Abstract
Previous studies have reported associations between newly diagnosed diabetes and poor outcomes after percutaneous coronary intervention (PCI), but there is limited data focusing on elderly patients (age ≥ 65). This study aimed to analyze the prevalence and clinical implications of newly diagnosed diabetes in elderly patients who underwent PCI. From 2004 to 2021, a total of 2456 elderly patients who underwent invasive PCI at Korea University Guro Hospital were prospectively enrolled and followed up for a median of five years. The primary endpoint was five-year major adverse cardiovascular events (MACE). Cox regression was used to evaluate whether newly diagnosed diabetes impacted on long-term clinical outcomes. Newly diagnosed diabetes was presented in approximately 8.1% to 10.9% of elderly patients who underwent PCI. Those who had a new diagnosis of diabetes had a higher risk of MACE than previously known diabetes (25.28% vs. 19.15%, p = 0.039). After adjusting for significant factors, newly diagnosed diabetes remained an independent predictor of MACE (HR [hazard ratio] 1.64, 95% confidence interval [CI] 1.24–2.17, p < 0.001), cardiac death (HR 2.15, 95% CI 1.29–3.59, p = 0.003) and repeat revascularization (HR 1.52, 95% CI 1.09–2.11, p = 0.013), but not for non-fatal myocardial infarction (HR 1.66, 95% CI 0.94–2.12, p = 0.081). Newly diagnosed diabetes was associated with an increased risk of 5-year MACE compared with non-diabetes and previously diagnosed diabetes in elderly patients underwent PCI. More attention should be given to those elderly newly diagnosed diabetes population.
Similar content being viewed by others
Introduction
Patients with coronary artery disease (CAD) who also have diabetes mellitus (DM) experience more cardiovascular events compared to non-diabetic patients1,2. Many studies have demonstrated a higher prevalence of DM in patients who underwent percutaneous coronary intervention3,4,5 (PCI) and those with DM were at a heightened risk of cardiovascular events6,7, such as restenosis8, stent thrombosis9, and higher rates of revascularization10. Furthermore, several researches have indicated that about 16–19% of patients undergoing PCI had newly diagnosed DM4,5,11. And newly diagnosed DM is shown to be associated with increased short-term and one-year major adverse cardiovascular and cerebral events (MACCE)5,12. However, there were limited data regarding the impact of newly diagnosed DM up to five years outcomes in elderly patients (age ≥ 65) who underwent PCI.
Thus, the objective of this study was to assess the prognostic implications of newly diagnosed DM in elderly patients undergoing PCI after a median follow-up of 5 years, in comparison to individuals with known DM or without DM.
Methods
Study population
Since 2004, all patients who underwent invasive PCI at Korea University Guro Hospital (KUGH) in Seoul, South Korea, were prospectively enrolled in the KUGH-PCI registry. It is a prospective study of all comers conducted at a single center that reflects ‘real world’ practice. All patients’ demographic data, clinical characteristics, description of PCI, medications on discharge, and blood tests including admission blood glucose, and glycated hemoglobin A1c (HbA1c) level were collected. The study exclusion criterion was defined as the exclusion of patients aged < 65 years, PCI procedural failure, no-drug-eluting stents (DES) or absent HbA1c level. For clinical diagnoses and clinical events, standard definitions were used for all variables related to patients and lesions. For all the participants or their legal guardians, a thorough literal and verbal explanation of study procedures was provided before their written informed consents were obtained. The Institutional Review Board of KUGH approved this study (#KUGH10045). All methods were performed in accordance with relevant guidelines and regulations.
Study definitions
In this study, newly diagnosed DM was defined as admission HbA1c ≥ 6.5%, without known DM history or current use of hypoglycemic agents. Multivessel disease was defined as at least two coronary vessels or left main coronary disease with more than 50% luminal narrowing. Diffuse long lesions referred to lesion length > 30 mm. Chronic total occlusion (CTO) was an obstruction of a native coronary artery that lasts for more than three months. Target lesion revascularisation (TLR) referred to the repeat revascularization in the previously implanted stent or 5 mm proximal or distal to the stented segment. Target vessel revascularisation (TVR) referred to the intervention in the same treated vessel. And non-TVR referred to a revascularization of any segment of the non-target coronary artery.
The primary clinical outcomes of interest were major adverse cardiovascular events (MACE) defined as the composite of cardiac death, non-fatal myocardial infarction (MI), and any repeat revascularization (including TLR, TVR, and non-TVR) among the three groups. Secondary outcomes were the individual components of MACE, all-cause mortality, TLR, TVR, non-TVR, stent thrombosis and stroke.
Statistical analysis
For continuous variables, data were expressed as mean ± standard deviations, or median (IQR) for variables that are not normally distributed. Differences among the three groups were evaluated by one-way ANOVA or Kruskal Wallis test and a post hoc test was applied: the Tukey’s Honestly Significant Difference test or Steel–Dwass test. For categorical variables, differences were expressed as counts and percentages and analyzed with χ2 or Fisher’s exact test between the groups as appropriate. Random forest method was used to impute missing values (using the randomForest package in the R language).
To adjust for potential confounders, univariable Cox proportional hazards model analysis was performed. We tested available 20 baseline clinical and angiographic variables that could be of relevance: sex, age, ST-segment elevation myocardial infarction (STEMI), cardiogenic shock, previous myocardial infarction (MI), previous PCI, previous coronary artery bypass grafting (CABG), hypertension, chronic kidney disease (CKD), atrial fibrillation (AF), smoking, multivessel disease, left main coronary lesion, bifurcation lesion, ca1cification lesion, diffuse long lesion, CTO and number of stents, total stent length. All variables with P < 0.05 or considered of clinical implications were included for further multivariable Cox analysis. A nomogram was constructed to visualize the risk factors for clinical outcomes with best discrimination and calibration. A two-tailed p-value of < 0.05 was considered to be statistically significant. The Bonferroni correction was used to adjust the P values for pairwise comparisons. Various 5-year clinical outcomes were estimated with Kaplan–Meier method, and differences between groups were compared with log-rank test. Data processing and analysis were performed using R version 4.3.0 (2023–04–21), along with Storm Statistical Platform (www.medsta.cn/software).
Results
Population
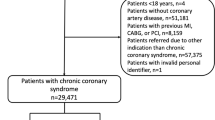
A total of 6972 patients who underwent PCI were enrolled during January 2004 and June 2021 (Fig. 1). Of these, 3529 were elderly patients (≥ 65 years old), 287 (8.1%) patients were newly diagnosed with DM, 1127 (32.0%) patients had previously known DM, and 2115 (59.9%) patients did not have DM. The median follow-up was 1806 days (5.0 years, median 825–2740 days [2.3–7.6 years]). Eventually, patients aged < 65 years (n = 3443), PCI procedural failure or no-DES (n = 149), absent HbA1c level (n = 924) were excluded (Fig. 1).
Considering the potential impact of stent generation and PCI procedural failure on clinical outcomes, a total of 2456 patients with DES, successful PCI revascularization and available record of blood glucose and HbA1c level were included in the final analysis. In this study population, 269 (10.9%) patients were newly diagnosed DM, 820 (33.4%) patients had previously known DM, and 1367 (55.7%) patients were non-DM. The median follow-up was 1975 days (5.4 years, median 882–2925 days [2.4–8.0 years]).
Baseline clinical and angiographic characteristics
The baseline clinical characteristics of patients categorized by glycemic status are detailed in Table 1. Newly diagnosed diabetic patients were younger (median age, 71 vs. 73 years old, p = 0.026), had higher rates of previous MI (2.23% vs. 0.24%, p = 0.005), previous PCI (4.46% vs. 0.00%, p < 0.001), previous CABG (1.86% vs. 0.24%, p = 0.007) and lower rates of hypertension (71.38% vs. 79.27%, p < 0.001), AF (3.35% vs. 7.07%, p = 0.004) and CKD (5.95% vs. 10.98%, p < 0.001) compared to those with previously known DM. Higher levels of HbA1c (median level, 7.1% vs. 7.0%, p < 0.001), total cholesterol (median level, 4.29 vs. 4.01 mmol/l, p < 0.001), total triglycerides (median level, 1.30 vs. 1.19 mmol/l, p < 0.001) and low-density lipoprotein cholesterol (median level, 2.79 mmol/l vs. 2.30 mmol/l, p < 0.001) were more common in newly diagnosed diabetes group and non-diabetes group compared to previously known diabetes group.
The angiographic characteristics and stent information across three groups are displayed in Table 1. Newly diagnosed DM and previously known DM patients had similar prevalence of multi-vessel disease (29.74% vs. 34.15%, p = 0.363), left main coronary disease (4.46% vs. 5.12%, p = 0.900), bifurcation lesions (34.94% vs. 27.69%, p = 0.067), ca1cification lesion (22.30% vs. 21.38%, p = 0.984), diffuse long lesions (54.65% vs. 48.54%, p = 0.185), and CTO (5.95% vs. 8.90%, p = 0.250). Thus, newly diagnosed DM and previously known DM patients had similar number of stents (1.69 ± 0.97 vs. 1.85 ± 1.11, p = 0.073) and total stent length (42.79 ± 27.10 mm vs. 43.70 ± 30.72 mm, p = 0.430). Over 98% of the patients was prescribed aspirin and clopidogrel after discharge. And there was no significant disparity between the utilization of antiplatelet therapy in all three groups (p > 0.100).
Five-year clinical outcomes
The newly diagnosed and previously known DM groups exhibited higher rates of total death (13.38% vs. 8.05%, p = 0.011; 12.32% vs. 8.05%, p = 0.004), cardiac death (7.81% vs. 3.88%, p = 0.022; 6.22% vs. 3.88%, p = 0.025) and MACE (25.28% vs. 15.44%, p < 0.001; 19.15% vs. 15.44%, p = 0.039) compared to the non-diabetic group (Table 1). Newly diagnosed DM seemed to have higher risk of MACE (25.28% vs. 19.15%, p = 0.039) and a trend towards higher MI (5.95% vs. 2.68%, p = 0.058) than previously known DM. However, there were no statistically significant differences in terms of TLR, TVR, non-TVR, and stent thrombosis across the three groups.
Kaplan–Meier survival analysis demonstrated that the 5-year cumulative incidences of MACE were significantly higher in the newly diagnosed diabetes and previously known diabetes, compared to non-diabetic group (pairwise log-rank p < 0.001; pairwise log-rank p = 0.003; Fig. 2D), but the difference between newly diagnosed and previously known diabetes was not significant (pairwise log-rank p = 0.135). The components of MACE in different glycemic status are shown in Fig. 2A–C. The 5-year cumulative incidences of cardiac death and repeat revascularization were similar as MACE. Only 5-year cumulative incidence of no-fatal MI in newly diagnosed diabetes was significantly higher than that in previously known diabetes (pairwise log-rank p = 0.031).
Multivariable Cox regression model
The detailed results could be found in Table 2 and more univariate Cox analysis information in Supplementary Material. Multivariate Cox regression showed that newly diagnosed diabetes was an independent predictor of MACE [hazard ratio (HR) 1.64, 95% confidence internal (CI) 1.24–2.17, p < 0.001], cardiac death (HR 2.15, 95% CI 1.29–3.59, p = 0.003) and repeat revascularization (HR 1.52, 95% CI 1.09–2.11, p = 0.013), except for the non-fatal MI (HR 1.66, 95% CI 0.94–2.12, p = 0.081). While previously known DM was only independently associated with five-year MACE (HR 1.24, 95% CI 1.01–1.54, p = 0.044). Besides, cardiogenic shock was the strongest predictor of MACE (HR 4.54, 95% CI 3.28–6.30, p < 0.001), cardiac death (HR 9.85, 95%CI 6.41–15.14, p < 0.001), non-fatal MI (HR 3.66, 95% CI 1.68–7.97, p = 0.001) and repeat revascularization (HR 1.88, 95%CI 1.07–3.29, p = 0.027). Additionally, CKD remained a significant predictor of MACE (HR 1.71, 95% CI 1.23–2.37, p = 0.001), cardiac death (HR 3.24, 95% CI 1.99–5.28, p < 0.001), and non-fatal MI (HR 2.24, 95% CI 1.11–4.51, p = 0.024).
To assess the performance of the models described above, concordance index (C-index) was calculated, and calibration curve was determined for the best regression model. The multivariable Cox regression model for five-year cardiac death had the best discrimination with C-index of 0.796 (95% CI 0.756–0.836). The subsequent nomogram and calibration curve are showed in Fig. 3.
The figure (A) is a nomogram predicting the risk of five-year cardiac death in elderly patients underwent PCI. A score was given to the value of each variable on the point scale axis. By adding each score, a total score could be calculated and projected to the lower total score scale, so we could estimate five-year cardiac-death free survival probability. The figure (B) is the calibration curves for the nomogram. The x-axis represents the nomogram-predicted probability and y-axis represents the actual probability of cardiac death. Perfect prediction would correspond to the 45° gray dashed line. The red dotted line represents the entire cohort (n = 2456), and the blue solid line is bias-corrected by bootstrapping (B = 500 repetitions), indicating observed nomogram performance. CKD = chronic kidney disease, STEMI = ST-segment elevation myocardial infarction.
Discussion
In this study, newly diagnosed DM was presented in approximately 8.1–10.9% of elderly patients who underwent PCI. Moreover, newly diagnosed DM was independently associated with increased risk of five-year MACE, and was a stronger risk factor compared with previously known DM.
Several studies have analysed the prevalence of newly diagnosed DM in specific CAD patients undergoing PCI and subsequent clinical outcomes. De la Hera et al.4 reported 16.2% of studied patients (stable angina or NSTEMI, n = 580) who underwent PCI was newly detected diabetes, based on the oral glucose tolerance teat (OGTT) after discharge. And newly diagnosed DM was not an independent predictor of 1-year outcomes. Tailakh et al.5 demonstrated that 19% of total 1151 CAD patients had newly diagnosed DM based on the HbA1c level. Newly diagnosed DM was independently associated with increased MACCE at one-month but not at one-year. Subgroup analysis showed male and patients younger than 75 years appeared higher one-year MACCE risk. Jimenez-Navarro et al.13 discovered that 21.4% of 374 CAD patients who underwent PCI were newly detected diabetes and previously known diabetes remained the only independent predictor of cardiovascular events in a mean follow-up of 35.8 ± 13.43 months. Tsuchida et al.14 reported 17% of the 298 patients studied had newly diagnosed DM, which was not a predictor of up to 10-year cardiovascular disease risk. Other studies focused on only STEMI patients15,16. Therefore, newly diagnosed DM seemed to have greater short-term impact and less long-term impact according to the above studies. But there is limited data to evaluate the impact of newly diagnosed DM in elderly patients.
As far as we know, our study focused specifically on elderly population and for the first time, investigating whether or not newly diagnosed DM impacted on five-year clinical outcomes in elderly patients undergoing PCI. The prevalence of newly diagnosed DM in elderly patients undergoing PCI was similar to that in prior studies across all age groups. All patients with DM, no matter newly or previously diagnosed, had more cardiovascular events than patients without DM, which has been investigated in numerous studies12,17,18,19. Our results are in agreement with previous findings, newly diagnosed diabetic patients were younger and had less comorbidities5,12. Furthermore, we reported more detailed information about angiographic characteristics of newly diagnosed diabetes than former studies. Despite having similar baseline to patients without DM, patients with newly diagnosed diabetes had comparable complicated coronary lesions with previous DM patients. Notably, newly diagnosed diabetic patients had more history of previous MI, PCI and CABG, along with higher HbA1c level, which may account for its poor prognosis5,19,20,21. A possible reason is that those patients with newly diagnosed DM may have been unaware of asymptomatic and uncontrolled DM for a long time. A recent study22 has shown similar impact of DM on increased risk of 5-year cardiovascular outcomes after PCI.
In the present study, we focused on elderly patients with newly diagnosed diabetes, a distinctive cohort that warrants special attention. It might be assumed that newly diagnosed diabetes has a lesser impact on elderly individuals. However, it is essential to recognize that older adults often face a unique set of challenges, including a higher risk of physical and mental frailty 23,24, a vulnerable immune system25, an increased burden of diabetes-related complications26, poorer treatment adherence27, and a potentially more conservative approach to blood glucose control due to concerns about hypoglycemia28. As a result, these factors may collectively contribute to the elevated incidence of adverse outcomes in the elderly population, which underscores the importance of our study's focus on this particular demographic. By acknowledging these factors and their implications, we can better appreciate why there is a need for a more targeted and nuanced approach to managing diabetes in elderly patients.
There are some limitations should be considered. Firstly, this was a single-center study, it is important to evaluate the findings in a larger population involving multiple centers. Despite a monocenter study, we included more than two thousand elderly patients underwent PCI to preliminarily explore the long-term outcomes of newly diagnosed DM. Secondly, there was no information available to evaluate the status of diabetes controlled, the treatment modalities, changes on medication details and adherence, which may affect the outcomes of patients undergoing PCI. There should be more specific work on those elements in the future. Thirdly, due to the absence of available variables, a mount of cases were excluded from the analysis, which could have biased our findings. Besides, it is possible that multivariable models may contain incomplete adjustments or unknown confounders that have not been consolidated.
Conclusions
In conclusion, our study indicated that newly diagnosed DM was associated with an increased risk of five-year MACE compared with non-DM and previously diagnosed DM in elderly patients who underwent PCI. Our findings support the importance of identifying and treating diabetes at early stage for elderly CAD patients undergoing PCI. And it is necessary to monitor on the blood glucose, and perform HbA1c screening among high-risk elderly patients who undergoing PCI. It is hoped that more attention and care should be given to the older population.
Data availability
Data are available by contacting the corresponding author on reasonable requests.
References
Rawshani, A., Rawshani, A. & Gudbjornsdottir, S. Mortality and cardiovascular disease in type 1 and type 2 diabetes. N. Engl. J. Med. 377(3), 300–301 (2017).
Billinger, M. et al. Two-year clinical outcome after implantation of sirolimus-eluting and paclitaxel-eluting stents in diabetic patients. Eur. Heart J. 29(6), 718–725 (2008).
Tada, T. et al. Comparison of three-year clinical outcomes after sirolimus-eluting stent implantation among insulin-treated diabetic, non-insulin-treated diabetic, and non-diabetic patients from j-Cypher registry. Am. J. Cardiol. 107(8), 1155–1162 (2011).
de la Hera, J. M. et al. Prevalence and outcome of newly detected diabetes in patients who undergo percutaneous coronary intervention. Eur. Heart J. 30(21), 2614–2621 (2009).
Tailakh, M. A. et al. Prospective study of the impact of diabetes mellitus newly diagnosed by glycated hemoglobin on outcomes in patients undergoing percutaneous coronary intervention. Eur. J. Intern Med. 37, 69–74 (2017).
Mathew, V. et al. Outcomes in patients with diabetes mellitus undergoing percutaneous coronary intervention in the current era: A report from the Prevention of REStenosis with Tranilast and its Outcomes (PRESTO) trial. Circulation 109(4), 476–480 (2004).
Wilson, S. R. et al. Effect of diabetes on long-term mortality following contemporary percutaneous coronary intervention: Analysis of 4284 cases. Diabetes Care 27(5), 1137–1142 (2004).
Kornowski, R. et al. Increased restenosis in diabetes mellitus after coronary interventions is due to exaggerated intimal hyperplasia: A serial intravascular ultrasound study. Circulation 95(6), 1366–1369 (1997).
Iakovou, I. et al. Incidence, predictors, and outcome of thrombosis after successful implantation of drug-eluting stents. JAMA 293(17), 2126–2130 (2005).
Sato, T. et al. Differences in clinical and angiographic outcomes with different drug-eluting stents in Japanese patients with and without diabetes mellitus. J. Cardiol. 60(5), 361–366 (2012).
Muhlestein, J. B. et al. Effect of fasting glucose levels on mortality rate in patients with and without diabetes mellitus and coronary artery disease undergoing percutaneous coronary intervention. Am. Heart J. 146(2), 351–358 (2003).
Aguilar, D. et al. Newly diagnosed and previously known diabetes mellitus and 1-year outcomes of acute myocardial infarction: The VALsartan In Acute myocardial iNfarcTion (VALIANT) trial. Circulation 110(12), 1572–1578 (2004).
Jimenez-Navarro, M. F. et al. Newly impaired glucose metabolism and prognosis after percutaneous revascularization. Cardiol. J. 22(1), 44–51 (2015).
Tsuchida, K. et al. Impaired glucose tolerance and future cardiovascular risk after coronary revascularization: A 10-year follow-up report. Acta Diabetol. 57(2), 173–182 (2020).
Aggarwal, B. et al. Utility of glycated hemoglobin for assessment of glucose metabolism in patients with ST-segment elevation myocardial infarction. Am. J. Cardiol. 117(5), 749–753 (2016).
Ostrominski, J. W. et al. Missed opportunities for screening and management of Dysglycemia among patients presenting with acute myocardial infarction in North India: The prospective NORIN STEMI registry. Glob. Heart 17(1), 54 (2022).
Marso, S. P. et al. Plaque composition and clinical outcomes in acute coronary syndrome patients with metabolic syndrome or diabetes. JACC Cardiovasc. Imaging 5(3 Suppl), S42-52 (2012).
Ojeda, S. et al. Immediate results and long-term clinical outcome of patients with unprotected distal left main restenosis: The CORPAL registry (Cordoba and Las Palmas). JACC Cardiovasc. Interv. 7(2), 212–221 (2014).
Selvin, E. et al. Glycated hemoglobin, diabetes, and cardiovascular risk in nondiabetic adults. N. Engl. J. Med. 362(9), 800–811 (2010).
Baber, U. et al. Hemoglobin A(1c) and cardiovascular outcomes following percutaneous coronary intervention: Insights from a large single-center registry. JACC Cardiovasc. Interv. 14(4), 388–397 (2021).
Timmer, J. R. et al. Prognostic value of admission glycosylated hemoglobin and glucose in nondiabetic patients with ST-segment-elevation myocardial infarction treated with percutaneous coronary intervention. Circulation 124(6), 704–711 (2011).
Kosmidou, I. et al. Long-term outcomes in women and men following percutaneous coronary intervention. J. Am. Coll. Cardiol. 75(14), 1631–1640 (2020).
Veronese, N. et al. Prevalence of multidimensional frailty and pre-frailty in older people in different settings: A systematic review and meta-analysis. Ageing Res. Rev. 72, 101498 (2021).
Soysal, P. et al. Relationship between depression and frailty in older adults: A systematic review and meta-analysis. Ageing Res. Rev. 36, 78–87 (2017).
Eggersdorfer, M. et al. Perspective: Role of micronutrients and Omega-3 long-chain polyunsaturated fatty acids for immune outcomes of relevance to infections in older adults—A narrative review and call for action. Adv. Nutr. 13(5), 1415–1430 (2022).
Gopalraj, R. The older adult with diabetes and the busy clinicians. Primary Care: Clin. Off. Pract. 44(3), 469–479 (2017).
Chiatti, C. et al. The economic burden of inappropriate drug prescribing, lack of adherence and compliance, adverse drug events in older people a systematic review. Drug Saf. 35, 73–87 (2012).
Bruce, D. G., Davis, W. A. & Davis, T. M. E. Glycaemic control and mortality in older people with type 2 diabetes: The Fremantle Diabetes Study Phase II. Diabetes, Obesity and Metabolism 20(12), 2852–2859 (2018).
Acknowledgements
This work was supported by Key Project of Tianjin Natural Science Foundation [Grant No: 21JCZDJC01080]. This work was also partly supported by Academic Backbone of “Clinical Talent Training and Climbing Plan” of Tianjin Medical University, and “Jinmen Medical Talent” of Tianjin Health Industry High-Level Talent Selection and Training Project.
Author information
Authors and Affiliations
Contributions
Study conception and design: K.-Y.C. and Z.-K.X.; data collection: X.-Y.D., S.-T.H., S.P., C.-U.C., B.-G.C. and S.-W.R.; analysis and interpretation of results: Z.-K.X., J.-Y.R., Y.-K.Z., P.W., X.W. and J.-K.Z.; draft manuscript preparation: Z.-K.X., X.-Y.D., J.-Y.R., T.L., Y.-K.Z. and G.T. All authors reviewed the manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Xue, ZK., Dai, XY., Ren, JY. et al. Prevalence, clinical characteristics, and long-term outcomes of new diabetes diagnosis in elderly patients undergoing percutaneous coronary intervention. Sci Rep 14, 14814 (2024). https://doi.org/10.1038/s41598-024-65426-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-65426-1
- Springer Nature Limited