Abstract
Previous published data have confirmed that the addition of a citric acid meal improves the accuracy of the 13C-urea breath test (13C-UBT). However, some studies have suggested that a citric acid test meal may not be necessary. Thus, the aim of this study was to evaluate the combination of a 13C-UBT with a citric acid meal for the diagnosis of Helicobacter pylori (Hp) infection in a Chinese population, particularly for patients with results in the gray zone. In this paired self-controlled study, all subjects had previously undergone 13C-UBTs without citric acid meals and were randomly divided into two groups based on different doses of citric acid (a low-dose citric acid group and a high-dose citric acid group, comprising meals with 0.68 g and 3.84 g citric acid powder, respectively). Positive rapid urease test (CLO) test and histology results were considered the 'gold standard'. The mean delta over baseline (DOB) value, sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV) and accuracy were compared between the two groups, particularly for patients with results in the gray zone. In total, 285 patients were tested. Of these patients, 189 were included in the low-dose citric acid group, and 96 were included in the high-dose citric acid group. Among patients with a positive 13C-UBT result without citric acid [delta over baseline (DOB) value ≥ 4‰, n = 174] and a negative 13C-UBT result without citric acid (DOB value < 4‰, n = 111), 8.0% (14/174) were false positive, and 0.9% (1/111) was false negative as determined by gold standard. Of 14 patients with false positive, 78.6% (11/14) false positive were in the gray zone of 4–10‰. However, there were no false positive 13C-UBT results with citric acid in the the gray zone of 4–10‰. In the comparison of the commercial 13C-UBT with the 13C-UBT in the low-dose citric acid group, the sensitivity, specificity, PPV, NPV and accuracy at 15 min were as follows: 99.1% vs. 99.1%, 97.5% vs. 88.9%, 98.2% vs. 92.2%, 98.8% vs. 98.6% and 98.4% vs. 94.7%, respectively. In the the gray zone of 4.0–10.0‰, the comparison of the commercial 13C-UBT with the 13C-UBT in the low-dose citric acid group, the sensitivity, specificity, PPV, and accuracy at 15 min were as follows: 94.4% vs. 100.0%, 100.0% vs. 0%, 100.0% vs. 75.0% and 95.8% vs. 75.0%, respectively. No significant difference was observed between the 15-min and 30-min measurement intervals in the low- and high-dose citric acid groups, including patients with results in the gray zone. The low-dose citric acid test, with an optimal measurement interval of 15 min, was highly accurate in the diagnosis of Hp infection in the Chinese population, especially for individuals with results in the gray zone.
Similar content being viewed by others
Introduction
The 13C-urea breath test (13C-UBT) is a noninvasive, simple, reliable and widely available test for diagnosing an active Helicobacter pylori (H. pylori) infection1,2,3,4,5,6,7. However, the optimal cutoff value to define whether a 13C-UBT result is positive or negative remains controversial8. Some authors have considered a gray zone, in which 13C-UBT results are inconclusive, to overcome this problem9. The gray zone, for which an exact range has not been defined, however, in two studies both by Kwon et al.9,10, they defined the gray zone to be 2.5–10.0‰ based on the known cutoff value of 2.5‰. Additionally, some studies have reported that most false-positive results are in the “gray zone”10,11.
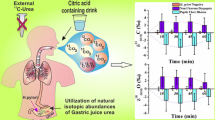
To improve the accuracy and sensitivity of the 13C-UBT test, citric acid meals have been proposed as being more favorable than other test meals, such as standard semiliquid meals, semifatty acid meals and orange or apple juice12,13. Citric acid helps lower intragastric pH, which tends to inhibit non-H. pylori ureases, delay gastric emptying, maximize gastric distribution of the substrate and increase the contact time with H. pylori urease12,14,15. Thus, theoretically, citric acid can increase the diagnostic accuracy of the 13C-UBT. Several studies have investigated the efficacy of the combination of a citric acid meal with the 13C-UBT by comparing the 13C-UBT with or without citric acid, but the results were mixed9,12,13,16,17,18,19,20,21. Most of the published studies have focused the Western population. The study of Graham et al.12, one of the representative studies, revealed a dose–response relationship between urease activity and the amount of citric acid from 1 to 4 g; compared with commercial pudding, meals with 1, 2, or 4 g citric acid led to significant increases in breath 13CO2 activity (p < 0.05). Standard protocols in the United States and Europe recommend combining a citric acid meal with the 13C-UBT13. Moreover, the Maastricht VI/Florence consensus report published in 2022 provides a strong agreement and high-quality statement that citric acid is an essential component of the 13C-UBT22. However, relatively few studies assessing the combination of a citric acid meal with the 13C-UBT have been conducted in Asian populations, and there is no unified standard for 13C-UBT detection reagents.
Based on this background, the aim of this study was to evaluate the combination of the 13C-UBT with a citric acid meal for the diagnosis of H. pylori infection in the Chinese population and validate the hypothesis that a citric acid meal could improve the diagnostic accuracy of the 13C-UBT in Chinese individuals, particularly those with results in the gray zone.
Methods
All methods were carried out in accordance with relevant regulations and guidelines.
Patient population
A total of 297 patients were referred to the endoscopy unit of the Department of Gastroenterology, The First Affiliated Hospital of Anhui Medical University, between September 2022 and December 2022. The inclusion criteria were as follows: male and female patients aged 18–80 years. The exclusion criteria were (1) patients who had undergone gastric surgery; (2) patients who were administered antibiotics or consumed bismuth compounds within the last 4 weeks or who were administered proton pump inhibitors (PPIs) or H2 receptor antagonists within 2 weeks prior to the 13C-UBT and endoscopy; and (3) patients who had received prior H. pylori eradication therapy. Written informed consent was obtained from all patients, and the study was approved by the Ethics Committee of First Affiliated Hospital of Anhui Medical University. The study was registered with the Chinese Clinical Trial Registration Center (www.chictr.org.cn; registration numbers ChiCTR2200064083; registration date 26/09/2022).
13C-UBT procedure
The 13C-UBT, with or without a test meal, was performed within one week for all patients after fasting for a minimum of 2 h. The test meals comprised 0.68 g citric acid (low-dose group, n = 189) and 3.84 g citric acid (high-dose group, n = 96). All patients were randomly assigned to one of the two groups based on the order of the draw. A 75-mg 13C-urea capsule(Urea 13C capsule breath test Kit, Zhonghe Headway Bio-Sci & Tech Co., Ltd., Shenzhen, China, cutoff value: 4‰) and citric acid solution [Headway Citric acid solid drink, Shenzhen, China, 5 g (containing 3.84 g citric acid powder, maltose and sucrose polymer with artificial sweetener) and 2 g (containing 0.68 g citric acid powder, maltose and sucrose polymer with artificial sweetener)] dissolved in 50 mL of water were administered orally. Further breath samples were taken at 15 and 30 min. Breath samples for the commercial 13C-UBT (self-control 30 min) were taken at 30 min without citric acid. All patients maintained a seated position throughout the whole test. Collected samples were analyzed by the purpose-built isotope ratio mass spectrometer in the Key Laboratory of Gastroenterology of Anhui Province, The First Affiliated Hospital of Anhui Medical University. The results are expressed as the delta over baseline (DOB) value, and a DOB value greater than 4‰ was considered to indicate a positive result for H. pylori infection12. The cutoff value of 4‰, recommended by the manufacturer, was also used. 13C-UBT gray zone was defined from 4.0 to 10.0‰ in this study. The sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV) and accuracy of the 13C-UBT were evaluated at different measurement intervals (15 and 30 min), especially in the gray zone, and compared between the low-dose group and the high-dose group.
Gastric biopsies
All patients had two biopsy samples taken from the corpus and antrum for histological assessment and underwent a rapid urease test (CLO test). Specimens were examined by a pathologist who specialized in gastroenterology and was blinded to all clinical information, including the 13C-UBT and CLO test results. The presence of H. pylori was assessed by modified Giemsa staining. In this study, H. pylori infection was defined as a positive result for both the CLO test and histology, which was used as the 'gold standard'. The absence of H. pylori infection was defined as negative results for both tests. Patients with equivocal results (one test with positive results and the other with negative results) were excluded from our analysis.
Statistical analysis
In this study, we used paired t tests or paired Wilcoxon signed-rank tests, depending on whether the data were normally distributed. The sensitivity, specificity, PPV, NPV and overall accuracy were calculated. A p < 0.05 was considered to indicate statistical significance.
Results
The flow of the current study and effect of a citric acid meal on the diagnostic accuracy of the 13C-UBT
A total of 297 patients were recruited for the study. Among these patients, 12 could not be classified as having Hp infection according to our 'gold standard', i.e., patients with positive results for only one of the two tests. The remaining 285 patients were included for analysis. Of these patients, 189 were included in the low-dose citric acid group, and 96 were included in the high-dose citric acid group. The study flow is summarized in Fig. 1. Urease activity was increased in H. pylori-infected patients (Table 1). The mean DOB value of H. pylori-infected patients in the two groups, the measurement intervals were 15 min and 30 min, which were statistically (P < 0.0001) greater than those of the commercial 13C-UBT without citric acid, in which breath samples are taken at 30 min (Table 1). Although the mean DOB value of H. pylori-uninfected patients in the two groups at 15 min and 30 min, which were decreased than those of the commercial 13C-UBT without citric acid at 30 min, the decrease was not statistically (P > 0.05) significant (Table 1). When the diagnostic accuracy of the 13C-UBT was calculated, the 15-min measurement interval in the high-dose citric acid group had the highest sensitivity, specificity, PPV, NPV and accuracy for the 13C-UBT, with no false negative or false positive results (Table 1). When compared with the results in the 15-min measurement interval between the low- and high-dose groups, the sensitivity (99.1% vs. 100.0%), specificity (97.5% vs. 100.0%), PPV (98.2% vs. 100.0%), NPV (98.8% vs. 100.0%) and accuracy (98.4% vs. 100.0%) of the 13C-UBT were similar between the two groups. No significant difference was observed between the 15-min and 30-min measurement intervals in the the low- and high-dose groups (Table 1).
Diagnostic accuracy of the 13C-UBT for patients with results in the gray zone of 4–10‰
Of the 285 participants, 13%(37/285) were in the the gray zone of 4–10‰, which 64.9% (24/37) were in the low-dose citric acid group and 35.1% (13/37) were in the high-dose citric acid group. Among patients with a positive 13C-UBT result without citric acid (≥ 4‰, n = 174) and a negative 13C-UBT result without citric acid (< 4‰, n = 111), 8.0% (14/174) were false positive, and 0.9% (1/111) was false negative as determined by 'gold standard'. Of 14 patients with false positive, 78.6% (11/14) false positive were in the gray zone of 4–10‰. The false-positive rates of 13C-UBT at cutoff values between 4 and 10‰ ranged from 12.5 to 57.1% (Fig. 2). However, there were no false positive 13C-UBT results in the the gray zone of 4–10‰ with citric acid, including low-dose and high-dose groups. In the the gray zone, the mean DOB value of H. pylori-infected patients in the two groups, the measurement intervals were 15 min and 30 min, which were statistically (P = 0.008) greater than those of the commercial 13C-UBT without citric acid, in which breath samples are taken at 30 min (Table 2). When the diagnostic accuracy of the 13C-UBT in the gray zone was calculated, the 15-min measurement interval in the high-dose citric acid group had the highest sensitivity, specificity, PPV, NPV and accuracy of 100.0% (8/8), 100.0% (5/5), 100.0% (8/8), 100.0% (5/5), and 100.0% (13/13), respectively (Table 2). The commercial 13C-UBT breath samples taken at 30 min without citric acid in the gray zone showed the lowest specificity, PPV and accuracy of 0% (0/5), 61.5% (8/13) and 61.5% (8/13), respectively (Table 2). When compared with the results in the 15-min measurement interval between the low- and high-dose groups in the gray zone, the sensitivity (94.4% vs. 100.0%), specificity (100.0% vs. 100.0%), PPV (100.0% vs. 100.0%), NPV (87.5% vs. 100.0%) and accuracy (95.8% vs. 100.0%) of the 13C-UBT were similar between the two groups. No significant difference was observed between the 15-min and 30-min measurement intervals in the the low- and high-dose groups (Table 2).
Discussion
As noted earlier, this was a paired self-controlled study based on the 'gold standard' to determine whether a citric acid meal could improve the diagnostic accuracy of the 13C-UBT in Chinese individuals, particularly those with results in the gray zone. We found that the sensitivity, specificity, PPV, NPV and accuracy of the citric acid group were significantly higher than those of the self-control group, particularly for patients with results in the gray zone. However, no statistically significant difference was observed between the low- and high-dose groups. Moreover, there was no significant difference between the 15-min and 30-min measurement intervals in the citric acid group.
Furthermore, inconsistent efficacy of the combination of a citric acid meal with the 13C-UBT has been reported worldwide, and most of the studies were based on Western data9,12,13,16,17,18,19,20,21. The present paired self-controlled study reported that the mean 13C-UBT value, sensitivity, specificity, PPV, NPV and accuracy of the citric acid group (both low- and high-dose groups) were significantly higher than those of the self-control group. Nevertheless, there was no significant difference between the 15-min and 30-min measurement intervals in the citric acid group (both low- and high-dose groups). This result suggests that the use of a citric acid test meal could potentially increase the accuracy of the 13C-UBT and allow for a shorter test duration. The fact that urease activity was markedly enhanced after the ingestion of urea in citric acid suggested that citric acid could increase urea hydrolysis by H. pylori and lower intragastric pH, which tends to inhibit non-H. pylori ureases14. Urea might also delay gastric emptying and maximize the distribution of the substrate within the stomach, thereby enhancing the contact area and time between the bacteria and the substrate1,8. Graham et al.12 conducted a single-center, paired self-controlled study in the United States and evaluated the effect of the combination of citric acid test meals (1 g, 2 g and 4 g citric acid dissolved in 200 mL of water) with the 13C-UBT (125 mg of 13C-urea, cutoff value 2.4 DOB, n = 46) and revealed a dose‒response relationship between the mean DOB value and the amount of citric acid (increasing from 1 to 4 g) compared with commercial pudding (p < 0.05). In addition, a 2019 prospective study by Kwon et al.9, on the effect of citric acid on the accuracy of the 13C-UBT after H. pylori eradication therapy in Korea reported that the mean 13C-UBT value of the citric acid group was significantly (p < 0.001) higher than that of the control group; however, interestingly, the inclusion of a citric acid meal did not increase the diagnostic accuracy or specificity of the 13C-UBT after H. pylori eradication therapy. In 2000, Wong et al.21 conducted a single-center, paired self-controlled clinical study in Hong Kong, China and revealed that the 13C-UBT with or without a citric acid test meal produced highly accurate and reliable results.
Some studies suggested that most false-positive results are in the gray zone and should be considered inconclusive10,11. Moreover, the interpretation of the gray zone, for which an exact range has not been defined, remains a controversial issue. A study by Kwon et al.10, 1891 patients who had received H. pylori eradication therapy in Korea, they defined the gray zone to be 2.5–10.0‰ based on the known cutoff value of 2.5‰, and the false-positive rates of 13C-UBT value in the gray zone ranged from 6.7% to 77.3%. However, citric acid had no beneficial effect on the diagnostic validity of results in the gray zone. As we known, there were no reports in the Chinese population on the combination of a citric acid meal with the 13C-UBT in the gray zone. Therefore, our study is the first to evaluate the 13C-UBT for results in the gray zone for the diagnosis of H. pylori infection in the Chinese population. As we expected, the combination of the 13C-UBT with a citric acid meal showed reliable and excellent results in the diagnosis of H. pylori infection in the Chinese population. We found that the citric acid group had a significantly reduced false-positive rate compared with the group who underwent a commercial 13C-UBT and had results in the gray zone. This suggested that the combination of the 13C-UBT with a citric acid meal benefited the diagnostic validity, which became more prominent for patients in the gray zone. The discrepancy of results between our study and a study by Kwon et al. can be explained as follows. First, the gold standard for diagnosing H. pylori infection is different. In Kwon et al.’s study9, the 'gold standard' for H. pylori infection is either positive CLO test or histology results. The number of patients who underwent histology was only 10.1% (122/1207) of all enrolled patients; moreover, only 92 participants were evaluated by both histology and the CLO test, which may have affected the relatively low accuracy of the 13C-UBT. However, in our study, 285 patients were included for analysis and all patients were evaluated by endoscopic biopsy methods(both histology and the CLO test). Positive CLO test and histology results were considered the 'gold standard' in our study. Second, it should be noted that differences in research methods might be a potential explanation. Our approach was the same as that in Graham’s study12; in this paired self-control study, all subjects previously underwent the 13C-UBT without citric acid meals and were blindly assigned citric acid groups receiving different doses (citric acid powder dissolved in 50 mL of water). Nevertheless, Kwon et al.9 randomly divided patients into two groups, one group with a citric acid meal and the other without a citric acid meal (4 g in 200 mL of water containing 50 g glucose polymer with artificial sweetener). Third, the study population is different. In a study by Kwon et al.9, all patients were after Helicobacter pylori Eradication Therapy. In our study, all patients who had not received prior H. pylori eradication therapy. Fourth, other potential explanations include differences in the distribution, delivery and emptying of 13C-urea and ethnic differences in gastric emptying23.
This study has several limitations. First, this was a paired self-controlled study conducted at a single center with a relatively modest sample size; hence, a well-designed, prospective, multicenter, randomized controlled study is needed to verify the results. Third, the effect of citric acid meals on the accuracy of the 13C-UBT after H. pylori eradication therapy still needs to be evaluated.
Citric acid solutions are bitter and unpleasant. Our data suggested that the ability to achieve favorable results was similar between the low- and high-dose citric acid groups at the 15-min measurement interval. Low-dose citric acid may be a good alternative to improve palatability for patients. Additionally, a citric acid test meal can reduce the false positive rate and improve accuracy; to some extent, it can also reduce the unnecessary psychological burden and medical expenses for patients. To date, there are no reports that the addition of citric acid disturbs 13C-UBT results. Overall, citric acid meals can increase the sensitivity, specificity, and accuracy of the 13C-UBT in detecting H. pylori infection, especially for patients with results in the gray zone, and there is little justification for not using citric acid as an adjuvant to the 13C-UBT24. Taken together, our findings demonstrated that a low-dose citric acid meal, with an optimal measurement interval of 15 min, was highly accurate in the diagnosis of H. pylori infection in the Chinese population, especially for patients with results in the gray zone. The combination of the 13C-UBT with a citric acid meal may become the standard protocol in the Chinese population.
Data availability
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
References
Graham, D. Y. et al. Campylobacter pylori detected noninvasively by the 13C-urea breath test. Lancet 1, 1174–1177 (1987).
Logan, R. P. et al. Simplified single sample 13Carbon urea breath test for Helicobacter pylori: Comparison with histology, culture, and ELISA serology. Gut 32, 1461–1464 (1991).
Logan, R., Dill, S., Bauer, F. E. & Misiewicz, J. The European 13C-urea breath test for the detection of Helicobacter pylori. Eur. J. Gastroenterol. Hepatol. 3, 915–921 (1991).
Eggers, R. A methodological analysis of the 13C-urea breath test for detection of Helicobacter pylori infections: High sensitivity and specificity within 30 min using 75 mg of 13 C-urea. Eur. J. Gastroenterol. Hepatol. 2, 437–444 (1990).
Lotterer, E. et al. The simplified 13C-urea breath test–one point analysis for detection of Helicobacter pylori infection. Z Gastroenterol. 29, 590–594 (1991).
Gisbert, J. P. & Pajares, J. M. Review article: 13C-urea breath test in the diagnosis of Helicobacter pylori infection—a critical review. Aliment. Pharmacol. Ther. 20, 1001–1017 (2004).
Best, L. M., Takwoingi, Y., Siddique, S., Selladurai, A., Gandhi, A., Low, B., Yaghoobi, M., & Gurusamy, K. S. Non-invasive diagnostic tests for Helicobacter pylori infection. Cochrane Database Syst. Rev. 3, CD012080 (2018).
Graham, D. Y., & Klein, P. D. Accurate diagnosis of Helicobacter pylori. 13C-urea breath test. Gastroenterol. Clin. N. Am. 29, 885 (2000).
Kwon, Y. H. et al. Effect of citric acid on accuracy of 13C-urea breath test after Helicobacter pylori eradication therapy in a region with a high prevalence of atrophic gastritis. Gut Liver. 13, 506–514 (2019).
Kwon, Y. H. et al. The diagnostic validity of citric acid-free, high dose (13)C-Urea breath test after Helicobacter pylori eradication in Korea. Helicobacter. 20, 159–168 (2015).
Calvet, X. et al. Accuracy of diagnostic tests for Helicobacter pylori: A reappraisal. Clin. Infect. Dis. 48, 1385–1391 (2009).
Graham, D. Y., Runke, D., Anderson, S. Y., Malaty, H. M. & Klein, P. D. Citric acid as the test meal for the 13C-urea breath test. Am. J. Gastroenterol. 94, 1214–1217 (1999).
Domínguez-Muñoz, J. E., Leodolter, A., Sauerbruch, T. & Malfertheiner, P. A citric acid solution is an optimal test drink in the 13C-urea breath test for the diagnosis of Helicobacter pylori infection. Gut. 40, 459–462 (1997).
Miederer, S. E. & Grübel, P. Profound increase of Helicobacter pylori urease activity in gastric antral mucosa at low pH. Dig. Dis. Sci. 41, 944–949 (1996).
Leodolter, A., Domínguez-Muñoz, J. E., Von Arnim, U. & Malfertheiner, P. Citric acid or orange juice for the 13C-urea breath test: The impact of pH and gastric emptying. Aliment Pharmacol. Ther. 13, 1057–1062 (1999).
Gisbert, J. P. et al. 13C-urea breath test for the diagnosis of Helicobacter pylori infection: Are basal samples necessary?. Eur. J. Gastroenterol. Hepatol. 12, 1201–1205 (2000).
Graham, D. Y., Malaty, H. M., Cole, R. A., Martin, R. F. & Klein, P. D. Simplified 13C-urea breath test for detection of Helicobacter pylori infection. Am. J. Gastroenterol. 96, 1741–1745 (2001).
Gatta, L. et al. A rapid, low-dose, 13C-urea tablet for the detection of Helicobacter pylori infection before and after treatment. Aliment Pharmacol. Ther. 17, 793–798 (2003).
Kopácová, M. et al. Comparison of different protocols for 13C-urea breath test for the diagnosis of Helicobacter pylori infection in healthy volunteers. Scand. J. Clin. Lab. Invest. 65, 491–498 (2005).
Ortiz-Olvera Nayeli, N. X., Morán Villota, S., Gallardo Wong, I., Blancas Valencia, J. M. & Cabrera Muñoz, L. Validación de método simplificado de la prueba en aliento con urea-13C para diagnóstico de infección por Helicobacter pylori [Validation of a simplified 13C-urea breath test method for the diagnosis of Helicobacter pylori infection]. Rev. Esp. Enferm Dig. 99, 392–397 (2007).
Wong, W. M. et al. (13)C-urea breath test without a test meal is highly accurate for the detection of Helicobacter pylori infection in Chinese. Aliment Pharmacol. Ther. 14, 1353–1358 (2000).
Malfertheiner, P., Megraud, F., Rokkas, T., Gisbert, J. P., Liou, J. M., Schulz, C., Gasbarrini, A., Hunt, R. H., Leja, M., O'Morain, C., Rugge, M., Suerbaum, S., Tilg, H., Sugano, K., El-Omar, E. M., & European Helicobacter and Microbiota Study group. Management of Helicobacter pylori infection: the Maastricht VI/Florence consensus report. Gut. 2022, 327745 (2022).
Schwartz, J. G., Salman, U. A., McMahan, C. A. & Phillips, W. T. Gastric emptying of beer in Mexican-Americans compared with non-Hispanic whites. Metabolism. 45, 1174–1178 (1996).
Graham, D. Y. & Miftahussurur, M. Helicobacter pylori urease for diagnosis of Helicobacter pylori infection: A mini review. J. Adv. Res. 13, 51–57 (2018).
Acknowledgements
This work was supported by the National Natural Science Foundation of China (no. 81700521).
Author information
Authors and Affiliations
Contributions
Gang Chen: performed the experiment, the data analyses and wrote the manuscript; Weiping Zhang, Qiaoling Wu, Wenwu Luo: helped performed the experiment; Qin Yu, Jianming Xu: contributed significantly to analysis and manuscript preparation; Yongping Cai: provide pathological guidance; Lei Zhang, Rutao Hong: helped perform the analysis with constructive discussions. All authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chen, G., Zhang, W., Wu, Q. et al. Application of citric acid can enhance the accuracy for 13C-urea breath tests in the diagnosis of Helicobacter pylori infection in Chinese patients. Sci Rep 14, 14658 (2024). https://doi.org/10.1038/s41598-024-64927-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-64927-3
- Springer Nature Limited