Abstract
Exposures to social and environmental stressors arise individual behavioural response and thus indirectly affect cardiometabolic health. The aim of this study was to investigate several social and environmental stressors and the paths of their influence on cardiometabolic health. The data of 2154 participants (aged 25–64 years) from the cross-sectional population-based study were analysed. The composite score of metabolic disorders (MS score) was calculated based on 5 biomarkers: waist circumference, blood pressure, fasting blood glucose, HDL-cholesterol, triglycerides. The effects of social stressors (education level, income), environmental stressors (NO2, noise) and behavioural factors (unhealthy diet, smoking, alcohol consumption, sedentary behaviours) on MS score were assessed using a structural model. We observed a direct effect of education on MS score, as well as an indirect effect mediated via an unhealthy diet, smoking, and sedentary behaviours. We also observed a significant indirect effect of income via sedentary behaviours. The only environmental stressor predicting MS was noise, which also mediated the effect of education. In summary, the effect of social stressors on the development of cardiometabolic risk had a higher magnitude than the effect of the assessed environmental factors. Social stressors lead to an individual’s unhealthy behaviour and might predispose individuals to higher levels of environmental stressors exposures.
Similar content being viewed by others
Introduction
Cardiovascular diseases (CVD) are globally responsible for the biggest proportion of deaths. In 20191, there were approximately 523 million cases of CVD and 19 million CVD deaths worldwide. In Europe, cardiovascular mortality in the last three decades slightly decreased, from 48% in 1990 to 44% in 2019. The drop was even more noticeable in Czechia, where the proportion of deaths caused by CVD decreased from 55% in 1990 to 45% in 20192. The reduction of cardiovascular mortality can be explained by the improvements in healthcare after the socio-political transformation in the early 90s3 as well as positive changes in the individual lifestyle4,5. Although the CVD mortality rate declined in recent years, the burden of cardiometabolic drivers such as abnormal adiposity and dysglycaemia in the population increased2. Cardiometabolic health is influenced by a complex network of social and environmental stressors6, as demonstrated by the ubiquitous health inequalities in human populations. This complex system of exposures, acting on the background of the human genome, influences morbidity and mortality risk, and it has been recently included in so-called exposome approach to disease7. The exposome concept represents the overall impact of diverse factors on human health and consists of both, external and internal factors8.
The social environment is formed by a complex network of social and economic conditions such as level of education, income, financial deprivation, occupation, social status as well as neighbourhood or cultural characteristics9. People from disadvantaged environments experience higher rates of poor health and disabilities and, therefore, are at a higher risk of premature death9,10,11. Previous studies also reported significant associations between lower socioeconomic position and increased CVD incidence and mortality12,13. Similarly, in a previous study including 8449 subjects from Czechia10, the level of education was identified as the strongest determinant of cardiovascular mortality, followed by hypertension and smoking10. Socioeconomic disadvantages also predispose individuals to increased external stressors exposure including negative life events, lack of resources, life insecurity, limited access to health care, or environmental stressors exposure14,15.
The environmental stressors represent characteristics of the built environment together with the natural condition of the living areas as well as physical and chemical pollution. The built environment consists of aspects built by humans such as urban spaces, access to greenspace, transportation, walkways, etc. Previous studies suggested that living in more walkable, less sprawled areas16 and having good access to greenspace17, are associated with a lower risk of obesity, type 2 diabetes, and hypertension. Physical and chemical pollution refers to short-term and long-term exposures to environmental factors that mostly result from various human activities such as industry, power plants, transportation, or household activities. Air pollution, noise, and heavy metal emissions belong among the most important environmental hazards that affect public health18.
Air pollution is characterized by exposure to PM2.5, PM10, and NO2, which has been previously associated with adverse cardiometabolic health including dysglycaemia19 and hypertension20. The mixed evidence about the relationship between air pollution exposure and adiposity was observed. In a systematic review from 2018, An et al. described that only 56% of assessed studies found a significant relationship between adiposity and air pollution, with the association being positive in 44% of studies and negative in 12%21. The main sources of PM2.5, PM10, and NO2 in urban environment is traffic, which is also a major source of another environmental stressor—noise.
The effect of long-term noise exposure on diverse cardiometabolic health biomarkers has been reported. There is considerable evidence about the association between excessive noise exposure and hypertension22,23 and type 2 diabetes24. Traffic noise has been positively associated also with higher BMI and waist circumference, although the effects were generally small and less consistent25,26,27,28,29.
It is important to consider, that all factors including social and environmental stressors are interconnected. In particular, socioeconomic disadvantage may trigger exposure to other external risk factors9. Similarly, the exposure to social and environmental stressors arises behavioural response and thus indirectly affects health30.
The impact of stressors is even enhanced by their cumulation31 and a wide range of their interactions and pathways. The exposome approach thus offers the concept of complex exposure assessment which can help to identify the pathways by which stressors affect human health and allow us to better understand the aetiology of chronic diseases7,8,32. Despite the large amount of previous literature focused of social and environmental stressors, there is still need for extension of the evidence focused on exposome concept in the exposure assessment. Most of the reported literature focus on the assessment of the individual effect of risk factors, but evidence including a comprehensive view of the entire exposome is limited. For a successful strategy of declining inequalities, a deep understanding of social and environmental stressors and their influence is needed. This study aims to model structural relations between social and environmental stressors and cardiometabolic health.
Methods
Design and population
Data from the Kardiovize study33 were used. The Kardiovize study is an epidemiological study including a random sample of adult residents (aged 25 to 65 years) of the city of Brno, the second-largest city in Czechia, with 373,327 residents. Survey sampling was done in January 2013 with technical assistance from the health insurance companies. A random age and sex-stratified sample of 2154 men and women has been enrolled in the study. No information on non-respondents was available due to confidentiality restrictions.
Data collection
In-person health interviews were performed by trained nurses and physicians at the International Clinical Research Center of the St Anne’s University Hospital in Brno. The questionnaire included demographics, socioeconomic characteristics, cardiovascular risk behaviours, smoking status, medical history, and mental health. The geocode for the living location has been obtained at the street level for 2157 participants and at the district level for 71 participants.
Measures
Cardiometabolic risk
Five cardiometabolic biomarkers were assessed. Waist circumference was measured using manual tape. Blood pressure was measured with the participant alone using an automated office measurement device (BpTRU, model BPM 200; Bp TRU Medical Devices Ltd., Canada). Three measurements were performed and averaged. Laboratory analyses were performed with12-hour fasting full blood samples. The composite score of cardiometabolic risk was calculated based on the presence of metabolic syndrome components. The components of metabolic syndrome were assessed based on the previous definitions34: (1) waist circumference > 94 cm in men or > 80 cm in women; (2) systolic blood pressure > 130 mmHg or diastolic blood pressure > 85 mmHg or the reported use of antihypertensive medication; (3) fasting blood glucose > 5.6 mmol/l or the reported use of antidiabetic medication; (4) HDL-cholesterol < 1.0 mmol/l in men or < 1.3 mmol/l in women or reported use of hypolipidemic medication; (5) triglycerides > 1.7 mmol/l or reported use of hypolipidemic medication. The five components were summed up, and the MS score was created, ranging from 0 to 5 points, with higher scores representing higher cardiometabolic risk.
Social stressors
Education
Educational attainment was classified into three groups: “high”, including subjects with higher professional or university education, where higher professional qualification refers to specialized training beyond secondary education, leading to recognized certification or licensure for specific occupations; “middle”, defined as high school education with a final graduation exam; and “low”, defined as elementary or vocational education without a final graduation exam.
Income
Self-reported household income was assessed in the equalized form to consider the differences in a household’s size and composition. Data about total household income were collected using categories defined by income ranges. The mid value of each range was then used. The equivalized household income was calculated as a ratio of total household income and equivalent size. The equivalent size is calculated by attributing a weight to all members of household in following way: 1.0 for the first person and 0.5 for each subsequent person in the household. The equivalent size is the sum of the weights of all the members of a given household35.
Environmental stressors
Air pollution
To assess the effect of air pollution on cardiometabolic risk, nitrogen dioxide (NO2) exposure was included in the model. For the complete assessment of the effect of air pollution on cardiometabolic health, it would be desirable to also consider the effect of PM10 and PM2.5, however, the variance in their exposure was insufficient, with an interquartile range of 2.90 and 3.75 μg/m3, respectively. Similar variance has been observed in previous study from Brno36.
5 year mean NO2 concentrations for the years 2008–2012 were obtained from air pollution level maps of Czech Hydrometeorological Institute at a spatial resolution of 1 × 1 km37. The pollution maps are interpolated on annual basis from a combination of measured air pollution data, several models of dispersion (primarily CAMx, SYMOS and EMEP), traffic emissions, elevation, and population density (see Škáchová and Vlasáková38 for more details). Ground-level NO2 concentrations were obtained for each residential building at its centroid, and mean, median and standard deviation values of residential buildings’ concentrations were obtained for each street. For the addresses geocoded on the street level, the mean values of residential buildings’ concentrations were used. For the addresses geocoded at the district level, air pollution levels were imputed from 50 buildings nearest to the district centroid.
Noise
The environmental noise exposures were obtained from the results of the prediction model of the 2nd report on Strategic noise mapping in the Czech Republic (2012), conducted in accordance with the environmental noise directive (END) requirements and methods39. Global combined (road, railway, and airport) day-evening-night noise levels (Lden) were calculated for each residential building at its centroid, and mean, median and standard deviation values were obtained for each street. Missing data in the noise prediction model within the borders of the modeled territory were imputed with the lowest category of the noise level. For the addresses geocoded at the district level, noise levels were imputed from 50 buildings nearest to the district centroid.
Behavioural factors
Dietary risk
Dietary risky patterns were assessed using a dietary risk score derived from the 43-item food frequency questionnaire (FFQ). Participants were asked to indicate the frequency of consumption of specific food groups in the past week on a scale including 10 options from “almost never” to “six or more times a day”. In total, six specific risky dietary patterns were identified based on the global burden of disease (GBD)40 methodology (Table 1). The occurrences of each risky dietary patterns were summed, so the total dietary risk score ranged from 0 to 6 points.
Smoking
Smoking status was assessed using the self-report method and categorized as current smokers, ex-smokers, and non-smokers.
Alcohol intake
Alcohol intake was evaluated as the self-reported total amount of ethanol (derived from reported amount of beer, wine and spirits) in grams consumed during the week before data collection.
Sedentary behaviours
Sedentary behaviours were based on total sitting time in minutes per week, obtained from the long version of the international questionnaire of physical activity41 (IPAQ).
Data analysis
Data analyses were performed using STATA42 software (version 16.0, StataCorp, College Station, TX, USA) and MPlus 8.643.Continuous variables were described using means, and categorical variables using frequencies. The Ordinal regression was performed to assess the association between social or environmental factors and cardiometabolic risk score. General structural equation modeling was implemented to describe the pathways and structural relationships between the stressors, and between the stressors and outcome. We constructed structural model with social factors as independent variables determining behavioural factors as well as environmental exposures, and cardiometabolic risk as the main assessed outcome, predicted by social factors directly but also indirectly. Thus, we tested the direct effects of social and environmental stressors on cardiometabolic risk as well as the indirect effects of social stressors through behavioural and environmental mediators. All variables were ordered from the lowest value (the lowest category for ordinal variables) to the highest. All tested associations were further adjusted for sex and age. P values less than 0.05 were considered statistically significant. A complete case analysis method was used for handling missing data.
Ethical statements
The study protocol complied with the Helsinki declaration and all participants signed the informed consent. The study was approved by the ethical committee of St Anne’s University Hospital, Brno, Czech Republic on 13 June 2012 (reference number 2 G/2012).
Results
Subjects’ characteristics
In total, 2154 (54.7% women) subjects were included in the analysis with a mean age of 47.29 years. The descriptive characteristics are shown in Table 2. The most prevalent level of education was high (41.60%). The exposure concentrations to NO2 ranged from 7.80 to 42.30 μg/m3. The noise exposure ranged from 42.50 to 66.97 dB.
The association between stressors and cardiometabolic risk
We tested the total effect of each social, environmental, and behavioural factor on MS score in a separate model using ordinal regression analysis. The results showed that better socioeconomic condition was associated with lower risk of increased MS score. Those with high education level showed 52% lower odds of having higher MS score compared to those with low education level and by every 10,000CZK increase in household income, the odds of higher MS score decreased by 11% (Table 3).
Our results also indicated 34% increase odds of higher MS score with every 10 dB increase in environmental noise exposure. Among behavioural factors, we identified significantly increased odds of higher MS score with increased dietary risk, higher sedentary time and in smokers or ex-smokers compared to non-smokers (Table 3).
The structural model of stressors, behavioural factors, and cardiometabolic risk
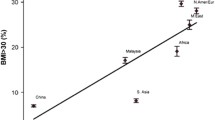
The results of structural model showed that higher level of education significantly predicted increased income and decreased dietary risk and decreased smoking. However, at the same time, higher education was associated with increased sedentary behaviours (Table 4). The only environmental stressor significantly predicting higher MS score was noise (β = 0.050; 95% CI [0.004, 0.092]) (Fig. 1, Table 4).
Observed statistically significant relationships in complex structural model. Bold values represent direct and the indirect effect through specific mediator. Reported results significant at p < 0.05. Dotted lines represent tested but statistically non-significant relationships (at 5% level of significance).
We observed a significant direct effect of higher education on MS score (β = − 0.117; 95% CI [− 0.161, − 0.073], as well as an indirect effect mediated via dietary risk (β = − 0.0153; 95% CI [− 0.024, − 0.008]), smoking (β = − 0.017; 95% CI [− 0.032, − 0.005]), sedentary behaviours (β = 0.014; 95% CI [0.008, 0.024]) and noise exposure (β = − 0.003; 95% CI [− 0.007, − 0.001]). We also observed significant indirect effect via the path including income and sedentary behaviours as successive mediators. The total mediation ratio was 21.0% (Table 5). Although we did not observe a statistically significant direct effect of income on MS score, the results showed a significant indirect effect of higher income via sedentary behaviours (β = 0.013; 95% CI [0.007, 0.021]) (Table 5).
As a sensitivity analysis, we run the sex-stratified analysis (Supplementary Table 1). In men, we observed slightly higher effect of smoking and lower effect of dietary risk on MS score, compared to women. Similarly, in women, we observed higher effect of income and lower effect of education on sedentary, compared to men. In men and women, the overall indirect effects were − 0.040 (p = 0.032) and − 0.037 (p = 0.017) with a mediation ratio of 25.3% and 26.8%, respectively. In general, the overall differences between men and women are small, therefore we included the full results in supplementary materials.
Discussion
The purpose of this study was to investigate the network of social and environmental stressors and the paths of their effect on cardiometabolic risk. Lower level of education was associated with increased cardiometabolic risk but also with smoking and unhealthy dietary patterns as well as increased exposure to environmental noise, which all together contribute to cardiometabolic risk. On the contrary, higher levels of education was associated with increased sedentary behaviours, also associated with increased cardiometabolic risk. Sedentary behaviours, therefore, potentially decreased the protective effect of higher education on cardiometabolic risk. Additionally, sedentary behaviour was identified as a significant mediator of increased cardiometabolic risk in individuals with higher income though income itself was not directly associated with cardiometabolic risk.
The direct effect of social determinants on health is driven by physiological responses to stress, arising from disadvantageous life environment. People with disadvantaged socioeconomic position exhibit more physiological stress44 which therefore lead to the internal dysregulation and increased cardiometabolic risk.
The indirect effect of social determinants may be mediated through several pathways. In our study, we investigated the mediating role of behavioural factors and environmental exposures. The increased prevalence of inappropriate lifestyle in socio-economically disadvantaged group has been previously described. According to previous literature, socio-economically disadvantaged groups develop and exhibit more unhealthy behaviours, such as tobacco use, excessive alcohol use, physical inactivity, and poor nutrition45. At the same time, lower education may be reflected in reduced knowledge-related skills and limited health literacy46, which all together again trigger unhealthy behaviours. Additionally, according to the previous studies, disadvantaged populations live in less prestigious neighbourhoods with limited resources that may be reflected for instance in lower availability of sport facilities and greenspaces47,48,49, increased exposure to unhealthy diet options47,50,51,52,53 and higher environmental pollution15. Therefore, we can assume that unhealthy behaviour as cardiometabolic risk factors arise from socio-economic disadvantage and at the same time, behavioural response may partially explain social inequalities in cardiometabolic health. However, we cannot neglect the role of sedentary behaviour, which is, on the contrary, a cardiometabolic risk factor linked to socioeconomic advantage. The increasing prevalence of sedentary behaviours in recent years54 could in the future lead to increase of burden of cardiometabolic risk in higher socioeconomic groups.
The second investigated path included environmental exposure as mediators of the effect of social determinants on cardiometabolic risk. Previous studies reported that socioeconomic disadvantage may predispose individuals to increased environmental exposures9. The United States Environmental Protection Agency (US EPA) acknowledged that that environmental exposures are considered as an additional health burden to these disadvantaged groups. Several societies have addressed this issue by adopting specific plans to strengthen environmental justice55. We investigated the role of long-term air pollution exposure (NO2) and environmental noise exposure. Our results showed no significant association between long-term NO2 exposure on cardiometabolic risk. Even though the exposures have been historically relatively low in city of Brno (IQR = 20.40–29.95) compared to capitols and big cities in Europe, the concentrations still exceeded the Air Quality Guideline (annual NO2 = 10 μg/m3) recommended by WHO in 2021. On the other hand, the effects of low-level exposures on cardiometabolic outcomes have been generally very weak in previous studies. For instance, a study of the Dutch national health survey represented by more than 380,000 adults showed that NO2 exposure predicted only 6% odds (OR = 1.06; 95% CI 1.04–1.09) of diabetes and 2% odds (OR = 1.06; 95% CI 1.04–1.09) for hypertension56. Therefore, we assume that our inconclusive results might be caused by relatively low study power as well as low exposure variance in the area.
The environmental noise was the only environmental stressor identified as mediator of the association between social determinants and cardiometabolic risk. The effect of long-term noise exposure on cardiometabolic health has been previously investigated. There is evidence about the association between excessive noise exposure and hypertension22,23, as well as type 2 diabetes24 and waist circumference25. Previous studies also suggested several underlying mechanisms of reported associations. Environmental noise exposure influence haemostasis and vascular function and incites oxidative stress as well as systematic inflammation57. Long-term environmental noise exposure also causes sleep deprivation which may lead to other physiological or psychological consequences57. Based on our results, we may assume that noise exposure associated with urban life environment is another explanation of social inequalities in cardiometabolic health.
The major strength of the present study is the complex approach of cardiometabolic risk assessment, including multiple measures of cardiometabolic health. Also, we examined a wide spectrum of healthy behaviour risk factors as well as two important environmental exposures. Furthermore, we included confounding and mediation analyses that contributed to reveal important interplay mechanisms between socioeconomic, behavioural and environmental stressors of cardiometabolic health. However, there are some limitations of this study that deserve to be mentioned. First, the cross-sectional design of the study does not allow for evaluating causality, thus the direction of the associations set in the structural model was constructed based on previous evidence, and reverse causation bias might occur. Second, we had no information about the year of onset of risky levels of cardiometabolic biomarkers, therefore, we may not be sure whether exposures precede the heath outcome. Third, the residential mobility of the participants may lead to under- or over-estimation of the exposure levels. Forth, study sample probably did not provide enough study power to reveal a significant association between air pollution exposure and cardiometabolic risk. Moreover, occupational exposures have not been considered due to data unavailability. Fifth, the study sample only included a city-based population; thus, the study findings should not be generalized beyond the urban population. Additionally, the study population included only White Europeans, thereby limiting the generalizability of the findings for other ethnicities.
Conclusion
This study highlights the intricate network of social and environmental stressors and their impact on cardiometabolic risk. Lower levels of education were found to directly increase cardiometabolic risk while also predisposing individuals to unhealthy behaviours such as smoking and poor dietary patterns. Additionally, lower education levels were associated with increased exposure to environmental noise, further contributing to cardiometabolic risk. On the other hand, higher levels of education and income were linked to increased sedentary behaviours, which diminished the protective potential against cardiometabolic risk. The findings emphasize the role of both physiological responses to stress and behavioural factors in the direct and indirect effects of social determinants on health. Moreover, environmental exposures, particularly long-term noise exposure, were identified as mediators of the association between social determinants and cardiometabolic risk. Nevertheless, this study underscores the importance of addressing social inequalities and environmental factors to improve public health outcomes related to cardiometabolic risk.
Data availability
The data that support the findings of this study are available from ICRC—FNUSA but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are available from Juan Pablo Gonzalez Rivas upon reasonable request and with permission of ICRC-FNUSA.
References
Roth, G. A. et al. Global burden of cardiovascular diseases and risk factors, 1990–2019: Update from the GBD 2019 study. J. Am. Coll. Cardiol. 76, 2982–3021 (2020).
Institute for Health Metrics and Evaluation (IHME). GBD Compare. University of Washington. https://vizhub.healthdata.org/gbd-compare/ (2015).
Dzúrová, D. Mortality differentials in the Czech Republic during the post-1989 socio–political transformation. Health Place 6, 351–362 (2000).
Žejglicová, K., Kratěnová, J., Lustigová, M. & Malý, M. Trends in health indicators in the urban middle-aged population in the Czech Republic in 1998–2010. Public Health 137, 81–87 (2016).
Cífková, R. et al. 30-year trends in major cardiovascular risk factors in the Czech population, Czech MONICA and Czech post-MONICA, 1985–2016/17. PLoS One 15, e0232845 (2020).
Juarez, P. D., Hood, D. B., Song, M. A. & Ramesh, A. Use of an exposome approach to understand the effects of exposures from the natural, built, and social environments on cardio-vascular disease onset, progression, and outcomes. Front. Public Health https://doi.org/10.3389/fpubh.2020.00379 (2020).
Vrijheid, M. The exposome: A new paradigm to study the impact of environment on health. Thorax 69, 876–878 (2014).
Wild, C. P. The exposome: From concept to utility. Int. J. Epidemiol. 41, 24–32 (2012).
Marmot, M. & Allen, J. J. Social determinants of health equity. Am. J. Public Health 104, S517–S519 (2014).
Lustigova, M., Dzurova, D., Pikhart, H., Kubinova, R. & Bobak, M. Cardiovascular health among the Czech population at the beginning of the 21st century: A 12-year follow-up study. J. Epidemiol. Community Health 1978(72), 442–448 (2018).
Marmot, M. & Bell, R. Social determinants and non-communicable diseases: time for integrated action. BMJ https://doi.org/10.1136/bmj.l251 (2019).
Wang, T., Li, Y. & Zheng, X. Association of socioeconomic status with cardiovascular disease and cardiovascular risk factors: A systematic review and meta-analysis. J. Public Health (Bangkok) https://doi.org/10.1007/s10389-023-01825-4 (2023).
Wang, S., Zhai, H., Wei, L., Shen, B. & Wang, J. Socioeconomic status predicts the risk of stroke death: A systematic review and meta-analysis. Prev. Med. Rep. 19, 101124 (2020).
Siew, R. V. K., Nabe-Nielsen, K., Turner, A. I., Bujtor, M. & Torres, S. J. The role of combined modifiable lifestyle behaviors in the association between exposure to stressors and allostatic load: A systematic review of observational studies. Psychoneuroendocrinology 138, 105668 (2022).
Bowen, W. An analytical review of environmental justice research: What do we really know?. Environ. Manag. 29, 3–15 (2002).
Chandrabose, M. et al. Built environment and cardio-metabolic health: Systematic review and meta-analysis of longitudinal studies. Obes. Rev. 20, 41–54 (2019).
Yang, B.-Y. et al. Greenspace and human health: An umbrella review. The Innovation 2, 100164 (2021).
González Ortiz, A., Guerreiro, C., Soares, J. & European Environment Agency. Air Quality in Europe : 2020 Report.
Li, X. et al. Obesity and the relation between joint exposure to ambient air pollutants and incident type 2 diabetes: A cohort study in UK Biobank. PLoS Med. 18, e1003767 (2021).
Yang, B. Y. et al. Global association between ambient air pollution and blood pressure: A systematic review and meta-analysis. Environ. Pollut. 235, 576–588 (2018).
An, R., Ji, M., Yan, H. & Guan, C. Impact of ambient air pollution on obesity: A systematic review. Int. J. Obes. 42, 1112–1126 (2018).
Dzhambov, A. M. & Dimitrova, D. D. Residential road traffic noise as a risk factor for hypertension in adults: Systematic review and meta-analysis of analytic studies published in the period 2011–2017. Environ. Pollut. 240, 306–318 (2018).
Bolm-Audorff, U. et al. Occupational noise and hypertension risk: A systematic review and meta-analysis. Int. J. Environ. Res. Public Health 17, 6281 (2020).
Zare Sakhvidi, M. J., Zare Sakhvidi, F., Mehrparvar, A. H., Foraster, M. & Dadvand, P. Association between noise exposure and diabetes: A systematic review and meta-analysis. Environ. Res. 166, 647–657 (2018).
An, R., Wang, J., Ashrafi, S. A., Yang, Y. & Guan, C. Chronic noise exposure and adiposity: A systematic review and meta-analysis. Am. J. Prev. Med. 55, 403–411 (2018).
Oftedal, B. et al. Road traffic noise and markers of obesity—A population-based study. Environ. Res. 138, 144–153 (2015).
Christensen, J. S. et al. Long-term exposure to residential traffic noise and changes in body weight and waist circumference: A cohort study. Environ. Res. 143, 154–161 (2015).
Christensen, J. S. et al. Road traffic and railway noise exposures and adiposity in adults: A cross-sectional analysis of the danish diet, cancer, and health cohort. Environ. Health Perspect. 124, 329–335 (2016).
Dzhambov, A. et al. Association between community noise and adiposity in patients with cardiovascular disease. Noise Health 19, 270 (2017).
Frank, L. D., Iroz-Elardo, N., MacLeod, K. E. & Hong, A. Pathways from built environment to health: A conceptual framework linking behavior and exposure-based impacts. J. Transp. Health 12, 319–335 (2019).
Williams, P. R. D., Dotson, G. S. & Maier, A. Cumulative risk assessment (CRA): Transforming the way we assess health risks. Environ. Sci. Technol. 46, 10868–10874 (2012).
Beulens, J. W. J. et al. Environmental risk factors of type 2 diabetes—An exposome approach. Diabetologia 65, 263–274 (2022).
Movsisyan, N. K. et al. Kardiovize Brno 2030, a prospective cardiovascular health study in Central Europe: Methods, baseline findings and future directions. Eur. J. Prev. Cardiol. 25, 54–64 (2018).
Nilsson, P. M., Tuomilehto, J. & Rydén, L. The metabolic syndrome—What is it and how should it be managed?. Eur. J. Prev. Cardiol. 26, 33–46 (2019).
Eurostat. Glossary: Equivalised disposable income (2021).
Šulc, L. et al. City-scale assessment of long-term air quality impacts on the respiratory and cardiovascular health. Front. Public Health https://doi.org/10.3389/fpubh.2022.1006536 (2022).
ČHMU. Pětileté průměrné koncentrace. https://www.chmi.cz/files/portal/docs/uoco/isko/ozko/ozko_CZ.html (2022).
Škáchová, H. & Vlasáková, L. Air pollution in the Czech Republic in 2019 overall editing (2020).
The European parliament and The Council of the European Union. Directive 2002/49/EC Of The European Parliament And Of The Council (2002).
Afshin, A. et al. Health effects of dietary risks in 195 countries, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 393, 1958–1972 (2019).
Craig, C. L. et al. International physical activity questionnaire: 12-country reliability and validity. Med. Sci. Sports Exerc. 35, 1381–1395 (2003).
StataCorp. Stata Statistical Software: Release 16 (2019).
Muthén, L. K. & Muthén, B. O. Statistical analysis with latent variables user’s guide. www.StatModel.com (2017).
Cohen, S., Doyle, W. J. & Baum, A. Socioeconomic status is associated with stress hormones. Psychosom. Med. 68, 414–420 (2006).
Pampel, F. C., Krueger, P. M. & Denney, J. T. Socioeconomic disparities in health behaviors. Annu. Rev. Sociol. 36, 349–370 (2010).
Svendsen, M. T. et al. Associations of health literacy with socioeconomic position, health risk behavior, and health status: A large national population-based survey among Danish adults. BMC Public Health https://doi.org/10.1186/s12889-020-08498-8 (2020).
Coutinho, S. R., Andersen, O. K., Lien, N. & Gebremariam, M. K. Neighborhood deprivation, built environment, and overweight in adolescents in the city of Oslo. BMC Public Health 23, 812 (2023).
Gordon-Larsen, P., Nelson, M. C., Page, P. & Popkin, B. M. Inequality in the built environment underlies key health disparities in physical activity and obesity. Pediatrics 117, 417–424 (2006).
Estabrooks, P. A., Lee, R. E. & Gyurcsik, N. C. Resources for physical activity participation: Does availability and accessibility differ by neighborhood socioeconomic status?. Ann. Behav. Med. 25, 100–104 (2003).
Black, C., Moon, G. & Baird, J. Dietary inequalities: What is the evidence for the effect of the neighbourhood food environment?. Health Place 27, 229–242 (2014).
Pinho, M. G. M. et al. Recent changes in the Dutch foodscape: Socioeconomic and urban-rural differences. Int. J. Behav. Nutr. Phys. Act. 17, 43 (2020).
Maguire, E. R., Burgoine, T. & Monsivais, P. Area deprivation and the food environment over time: A repeated cross-sectional study on takeaway outlet density and supermarket presence in Norfolk, UK, 1990–2008. Health Place 33, 142–147 (2015).
Hemphill, E., Raine, K., Spence, J. C. & Smoyer-Tomic, K. E. Exploring obesogenic food environments in Edmonton, Canada: The association between socioeconomic factors and fast-food outlet access. Am. J. Health Promot. 22, 426–431 (2008).
López-Valenciano, A. et al. Changes in sedentary behaviour in European Union adults between 2002 and 2017. BMC Public Health https://doi.org/10.1186/s12889-020-09293-1 (2020).
U.S. Environmental Protection Agency. Plan Environmental Justice 2014 (2011).
Klompmaker, J. O. et al. Associations of combined exposures to surrounding green, air pollution, and road traffic noise with cardiometabolic diseases. Environ. Health Perspect. https://doi.org/10.1289/EHP3857 (2019).
Chen, X. et al. Environmental noise exposure and health outcomes: An umbrella review of systematic reviews and meta-analysis. Eur. J. Public Health https://doi.org/10.1093/eurpub/ckad044 (2023).
Funding
This work has received funding under grant agreement No 857487 (R-Exposome Chair) and was supported under grant agreement No 857560 (CETOCOEN Excellence) from the European Union’s Horizon 2020 research and innovation programme. This publication reflects only the author’s view, and the European Commission is not responsible for any use that may be made of the information it contains. Authors thank the RECETOX Research Infrastructure (No LM2023069) financed by the Ministry of Education, Youth and Sports for supportive background. This output was supported by the NPO “Systemic Risk Institute” number LX22NPO5101, funded by European Union—Next Generation EU (Ministry of Education, Youth and Sports, NPO: EXCELES).
Author information
Authors and Affiliations
Contributions
AB, AD, and HP conceived and designed the study. AB and DS analysed the data. AB wrote the first draft of the manuscript with a support of AD and HP. HP, MB and JG provided critical revisions. All authors read and approved the submitted manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bartoskova Polcrova, A., Dalecka, A., Szabo, D. et al. Social and environmental stressors of cardiometabolic health. Sci Rep 14, 14179 (2024). https://doi.org/10.1038/s41598-024-64847-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-64847-2
- Springer Nature Limited