV and OARs, specifically the lung and heart, depending on the patient's treatment position, are depicted in Fig. 4 and summarized in Supplementary Table S2. In terms of the separation between the PTV and OARs, it was observed that the supine position led to a more substantial separation effect for the heart, while the prone position allowed the ipsilateral lung to separate more from the PTV as compared to the supine position (p < 0.05).
Differences in the PTV volume and separation distance between the supine and prone positions. Separation distance was defined as the shortest three-dimensional distance from the 3D contours of PTV and OARs. Red circle and blue triangle marks represent the left- and right-sided breast cancer patients, respectively. Light orange and light green shaded areas correspond to PTV volume and separation distance of OARs from PTV, respectively.
Estimation of secondary cancer risk
Figure 5 illustrates the differences in the mean EAR for the contralateral breast, ipsilateral lung, and contralateral lung in the supine and prone positions. VMAT yielded the highest mean EAR estimate, followed by 3DCRT. Statistically, the mean EARs in PBT were significantly lower than those for XRT. No statistical significance was found between static-field PBT and arc-delivery PBT. Furthermore, in the supine position, proton therapy better reduced the mean EAR than CIRT (Supplementary Table S3).
Discussion
Advanced treatment techniques such as PBT and the use of prone positions can effectively reduce the radiation doses delivered to adjacent OARs while maintaining the same level of disease control in breast cancer patients. To support clinical decision-making, we conducted a thorough analysis of the dosimetric evidence that underlies the potential advantages of radiotherapy. We also evaluated the dosimetric efficacy of these techniques based on treatment positions.
PBT significantly lowered the mean heart dose, mean lung dose, and mean contralateral breast dose compared to XRT. This outcome is attributed to the excellent depth-dose distributions of PBT, allowing for a substantial reduction in OAR doses while preserving target coverage. Prior research has consistently reported that proton therapy offers significant advantages in sparing the heart and lungs compared to XRT25,26,27,28. Ischemic heart disease can persist for up to 20 years after radiation exposure, and there is a proportional increase in coronary events with the mean dose to the heart, without a clear cutoff value. Therefore, to reduce the incidence of coronary events, minimizing the mean heart dose to the greatest extent possible is crucial7. Vega et al. suggested proton therapy as a cost-effective measure for patients with cardiac risk factors for mean heart dose ≥ 5 Gy44. A recent study has established a direct correlation between low-dose radiation (specifically, V5) and the occurrence of acute coronary events. Thus, the increase in heart volume exposed to radiation should be reduced45. Notably, our study revealed that the mean heart dose in PBT was consistently less than 0.5 Gy (RBE), indicating its potential to mitigate radiation-related cardiac morbidity. The use of CIRT breast cancer treatment has been primarily limited due to the scarcity of facilities offering this treatment and the associated high costs46. Moreover, the eligibility criteria for CIRT generally target low-risk stage I breast cancer cases, which are typically amenable to partial breast irradiation47,48. This study represents the first comparative dosimetric analysis of CIRT in the context of whole-breast irradiation. Interestingly, our results showed similarities between CIRT and proton therapy in terms of sparing OARs. Consequently, CIRT may present an attractive option for treating patients with a high locoregional recurrence rate or unresected nodal disease in specific areas such as the supraclavicular fossa or internal mammary nodes21. However, further clinical investigations are needed to fully understand the role of CIRT in various treatment settings, including whole-breast irradiation.
This study compared static and arc delivery in XRT and PBT to evaluate the dosimetric effects of beam delivery methods. In XRT, VMAT demonstrated superior target dose conformity when compared to 3DCRT. However, VMAT resulted in higher mean doses and elevated secondary cancer risk for the contralateral breast (as indicated in Figs. 3 and 5). In general, VMAT can reduce the dose to the heart and ipsilateral lung while delivering a more uniform dose distribution to the target compared to 3DCRT. However, VMAT produces higher mean and low-dose volumes in OARs49,50,51,52. Arc-delivery PBT offers several benefits, including reduced calculation complexity and uncertainties, as well as optimization of high linear energy transfer deposition in tissues53. Arc-delivery PBT can be more robust than static-field PBT as range uncertainty is spread between different beam angles, and the RBE is increased within the target53,54,55,56. This approach has gained attention primarily due to the utilization of rotating gantries and spot-scanning techniques54. In particular, spot-scanning proton arc (SPArc) can provide better target coverage and a significantly lower dose of OARs across various sites in comparison to IMPT54,55. Notably, a study by Chang et al. underscored that SPArc could achieve superior OAR sparing and ensure robust plan quality, particularly in the context of left-sided WBRT compared to IMPT24. However, the results of our study did not indicate any discernible benefits of arc-delivery PBT for both proton therapy and CIRT. This discrepancy can be attributed to several methodological distinctions between the two studies. First, our study employed three beam angles for IMPT and 13–16 beam angles for arc therapy, whereas the study by Chang et al. utilized one beam for IMPT and 39 beams for SPArc24. Increasing the number of beams can potentially improve the dose gradient57. Another difference is that arc-delivery PBT in our study was generated by combining multiple fixed-angle beam. Conversely, SPArc was based on an algorithm that optimized the number of arc control points and energy layers delivered from each angle53. Dynamic arc delivery, such as SPArc, where the gantry rotates dynamically during dose delivery, can improve dosimetric quality compared to multiple fixed-angle beam delivery. Dynamic arc therapy uses hundreds of beam angles with an energy layer selection algorithm to optimize the RBE inside the target volume, thereby increasing the biological effectiveness of particle therapy. This method offers additional degrees of freedom in optimization and delivery, potentially streamlining the treatment process with a single arc trajectory24. However, current limitations in hardware, beam control systems, and treatment planning systems restrict the clinical and practical application of dynamic particle arc therapy. Consequently, the multiple fixed-angle beam delivery used in this study serves as an alternative feasible technique but should not be equated with dynamic arc delivery. Therefore, caution is necessary when interpreting the results of this study using multiple fixed-angle particle beams in terms of dynamic arc delivery. Further research is required to compare multiple fixed-angle beam delivery with dynamic arc delivery planning and better understand the clinical significance and application of arc-delivery PBT.
The results of existing studies on the prone position are heterogeneous, primarily focusing on patients with larger breast volumes40,58,59,60,61,62. Improvements in cardiac dosimetry in the prone position are closely related to breast volume and were particularly effective in reducing cardiac dose in patients with breast volumes exceeding 750 or 1000 cm363,64. The results of our study in XRT were consistent with previous research. The mean breast volume in the patient's prone position was 571.43 ± 294.78 cm3, and no significant improvement in cardiac dose was observed for the prone position. However, the prone position in XRT has been confirmed to reduce lung dose (as depicted in Fig. 3). The prone position can significantly reduce radiation exposure to the ipsilateral lung58,60,61,64,65, and may alleviate acute and late pulmonary toxicity64,66. A novelty of this study was the measurement of the shortest distances between the 3D contours of the PTV and OARs for highly conformal RT-suitable analyses such as VMAT. Consequently, we observed that the heart and ipsilateral lungs were positioned farther from the PTV in the supine and prone positions, respectively (as illustrated in Fig. 4). These findings resulted in dosimetric benefits attributed to the chosen treatment position in XRT (as shown in Fig. 6). Our study found that PBT consistently reduced doses to OARs regardless of treatment position. However, the prone position presents challenges such as decreased setup accuracy and larger inter-fractional motion compared to the supine position52,59,67. Considering the complexities and learning curves associated with prone radiotherapy, the supine position may be a more practical choice for PBT. Dosimetric improvements due to treatment position can vary depending on the treatment technique. While treatment position can influence dosimetric outcomes, patient characteristics such as breast size can also impact the consistency of patient positioning (setup reproducibility). This highlights the importance of tailoring treatment position selection to individual patients and the specific treatment technique being used.
Investigating secondary cancer risk in breast cancer patients is necessary in terms of improving long-term quality of life. In this study, VMAT demonstrated the highest EAR estimate, and PBT showed a significantly lower EAR compared to XRT (Supplementary Table S3). Furthermore, we compared proton therapy and CIRT in the context of whole-breast irradiation, with proton therapy yielding a smaller risk estimate compared to CIRT. This study is the first to analyze secondary cancer risk in CIRT for whole-breast irradiation, although the contribution of neutrons to the total dose was not included. In addition, the impact of the variable RBE on secondary cancer risk was not considered in the current model. Consequently, generalizing the results of this study may be challenging due to inherent biological uncertainties, model limitations in accounting for RBE in tumor initiation, and the presence of significant inter-patient variation68,69. Nevertheless, these findings are expected to provide valuable insights for clinicians and patients in their decision-making processes, particularly in the context of reducing the secondary cancer risk when considering PBT.
This study has several limitations. First, the study involved a relatively small number of patients from a single institution, which restricts the generalizability of the findings. In addition, our study did not investigate Intensity-modulated radiation therapy and various 3DCRT techniques. Further studies with a larger patient cohort are required to validate and expand upon the results. Second, although many factors affect radiotherapy's therapeutic effect, the experimental design of our study is limited. Recently, the application of the prone position and advanced treatment techniques has been increasing in regional nodal irradiation to protect normal tissues70,71. However, our study did not investigate regional nodal irradiation or simultaneously integrated boost techniques. Furthermore, various hypofractionated approaches were also not considered. In addition to considering treatment techniques and patient position, cost-efficient aspects such as overall treatment time may also be essential for clinical decisions. Third, the robustness of treatment plans and the potential impact of patient respiratory motion on beam delivery were not assessed in this study. Despite the documented dosimetric benefits of PBT, concerns about plan robustness in the face of treatment uncertainties could pose challenges to its clinical adoption. PBT may be more susceptible to patient movements, including respiratory motion. Further investigations are therefore necessary to understand the robustness of treatment techniques and positions in the context of anatomical variations, such as breathing motion or breast swelling. Fourth, this study did not consider respiration-guided techniques, including deep inspiration breath hold (DIBH), which have been shown to effectively reduce heart doses58,59,61. DIBH suggests a measurable improvement in the dosimetric outcomes of conventional approaches. However, it is important to consider that DIBH procedures generally require more treatment time than free-breathing radiotherapy72. Our study demonstrated that PBT achieved a mean heart dose of less than 0.5 Gy, indicating that PBT in free breathing could be a valuable technique for cardiac sparing in appropriately selected patients. Lastly, differences in dose calculation algorithms between photon and proton plans may have introduced bias into our results. In addition, potential variations in RBE could impact the robustness of our findings. Therefore, cautious interpretation of these results is warranted.
Conclusions
To extend the life expectancy of breast cancer patients, radiation oncologists must prioritize the mitigation of radiation toxicity risks. Thoughtful consideration of radiation techniques and treatment positions can lead to reduced OAR doses and an enhancement in the management of treatment-related toxicity. The choice of the ideal radiotherapy technique for breast cancer should be personalized, considering both patient-specific characteristics and cost-effectiveness. This study provides crucial dosimetric insights that can significantly inform the decision-making process concerning treatment techniques and positions.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
Lei, S. et al. Global patterns of breast cancer incidence and mortality: A population-based cancer registry data analysis from 2000 to 2020. Cancer Commun. 41, 1183–1194 (2021).
Soerjomataram, I. & Bray, F. Planning for tomorrow: Global cancer incidence and the role of prevention 2020–2070. Nat. Rev. Clin. Oncol. 18, 663–672 (2021).
Bray, F. et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 68, 394–424 (2018).
Fisher, B. et al. Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer. N. Engl. J. Med. 347, 1233–1241 (2002).
Early Breast Cancer Trialists’ Collaborative Group et al. Effect of radiotherapy after breast-conserving surgery on 10-year recurrence and 15-year breast cancer death: Meta-analysis of individual patient data for 10,801 women in 17 randomised trials. Lancet 378, 1707–1716 (2011).
Aznar, M. C., Duane, F. K., Darby, S. C., Wang, Z. & Taylor, C. W. Exposure of the lungs in breast cancer radiotherapy: A systematic review of lung doses published 2010–2015. Radiother. Oncol. 126, 148–154 (2018).
Darby, S. C. et al. Risk of ischemic heart disease in women after radiotherapy for breast cancer. N. Engl. J. Med. 368, 987–998 (2013).
Darby, S. C., McGale, P., Taylor, C. W. & Peto, R. Long-term mortality from heart disease and lung cancer after radiotherapy for early breast cancer: Prospective cohort study of about 300,000 women in US SEER cancer registries. Lancet Oncol. 6, 557–565 (2005).
Sato, H. et al. Incidence of organizing pneumonia after whole-breast radiotherapy for breast cancer, and risk factor analysis. J. Radiat. Res. 59, 298–302 (2018).
Taylor, C. et al. Estimating the risks of breast cancer radiotherapy: Evidence from modern radiation doses to the lungs and heart and from previous randomized trials. J. Clin. Oncol. 35, 1641–1649 (2017).
Taylor, C. et al. Cardiac structure injury after radiotherapy for breast cancer: Cross-sectional study with individual patient data. J. Clin. Oncol. 36, 2288–2296 (2018).
Wennstig, A. K. et al. The relationship between radiation doses to coronary arteries and location of coronary stenosis requiring intervention in breast cancer survivors. Radiat. Oncol. 14, 40 (2019).
Piroth, M. D. et al. Heart toxicity from breast cancer radiotherapy: Current findings, assessment, and prevention. Strahlenther. Onkol. 195, 1–12 (2019).
Burt, L. M., Ying, J., Poppe, M. M., Suneja, G. & Gaffney, D. K. Risk of secondary malignancies after radiation therapy for breast cancer: Comprehensive results. Breast 35, 122–129 (2017).
Gao, X., Fisher, S. G. & Emami, B. Risk of second primary cancer in the contralateral breast in women treated for early-stage breast cancer: A population-based study. Int. J. Radiat. Oncol. Biol. Phys. 56, 1038–1045 (2003).
de Gonzalez, A. B. et al. Second solid cancers after radiotherapy for breast cancer in SEER cancer registries. Br. J. Cancer 102, 220–226 (2010).
Roychoudhuri, R., Evans, H., Robinson, D. & Moller, H. Radiation-induced malignancies following radiotherapy for breast cancer. Br. J. Cancer 91, 868–872 (2004).
Ahmad, I. et al. Plan quality assessment of modern radiotherapy delivery techniques in left-sided breast cancer: An analysis stratified by target delineation guidelines. BJR Open 2, 20200007 (2020).
Chen, S. N., Ramachandran, P. & Deb, P. Dosimetric comparative study of 3DCRT, IMRT, VMAT, Ecomp, and hybrid techniques for breast radiation therapy. Radiat. Oncol. J. 38, 270–281 (2020).
Chang, K. H. et al. A retrospective dosimetric analysis of the new ESTRO-ACROP target volume delineation guidelines for postmastectomy volumetric modulated arc therapy after implant-based immediate breast reconstruction. Front. Oncol. 10, 578921 (2020).
Malouff, T. D. et al. Carbon ion radiation therapy in breast cancer: A new frontier. Breast Cancer Res. Treat. 181, 291–296 (2020).
Mutter, R. W. et al. Proton therapy for breast cancer: A consensus statement from the particle therapy cooperative group breast cancer subcommittee. Int. J. Radiat. Oncol. Biol. Phys. 111, 337–359 (2021).
Ding, X. et al. Spot-scanning proton arc (SPArc) therapy: The first robust and delivery-efficient spot-scanning proton arc therapy. Int. J. Radiat. Oncol. Biol. Phys. 96, 1107–1116 (2016).
Chang, S. et al. Feasibility study: Spot-scanning proton arc therapy (SPArc) for left-sided whole breast radiotherapy. Radiat. Oncol. 15, 232 (2020).
Sun, T. et al. Heart and cardiac substructure dose sparing in synchronous bilateral breast radiotherapy: A dosimetric study of proton and photon radiation therapy. Front. Oncol. 9, 1456 (2019).
Stick, L. B. et al. Joint estimation of cardiac toxicity and recurrence risks after comprehensive nodal photon versus proton therapy for breast cancer. Int. J. Radiat. Oncol. Biol. Phys. 97, 754–761 (2017).
Ko, H. et al. Dosimetric comparison of radiation techniques for comprehensive regional nodal radiation therapy for left-sided breast cancer: A treatment planning study. Front. Oncol. 11, 645328 (2021).
Cunningham, L., Penfold, S., Giles, E., Le, H. & Short, M. Impact of breast size on dosimetric indices in proton versus X-ray radiotherapy for breast cancer. J. Pers. Med. 11, 282 (2021).
Speleers, B. A. et al. Comparison of supine or prone crawl photon or proton breast and regional lymph node radiation therapy including the internal mammary chain. Sci. Rep. 9, 4755 (2019).
Paganetti, H. et al. The risk for developing a secondary cancer after breast radiation therapy: Comparison of photon and proton techniques. Radiother. Oncol. 149, 212–218 (2020).
Zhang, Q. et al. Secondary cancer risk after radiation therapy for breast cancer with different radiotherapy techniques. Sci. Rep. 10, 1220 (2020).
Cartechini, G. et al. Proton pencil beam scanning reduces secondary cancer risk in breast cancer patients with internal mammary chain involvement compared to photon radiotherapy. Radiat. Oncol. 15, 228 (2020).
Unkelbach, J. et al. Robust radiotherapy planning. Phys. Med. Biol. 63, 2202 (2018).
Cubillos-Mesias, M. et al. Quantification of plan robustness against different uncertainty sources for classical and anatomical robust optimized treatment plans in head and neck cancer proton therapy. Br. J. Radiol. 93, 20190573 (2020).
Inaniwa, T. et al. Treatment planning for a scanned carbon beam with a modified microdosimetric kinetic model. Phys. Med. Biol. 55, 6721–6737 (2010).
Inaniwa, T. & Kanematsu, N. Adaptation of stochastic microdosimetric kinetic model for charged-particle therapy treatment planning. Phys. Med. Biol. 63, 095011 (2018).
Inaniwa, T. et al. Effects of dose-delivery time structure on biological effectiveness for therapeutic carbon-ion beams evaluated with microdosimetric kinetic model. Radiat. Res. 180, 44–59 (2013).
Feuvret, L., Noel, G., Mazeron, J. J. & Bey, P. Conformity index: A review. Int. J. Radiat. Oncol. Biol. Phys. 64, 333–342 (2006).
Wu, Q., Mohan, R., Morris, M., Lauve, A. & Schmidt-Ullrich, R. Simultaneous integrated boost intensity-modulated radiotherapy for locally advanced head-and-neck squamous cell carcinomas. I: Dosimetric results. Int. J. Radiat. Oncol. Biol. Phys. 56, 573–585 (2003).
Paddick, I. A simple scoring ratio to index the conformity of radiosurgical treatment plans: Technical note. J. Neurosurg. 93(Suppl 3), 219–222 (2000).
The 2007 Recommendations of the International Commission on Radiological Protection. ICRP publication 103. Ann ICRP 37, 1–332 (2007).
Schneider, U., Sumila, M. & Robotka, J. Site-specific dose-response relationships for cancer induction from the combined Japanese A-bomb and Hodgkin cohorts for doses relevant to radiotherapy. Theor. Biol. Med. Model 8, 27 (2011).
Schneider, U. & Kaser-Hotz, B. Radiation risk estimates after radiotherapy: Application of the organ equivalent dose concept to plateau dose-response relationships. Radiat. Environ. Biophys. 44, 235–239 (2005).
Mailhot Vega, R. B. et al. Establishing cost-effective allocation of proton therapy for breast irradiation. Int. J. Radiat. Oncol. Biol. Phys. 95, 11–18 (2016).
van den Bogaard, V. A. et al. Validation and modification of a prediction model for acute cardiac events in patients with breast cancer treated with radiotherapy based on three-dimensional dose distributions to cardiac substructures. J. Clin. Oncol. 35, 1171–1178 (2017).
Luo, W. et al. Particle therapy for breast cancer: Benefits and challenges. Front. Oncol. 11, 662826 (2021).
Karasawa, K. et al. A Phase I clinical trial of carbon ion radiotherapy for Stage I breast cancer: Clinical and pathological evaluation. J. Radiat. Res. 60, 342–347 (2019).
Karasawa, K. et al. A clinical study of curative partial breast irradiation for stage I breast cancer using carbon ion radiotherapy. Radiat. Oncol. 15, 265 (2020).
Bogue, J., Wan, J., Lavey, R. S. & Parsai, E. I. Dosimetric comparison of VMAT with integrated skin flash to 3D field-in-field tangents for left breast irradiation. J. Appl. Clin. Med. Phys. 20, 24–29 (2019).
Liu, Y. C., Chang, H. M., Lin, H. H., Lu, C. C. & Lai, L. H. Dosimetric comparison of intensity-modulated radiotherapy, volumetric modulated arc therapy and hybrid three-dimensional conformal radiotherapy/intensity-modulated radiotherapy techniques for right breast cancer. J. Clin. Med. 9, 3884 (2020).
Viren, T. et al. Tangential volumetric modulated arc therapy technique for left-sided breast cancer radiotherapy. Radiat. Oncol. 10, 79 (2015).
Mulliez, T. et al. Setup accuracy for prone and supine whole breast irradiation. Strahlenther. Onkol. 192, 254–259 (2016).
Mazal, A. et al. Biological and mechanical synergies to deal with proton therapy pitfalls: Minibeams, FLASH, arcs, and gantryless rooms. Front. Oncol. 10, 613669 (2020).
Zhou, Y., Li, Y., Kubota, Y., Sakai, M. & Ohno, T. Robust angle selection in particle therapy. Front. Oncol. 11, 715025 (2021).
Bertolet, A. & Carabe, A. Proton monoenergetic arc therapy (PMAT) to enhance LETd within the target. Phys. Med. Biol. 65, 165006 (2020).
Li, X. et al. Improve dosimetric outcome in stage III non-small-cell lung cancer treatment using spot-scanning proton arc (SPArc) therapy. Radiat. Oncol. 13, 35 (2018).
Toussaint, L. et al. Towards proton arc therapy: Physical and biologically equivalent doses with increasing number of beams in pediatric brain irradiation. Acta Oncol. 58, 1451–1456 (2019).
Lai, J. et al. Prone position versus supine position in postoperative radiotherapy for breast cancer: A meta-analysis. Medicine 100, e26000 (2021).
Kahan, Z. et al. A simple clinical method for predicting the benefit of prone vs supine positioning in reducing heart exposure during left breast radiotherapy. Radiother. Oncol. 126, 487–492 (2018).
Duma, M. N., Munch, S., Oechsner, M. & Combs, S. E. Heart-sparing radiotherapy in patients with breast cancer: What are the techniques used in the clinical routine?: A pattern of practice survey in the German-speaking countries. Med. Dosim. 42, 197–202 (2017).
Yu, T. et al. External-beam partial breast irradiation in a supine versus prone position after breast-conserving surgery for Chinese breast cancer patients. Sci. Rep. 8, 15354 (2018).
Kirby, A. M. et al. Prone versus supine positioning for whole and partial-breast radiotherapy: A comparison of non-target tissue dosimetry. Radiother. Oncol. 96, 178–184 (2010).
Bartlett, F. R. et al. The UK heart spare study (stage IB): Randomised comparison of a voluntary breath-hold technique and prone radiotherapy after breast conserving surgery. Radiother. Oncol. 114, 66–72 (2015).
Vakaet, V. et al. 5-year outcomes of a randomized trial comparing prone and supine whole breast irradiation in large-breasted women. Int. J. Radiat. Oncol. Biol. Phys. 110, 766–771 (2021).
Deseyne, P. et al. Whole breast and regional nodal irradiation in prone versus supine position in left sided breast cancer. Radiat. Oncol. 12, 89 (2017).
Budhi Singh Yadav, D. D., Thakur, N., Ghoshal, S., Sharma, R. & Singh, A. O. Dosimetric comparison of supine versus prone radiotherapy techniques in patients with breast cancer. J. Radiat. Oncol. 9, 6 (2020).
Chung, Y., Yu, J. I., Park, W. & Choi, D. H. Korean first prospective phase II study, feasibility of prone position in postoperative whole breast radiotherapy: A dosimetric comparison. Cancer Res. Treat. 51, 1370–1379 (2019).
Eley, J. G. et al. Comparative risk predictions of second cancers after carbon-ion therapy versus proton therapy. Int. J. Radiat. Oncol. Biol. Phys. 95, 279–286 (2016).
Ytre-Hauge, K. S. et al. Inter-patient variations in relative biological effectiveness for cranio-spinal irradiation with protons. Sci. Rep. 10, 6212 (2020).
Sethi, R. A., No, H. S., Jozsef, G., Ko, J. P. & Formenti, S. C. Comparison of three-dimensional versus intensity-modulated radiotherapy techniques to treat breast and axillary level III and supraclavicular nodes in a prone versus supine position. Radiat. Oncol. 102, 74–81 (2012).
Jimenez, R. B. et al. Phase II study of proton beam radiation therapy for patients with breast cancer requiring regional nodal irradiation. J. Clin. Oncol. 37, 2778 (2019).
Remouchamps, V. M. et al. Initial clinical experience with moderate deep-inspiration breath hold using an active breathing control device in the treatment of patients with left-sided breast cancer using external beam radiation therapy. Int. J. Radiat. Oncol. Biol. Phys. 56, 704–715 (2003).
Acknowledgements
This work was supported by a faculty research grant of Yonsei University College of Medicine (6-2021-0234), by Korea Institute for Advancement of Technology (KIAT) Grant funded by the Korea Government (P0026103), by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (RS-2023-00249964), and by the Nuclear Safety Research Program (RS-2022-KN071210) through the Korea Foundation of Nuclear Safety (KOFONS) using the financial resource granted by the Nuclear Safety and Security Commission (NSSC) of the Republic of Korea.
Author information
Authors and Affiliations
Contributions
Conceptualization, D.W.K., C.-S.H., and J.S.K.; methodology, D.W.K., J.S., S.Y.K., and C.-S.H.; soft-ware, Y.I.P.; validation, D.W.K, J.S., S.Y.K., and C.-S.H.; formal analysis, D.W.K., and C.-S.H.; investigation, M.C. and W.K.C.; resources, M.C. and W.K.C.; data curation, M.C.H., J.K., and H.K.; writing—original draft preparation, D.W.K. and C.-S.H.; writing—review and editing, D.W.K. and C.-S.H.; visualization, Y.I.P. and C.-S.H.; supervision, D.W.K.; project administration, D.W.K., C.-S.H., and J.S.K.; funding acquisition, D.W.K. and C.-S.H.
All authors have read and agreed to the published version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kim, D.W., Hong, CS., Son, J. et al. Dosimetric analysis of six whole-breast irradiation techniques in supine and prone positions. Sci Rep 14, 14347 (2024). https://doi.org/10.1038/s41598-024-65461-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-65461-y
- Springer Nature Limited