Abstract
Proteinuria poses a substantial risk for the progression of chronic kidney disease (CKD) and its related complications. Kidneys excrete hundreds of individual proteins, some with a potential impact on CKD progression or as a marker of the disease. However, the available data on specific urinary proteins and their relationship with CKD severity remain limited. Therefore, we aimed to investigate the urinary proteome and its association with kidney function in CKD patients and healthy controls. The proteomic analysis of urine samples showed CKD stage-specific differences in the number of detected proteins and the exponentially modified protein abundance index for total protein (p = 0.007). Notably, specific urinary proteins such as B2MG, FETUA, VTDB, and AMBP exhibited robust negative associations with kidney function in CKD patients compared to controls. Also, A1AG2, CD44, CD59, CERU, KNG1, LV39, OSTP, RNAS1, SH3L3, and UROM proteins showed positive associations with kidney function in the entire cohort, while LV39, A1BG, and CERU consistently displayed positive associations in patients compared to controls. This study suggests that specific urinary proteins, which were found to be negatively or positively associated with the kidney function of CKD patients, can serve as markers of dysfunctional or functional kidneys, respectively.
Similar content being viewed by others
Introduction
Chronic kidney disease (CKD) is one of the leading global health challenges, imposing a substantial burden on society. Recent studies show that around 10% of people in developed countries are affected by CKD, mainly people over 65 years of age, due to comorbidities and age-related factors1,2. Over the last three decades, CKD-related mortality has increased by almost 1% yearly, becoming a serious global health issue3,4. Unfortunately, the disease is projected to become the fifth leading cause of death by 20405. This is a concerning trend that highlights its impact on global mortality rates. Contributing factors to the increase in CKD-related mortality include the aging population and the rise of CKD-causing diseases, including diabetes and arterial hypertension6. Also, late diagnosis of CKD and the financial burden associated with initiating treatments at advanced stages exacerbate CKD progression, leading to end-stage kidney disease (ESKD) and cardiovascular complications.
Therefore, early detection and intervention are essential to address these challenges. Lifestyle modifications and medications, such as SGLT2 inhibitors and renin–angiotensin–aldosterone modulators, have shown promise in preserving kidney function7.
Notably, biomarkers, particularly proteinuria, are crucial in identifying and managing CKD. The levels of proteinuria serve as a marker for disease progression and associated outcomes in non-diabetic and diabetic individuals8. Higher proteinuria levels often correlate with rapid CKD progression9. However, clinical observations indicate that some patients with high proteinuria experience a slower decline in kidney function compared to those with lower levels of urinary protein excretion. This variability suggests that the toxic properties of the filtered proteins, rather than just the quantity, play a significant role in influencing the disease progression10,11. For example, filtered albumin has been reported to promote cellular reactive oxygen species-mediated tubulointerstitial inflammation and endothelin-1-mediated tubulointerstitial fibrosis11. Thus, identifying potential toxic urinary proteins associated with kidney function and understanding its pathophysiological mechanisms are crucial for early CKD detection11.
Urine proteomics holds promise in understanding CKD. It offers insights into dynamic protein changes and potential biomarkers for disease identification. Previous proteomic investigations have revealed numerous potential biomarkers for CKD. However, these studies frequently focused on analyzing blood proteins12 or spot urine samples13,14, potentially limiting their representativeness.
Therefore, the urinary proteome extracted from 24-h urine samples was analyzed in this study. This methodology provides a more comprehensive and stable representation of the dynamic proteome changes associated with CKD disease. Our study aimed to compare the urinary protein profiles of CKD patients with stages 1–3 and healthy participants. The objective was to identify potential biomarkers for clinical use and deepen our understanding of CKD's progression via molecular mechanisms.
Materials and methods
Patients and study design
In this cross-sectional study, we enrolled 88 patients with CKD and 49 age-matched healthy controls. Participants with CKD were identified during hospital admission and/or nephrology consultation at the National Scientific Medical Center (NSMC, Astana, Kazakhstan) and were recruited between March 2020 and December 2022. Age-matched healthy controls were volunteers recruited at the same hospital setting after advertising the invitation to this research study.
We included individuals aged ≥ 18 and ≤ 70 years old with CKD stages 1–3, categorized by eGFR according to KDIGO 2012 guidelines15. Diagnosis relied on eGFR, kidney damage markers, and clinical evaluation due to the unavailability of kidney biopsies. Kidney function was assessed using the serum creatinine-based eGFR via the 2021 CKD-EPI (CKD Epidemiology Collaboration) equation16. Control participants had no clinical or laboratory indicators of CKD, hypertension, or other known diseases. Exclusions comprised age outside the 18–70 range, eGFR < 60 mL/min for controls, and eGFR < 30 mL/min for patients, presence of acute infections, cancer, and pregnancy.
Written informed consent was obtained from all the study participants. This study was approved by the Nazarbayev University Institutional Review Ethics Committee (NU-IREC 208/06122019) and registered in ClinicalTrials.gov as a part of a clinical trial (ID NCT04311684)17. Based on good medical and laboratory practice, all the principles of the Declaration of Helsinki for Biomedical Research Involving Human Participants were met during patient examinations.
Laboratory tests
Sample collection procedures were conducted independently of patient prognoses. All laboratory personnel involved were blinded to the clinical outcomes. Blood samples were used for complete blood count and biochemical analyses, assessing various metabolic parameters such as glucose, lipids, urea, creatinine, uric acid, and total protein.
Moreover, 24-h urine samples were used for biochemical analysis to determine total protein levels. The blood and urine clinical laboratory analyses were performed using a colorimetric method on a COBAS Integra 400 plus analyzer (Roche Diagnostics, Indianapolis, Indiana, United States) at the NSMC.
The remaining urine samples were stored at − 80 °C and subsequently utilized for proteomics analysis at the National Center for Biotechnology (NCB) in Astana. The proteomics process involved extracting protein from 24-h urine samples using an acetone precipitation method18. Proteins were resuspended and stored at − 80 °C before concentration measurement with a NanoDrop 1000 (Thermo Scientific, Waltham, Massachusetts, United States). In-solution protein digestion was performed with protein concentrations ranging from 30 to 50 μg.
Mass spectrometry analysis
Urinary proteins underwent trypsin digestion (20 ng/μL) at 37 °C overnight following reduction and alkylation. Peptide mixtures were purified and concentrated using a ZipTip with 0.6 μL C18 resin (Millipore, Burlington, Massachusetts, United States). Eluted peptides were processed with a centrifugal evaporator (Eppendorf, Hamburg, Germany), resuspended in 16 μL of 0.1% trifluoroacetic acid, and 15.5 μL of the sample was loaded into a liquid chromatography-tandem mass spectrometry (LC–MS/MS) machine.
Chromatography was performed using a Dionex HPLC pump with an Acclaim PepMap100 C18 pre-column and Acclaim PepMap100 C18 RSLC column (Thermo Scientific, Waltham, Massachusetts, United States). The samples were analyzed using a nanoflow reversed-phase C18 LC–MS/MS instrument. The Impact II ESI-QUAD-TOF mass spectrometer (Bruker Daltonics, Bremen, Germany) with a whole captive spray ion source was utilized for analyzing digested urinary proteins, operating at parameters such as dry temperature 150 °C, dry gas 3.0 L/min, capillary 1500 V.
Full-scan MS spectra were obtained at a 2.0 Hz spectral rate, followed by one MS/MS spectrum. Data Analysis 3.4 software (Bruker Daltonics, Bremen, Germany) was used to analyze the retrieved MS/MS data, saved in Mascot generic format (*.mgf).
Proteins and peptides were identified using Mascot 2.6.1 software (Matrix Science, London, UK) against the Swiss-Prot database (release February 2021), which was taxonomically restricted to Homo sapiens. The following parameters were applied to the search in the Mascot software: carbamidomethylation of cysteine residues as the fixed modification and oxidation of methionine as the variable modification; the maximum missed cleavages of tryptic peptides were set to two; peptides and proteins were identified with two significance thresholds: P < 0.05 and P < 0.001. The decoy database search was used for the false discovery rate (FDR) estimation, and the FDR was set to 1%. Allowed mass error windows for MS and MS/MS were 100 ppm and 0.05 Da, respectively. The Exponentially Modified Protein Abundance Index (emPAI) was used for label-free peptide quantification19.
The proteomic dataset underwent log2-transformation and average and slope-based normalization steps to ensure data consistency and integrity for subsequent analyses.
Gene Ontology (GO) enrichment analysis
The significant GO terms associated with negatively and positively correlated proteins with eGFR, adjusted for proteinuria, were identified using the org.Hs.eg.db20 and clusterProfiler21 packages in R. Proteins from both correlation and regression analyses were considered. The enrichGO function was used for the enrichment analysis, categorizing negatively and positively associated proteins based on their involvement in biological processes, cellular components, and molecular functions. The FDR cutoff of 0.05 was considered.
Reactome pathway analysis
The pathways associated with negatively and positively correlated proteins with eGFR, adjusted for proteinuria, were identified using the ReactomePA package22 in R. Proteins from both correlation and regression analyses were considered. The enrichPathway function was used to identify significantly enriched pathways with P value < 0.05 and an adjusted q value < 0.05.
Protein–protein interaction analysis
STRING-DB (version 12)23 was utilized to explore protein–protein interactions. The corresponding gene identifiers of negatively and positively correlated proteins with eGFR, adjusted for proteinuria, were input into the STRING web platform, enabling the exploration of known and predicted protein interactions from various sources, including experimental data, co-expression, and text mining.
Data visualization
The visualization was created using the ggplot2 package24 in R. A heatmap was generated to represent the presence of proteins in control and CKD 1–3 groups. Also, volcano plots were generated to visualize the relationship between eGFR and urinary proteins, depicting significance levels and coefficients. The top enriched GO terms and Reactome pathways were also visualized. Bar plots were generated to demonstrate the most significantly enriched biological processes and pathways for up and downregulated protein sets. The results were reported in -log10 scale to enhance visual clarity.
Statistical analyses
Statistical analyses were performed using Stata MP2 18. Normally distributed numeric variables were presented as mean ± standard deviation (SD) and non-normally distributed variables as the median and interquartile range (IQR). A two-sided t-test and Wilcoxon rank-sum test were used to analyze parametric and non-parametric data between CKD patients and healthy control group (CG). Moreover, patients were categorized into three CKD stage groups; therefore, one-way ANOVA and Kruskal–Wallis tests were used to analyze parametric and non-parametric data between multiple groups. A chi-square test was used to analyze categorical variables, and they were reported as numbers and percentages. Furthermore, Spearman’s correlation test was used to identify the association of the urinary proteome with kidney function (i.e., eGFR). In addition, linear regression analysis was carried out using eGFR and urinary proteome data to determine the influence of proteins on kidney function. Furthermore, regression analysis between eGFR and urinary proteome was performed, adjusting for the amount of 24-h urine protein.
Prior presentation
Parts of this study were presented at the ISN WCN 2022 and HUPO 2023 Congresses.
Results
Clinical and biochemical characteristics of study population
In our study, we categorized participants into CKD risk groups and stages 1, 2, and 3 (Supplementary Table 1). Both groups were age-matched, with mean ages of 38.6 years (SD = 12.3) for patients and 37.2 years (SD = 7.9) for the control group. The patient group included 48% females and 52% males, while the control group included 69% females and 31% males. Analysis of clinical and biochemical parameters at different stages of CKD showed marked differences between the CKD groups as compared to the control group (Table 1). Notably, metabolic markers, including serum urea and glucose, showed significant variations (P < 0.001 and P = 0.001, respectively), emphasizing the systemic impact of CKD on metabolic homeostasis. Proteinuria was higher in patients with more advanced stages of CKD (Table 1).
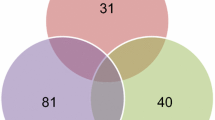
The proteomic analysis of urine samples revealed significant differences in the number of detected proteins and exponentially modified protein abundance index (emPAI) for total protein between the control and patient groups (P = 0.007; Table 1). Additionally, marked differences in the distribution of different protein types were observed across the control and CKD groups (Fig. 1). The number of detected proteins was higher in healthy controls compared to the CKD group, and a lower number of proteins was observed in patients with more advanced stages of CKD (Table 1 and Fig. 1).
Heatmap of distribution rate of proteins in the control and patient groups. Each row on the Y-axis corresponds to a specific protein, while the X-axis columns represent different groups. The color intensity in each heatmap cell reflects the percentage of protein occurrence within the respective sample group, with higher values and color intensity indicating a higher detection rate in that group. CKD = chronic kidney disease.
Urinary proteins correlated with kidney function
The correlation analysis between urinary proteome and kidney function showed that some urinary proteins were correlated with eGFR among all study participants (Table 2). In particular, proteins FETUA, B2MG, IGK, KVD20, IGL1, VTDB, and IGHA1 exhibited negative correlations, while proteins IC1, CLUS, VMO1, VTNC, CD59, REG1A, KNG1, LV39, CD44, SH3L3, OSTP, A1AG2, CERU, RNAS1, UROM, and PTGDS were positively correlated with eGFR. While statistically significant, these correlations were predominantly moderate in magnitude.
Then, correlation analysis was conducted separately in CKD and control participants to identify differences between the two groups (Table 3). In CKD patients, FETUA, B2MG, AMBP, and VTDB proteins were negatively correlated, while LV39, CD59, A1BG, and CERU were positively correlated with eGFR levels. Among control participants, ATRN, SAP, and LG3BP protein were negatively correlated, and PGRP1 and CRNN were positively correlated with eGFR. The average emPAI values of identified proteins between the two groups are depicted in Supplementary Table 2.
Association of urinary proteome with kidney function
Following the correlation analysis, regression analysis was performed to investigate the specific association of proteins (correlated with eGFR) with kidney function (Fig. 2). Among the correlated proteins, B2MG, FETUA, IGK, and VTDB showed a negative coefficient with eGFR of all participants, while A1AG2, CD44, CD59, CERU, KNG1, LV39, OSTP, PTGDS, REG1A, RNAS1, SH3L3, UROM, VMO1, and VTNC exhibited a positive coefficient with eGFR (Fig. 2A and Supplementary Table 3).
Volcano plot showing association between eGFR and emPAI of proteins. Regression analysis in all participants (A) and in patient (B) and control groups (C). On the X-axis, coefficient values show the relationship of individual proteins with eGFR, while the Y-axis conveys -log10-transformed P values for proteins with adjusted P values < 0.05. In the volcano plot, red dots indicate proteins positively associated with eGFR and P < 0.05. Blue dots indicate proteins negatively associated with eGFR and P < 0.05. Gray dots represent proteins that lack statistical significance in their association with eGFR.
Furthermore, regression analysis was performed separately in CKD and control groups to identify the specific association of proteins (correlated with eGFR) with kidney function within each group. In CKD patients, correlated proteins such as B2MG, FETUA, IGK, AMBP, and VTDB showed a negative coefficient with eGFR, while LV39, CD59, A1BG, and CERU exhibited a positive coefficient (Fig. 2B). Among control participants, ATRN, SAP, and LG3BP protein showed a negative coefficient with eGFR, and only CRNN exhibited a positive coefficient with eGFR (Fig. 2C).
Additionally, a regression analysis, adjusting for 24-h proteinuria, was performed to examine the association between eGFR and urinary proteins (Fig. 3). After adjustment for 24-h proteinuria, the correlated proteins B2MG, FETUA, IGK, and VTDB exhibited negative coefficients, while A1AG2, CD44, CD59, CERU, KNG1, LV39, OSTP, RNAS1, SH3L3, and UROM exhibited positive coefficients in the whole cohort (Fig. 3A and Supplementary Table 4).
Volcano plot showing association between eGFR and emPAI of proteins adjusted for proteinuria. Regression analysis in all participants (A) and in patient (B) and control groups (C). On the X-axis, coefficient values show the relationship of individual proteins with eGFR, while the Y-axis conveys -log10-transformed P values for proteins with adjusted P values < 0.05. In the volcano plot, red dots indicate proteins positively associated with eGFR and P < 0.05. Blue dots indicate proteins negatively associated with eGFR and P < 0.05. Gray dots represent proteins that lack statistical significance in their association with eGFR.
In separate regression analysis, B2MG, FETUA, AMBP, and VTDB proteins consistently showed a negative coefficient with eGFR, while LV39, A1BG, and CERU exhibited positive coefficients in the patient group (Fig. 3B). In the control group, ATRN, SAP, and LG3BP protein consistently showed a negative coefficient with eGFR, and only CRNN consistently exhibited a positive coefficient with eGFR (Fig. 3C).
Gene Ontology (GO) enrichment analysis
The GO analysis based on biological processes showed that negatively associated proteins with eGFR demonstrated notable enrichment in retina homeostasis, tissue homeostasis, anatomical structure homeostasis, and immune response-related biological processes in the CKD group (Fig. 4). Conversely, positively associated proteins showed marked enrichment in the regulation and negative regulation of endopeptidase activity, negative regulation of proteolysis, negative regulation of hydrolase activity, negative regulation of peptidase activity, humoral immune response, hemostasis, and coagulation system processes in the CKD group.
The top 10 terms for each GO category and associated proteins with kidney function. Each point represents a GO term listed on the left Y-axis. The size of the points corresponds to the count of proteins enriched in the respective term, and the color represents the adjusted P value significance. The plot is characterized by ontology categories, including biological process (BP), cellular component (CC), and molecular function (MF). The top 10 enriched terms for each category and the direction of negatively and positively associated proteins are highlighted.
The GO analysis based on cellular components exhibited prominently enriched blood microparticle, IgA immunoglobulin immunocomplex, and IgG immunoglobulin immunocomplex only in patients.
The GO analysis based on molecular functions showed that negatively associated proteins were enriched in antigen binding, while positively associated proteins exhibited enrichment in extracellular matrix structural constituent, glycosaminoglycan binding, in patients.
Pathway enrichment analysis
Pathway enrichment analysis of the negatively and positively associated proteins with eGFR adjusted for proteinuria showed that negatively associated proteins were enriched in pathways related to the immune system, including neutrophil degranulation in patients (Table 4). Furthermore, immune system regulation-related pathways, such as regulation of the complement system, complement cascade, and homeostasis-related pathways, such as response to elevated platelet cytosolic Ca2+, platelet activation, signaling and aggregation, and fibrin clot pathways, were enriched by positively associated proteins in the CKD group. Also, the cellular adhesion pathway and integrin cell surface interactions were enriched by positively associated proteins in the CKD group (Table 4).
Protein–protein interaction analysis
Among negatively associated proteins VTDB, showed interactions with B2MG and FETUA, while among positively associated proteins CERU, LV39, IC1, CLUS, VMO1, VTNC, CD59, REG1A, KNG1, CD44, SH3L3, OSTP, A1AG2, RNAS1, UROM, and PTGDS had complex interactions (Supplementary Fig. 1).
Discussion
In this study, label-free quantitative proteomics was used to analyze the comprehensive 24-h urinary proteome of patients with early-stage CKD (stages 1–3) and healthy controls. Unlike prior research that often used spot urine samples and blood samples in CKD12,13,14,25, our approach offers a comprehensive perspective of the urinary proteome in early-stage CKD research. Also, we chose regression analysis adjusted for proteinuria over differential expression analysis to capture the nuanced relationships more accurately between urinary proteins and kidney function. This method allows for the consideration of covariates and predictive biomarkers, providing a comprehensive understanding of the underlying mechanisms involved. The analysis revealed positive and negative associations between kidney function and specific urinary proteins. Furthermore, the study identified distinct urinary protein profiles in CKD patients compared to healthy participants. Notably, proteins negatively associated with eGFR in CKD patients exhibited functional enrichment in processes related to tissue and structural homeostasis as well as immune system activity. Furthermore, positively associated proteins in CKD participants demonstrated significant enrichment in pathways related to extracellular matrix organization, cellular adhesion, coagulation, and the regulation of the immune system and enzyme activities.
Proteinuria is a complex pathophysiological process involving two common renal mechanisms: (i) abnormal protein excretion from the glomerular filter barrier, leading to glomerular proteinuria, and (ii) a disturbance in renal tubular handling of filtered proteins, causing tubular proteinuria. Heavy glomerular proteinuria places a significant strain on proximal tubular epithelial cells (PTECs). Alongside the toxic effects of proteinuria, this strain induces tubulointerstitial inflammation and fibrosis11. In routine clinical practice, only a few urinary proteins, such as kappa/lambda light chains and albumin, are employed as diagnostic markers. However, many other proteins remain undetectable and/or are not utilized in laboratory diagnostics.
We observed a substantially higher number of urinary proteins in healthy participants than in CKD patients (Table 1). Analyzing proteomes in complex biological samples is difficult, primarily because of the wide range of protein concentrations. In plasma, for instance, highly abundant proteins such as immunoglobulins and albumin, which can vary by over 10 orders of magnitude in concentration, can obscure the detection of low-abundant proteins, complicating the effectiveness of the MS method26. Similarly, the masking effect of highly abundant proteins can be observed when analyzing the urinary proteome of CKD patients, who have elevated levels of urinary albumin and other abundant proteins, making the identification of low-concentration urinary proteins challenging27,28.
Interestingly, our study's results align with prior research on the correlation patterns between protein molecular weight categories and renal markers. High molecular weight proteins (> 60 kDa), including KNG1, CD44, CERU, and UROM, exhibited a statistically significant positive correlation with eGFR in the whole cohort (Table 2). This consistency supports the notion that larger molecular weight proteins can serve as indicators of renal function29,30,31. Similarly, negative correlations of low molecular weight proteins, including FETUA, B2MG, IGK, KVD20, IGL1, VTDB, and IGHA1, with eGFR reflect trends observed in earlier studies32,33,34,35. On the other hand, low molecular weight proteins (< 60 kDa), such as VMO1, VTNC, CD59, REG1A, LV39, SH3L3, OSTP, A1AG2, RNAS1, and PTGDS, demonstrated positive correlations with eGFR in the whole cohort.
The regression analyses shed light on the complex relationship between urinary proteins and kidney function. Notably, proteins with negative coefficients, such as B2MG, FETUA, IGK, and VTDB, consistently exhibited associations with eGFR in the entire cohort, even after adjusting for proteinuria. Importantly, our further group-specific comprehensive analysis revealed that, among correlated proteins in the CKD group (Table 3), B2MG, FETUA, VTDB, and AMBP consistently demonstrated associations with eGFR, even after accounting for proteinuria (Figs. 2 and 3). These consistent negative associations raise the possibility regarding the role of these proteins as potential biomarkers for underlying kidney dysfunction.
In addition, the positively correlated proteins, including A1AG2, CD44, CD59, CERU, KNG1, LV39, OSTP, RNAS1, SH3L3, and UROM, exhibited robust associations with eGFR in the entire cohort, persisting even after adjustment for proteinuria. However, after group-specific analysis, only LV39, A1BG, and CERU, which were positively correlated with eGFR in the CKD group (Table 3), exhibited consistent associations with kidney function (Figs. 2 and 3). Persistent associations of these proteins suggest that elevated levels of these proteins in urine may reflect high or normal eGFR, indicating preserved kidney function. Exploring the clinical implications of these findings could pave the way for novel diagnostic approaches and therapeutic strategies.
The increase in low molecular weight proteins in urine, negatively associated with eGFR in patients, primarily reflects proximal tubular dysfunction and reduced tubular reabsorption36. Several studies have indicated the utility of urine B2MG levels in diagnosing tubular injury induced by sepsis, aminoglycosides, tenofovir, lithium, and heavy metals33. Also, elevated urinary B2MG levels have been linked to ongoing tubular dysfunction in adults with snake venom poisoning, persisting even after 6 months of eGFR recovery37, and were associated with lower eGFR after 1 year of acute kidney disease38. Besides, B2MG has been shown to induce oxidative damage to PTECs through the cadmium–B2MG complex and the FcRn–B2MG complex in proteinuric CKD33,39. Notably, an enrichment of an oxidative damage pathway was also reported in proteinuric patients, although this was not specifically linked to B2MG40. Another negatively associated protein, FETUA (fetuin-A), a hepatic secretory protein involved in various physiological processes, has emerged as another potential biomarker. Recent studies have reported an association between urinary FETUA and eGFR, suggesting its relevance in monitoring kidney function decline34,41. FETUA has also been found to protect kidneys from hypoxia-induced kidney damage, inflammation, and fibrosis42. Similarly, urinary AMBP (alpha-1-microglobulin/bikunin precursor) is a hepatic secretory protein readily filtered by the glomerulus and reabsorbed by PTECs. AMBP exhibits reductase, radical-scavenging, and heme-binding activities, protecting PTECs from oxidative damage by supporting mitochondrial function43. An increase in urinary AMBP levels has been noted as a marker of tubular dysfunction in patients with IgA nephropathy, diabetes and CKD29,44. VTDB (vitamin D-binding protein), the primary transporter protein of plasma vitamin D, has shown significant associations with eGFR and kidney function decline in studies on diabetic nephropathy and IgA nephropathy29,32. These consistent findings across different studies underscore the potential clinical significance of these proteins as indicators of kidney dysfunction and warrant further investigation into their diagnostic and prognostic utility. Our functional enrichment analysis results were also consistent with existing data that negatively associated proteins were predominantly associated with pathways involved in immune dysregulation and inflammatory response modulation corresponding to early-stage CKD pathology.
Among positively associated proteins with eGFR in patients, CERU (ceruloplasmin) is a high-molecular-weight protein and is responsible for 95% copper transport in the blood45. CERU was previously reported to correlate positively with eGFR in IgA nephropathy29. Normally, CERU (ceruloplasmin) is not freely filtered by the glomerulus. However, CERU can enter the tubule lumen during proteinuria and exert cytotoxic effects on PTECs under acidic conditions, thereby contributing to kidney pathology46. Other positively associated proteins, such as A1BG (alpha-1B-glycoprotein) and LV39 (immunoglobulin lambda variable 3–9) have received limited attention in the context of CKD, with few studies investigating their significance in this condition. A1BG, a plasma glycoprotein, previously was suggested as a marker to differentiate steroid-resistant nephrotic syndrome from non-resistant conditions in children47. Interestingly, in a recent study, A1BG was significantly upregulated in urine of snakebite patients with acute kidney injury (AKI)48. However, CKD and AKI have different causes, pathophysiological mechanisms, and progression, although there might be some overlap in biomarkers49. Overall, the functional enrichment of positively associated proteins with kidney function shows molecular mechanisms crucial for extracellular matrix organization, immune defense, and coagulation in CKD patients. The regulation of the extracellular matrix is essential to suppress its accumulation, prevent fibrosis formation, and maintain intercellular and ECM integrity. Importantly, proteinuria is a known contributor to renal inflammation and fibrosis by inhibiting the degradation of ECM components and inducing extracellular matrix synthesis, ultimately leading to ESKD50. Furthermore, the marked enrichment of platelet function-related pathways probably indicates increased platelet accumulation and activation due to glomerular injury to block blood loss after vascular damage. Activated platelets can interact with white blood cells and promote inflammatory kidney diseases51,52. Aggregates formed by platelet-white blood cell interaction were suggested to represent a marker of renal diseases and the prognosis of patients in a study by Finsterbusch et al.52. Therefore, the reduction of positively associated urinary proteins may contribute to the progression of CKD by affecting the immune system, blood clotting, and extracellular matrix organization pathways.
In the final step, interactions within proteins negatively and positively associated with eGFR were observed. VTDB exhibited the highest interactions among the negatively associated proteins. CLUS, IC1, KNG1, VTNC, CERU, OSTP, A1AG2, and UROM demonstrated the highest interactions among the positively associated proteins.
Our current findings build upon our pilot study, offering significant advancements in understanding urinary proteomics in CKD35. By including a larger sample size and meticulous data analysis, we have strengthened the reliability of our results. Unlike our pilot study, where we grouped participants based solely on proteinuria levels, this study used KDIGO guidelines, considering both eGFR and proteinuria. We also delved deeper into the association between the urinary proteome and eGFR, using correlation and regression analyses separately for the CKD and control groups. This provides a more comprehensive understanding compared to our previous study, which only used correlation analysis across the entire cohort due to its smaller sample size.
Despite the potential of urinary proteomics (using mass spectrometry) in identifying biomarkers for kidney disease, their limitations must be considered. The emPAI is a semiquantitative computational approach to estimate protein abundance and has inherent limitations and may not represent accurate protein abundance. Thus, validation of individual proteins using sensitive and specific immunoassays such as ELISA is needed to accurately quantify the protein abundance and confirm the reliability of the results. Furthermore, patients with early-stage CKD (1–3) were enrolled in this study. Therefore, they need follow-up to address alterations for the current findings and whether significantly associated proteins are early potential biomarkers of CKD progression. Next, the number of participants in the CKD groups is limited. Additionally, there was a gender imbalance between the patient and control groups. This imbalance may introduce potential confounding factors that could influence the interpretation of our results. Thus, a study with a larger sample size with more balanced gender representation in groups is needed to validate the current findings. During urine sample preparation for MS analysis, depletion of high-abundant proteins was not performed, limiting the identification of low-abundant urinary proteins in patients compared to controls. Finally, the glomerular disease diagnosis was not validated by kidney biopsy.
In this proteomics study, the type and number of urinary proteins differed substantially between patients in CKD stages 1–3 and healthy control participants. Specific urinary proteins demonstrated strong negative and positive associations with kidney function. Proteins with a negative association exhibited significant enrichment in pathways related to structural and tissue homeostasis and immune response. Proteins with a positive association exhibited significant enrichment in pathways related to extracellular matrix organization, cellular adhesion, coagulation, and the regulation of the immune system and enzyme activities in the early stages of CKD. Further validation studies are recommended to confirm the significance of each urinary protein associated with kidney function using immunoassay methods.
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Sundström, J. et al. Prevalence, outcomes, and cost of chronic kidney disease in a contemporary population of 2.4 million patients from 11 countries: The CaReMe CKD study. Lancet Reg. Health Eur. 20, 100438 (2022).
Hill, N. R. et al. Global prevalence of chronic kidney disease—a systematic review and meta-analysis. PLoS ONE 11, e0158765 (2016).
Wang, H. et al. Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet 388, 1459–1544 (2016).
Thomas, B. et al. Global cardiovascular and renal outcomes of reduced GFR. J. Am. Soc. Nephrol. 28, 2167 (2017).
Foreman, K. J. et al. Forecasting life expectancy, years of life lost, and all-cause and cause-specific mortality for 250 causes of death: Reference and alternative scenarios for 2016–40 for 195 countries and territories. Lancet 392, 2052–2090 (2018).
Gansevoort, R. T. et al. Chronic kidney disease and cardiovascular risk: Epidemiology, mechanisms, and prevention. Lancet 382, 339–352 (2013).
Kalantar-Zadeh, K., Jafar, T. H., Nitsch, D., Neuen, B. L. & Perkovic, V. J. T. I. Chronic kidney disease. Lancet 398, 786–802 (2021).
Cravedi, P. & Remuzzi, G. Pathophysiology of proteinuria and its value as an outcome measure in chronic kidney disease. Brit. J. Clin. Pharmacol. 76, 516–523 (2013).
Chen, C.-H. et al. Proteinuria as a therapeutic target in advanced chronic kidney disease: A retrospective multicenter cohort study. Sci. Rep. 6, 26539 (2016).
Krolewski, A. S., Skupien, J., Rossing, P. & Warram, J. H. Fast renal decline to end-stage renal disease: An unrecognized feature of nephropathy in diabetes. Kidney Int. 91, 1300–1311 (2017).
Makhammajanov, Z. et al. Tubular toxicity of proteinuria and the progression of chronic kidney disease. Nephrol. Dial. Transpl. 39, 589–599 (2024).
Ramírez Medina, C. R. et al. Proteomic signature associated with chronic kidney disease (CKD) progression identified by data-independent acquisition mass spectrometry. Clin. Proteomics 20, 19 (2023).
Good, D. M. et al. Naturally occurring human urinary peptides for use in diagnosis of chronic kidney disease. Mol. Cell. Proteomics 9, 2424–2437 (2010).
Choi, Y. W. et al. Potential urine proteomics biomarkers for primary nephrotic syndrome. Clin. Proteomics 14, 1–9 (2017).
Levin, A. et al. Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int. Suppl. 3, 1–150 (2013).
Inker, L. A. et al. New creatinine-and cystatin C-based equations to estimate GFR without race. N. Engl. J. Med. 385, 1737–1749 (2021).
Gaipov, A. et al. Development and validation of hybrid Brillouin-Raman spectroscopy for non-contact assessment of mechano-chemical properties of urine proteins as biomarkers of kidney diseases. BMC Nephrol. 21, 1–9 (2020).
Sun, W., Gao, Y. J. R., Methods, U. P. Protocols. In Renal and Urinary Proteomics: Methods and Protocols. 271–279 (Wiley, 2009).
Ishihama, Y. et al. Exponentially modified protein abundance index (emPAI) for estimation of absolute protein amount in proteomics by the number of sequenced peptides per protein* s. Mol. Cell. Proteomics 4, 1265–1272 (2005).
org. Hs. eg. db: Genome wide annotation for Human v. R package version 3.16.0. (2022).
Wu, T. et al. clusterProfiler 4.0: A universal enrichment tool for interpreting omics data. Innovation 2, 100141 (2021).
Yu, G. & He, Q.-Y.J.M.B. ReactomePA: An R/Bioconductor package for reactome pathway analysis and visualization. Mol. Biosyst. 12, 477–479 (2016).
Szklarczyk, D. et al. STRING v11: Protein–protein association networks with increased coverage, supporting functional discovery in genome-wide experimental datasets. Nucleic Acids Res. 47, D607–D613 (2019).
Wickham, H. & Wickham, H. Data Analysis (Springer, 2016).
Shama, A. et al. The latest developments in using proteomic biomarkers from urine and serum for non-invasive disease diagnosis and prognosis. Biomark. Insights 18, 11772719231190218 (2023).
Borberg, E., Pashko, S., Koren, V., Burstein, L. & Patolsky, F. J. A. C. Depletion of highly abundant protein species from biosamples by the use of a branched silicon nanopillar on-chip platform. Anal. Chem. 93, 14527–14536 (2021).
Filip, S. et al. Comparison of depletion strategies for the enrichment of low-abundance proteins in urine. PLoS ONE 10, e0133773 (2015).
Govender, I. S., Mokoena, R., Stoychev, S. & Naicker, P. J. P. Urine-HILIC: Automated sample preparation for bottom-up urinary proteome profiling in clinical proteomics. Proteomes 11, 29 (2023).
Kalantari, S. et al. Urinary prognostic biomarkers and classification of IgA nephropathy by high resolution mass spectrometry coupled with liquid chromatography. PLoS ONE 8, e80830 (2013).
Prikryl, P. et al. Proteomic approach for identification of IgA nephropathy-related biomarkers in urine. Physiol. Res. 66, 621–632 (2017).
Schaeffer, C., Devuyst, O. & Rampoldi, L. Uromodulin: Roles in health and disease. Annu. Rev. Physiol. 83, 477–501 (2021).
Shoukry, A., Bdeer, S.E.-A. & El-Sokkary, R. H. J. M. Urinary monocyte chemoattractant protein-1 and vitamin D-binding protein as biomarkers for early detection of diabetic nephropathy in type 2 diabetes mellitus. Mol. Cell Biochem. 408, 25–35 (2015).
Argyropoulos, C. P. et al. Rediscovering beta-2 microglobulin as a biomarker across the spectrum of kidney diseases. Front. Med. 4, 73 (2017).
Bassey, P. E. et al. Causal association pathways between fetuin-A and kidney function: A mediation analysis. J. Int. Med. Res. 50, 03000605221082874 (2022).
Gaipov, A. et al. Urinary protein profiling for potential biomarkers of chronic kidney disease: A pilot study. Diagnostics 12, 2583 (2022).
Christensen, E. I., Birn, H., Storm, T., Weyer, K. & Nielsen, R. J. P. Endocytic receptors in the renal proximal tubule. Physiology 27, 223–236 (2012).
Jaswanth, C. et al. Short-term changes in urine beta 2 microglobulin following recovery of acute kidney injury resulting from snake envenomation. Kidney Int. Rep. 4, 667–673 (2019).
Puthiyottil, D. et al. Role of urinary beta 2 microglobulin and kidney injury molecule-1 in predicting kidney function at one year following acute kidney injury. Int. J. Nephrol. Renov. 14, 225–234 (2021).
Fels, J. et al. Cadmium complexed with β2-microglubulin, albumin and lipocalin-2 rather than metallothionein cause megalin: Cubilin dependent toxicity of the renal proximal tubule. Int. J. Mol. Sci. 20, 2379 (2019).
Hao, Y. et al. Changes of protein levels in human urine reflect the dysregulation of signaling pathways of chronic kidney disease and its complications. Sci. Rep. 10, 20743 (2020).
Piazzon, N. et al. Urine Fetuin-A is a biomarker of autosomal dominant polycystic kidney disease progression. J. Transl. Med. 13, 1–11 (2015).
Chekol Abebe, E. et al. The structure, biosynthesis, and biological roles of fetuin-A: A review. Front. Cell. Dev. Biol. 10, 945287 (2022).
Kristiansson, A. et al. α1-Microglobulin (A1M) protects human proximal tubule epithelial cells from heme-induced damage in vitro. Int. J. Mol. Sci. 21, 5825 (2020).
Amatruda, J. G. et al. Biomarkers of kidney tubule disease and risk of end-stage kidney disease in persons with diabetes and CKD. Kidney Int. Rep. 7, 1514–1523 (2022).
Lopez, M. J., Royer, A. & Shah, N. J. Biochemistry, Ceruloplasmin (StatPearls Publishing, 2020).
Ito, S. et al. Urinary copper excretion in type 2 diabetic patients with nephropathy. Nephron 88, 307–312 (2001).
Piyaphanee, N. et al. Discovery and initial validation of α 1-B glycoprotein fragmentation as a differential urinary biomarker in pediatric steroid-resistant nephrotic syndrome. Proteomics Clin. Appl. 5, 334–342 (2011).
Brasileiro-Martins, L. M. et al. Urinary proteomics reveals biological processes related to acute kidney injury in Bothrops atrox envenomings. PLoS Negl. Trop. Dis. 18, e0012072 (2024).
Van Nynatten, L. R. et al. A novel multiplex biomarker panel for profiling human acute and chronic kidney disease. Sci. Rep. 13, 21210 (2023).
Stephan, J.-P. et al. Albumin stimulates the accumulation of extracellular matrix in renal tubular epithelial cells. Am. J. Nephrol. 24, 14–19 (2004).
Gros, A., Ollivier, V. & Ho-Tin-Noé, B. Platelets in inflammation: Regulation of leukocyte activities and vascular repair. Front. Immunol. 5, 678 (2015).
Finsterbusch, M., Schrottmaier, W. C., Kral-Pointner, J. B., Salzmann, M. & Assinger, A. J. P. Measuring and interpreting platelet-leukocyte aggregates. Platelets 29, 677–685 (2018).
Funding
This project was funded with support from the Nazarbayev University Collaborative Research Program (Funder Project Reference: 211123CRP1603).
Author information
Authors and Affiliations
Contributions
A.G. and Z.M. conceived and designed the project; Z.M., D.A., and P.T. performed the experiments and acquired the data; Z.M. performed the data analysis, visualization, and interpretation and wrote the manuscript; A.G. and S.H.A. contributed to data analysis and interpretation; A.G., R.B., and D.T. acquired funding; A.K. provided resources; A.G., C.P.K., M.Z.M., M.K., and S.H.A. reviewed and edited the manuscript. All authors agreed to the order of authorship. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Makhammajanov, Z., Kabayeva, A., Auganova, D. et al. Candidate protein biomarkers in chronic kidney disease: a proteomics study. Sci Rep 14, 14014 (2024). https://doi.org/10.1038/s41598-024-64833-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-64833-8
- Springer Nature Limited